Dietary factors are implicated in approximately one in five deaths globally and are intricately linked to CVD and metabolic conditions, including coronary artery disease, stroke and type 2 diabetes(Reference Bauer, Briss and Goodman1–Reference Yoon, Bastian and Anderson3). CVD is the leading cause of morbidity and mortality worldwide, and disease prevalence in adults over the age of 20 years in the USA is 48 %(Reference Benjamin, Muntner and Alonso4). By 2035, CVD is projected to cost the US 1·1 trillion dollars in direct medical costs and indirect costs such as lost workplace productivity(5). Overall, food preferences and eating behaviours are major aetiological factors involved in the development of CVD and other lifestyle diseases(Reference Sahoo, Sahoo and Choudhury6).
In the USA in 2013–2014, 32% of the energy Americans consumed came from food away from home, with 12·9% of overall consumption coming from fast foods(Reference Todd7). The consumption of any type of food away from home is correlated with higher saturated fat and cholesterol intake and lower total fibre consumption(Reference Todd7,Reference An8) , and fast food, food away from home, is associated with increased dietary salt exposure and decreased intake of key vitamins and minerals(Reference An8). In contrast, adherence to the Mediterranean diet is directly correlated with decreased all-cause mortality, reduced incidence of CVD and overall chronic disease, and a decreased occurrence of coronary artery reocclusion after myocardial infarction(Reference de Lorgeril, Salen and Martin9–Reference Sofi, Cesari and Abbate13). The Mediterranean diet is defined by a high consumption of fibre as well plant and marine fatty acids and a low consumption of saturated fats and dietary cholesterol(Reference de Lorgeril, Salen and Martin9).
Numerous studies have shown that the development of food preferences is significantly influenced by eating environments during childhood and adolescent development(Reference Skinner, Carruth and Bounds14–Reference Cullen, Eagan and Baranowski19). During childhood food preference development, parental dietary habits play a highly influential role. In particular, repeated dietary exposures in childhood increase the preference for such foods later in life(Reference Sullivan and Birch20–Reference Birch and Marlin23). Parents control which foods their children are exposed to or restricted from, exhibit modelling behaviour during meals and impart attitudes about food to their children(Reference Garrahie, Moore and Singer24–Reference Vereecken and Maes29). Therefore, in order to minimise exposure to the typical Western diet and increase consumption and adherence to the Mediterranean diet, nutrition education and modification should begin at a young age. Current literature shows that incorporating hands-on nutritional education as a tool for diet modification can help lead to an increased diffusion of knowledge from parents to children(Reference Dudley, Cotton and Peralta30).
The Goldring Center for Culinary Medicine has previously shown via observational studies that the Health meets Food (HmF) curriculum is associated with improved Mediterranean diet adherence(Reference Monlezun, Leong and Joo31–Reference Monlezun, Dart and Vanbeber34). This proof-of-concept single-site randomised controlled trial expands upon the results of those prior observational studies. We report here the results of a single-site randomised parallel-arm design trial to test the effects of a hands-on, cooking-based nutrition education programme on Mediterranean diet adherence and food cost savings in families living in the Greater New Orleans region.
Materials and methods
Study design
The Cooking for Health Optimization-Family (CHOP-Family) study was a phase I, randomised trial designed to test whether family-oriented hands-on culinary education would improve Mediterranean diet adherence in families compared with standard nutrition education. The CHOP-Family study utilised a parallel design. The unit of recruitment for the current study was families with young children, and recruitment and participation occurred from 1 January 2017 to 20 September 2017.
Written informed consent was obtained from each adult family member participant aged 18 years old or older. The study protocol was approved by the institutional review board at Tulane University.
Study participants
Families in the Greater New Orleans region with at least one child between the ages of 4 and 18 years were included in the current study. Excluded from the study were families with children under the age of 4 years or older than the age of 18 years and households without any children. Thus, families with children outside the pre-specified age range (4–18 years) were excluded. The study participants were recruited through community outreach via brochures in New Orleans, Louisiana. The recruitment phase yielded forty-one families, including fifty-five parents and ninety children, who met eligibility criteria. Among those who met inclusion criteria, eighteen families (44%) were randomised to the intervention.
