Introduction
In the United Kingdom there are over 11 million older adults aged 65 years and over who make up 18% of the population (UK Office for National Statistics, 2017). Aligning with the United States and other developed countries (United Nations, 2015) this proportion is projected to increase to at least 24% by 2039 (UK Office for National Statistics, 2017). Although prolongation of life remains an important public health goal, of even greater significance is that extended life should involve preservation of the capacity to live independently, function well and quality of life (Rejeski et al., Reference Rejeski, Axtell, Fielding, Katula, King, Manini, Marsh, Pahor, Rego, Tudor-Locke and Newman2013). The purpose of this formative descriptive study was to explore current knowledge and attitudes towards physical activity (PA), as well as perceived barriers, facilitators and opportunities for PA participation among older adults living in the community. The findings were used to inform the design, delivery and recruitment strategies of an ongoing three-year community PA intervention project, Get Healthy, Get Active (GHGA), which forms part of Sport England’s national GHGA programme (Sport England, 2012).
Background
Guidelines issued by the UK Chief Medical Officers and the US Surgeon Generals recommend that older adults (⩾65 years) engage in at least 150 min of moderate (or 75 min of vigorous) PA per week in bouts of at least 10 min, with muscle-strengthening and balance activities included on at least two of those days (Department of Health, 2011; Centers for Disease Control and Prevention (CDC), 2015). Despite the recognised evidence base for the benefits of regular PA (CDC, 2015; Reid and Foster, Reference Reid and Foster2016; World Health Organization (WHO), 2017), objective summaries of PA levels among older adults show that only 15% of males and 10% of females within the United Kingdom, and 9.5% of males and 7% of females within the United States meet the recommended PA guidelines (Tucker et al., Reference Tucker, Welk and Beyler2011; Jefferis et al., Reference Jefferis, Sartini, Lee, Choi, Amuzu, Gutierrez, Casas, Ash, Lennnon, Wannamethee and Whincup2014). Given that current PA guidelines remain the same for both adults (18–64 years) and older adults (⩾65 years), such high levels of inactivity suggests that PA guidelines appear too demanding for the latter population (Booth and Hawley, Reference Booth and Hawley2015).
Accumulating evidence suggests that prolonged and continuous bouts of sedentary behaviours [SB; defined as waking behaviours in a sitting, reclining or lying posture with energy expenditure ⩽1.5 metabolic equivalents (Tremblay et al., Reference Tremblay, Aubert, Barnes, Saunders, Carson, Latimer-Cheung, Chastin, Altenburg and Chinapaw2017)] have similar physical (eg, premature mortality, chronic diseases and all-cause dementia risk) and psychosocial (eg, self-perceived quality of life, well-being and self-efficacy) risk factors to that of physical inactivity (Wilmot et al., Reference Wilmot, Edwardson, Achana, Davies, Gorely, Gray, Khunti, Yates and Biddle2012; Edwards and Loprinzi, Reference Edwards and Loprinzi2016; Falck et al., Reference Falck, Davis and Liu-Ambrose2016; Kim et al., Reference Kim, Im and Choi2016). In fact, SB is now an identifiable risk factor independent of other PA behaviours (Tremblay et al., Reference Tremblay, Aubert, Barnes, Saunders, Carson, Latimer-Cheung, Chastin, Altenburg and Chinapaw2017). Spending on average 80% of their time in a seated posture, and with 67% being sedentary for more than 8.5 h/day (Shaw et al., Reference Shaw, Čukić, Deary, Gale, Chastin, Dall, Skelton and Der2017), older adults are the most sedentary segment of society and seldom engage in moderate-to-vigorous PA (Chastin et al., Reference Chastin, Gardiner, Ashe, Harvey, Leask, Balogun, Helbostad and Skelton2017).
Several social (eg, social awkwardness and peer/family support), behavioural (eg, ageing stereotypes and lack of time), physical (eg, improved balance and flexibility) and environmental (eg, transport and neighbourhood safety) correlates of PA among older adults have been noted in recent formative (van Schijndel-Speet et al., Reference van Schijndel-Speet, Evenhuis, van Wijck, van Empelen and Echteld2014; Banerjee et al., Reference Banerjee, Kin, Strachan, Boyle, Anand and Oremus2015) and qualitative research (Franco et al., Reference Franco, Tong, Howard, Sherrington, Ferreira, Pinto and Ferreira2015; Devereux-Fitzgerald et al., Reference Devereux-Fitzgerald, Powell, Dewhurst and French2016; Phoenix and Tulle, Reference Phoenix and Tulle2017). Such findings are a first step in enabling policymakers and health care professionals to implement effective PA interventions and promote active ageing (Franco et al., Reference Franco, Tong, Howard, Sherrington, Ferreira, Pinto and Ferreira2015). Given the potential benefits associated with PA outlined, such interventions have the potential to reduce, age-related morbidity and declines in activities of daily living, maintain muscle strength and mass, improve quality of life, and thus reduce the primary and total health care costs associated with SB and physical inactivity among this population (Bauman et al., Reference Bauman, Merom, Bull, Buchner and Fiatarone Singh2016).
Prior research notes that interventions aimed at promoting PA participation should adopt an appropriate conceptual health promotion model to prioritise the key assets of the target group (Plotnikoff et al., Reference Plotnikoff, Lubans, Penfold and Courneya2014). The PRECEDE–PROCEED model of health programme design, implementation and evaluation (Green and Kreuter, Reference Green and Kreuter2005) provides the target population with a comprehensive and structured assessment of their own needs and barriers to a healthy lifestyle. The PRECEDE component of the model comprises of, predisposing, enabling and reinforcing factors has previously been used as a formative framework to guide PA intervention content and design (Mackintosh et al., Reference Mackintosh, Knowles, Ridgers and Fairclough2011; Banerjee et al., Reference Banerjee, Kin, Strachan, Boyle, Anand and Oremus2015). This model has also been adopted as a method for the identification of perceived PA barriers and facilitators among older adults (Banerjee et al., Reference Banerjee, Kin, Strachan, Boyle, Anand and Oremus2015; Gagliardi et al., Reference Gagliardi, Faulkner, Ciliska and Hicks2015) and other populations (Mackintosh et al., Reference Mackintosh, Knowles, Ridgers and Fairclough2011; Emdadi et al., Reference Emdadi, Hazavehie, Soltanian, Bashirian and Heidari Moghadam2015; Susan et al., Reference Susan, Mallan, Callaway, Daniels and Nicholson2017).
