Chronic disease is a growing cause of mortality and morbidity worldwide( 1 ). Fruit and vegetable intake is inversely associated with the risk of developing chronic disease, including CVD, type 2 diabetes and some cancers( Reference Liu, Li and Li 2 – Reference Aune, Lau and Chan 4 ). Adequate fruit and vegetable intake also confers other health benefits including reduced risk of hip fracture, obesity and age-related cognitive decline( Reference Byberg, Bellavia and Orsini 5 , Reference Loef and Walach 6 ). About 2·635 million deaths worldwide per year are attributed to inadequate fruit and vegetable consumption( Reference Lock, Pomerleau and Causer 7 ). Emerging evidence suggests that trends in chronic disease incidence could be significantly reversed by an increase in fruit and vegetable consumption( Reference Gundgaard, Nielsen and Olsen 8 ). As a result of this evidence, increasing fruit and vegetable intake is part of the WHO global public health strategy for the prevention of non-communicable diseases( 9 ).
Most national dietary guidelines have a strong focus on fruit and vegetable intake. Despite these recommendations, the majority of the population does not consume sufficient fruits and vegetables. In Australia, only 11 % of adults consume the recommended two servings of fruits and five servings of vegetables daily( Reference Magarey, McKean and Daniels 10 ); while in the USA, less than half of the population meets the recommended daily intake of five servings of fruits or vegetables daily( Reference Guenther, Dodd and Reedy 11 ). Inadequate intake of fruits and vegetables has significant direct and indirect costs to the economy. In Canada, low intake is estimated to cost $CAN 3·3 billion per year, with 30 % attributed to direct health-care costs related to ill health and 70 % to costs incurred by loss of productivity( Reference Ekwaru, Ohinmaa and Loehr 12 ). It is estimated that an increase of one serving of fruit and one serving of vegetable daily would result in savings of $CAN 9·2 billion over 20 years( Reference Ekwaru, Ohinmaa and Loehr 12 ).
For people in the community, lack of adequate dietary information or difficulty engaging with available information could contribute to the low uptake of national dietary recommendations. Clear information or knowledge gaps have been recently identified, as fewer than half of the Australian population reported that they believed that inadequate fruit and vegetable intake is associated with the risk of developing cancer( Reference Chapman, Havill and Watson 13 ). This implies a role for health literacy in increasing fruit and vegetable intake. Health literacy is defined as ‘the cognitive and social skills which determine the motivation and ability of individuals to gain access to, understand and use information in ways which promote and maintain good health’( Reference Nutbeam 14 ). The WHO describes health literacy as a fundamental pillar of health promotion, highlighting that knowledge and understanding remain powerful tools in health promotion. Improving health literacy in populations enables people to play an active role in improving their own health and to engage successfully with community action for health( 9 ). Low health-related reading and numeracy (i.e. functional health literacy) has been associated with poor health outcomes including less use of preventive services, higher rates of hospitalisation and poor overall health status( Reference Berkman, Sheridan and Donahue 15 ). Higher health literacy is associated with positive health behaviours including better self-care in asthma and diabetes, having regular meals and having sufficient physical activity( Reference Berkman, Sheridan and Donahue 15 , Reference Geboers, Reijneveld and Jansen 16 ).
Most previous studies have used unidimensional measures of health literacy, focusing on functional health literacy. To advance the field, we used the nine-scale Health Literacy Questionnaire (HLQ)( Reference Osborne, Batterham and Elsworth 17 ) which captures the wider concepts of health literacy. The aim of the present study was to determine whether health literacy and sociodemographic characteristics were associated with fruit and vegetable intake in adults residing in a rural region of Australia.
Methods
Participants
Participant recruitment took place within a larger study that investigated the cancer care pathway in the Grampians region of Victoria, Australia, between February and September 2015. We sought to include people who were representative of the wider community including those who may have low health literacy. We therefore undertook face-to-face recruitment at community events (e.g. agricultural events, fishing competitions) across the eleven local government areas in the region. Inclusion criteria were being aged >18 years, resident in the region and not previously diagnosed with cancer. All participants provided informed consent. As part of the larger study, people who had been diagnosed with cancer within the last 5 years were recruited but were excluded from the present study.