Intervention and control groups
Families were randomly assigned via a fixed 1:1 allocation ratio to intervention and control groups. The intervention group received hands-on cooking-based nutrition education through the HmF curriculum. The HmF curriculum is currently implemented in over fifty academic medical centres across the USA. The HmF family curriculum is a 12-h nutrition and culinary course delivered as a series of six modules. These modules instruct class participants, both parents and children, on general nutrition concepts and evidence-based principles of the Mediterranean diet through hands-on cooking. For the intervention arm of the study, all nutrition materials and recipes were provided by the Goldring Center for Culinary Medicine. The characteristics of the six modules including (i) kitchen safety, delegation, fundamental skills, (ii) breakfast, (iii) snack and healthy desserts, (iv) packed lunch, (v) make-ahead meals and (vi) compilation of family recipes are described in detail in the online supplementary material, Supplemental Table 1. Every adult and child participant had a primary care physician and paediatrician, respectively, who provided routine care as needed during the study. The control group was assigned to standard nutrition education provided in the participating families’ medical provider offices, none was provided by the Goldring Center for Culinary Medicine and no contact was had until after the control period. This nutrition education consisted of in-office dietary counselling by healthcare providers that advised to follow a Mediterranean dietary pattern rich in fruits, vegetables and unsaturated fats. Each family in the control group was also sent home with nutrition education materials and recipes from their respective physicians.
Outcomes
Mediterranean diet score
The primary end point of the CHOP-Family study is the validated Mediterranean diet adherence score validated by Trichopolou et al.(Reference Trichopoulou, Costacou and Bamia10) in 2003 (see online supplementary material, Supplemental Table 2). Mediterranean diet adherence was assessed in two ways. There were pre- and post-matched survey responses from control and intervention arms as well as collected grocery store receipts from families participating in the study. The receipts were assessed in concordance with the Mediterranean dietary pattern based on the diet’s nine integral components: fruits, vegetables, legumes, whole grains, monounsaturated fats, nuts/seeds, fish, meat and wine. Participants were given a score of 0 or +1 for each of the nine food components using receipt data and a FFQ intended to capture recent dietary habits. A value of +1 was assigned in the following situations: four or more servings per day for vegetables, one or more servings per week for legumes, three or more servings per week for fruit, one or more servings per week for nuts/seeds, less than two and three servings per week of red meat for women and men, respectively, two or more servings per week of non-fried fish, one or more servings per day for whole grains, higher reported intake of unsaturated fats v. saturated fats, half to one drink or less of alcohol per day for women and 1–2 drinks or less of alcohol per day for men. In all other situations, we assigned a 0 for each of the nine food components. Scores were totaled for each participant to yield a continuous composite score, with a higher score corresponding to higher adherence to the Mediterranean diet. In addition to the composite Mediterranean diet score, individual components of the diet score were also assessed as secondary study outcomes. Participants were offered $US 20 grocery store gift certificates to participate in the trial.
Cost efficacy
Among, secondary end points of the CHOP-Family study were cost efficacy or family food cost savings, determined through grocery store receipt data of participating families. Grocery store receipt data were obtained at baseline and after the 6-week intervention phase from families in both the control and intervention arms of the study. Participating families were requested to save receipts throughout the duration of the study and turn in receipt data at the end of the 6-week period. Projected weekly grocery store costs were calculated for each participant family by extrapolating study results and comparing extrapolations with published United States Department of Agriculture (USDA) family food costs and morbidity and mortality data(Reference Trichopoulou, Costacou and Bamia10,35,Reference Estruch, Ros and Salas-Salvadó36) . Supplementary Table 3, originally created by the USDA, is provided as a reference in the online supplementary material.
Statistical analysis
The CHOP-Family study was designed to provide >80% statistical power to detect a 15% increase in high or medium v. low Mediterranean diet adherence at a significance level of 0·05 using a two-tailed t test. A fixed-effects regression panel analysis was used to assess the effects of hands-on cooking education on the change in composite Mediterranean diet score, individual Mediterranean diet score components and family-level food cost savings(Reference Kabat, Heo and Allison37,Reference Saksena, Okrent and Anekwe38) . The fixed-effects panel analysis was conducted in STATA 14.2 (StataCorp) and used to obtain point estimates and CI, accounting for time invariant unobserved and unbalanced baseline covariates.
Results
The baseline characteristics of participating families by randomisation groups are displayed in Table 1. There were a total of eighteen families (sixty-two individuals) in the treatment arm and twenty-three families (eighty-three individuals) in the control arm. Families in the treatment group participated in 3·9 culinary medicine classes on average over 6 weeks, while those in the control group did not participate in culinary medicine education. There was a similar proportion of female children in both the treatment and control groups (55·2 v. 55·7%). The mean number of children per family (2·1 v. 2·2) and their average ages (10·7 v. 9·8 years) were comparable between the treatment and control groups. Class attendance rates for the treatment group are presented in Fig. 1.