The purpose of this formative study was to (i) explore current knowledge and attitudes towards PA, as well as the perceived barriers, facilitators and opportunities for PA participation among older adults living in the community who had agreed to take part in an ongoing PA programme; and (ii) use this data to inform the design, delivery and recruitment strategies of an ongoing community PA intervention programme, as well as international PA interventions among this population. Given the purpose and aims outlined, the Evidence Integration Triangle (Glasgow et al., Reference Glasgow, Green, Taylor and Stange2012) was adopted as the overarching theoretical framework. Through the prompt identification of success and failures across individual-focussed and patient–provider interventions, as well as health systems and policy-level change initiatives, the framework allows for the exploration of the three main evidence-based components of intervention program/policy, implementation processes and measures of progress. Hence, this framework enabled a steep learning cycle through an initial 12-week pilot GHGA programme delivered by the Metropolitan Borough Council within the chosen local authority. Results and analysis from this pilot were fed back to Sport England as the funder, as well as deliverers and participants in order to assess, evaluate and promptly inform adapted future iterations of the GHGA programme.
Methods
Participants and procedures
A descriptive formative study was undertaken from March to June 2016. Participants were recruited from one local authority in North West England recognised as having the highest percentage of inactive older adults (80%) compared to the UK national average, and the highest national health costs associated with physical inactivity (Active People Survey, 2014; Sport England’s Local Profile Tool, 2015). The first author facilitated six, mixed-gender focus groups. Representative of the uptake of participants within the target GHGA initiative, a homogenous purposive sample of 28 community dwelling white, British older adults (five male) participated in five of the focus groups, with an additional convenience pragmatic sub-sample of six participants (three male) recruited from an assisted living retirement home, participating in the sixth focus group. In total, 34 older adults (eight male), aged 65–90 years (M=78, SD=7 years), participated across the six sessions. Four focus groups involved a group size of six to ten participants, and two involved three participants (mean focus group size of 6±5 participants). Previous focus groups in PA studies have been conducted effectively with as many as 12 (Moran et al., Reference Moran, MacMillan, Smith-Merry, Kilbreath and Merom2015), and as few as four (Schneider et al., Reference Schneider, Goddard, Davis, Wilfond, Kauffman, Reiss, Gilmore, Himes, Lynch, Leo and McMullen2016) participants. Focus groups took place in two church halls, an assisted living retirement home lounge, and a theatre. All locations were free from background noise, and participants could be overlooked but not overheard. The inclusion criterion set out by Sport England as funders of the GHGA programme were that participants must be 65 years of age or over, reside within one local authority in North West England, could provide written informed consent to participate.
GHGA is an ongoing three-year project which seeks to increase the number of inactive older adults participating in PA at least once a week for 30 min, via a 12-week PA intervention delivered by the Metropolitan Borough Council within the assigned local authority. Participants due to participate in GHGA received a covering letter, participant information sheet, and consent form. Prior to the commencement of the study, institutional ethical approval was received (#SPA-REC-2015-329) and written informed consent was obtained for all participants prior to participation. All focus groups utilised the PRECEDE stage of the PRECEDE–PROCEDE model (Green and Kreuter, Reference Green and Kreuter2005) within their design allowing for the exploration of predisposing, enabling and reinforcing correlates of PA participation. To maximise the interaction between participants, focus group questions were reviewed by the project team for appropriateness of question ordering and flow. Subsequent minor additions were made to questions on social isolation and PA advertisement. The semi-structured discussion guide included open ended questions structured to prompt discussion with equal chance for participants to contribute (Stewart and Shamdasani, Reference Stewart and Shamdasani2014). Focus groups were led by a trained facilitator and with an observer/ note taker also present. Questions addressed knowledge, attitudes and beliefs towards PA as well as views on barriers and opportunities for PA participation. An example question from a section exploring barriers to PA was: ‘Can you tell me about what stops you from participating in physical activity?’ Questions therefore demonstrated aspects of face validity as they were transparent and relevant to both the topic and target population (French et al., Reference French, Olander, Chisholm and McSharry2015).
Data coding and analysis
Focus groups lasted between 20 and 45 min (M=29, SD=12), were audio recorded, and later transcribed verbatim, resulting in 66 pages of raw transcription data with Arial font, size 12 and double-spaced. Verbatim transcripts were read and re-read to allow familiarisation of the data and then imported into the QSR NVivo 11 software package (QSR International Pty Ltd., Doncaster, Victoria, Australia, 2017).