Measurements
Questionnaires were collected through face-to-face interview or self-administered. Health literacy was measured using the HLQ( Reference Osborne, Batterham and Elsworth 17 ), which has nine scales:
-
1. Feeling understood and supported by health-care providers;
-
2. Having sufficient information to manage my health;
-
3. Actively managing my health;
-
4. Social support for health;
-
5. Appraisal of health information;
-
6. Ability to actively engage with health-care providers;
-
7. Navigating the health-care system;
-
8. Ability to find good health information; and
-
9. Understand health information well enough to know what to do.
The HLQ was developed using a validity-driven approach( Reference Buchbinder, Batterham and Elsworth 18 ). Each scale was derived from extensive consultation with stakeholders and has four to six items. Responses in the first five scales were: 1=‘strongly disagree’, 2=‘disagree’, 3=‘agree’ and 4=‘strongly agree’. Responses to the remaining four scales were: 1=‘cannot do or always difficult’, 2=‘usually difficult’, 3=‘sometimes difficult’, 4=‘usually easy’ and 5=‘always easy’. These scales demonstrate high construct validity and reliability (composite reliability scores 0·8–0·9)( Reference Osborne, Batterham and Elsworth 17 ). Fruit and vegetable intake was assessed by asking: ‘On a typical day, how many servings of fruit/vegetable do you eat?’ with responses: none, 1, 2 or 3 or more servings. Age, gender, completed secondary education and private health insurance status were also collected.
Statistical methods
All analyses were carried out using the statistical software package IBM SPSS Statistics version 23.0. Descriptive statistics were conducted to describe the demographic characteristics (age, gender, having private health insurance, education), fruit and vegetable intake, and health literacy. Means and sd were calculated for each HLQ scale by adding the total score for that scale and then dividing by the number of items in the scale. Frequencies were provided for fruit and vegetable intakes. Logistic regression was used to estimate the OR of higher fruit and vegetable intakes and 95 % CI for each HLQ scale. Finally, OR were corrected for age, gender, level of education and having private health insurance. Statistical significance was assumed when P<0·05.
Results
A total of 1184 participants completed the survey. The mean age was 52 (sd 17) years and the majority had completed secondary education or higher (see Table 1). Two-thirds of the participants were female. The mean scores for each HLQ scale are presented in Table 2. About half (49 %) reported that they consumed at least 2 servings of fruits daily and 55 % had at least 3 servings of vegetables daily (see Table 1). Higher fruit and vegetable intake was associated with older age, being female and having private health insurance (Table 3). Completing secondary education was predictive of higher vegetable intake but not fruit intake (Table 3).
Table 1 Baseline characteristics of adult participants (n 1184) residing in the rural Grampians region, Victoria, Australia, February–September 2015
Table 2 Health Literacy Questionnaire (HLQ) scores of adult participants (n 1158) residing in the rural Grampians region, Victoria, Australia, February–September 2015
† Possible responses to questions 1 to 5 were: 1=‘strongly disagree’, 2=‘disagree’, 3=‘agree’ and 4=‘strongly agree’.
‡ Possible responses to questions 6 to 9 were: 1=‘cannot do or always difficult’, 2=‘usually difficult’, 3=‘sometimes difficult’, 4=‘usually easy’ and 5=‘always easy’.
Table 3 Associations between health literacy, sociodemographic factors and fruit and vegetable intake, identified in univariate and multivariate logistic regression analyses, among adult participants (n 1111) residing in the rural Grampians region, Victoria, Australia, February–September 2015
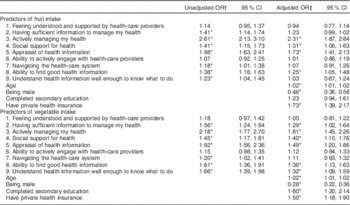
*P<0·05.
† Univariate analyses were performed to determine the relationship between each Health Literacy Questionnaire scale and intake of fruits or intake of vegetables.
‡ Multivariate analyses were performed to determine the relationship between each Health Literacy Questionnaire scale and intake of fruits or intake of vegetables, with age, gender, educational attainment and having private health insurance as covariates to correct for confounding effects.
An increase in ‘Actively managing my health’ score increased the odds of a participant reporting a higher level of fruit intake by 131 % on average, while adjusting for covariates (Table 3). Participants who scored higher on ‘Appraisal of health information’, ‘Ability to find good health information’ and ‘Social support for health’ were also more likely to report a higher level of fruit intake. ‘Ability to actively engage with health-care providers’, ‘Navigating the health-care system’ and ‘Feeling understood and supported by health-care providers’ were not associated with fruit intake.
An increase in ‘Actively managing my health’ score increased the odds of a participant reporting a higher level of vegetable intake by 80 % on average, while adjusting for other covariates (Table 3). Participants with higher scores in ‘Having sufficient information to manage my health’, ‘Appraisal of health information’ and ‘Social support for health’ were also more likely to report a higher vegetable intake after adjusting for age, education and having private health insurance. ‘Ability to actively engage with health-care providers’, ‘Navigating the health-care system’ and ‘Feeling understood and supported by health-care providers’ were not associated with vegetable intake.