Table 1 Characteristics of families randomised to treatment and control groups
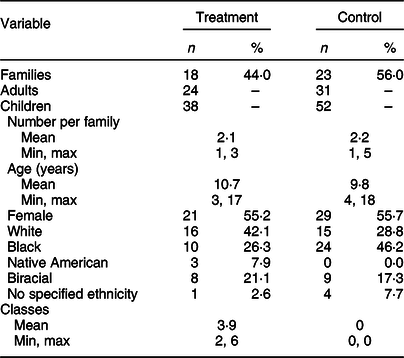
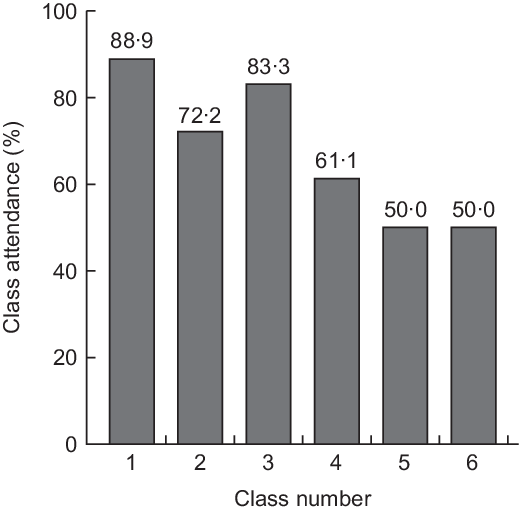
Fig. 1 Class attendance for families randomised to teaching kitchen-based nutrition education
Table 2 demonstrates the relationship between HmF curricula and Mediterranean diet adherence. Hands-on cooking and nutritional education improved Mediterranean diet score by 0·43 points on a nine-point scale (B 0·43, 95% CI 0·22, 0·65; P < 0·001). Compared with families receiving in-office nutrition education, families participating in kitchen-based nutrition classes experienced nearly a 3-fold increase in high or medium v. low Mediterranean adherence (OR 2·93, 95% CI 1·73, 4·95; P < 0·001). Similarly, HmF curricula significantly increased fruit (OR 4·54, 95% CI 2·52, 8·20; P < 0·001) and vegetable (OR 2·33, 95% CI 1·42, 3·80; P = 0·001) consumption by over 4-fold and 2-fold, respectively. Compared with the control group, families participating in the 6-week culinary education module series experienced a 65% increase in the consumption of whole grains (OR 1·65, 95% CI 1·15, 2·38; P = 0·007). There were no statistically significant differences in olive oil, legume, seafood, alcohol and red meat consumption between families assigned to hands-on cooking-based nutritional education and . traditional nutrition education.
Table 2 Effect of kitchen-based nutrition education on Mediterranean diet adherence and food cost savings, compared with standard nutrition education
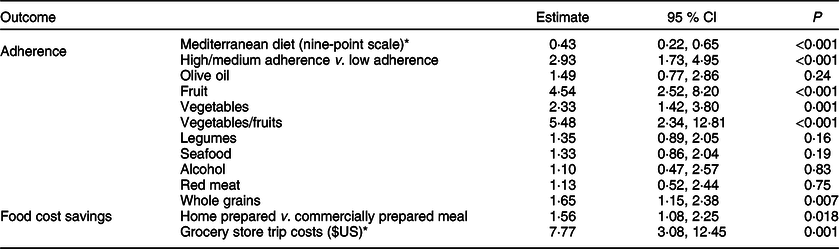
All parameter estimates are OR for kitchen-based nutrition education (intervention) compared with standard nutrition education (control), unless otherwise noted.
* Beta parameter estimate for kitchen-based nutrition education (intervention).
Participants receiving hands-on nutrition education and those receiving standard dietary counselling attended the grocery store a similar number of times per week (1·71 v. 1·83, P = 0·15). Although kitchen-based nutrition education led to an increase of $US 7·77 spent per grocery store trip compared with control, the kitchen-based curriculum was associated with an overall weekly cost savings by increasing the likelihood of home-prepared meals (OR 1·56, 95% CI 1·08, 2·25; P = 0·018). Based on current USDA statistics of an American family of four eating out 4·2 times per week, at a cost of $US 12·75 per meal and at current average grocery store costs for home-cooked supplies at $US 4 per person per home-cooked meal(Reference Saksena, Okrent and Anekwe38), switching one family meal from commercially prepared to home-cooked was projected to save families participating in kitchen-based education of $US 21·70 per week.
Discussion
Here, we have identified that kitchen-based nutrition education increases Mediterranean diet adherence among a diverse sample of families living in the Greater New Orleans region. Likewise, the pilot culinary medicine intervention was also projected to save families at least $US 20 per week by increasing the likelihood of home meal preparation. Diet is a crucial component in the prevention of CVD, serving as a major modifiable protective factor for incident events and mortality. Thus, it is of primary importance that prevention begins at a young age. When compared with other strategies for teaching nutritional health (e.g., enhanced curriculum, cross-curricular approaches, games approach), methods which utilise experiential learning, that is, cooking classes, are superior tools for altering child nutritional knowledge and behaviours(Reference Dudley, Cotton and Peralta30).