Previous research within this population has adopted analytical procedures including thematic analysis (Van Dyck et al., Reference Van Dyck, Mertens, Cardon, De Cocker and De Bourdeaudhuij2017), content analysis (Middelweerd et al., Reference Middelweerd, Mollee, van der Wal, Brug and te Velde2014) and used specialist qualitative data analysis packages, such as NVivo (Warmoth et al., Reference Warmoth, Lang, Phoenix, Abraham, Andrew, Hubbard and Tarrant2016). In supporting new methodologies and data representation within qualitative research (Orr and Phoenix, Reference Orr and Phoenix2015), the current study followed the pen profiling protocol. The pen profile approach has been used in recent child PA research (Mackintosh et al., Reference Mackintosh, Knowles, Ridgers and Fairclough2011; Boddy et al., Reference Boddy, Knowles, Davies, Warburton, Mackintosh, Houghton and Fairclough2012; Knowles et al., Reference Knowles, Parnell, Stratton and Ridgers2013; Noonan et al., Reference Noonan, Boddy, Fairclough and Knowles2016b) and presents findings from content analysis via a diagram of composite key emerging themes. In summary, data were initially analysed deductively via content analysis (Braun and Clarke, Reference Braun and Clarke2006), using the PRECEDE component of the PRECEDE–PROCEED model (Green and Kreuter, Reference Green and Kreuter2005) as a thematic framework which reflects the underlying study purpose. Inductive analysis then allowed for emerging themes to be created beyond the pre-defined categories. Data were then organised schematically to assist with interpretation of the themes (Aggio et al., Reference Aggio, Fairclough, Knowles and Graves2016). As akin to more traditional qualitative research, verbatim quotations were subsequently used to expand the pen profiles, provide context and verify participant responses. Previous studies have demonstrated this method’s applicability in representing analysis outcomes within PA research (Mackintosh et al., Reference Mackintosh, Knowles, Ridgers and Fairclough2011; Boddy et al., Reference Boddy, Knowles, Davies, Warburton, Mackintosh, Houghton and Fairclough2012; Knowles et al., Reference Knowles, Parnell, Stratton and Ridgers2013; Noonan et al., Reference Noonan, Boddy, Fairclough and Knowles2016a) making it accessible to researchers who have an affinity with both quantitative and qualitative backgrounds (Knowles et al., Reference Knowles, Parnell, Stratton and Ridgers2013; Noonan et al., Reference Noonan, Boddy, Fairclough and Knowles2016a). Recent findings suggest that the discrepancy between objective isolation and felt loneliness may be associated with undesirable health outcomes such as cognitive dysfunction.
Three pen profiles were developed to display themes within the data aligned to the PRECEDE component of the PRECEDE–PROCEED model (Green and Kreuter, Reference Green and Kreuter2005). Quotations were labelled by focus group number (Fn) and subsequent participant number (Pn) within that focus group. Characterising traits of this protocol include details of frequency counts and extracts of verbatim quotes to provide context to the themes. A minimum threshold for theme inclusion was based upon comparable participant numbers within previous research adopting a pen profiling approach (Boddy et al., Reference Boddy, Knowles, Davies, Warburton, Mackintosh, Houghton and Fairclough2012; Noonan et al., Reference Noonan, Boddy, Fairclough and Knowles2016a) and hence, was set as ⩾n=6, with n representing individual mentions per participant. However, multiple ‘mentions’ by the same participant were only counted once. Methodological rigour was demonstrated through a process of triangular consensus (Hawley- Hague et al., Reference Hawley-Hague, Horne, Skelton and Todd2016) between the authors. This offered transparency, credibility and trustworthiness of the results, as the data were critically reviewed using a reverse tracking process from pen profiles to verbatim transcripts, providing alternative interpretations of the data (Smith and Caddick, Reference Smith and Caddick2012). The process was repeated through cross-verification and discussion until subsequent agreement on data themes in relation to verbatim extracts was reached (Aggio et al., Reference Aggio, Fairclough, Knowles and Graves2016).
Findings and discussion
Predisposing correlates
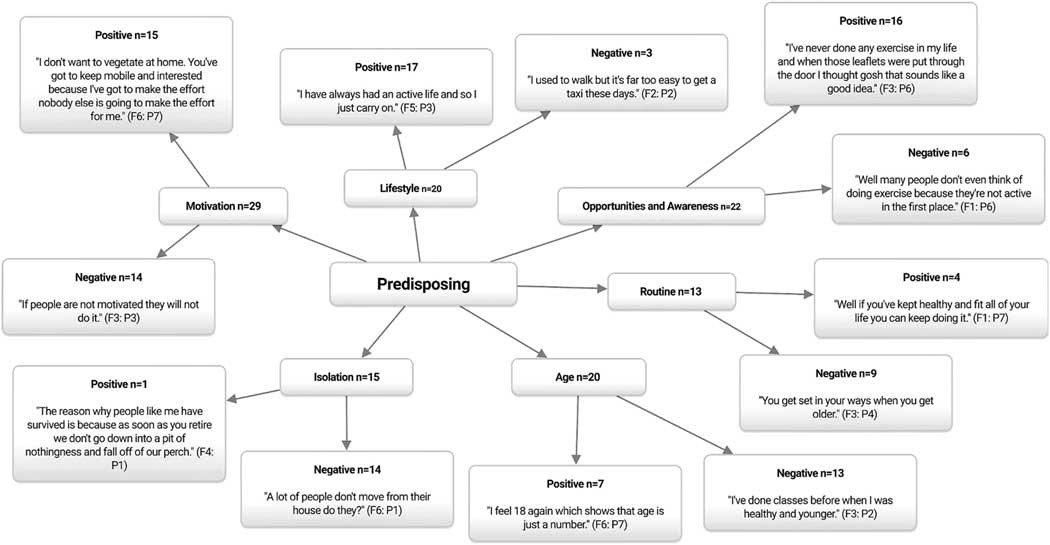
Figure 1 displays the predisposing correlates of PA participation. In agreement with previous research (Gray et al., Reference Gray, Murphy, Gallagher and Simpson2015; Kosteli et al., Reference Kosteli, Williams and Cumming2016), the most highly cited theme of motivation (n=29) was perceived to be both a facilitator (n=15) and barrier (n=14) to PA participation throughout. Some participants were proactive in seeking out opportunities for PA.