Discussion
The present study is the first to use a multidimensional health literacy assessment tool to explore the potential role of health literacy in fruit and vegetable intake. Previous studies have measured functional health literacy only, such as reading comprehension and numeracy skills( Reference Reisi, Javadzade and Heydarabadi 19 , Reference von Wagner, Knight and Steptoe 20 ). We found that among nine key areas of health literacy, ‘Actively managing my health’ has the strongest associations with fruit and vegetable consumption. This scale includes concepts such as making time to be healthy, setting health goals and regularly seeking ways to maintain health. Goal-setting and planning have been previously identified in a meta-regression on behaviour change techniques in diet or physical activity interventions to be the most effective elements in producing lifestyle behavioural changes( Reference Michie, Abraham and Whittington 21 ). The current study provides new insights into the importance of self-regulation skills in adopting and maintaining healthy eating patterns and provides insights into potential intervention points.
We also found that the ability to find and appraise health information was associated with fruit and vegetable intake. A review of thirty-five studies found that knowledge, self-efficacy and social support were the most predictive psychosocial constructs of fruit and vegetable intake in adults( Reference Shaikh, Yaroch and Nebeling 22 ). The current study extends this finding by suggesting that health literacy dimensions around accessing and deciding the validity of health information are also associated with fruit and vegetable intake. The ability to critically appraise information is particularly relevant to nutrition interventions, considering the numerous and conflicting nutritional messages confronted by the public at any time. Further research should aim to understand the process of knowledge management and uptake at the individual level to improve the effectiveness of public health nutrition interventions.
In the current study, males and younger adults were more likely to have lower fruit and vegetable intake, which is consistent with the Australian Health Survey 2011–12( 23 ). Consistent with previous research, we also found that those with higher education were more likely to report higher vegetable consumption( Reference McCabe-Sellers, Bowman and Stuff 24 ). The current study additionally found that health literacy was associated with fruit and vegetable intake independent of these demographic factors. This suggests that health literacy could be targeted to improve health and dietary behaviours in these at-risk populations.
Fruit intake in the present study is comparable to that in the Australian Health Survey in 2011–12, which also reported 49 % of adults aged 18 years or above having at least two servings of fruits daily( 25 ). Vegetable intake in the current study was higher than that reported in the Australian Health Survey 2011–12 (55 v. 49 % having at least three servings of vegetables daily) for adults( 25 ). This is consistent with a recent regional report which described greater vegetable intake in the Grampians region compared with the rest of the state (42 v. 36 %)( 26 ). Together, these data suggest that adults in the Grampians region have greater vegetable intake than the national average, although comparisons between studies should be interpreted with caution due to different biases introduced by different questionnaires used to determine intakes.
A strength of the present study is the large sample size from a region known to have an excess mortality rate for cancer( Reference Coory, Ho and Jordan 27 ). We also employed the widely used and well-tested HLQ with nine robust scales that allowed exploration of additional health literacy needs and strengths not assessed in previous studies on dietary behaviour. The study has some limitations. The measurement of fruit and vegetable intake was self-reported and subject to respondent bias, and the study was cross-sectional, limiting causal conclusions.
Conclusions
Health literacy, particularly being proactive, appraising information and having social support for healthy behaviours, is associated with fruit and vegetable intake. Future interventions should consider the inclusion of health literacy mechanisms in interventions designed to improve fruit and vegetable intake.
Acknowledgements
Acknowledgements: The authors would like to acknowledge Melanie Hawkins, Roy Batterham and Trish Livingston for assisting with the implementation of the project. They also wish to acknowledge the partners in this project for their contribution: the Ballarat Health Services (funder); and the Grampians Integrated Cancer Services (GICS) and the Victorian Department of Health and Human Services for their participation and guidance. Financial support: This work was funded by Ballarat Health Services. R.H.O. is funded in part through a National Health and Medical Research Council (NHMRC) Senior Research Fellowship (grant number #APP1059122). Ballarat Health Services and the NHMRC had no role in the design, analysis or writing of this article. Conflict of interest: All authors declare that they have no competing interests. Authorship: S.L. analysed the data and prepared the manuscript. S.D. led the implementation of the study and contributed to the manuscript. J.O., C.M., A.F. and C.W. implemented the study and contributed to the manuscript. R.H.O. and A.B. contributed to the study design and preparation of the manuscript. All authors have seen and approved the final version of the manuscript. Ethics of human subject participation: This study was approved by the Human Research Ethics Committees of Deakin University (approval number HEAG-H 07_2015), Ballarat Health (approval number HREC/15/BHSSJOG/36), Victorian Cancer Council (approval number HREC1503) and the Royal Australian College of General Practitioners (approval number NREEC15-002). Written or verbal informed consent was obtained from all participants. Verbal consent was obtained from participants who had difficulties reading or writing. In these settings verbal consent was witnessed and noted.