The current literature has shown that family-oriented early interventions are more effective in inducing favourable changes in children’s dietary preferences and eating behaviours than those which do not incorporate parental involvement. Parental involvement is also associated with habit maintenance, indicating that these interventions create a long-lasting shift in family dynamics and attitudes surrounding food(Reference Hingle, O’Connor and Dave39). Additionally, prior studies have demonstrated that children participating in child−parent partnered cooking classes experience higher vegetable consumption, enhanced kitchen skillset and an increase in self-efficacy with respect to asking for specific ingredients(Reference Hersch, Perdue and Ambroz40). Our study builds upon this literature by showing that hands-on cooking classes based on the Mediterranean diet also beneficially shift children’s dietary preferences in a low-income urban community setting.
While previous studies have incorporated hands-on cooking classes as part of a family-oriented early intervention, to our knowledge, none of them have incorporated hands-on cooking classes based on the Mediterranean diet. This pilot study is unique in that it utilises the strengths of family-centred cooking education and applies them to ensure increased Mediterranean diet adherence. By combining the two, we are not only allowing individuals to benefit from the empirically proven beneficial outcomes of the Mediterranean diet but also encouraging them to decrease their consumption of food away from home. Home-cooked meals save money and further reinforce healthy consumption habits. Thus, our intervention challenges the commonly held perception among low-income communities that healthy eating is necessarily cost-prohibitive(Reference Haws, Reczek and Sample41), indicating instead that the Mediterranean diet is one of the best options financially and healthwise for economically disadvantaged populations. As a result, these data suggest that our intervention could be used to educate low-income families, and that cost does not need to be a barrier to health.
Our results underline the importance of early childhood nutrition education by leaning on the strengths of the experiential learning model. Furthermore, our findings highlight the concept that experiential intervention programmes are highly successful in favourably altering family dynamics around food and children’s dietary preferences, particularly in low-income areas that lack access and education regarding affordable healthy food choices.
Notable limitations of the current study are the preliminary nature of our findings (single-site pilot study) and an inability to collect medical and cost data for all subjects. We specifically relied on grocery store receipts to conduct cost analyses, and participating families may have not submitted all grocery store receipts. Additionally, the fact that a food item is on the grocery store receipt does not necessarily guarantee that this item was consumed. Restaurant receipts were also not collected. Moreover, an important drop-off in class attendance was noted during the final 3 weeks of the intervention. Attrition has been a recognised issue with hands-on programming. Six weeks of classes are a significant commitment for many community members, and alternate means of attendance, including virtual programming using multimedia education, is a possible solution. Future studies can further build on our findings by expanding sample size and including multiple sites. Other improvements could include employing more thorough and accurate measures for recording actual food consumption. Additionally, the current study did not analyse the control group (traditional dietary counselling) for improvement in dietary habits above baseline, and instead, specifically focused on the effect of culinary medicine education v. traditional dietary counselling on Mediterranean diet adherence. Further work is required to determine the direct impact of family-centred culinary education classes on reducing hospital readmissions, morbidity and mortality. Follow-up studies which examine whether these changes in children’s food preferences and eating behaviours are maintained over time would also be of great value.
Conclusion
Altering children’s food preferences and eating behaviours through interventions aimed at shifting family dynamics and attitudes around food is a means to alter both the general nutritional and health status of children and parents. Our results indicate that hands-on family cooking and nutrition classes increase overall Mediterranean diet adherence among families and shift children’s food preferences and eating behaviours more towards a plant-based dietary pattern. Secondary analyses based on grocery store receipt data also suggest that kitchen-based nutrition education would produce projected food cost savings of at least $US 20 per week by increasing the likelihood of home-prepared meals. Further research should examine whether these changes in family dynamics and children’s food preferences and eating behaviours are long-lasting shifts, and whether such interventions can lower the burden of CVD among communities.
Acknowledgements
Acknowledgement: None. Financial support: The current study phase was funded through a grant from the Humana Foundation, grant no. 553 693. Conflict of interest: The authors have no competing interests to declare. Authorship: A.C.R. carried out statistical analysis, contributed to the interpretation of results and wrote the manuscript. A.S. contributed to the interpretation of results and in writing the manuscript. D.J.M. conceived and planned the study and carried out the statistical analysis. I.G.M. contributed to the interpretation of results and contributed to the final version of the manuscript. A.L. contributed to the interpretation of results and contributed to the final version of the manuscript. K.P. conceived, planned and carried out the study. C.M. planned and carried out the study. L.S. conceived, planned and carried out the study. E.S. planned and carried out the study. A.D. planned and carried out the study and contributed to the final version of the manuscript. T.S.H. conceived, planned and supervised the study and contributed to the final version of the manuscript. Ethics of human subject participation: The current study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by the Tulane University Institutional Review Board. Written informed consent was obtained from all subjects.
Supplementary material
For supplementary material accompanying this paper, visit https://doi.org/10.1017/S1368980020002256.