I’m a lung cancer survivor and I just ran a mile last month and I raised £550.(Focus group (F) 1: Participant (P) 2)
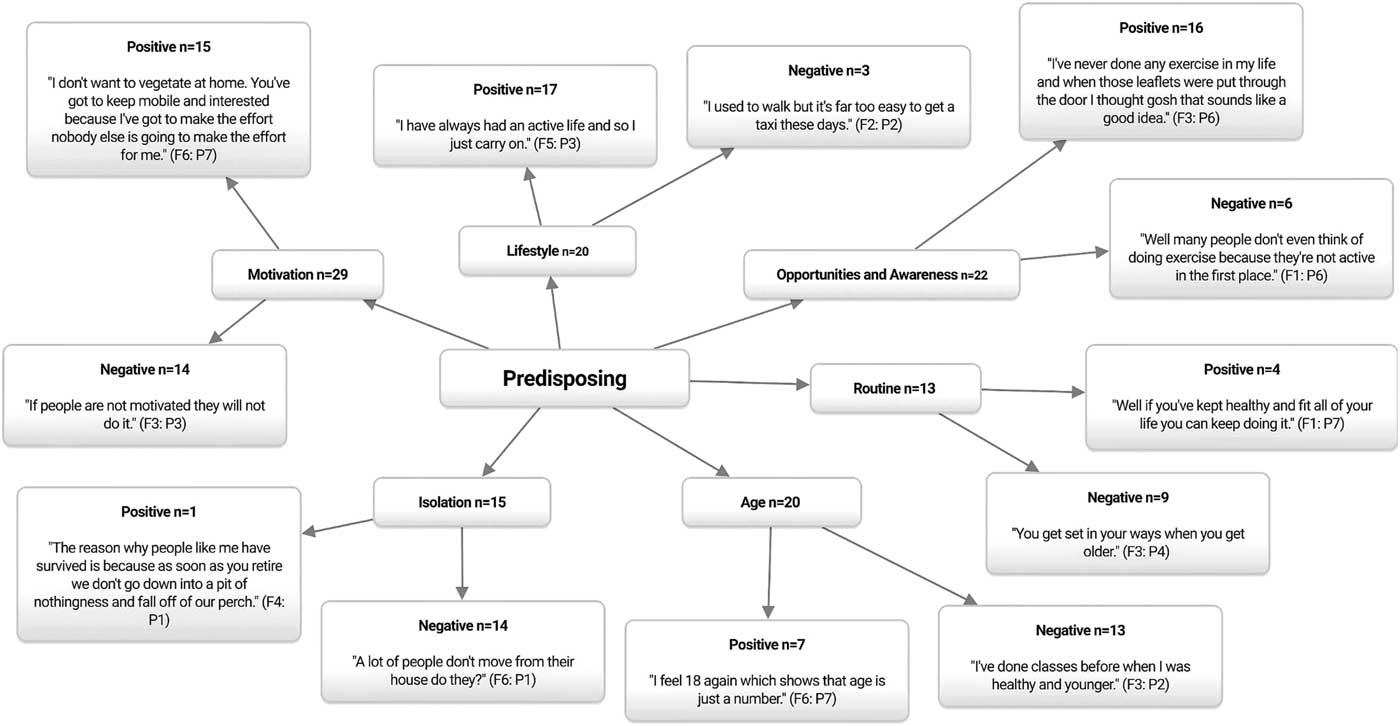
Figure 1 Predisposing correlates of physical activity participation among older adults. n=Individual mentions per person (multiple mentions not included); Fn=focus group number; Pn=participant number.
Contrastingly, others expressed disinterest in PA altogether believing that they would not derive any health benefit.
I’ve pushed these [PA] classes to lots and lots of friends and they still ignore it, they will not come to anything like this. (F1: P3)
Participants also reported laziness or apathy to prevent participation.
It’s [lack of PA] apathy, just apathy, people can’t be bothered. (F4: P3)
The importance of pre-intervention intrinsic motivation (eg, participating for enjoyment) among older adults is key for both initial adoption and maintenance of PA participation (Gray et al., Reference Gray, Murphy, Gallagher and Simpson2015). Hence, future interventions could promote intrinsic motivation for PA through the adoption of socio-emotional selectivity theory (Carstensen et al., Reference Carstensen, Isaacowitz and Charles1999). Recent findings support this theory’s notion that motivation for PA is more effectively promoted when paired with positive messages about the benefits of PA rather than with negative messages about the risks of inactivity (Notthoff et al., Reference Notthoff, Klomp, Doerwald and Scheibe2016).
The theme of age (n=20) was identified as a key barrier (n=13) to PA participation throughout.
They [older adults] get to a certain age and just give up. (F1: P7)
Social norms and cultural misconceptions often influence not only the type of PA in which older adults engage, but whether they participate at all (Greaney et al., Reference Greaney, Lees, Blissmer, Riebe and Clark2016). Moreover, participants noted that lifestyle (n=20) often affects individual views regarding ageing stereotypes, and therefore PA participation. Some participants felt that physically active older adults were more likely to be habituated to PA engagement over many years.
Well if you’ve kept healthy, kept fit all your life, you can keep doing it. (F1: P4)
Conversely, it was felt that inactive older adults were reluctant to start exercising.
You see the ones who haven’t been doing it [PA] are not going to be able to start and do it now. (F2: P1)
Previous research has also reported prior PA behaviours (eg, being sedentary or active) to be key correlates affecting older adults’ current PA participation levels (Franco et al., Reference Franco, Tong, Howard, Sherrington, Ferreira, Pinto and Ferreira2015). Additionally, ageing is associated with a decrease in the size of social networks and hence, older adults are at increased risks of isolation (Devereux-Fitzgerald et al., Reference Devereux-Fitzgerald, Powell, Dewhurst and French2016; Greaney et al., Reference Greaney, Lees, Blissmer, Riebe and Clark2016). Corroborating with prior research (Greaney et al., Reference Greaney, Lees, Blissmer, Riebe and Clark2016), participants throughout perceived isolation (n=15) to be a key barrier (n=14) to PA participation.
It’s so easy to get trapped inside and not go out. People sit in front of the television from the moment they wake up to when they go to bed. (F6: P5)
Isolation is associated with decreased social and psychological well-being (Owen et al., Reference Owen, Healy, Matthews and Dunstan2010; Milligan et al., Reference Milligan, Payne, Bingley and Cockshott2015) and increased SB among older adults (Nicholson, Reference Nicholson2012). Certain targeted intervention strategies can reduce isolation by providing an opportunity for older adults from differing socio-economic areas to take part in PA within local community spaces (eg, parks, leisure centres and churches), that promote social networking by encouraging camaraderie, adaptability and productive engagement, without the pressure to perform (Milligan et al., Reference Milligan, Payne, Bingley and Cockshott2015; Gardiner et al., Reference Gardiner, Geldenhuys and Gott2016). Given that SB is an independent and modifiable behavioural target for interventions (Lewis et al., Reference Lewis, Napolitano, Buman, Williams and Nigg2017), opportunities to replace SB with health-enhancing behaviours such as moderate-to-vigorous PA (Prince et al., Reference Prince, Saunders, Gresty and Reid2014), light PA (McMahon et al., Reference McMahon, Lewis, Oakes, Wyman, Guan and Rothman2017; Phoenix and Tulle, Reference Phoenix and Tulle2017) and standing (Healy et al., Reference Healy, Winkler, Owen, Anuradha and Dunstan2015) should be promoted. However, none of the participants in the current study noted negative health effects of prolonged sitting, or the importance of breaks in sedentary time. Previous research has noted that older adults are not yet familiar with the concept of SB and hence, are not motivated to reduce such behaviours (Van Dyck et al., Reference Van Dyck, Mertens, Cardon, De Cocker and De Bourdeaudhuij2017). Hence, it is first crucial to increase knowledge about the negative health consequences of SB independent from PA among both older adults and other populations (Van Dyck et al., Reference Van Dyck, Mertens, Cardon, De Cocker and De Bourdeaudhuij2017).
Participants also emphasised the importance of having a wide range of choice and opportunities for PA (n=22), and in general their perceptions of community provision were positive (n=16).
Yes it’s quite a good place [the local authority where the study took place]. There are a lot of different physical activity sessions to try. (F2: P1)
However, in line with recent research (Baert et al., Reference Baert, Gorus, Calleeuw, De Backer and Bautmans2016; Träff et al., Reference Träff, Cedersund and Nord2017), key barriers noted by the participants within the assisted living group included a lack of advertisement regarding PA opportunities, and few opportunities to take part in PA within the assisted living facility itself.
It’s hard to know what is on if you don’t read the noticeboards and to be honest most of us have even stopped looking at that [noticeboard] because there is never anything on it. (F3: P3)
Further research into the most effective advertisement strategies to engage older adults in assisted living facilities is warranted (Hildebrand and Neufeld, Reference Hildebrand and Neufeld2009). Regardless of living status, participants noted a strong preference not to engage with online and/or social media channels for advertising and awareness-raising.
A lot of people our age don’t like that technology stuff at all. I would not know where to start. (F5: P2)
These results suggest educational strategies outlining the potential benefits of technology in aiding PA participation are needed (Bird et al., Reference Bird, Clark, Millar, Whetton and Smith2015). This is especially salient given that recent research has shown technology-based interventions to have good adherence and provide a sustainable means of reducing SB and promoting PA participation among older adults (Garcia et al., Reference Garcia, Schoene, Lord, Delbaere, Valenzuela and Navarro2016; Skjæret et al., Reference Skjæret, Nawaz, Morat, Schoene, Helbostad and Vereijken2016).
Enabling correlates
Figure 2 displays the enabling correlates of PA participation. Consistent with previous research findings (Franco et al., Reference Franco, Tong, Howard, Sherrington, Ferreira, Pinto and Ferreira2015; Borodulin et al., Reference Borodulin, Sipilä, Rahkonen, Leino-Arjas, Kestilä, Jousilahti and Prättälä2016), cost (n=21) was perceived to be a key barrier (n=12) to PA participation exclusively among the community dwelling participants who were either unable, or unwilling to pay the perceived high costs associated with both attending and travelling to such programmes.
Money is the big bug bear [barrier to PA participation] isn’t it. (F2: P5)
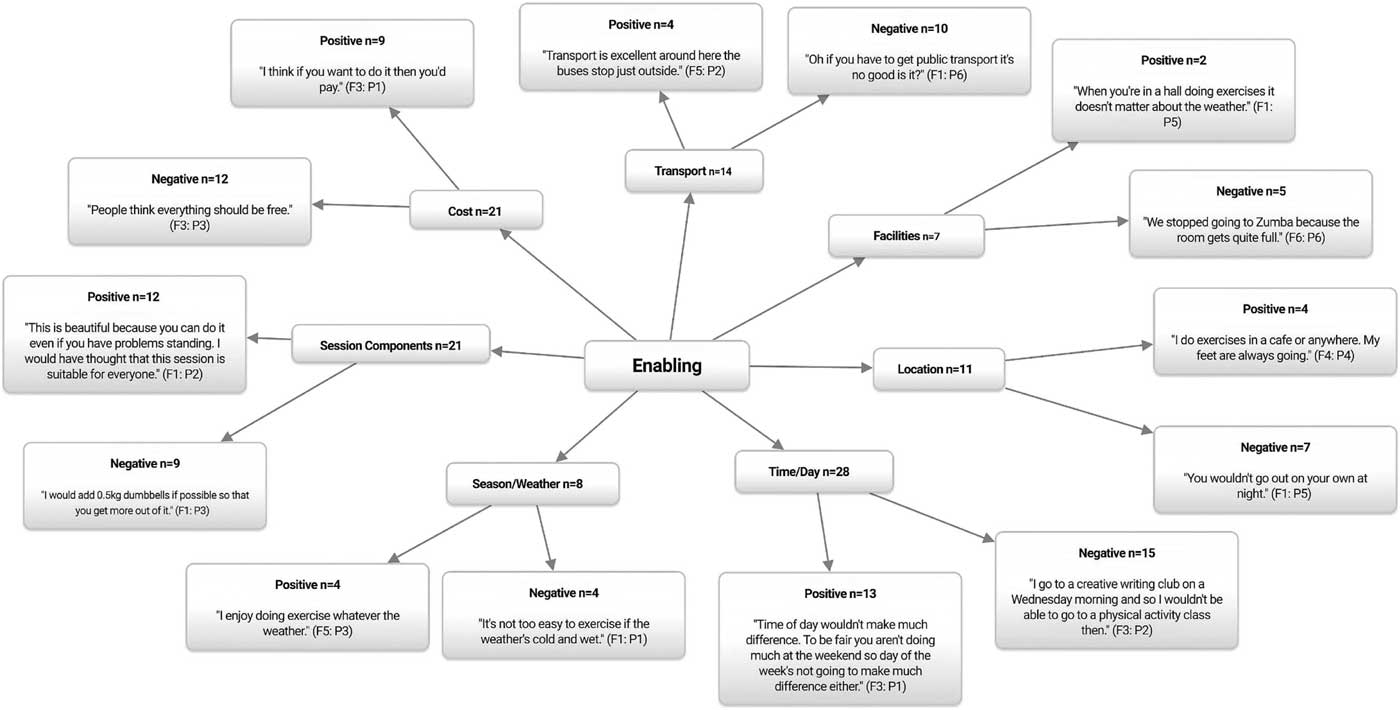
Figure 2 Enabling correlates of physical activity participation among older adults. n=Individual mentions per person (multiple mentions not included); Fn=focus group number; Pn=participant number.
Examples of competing programmes were also noted, with free and lower cost programmes taking precedence over the more expensive.
We like it [a local chair-based PA programme] because it’s free. (F4: P3)
Thus, to effectively increase PA participation within this population, health-promotion strategies should go further than merely educating and raising awareness about potential health benefits, and should also advocate for the provision of low-cost, and easy reachable PA opportunities regardless of financial status (Petrescu-Prahova et al., Reference Petrescu-Prahova, Belza, Kohn and Miyawaki2015; Borodulin et al., Reference Borodulin, Sipilä, Rahkonen, Leino-Arjas, Kestilä, Jousilahti and Prättälä2016). It is worth noting that for the participants recruited from the assisted living retirement home, any PA sessions delivered were included within the cost of the overall living fee, and hence lack of financial resources was rejected as a potential barrier for PA participation (Baert et al., Reference Baert, Gorus, Calleeuw, De Backer and Bautmans2016).
Participants’ views on the theme of location (n=11) centred on neighbourhood safety. Declining health and physical impairments associated with ageing increase the time spent in ones’ neighbourhood and thus, neighbourhood environmental factors such as, PA provision, proximity, traffic volume and overall neighbourhood safety are considered to be important correlates affecting older adults’ PA participation (Greaney et al., Reference Greaney, Lees, Blissmer, Riebe and Clark2016). Perceived neighbourhood safety was identified as a barrier (n=7) to PA participation exclusively among the community dwelling older adults.
You wouldn’t go out on your own at night around here. (F1: P5)
Participants from the assisted living retirement home did not view neighbourhood safety to be either a barrier to or facilitator of PA. This neighbourhood environment was perhaps viewed as the norm and therefore they did not associate safety concerns so acutely (Moran et al., Reference Moran, MacMillan, Smith-Merry, Kilbreath and Merom2015). This association could have also affected results obtained for the theme time/day of the week as such participants did not recognise this to be a barrier to PA participation either.
Time of day wouldn’t make much difference [to PA participation]. To be fair you aren’t doing much at the weekend so day of the week isn’t going to make much difference [to PA participation] either. (F3: P1)
Conversely, community dwelling participants reported time/day of the week to be a barrier (n=15), with early morning or early evening sessions identified as reducing PA participation, especially during the winter months when daylight hours are more limited. These findings could have been further amplified by the neighbourhood safety concerns also identified by this group (Hoppmann et al., Reference Hoppmann, Lee, Ziegelmann, Graf, Khan and Ashe2015; Prins and van Lenthe, Reference Prins and van Lenthe2015).
The theme of transportation (n=14) has been extensively reported to be both a barrier and facilitator to PA participation among older adults (Bouma et al., Reference Bouma, van Wilgen and Dijkstra2015; Haselwandter et al., Reference Haselwandter, Corcoran, Folta, Hyatt, Fenton and Nelson2015; Kosteli et al., Reference Kosteli, Williams and Cumming2016; Van Dyck et al., Reference Van Dyck, Mertens, Cardon, De Cocker and De Bourdeaudhuij2017). Within the current study transportation was identified as a barrier (n=10) restricting access to PA sessions regardless of living status.
I would like to go to the baths [swimming pool] but it’s difficult to get there and back so I just don’t bother. (F4: P5)
Transport is especially important for those lacking the ability to be more independently mobile as it allows individuals to bridge larger distances than they could by walking alone (Van Cauwenberg et al., Reference Van Cauwenberg, De Bourdeaudhuij, Clarys, Nasar, Salmon, Goubert and Deforche2016). Thus, lack of access to a car and inadequate availability, frequency and reliability of affordable public transport are all associated with decreased PA participation (Newitt et al., Reference Newitt, Barnett and Crowe2016). Additionally, being dependent upon others (eg, family, friends and peers) for transportation has been identified as a barrier to PA participation within this population (Baert et al., Reference Baert, Gorus, Mets and Bautmans2015). This was also noted in the current study.
I think the worst thing is having to rely on somebody else to take you [to a PA session] as anything can happen in your own life let alone somebody else’s. (F5: P2)
Prior research suggests the promotion of walking for transportation to PA sessions among physically independent older adults (Chudyk et al., Reference Chudyk, McKay, Winters, Sims-Gould and Ashe2017). However, given the neighbourhood safety concerns noted by participants, and the varying levels of functional ability among this population, further research examining access to PA sessions including walking facilities (eg, path and crossing quality), traffic safety and safety from crime is warranted (Van Cauwenberg et al., Reference Van Cauwenberg, De Bourdeaudhuij, Clarys, Nasar, Salmon, Goubert and Deforche2016).
Reinforcing correlates
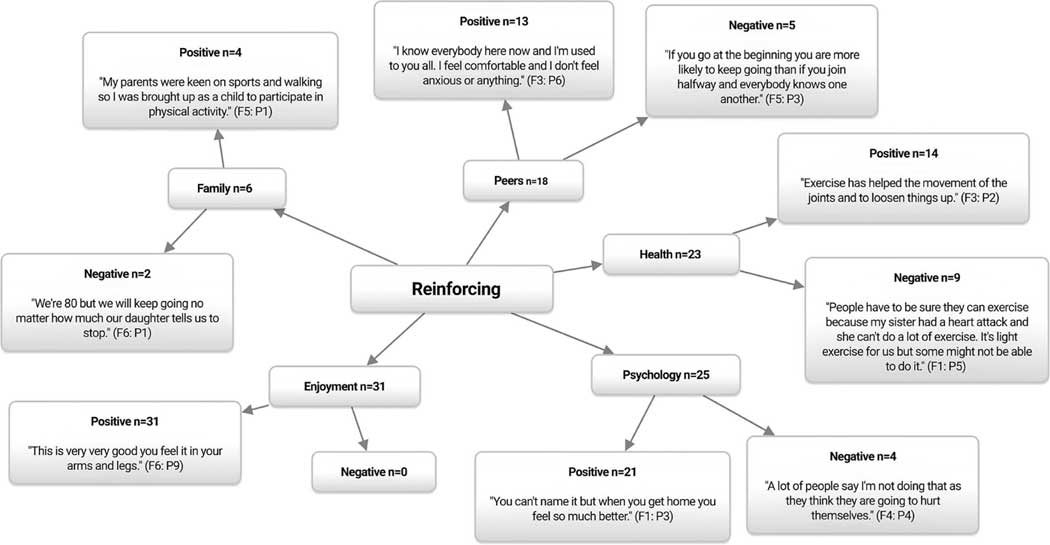
Figure 3 displays the reinforcing correlates of PA participation. Peer support is associated with PA adherence in older adults (Brown et al., Reference Brown, Spanjers, Atherton, Lowe, Stonehewer, Bridle, Sheehan and Lamb2015), and was identified as a key theme (n=18) and subsequent facilitator (n=13) to PA participation in the current study.
I’ve got to know everybody now and I’m used to you all. I feel more comfortable and I don’t feel anxious or anything. (F3: P6)
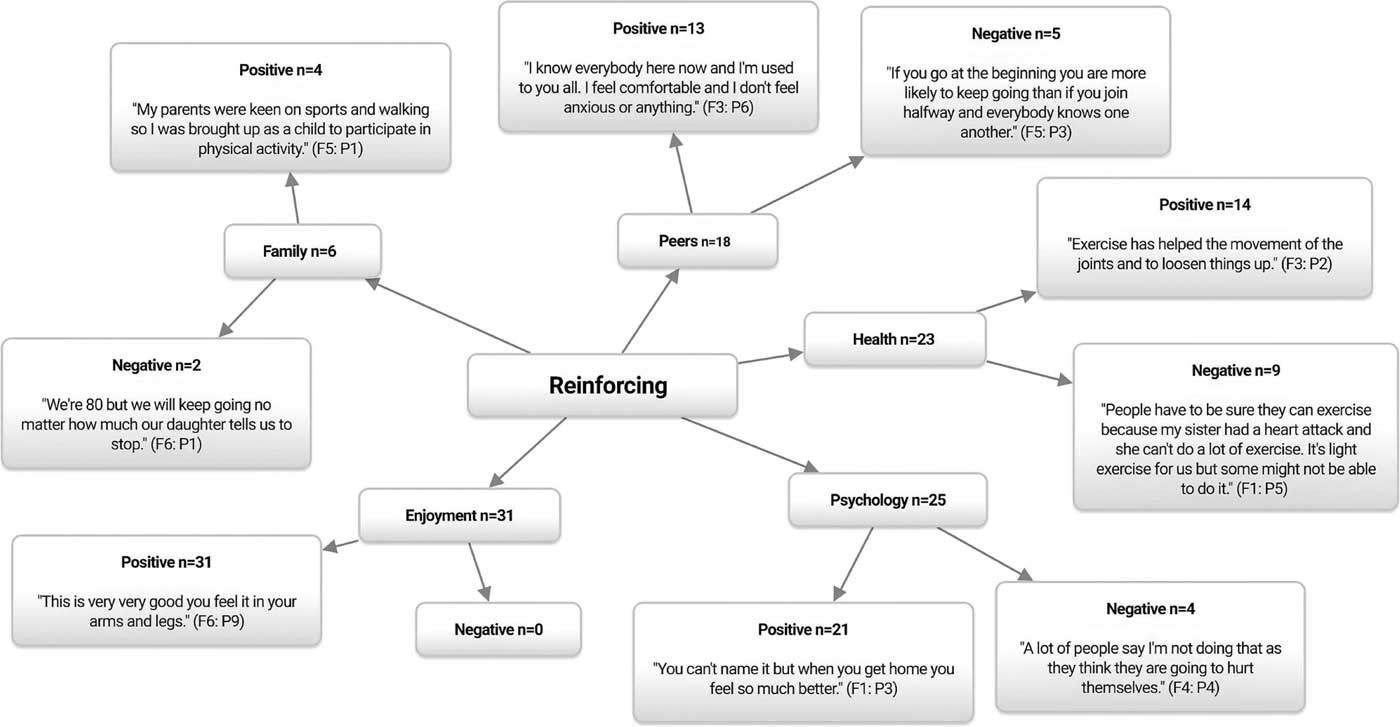
Figure 3 Reinforcing correlates of physical activity participation among older adults. n=Individual mentions per person (multiple mentions not included); Fn=focus group number; Pn=participant number.
Unsurprisingly, in light of the above several participants reported peers to be a barrier to PA participation (n=5) because of an unwillingness to attend other PA sessions due to anxieties about meeting new people.
I wouldn’t like to go somewhere else as I wouldn’t like to walk in on a crowd of new people. (F3: P6)
Although group-based activities offer older adults the chance to gain a sense of belonging, enjoyment and establish friendships, designing sustainable exit routes in order to retain the provision of group activities which continue to facilitate, build and retain social bonds post-intervention should be considered by PA programmers and policymakers (Wu et al., Reference Wu, Barnes, Ackerman, Lee, Chesney and Mehling2015).
In line with recent research (Devereux-Fitzgerald et al., Reference Devereux-Fitzgerald, Powell, Dewhurst and French2016; Smith et al., Reference Smith, Banting, Eime, O’Sullivan and van Uffelen2017), family members were identified as being both barriers (n=2) and facilitators (n=4) to PA participation. Specifically, a barrier often reported is overprotectiveness, in which family members may not allow older adults to participate in PA out of concern for their safety or health (Greaney et al., Reference Greaney, Lees, Blissmer, Riebe and Clark2016). Participants among the community dwelling groups also noted this.
My sons in for a shock that we’re coming to this as he’s like, ‘no long walks, no boat rides’, he goes ‘you’re past it’. (F6: P2)
Such results suggest a need to educate family members on the importance and benefits of PA among older adults. Educational resources such as the older adults PA guidelines infographics for the, United Kingdom (Reid and Foster, Reference Reid and Foster2016), Canada (Canadian Society for Exercise Physiology, 2016), Australia (Australian Government Department of Health and Ageing, 2013), New Zealand (Ministry of Health, 2013) and the United States (CDC, 2008) are appropriate tools advocating for older adults to be active safely, and can be understood by family members plus health care providers. Furthermore, the adoption of local/national mass media messages may be a cost effective educational solution at a time when there is a growing ageing population (United Nations, 2015; UK Office for National Statistics, 2017). However, given the resistance to technology-based PA noted in the current study, further educational strategies promoting enjoyable, easy-to-use technology within a family environment are needed for community dwelling older adults (Bird et al., Reference Bird, Clark, Millar, Whetton and Smith2015). Participants within the assisted living group did not perceive family members to be either barriers or facilitators to PA participation and thus, further research is needed to identify approaches to involve family members as additional facilitators of PA participation within this group.
Participants viewed the theme of perceived health benefits (n=23) to be both a facilitator (n=14) and barrier (n=9) to PA participation regardless of living status. Participants were knowledgeable regarding the potential benefits of PA for their physical health.
It [PA] loosens all your limbs up. (F2: P2)
Participants also noted the potential benefits of PA for their psychological health.
The wellbeing [from PA participation] makes you feel better. (F1: P3)
Despite the irrefutable evidence demonstrating the benefits of PA among older adults (CDC, 2015; Reid and Foster, Reference Reid and Foster2016; WHO, 2017), participants also noted health to be a potential barrier (n=14) to PA participation due to doubts about their capabilities, or fear of causing themselves harm, particularly if they were unfamiliar with it.
People have to be sure they can come to PA sessions because my sister had a heart attack … and she can’t do a lot of these exercises. (F1: P5)
To overcome such perceptions, educational strategies at a population level should focus on communicating the role of PA in gaining health benefits for all as well as how well-designed PA programmes can aid in the management of common comorbidities specific to this age group (Gillespie et al., Reference Gillespie, Robertson, Gillespie, Sherrington, Gates, Clemson and Lamb2012; Hamer et al., Reference Hamer, Lavoie and Bacon2013).
Taken together with the findings of recent qualitative studies examining correlates of PA participation among older adults living in both assisted living (Baert et al., Reference Baert, Gorus, Calleeuw, De Backer and Bautmans2016; Träff et al., Reference Träff, Cedersund and Nord2017) and community dwelling older adults (Fisher et al., Reference Fisher, Harrison, Bruner, Lawson, Reeder, Ashworth, Sheppard and Chad2017; Phoenix and Tulle, Reference Phoenix and Tulle2017), results from this formative research study have been used to inform the design, delivery and recruitment strategies of an ongoing community PA intervention project. Specifically, changes implemented to programme design have included the introduction of, increased intervention duration from 6 to 12-weeks, maintenance sessions post-initial 12-week intervention, tea and coffee after each session to promote social interaction, and a reduction of early morning and late afternoon sessions. Changes to programme delivery have included the introduction of, participant choice in session activities, videoing participants at week 1 and week 12 to show participants their progression, and signposting participants to other local PA programmes. Finally, changes implemented to recruitment strategies have included, improved relationships with general practitioners to enable them to refer participants onto the programme, leafleting in church halls and charity shops, and deliverers attending and subsequently advertising the programme at several Older Peoples’ Forums. Such methods could also be adopted throughout similar community PA programmes elsewhere in order to increase programme fidelity, representativeness and effectiveness.
Strengths and limitations
Methodological strengths include the exploration of consensus and associated discussion through the focus groups and subsequent analysis process which allowed insight into the predisposing, enabling and reinforcing correlates of PA participation among older adults. Consistency of themes, data credibility, transferability, and dependability were achieved through the triangulation consensus of data between authors and methods. While this study reiterates important insights into the perceived barriers, facilitators and opportunities for PA participation among both community dwelling and assisted living older adults, value outside of this to the wider research community may be limited due to programme funding which only allowed for formative research strategies to recruit participants who had agreed to take part in an ongoing PA programme. Consequently, sampling bias is a potential issue as it could be assumed that a high proportion of the participants were already inclined to be and/or currently physically active given the positive predisposing comments with regard to motivation towards PA and current lifestyle choices (Costello et al., Reference Costello, Kafchinski, Vrazel and Sullivan2011). This is especially important given that motivators and barriers towards regular PA vary among currently active and inactive adults across the age range (Costello et al., Reference Costello, Kafchinski, Vrazel and Sullivan2011; Hoare et al., Reference Hoare, Stavreski, Jennings and Kingwell2017). Considering that less than 10% of older adults (⩾ 65 years of age) meet the recommended PA guidelines (Jefferis et al., Reference Jefferis, Sartini, Lee, Choi, Amuzu, Gutierrez, Casas, Ash, Lennnon, Wannamethee and Whincup2014), future research should seek to identify barriers and facilitators among larger sample sizes of currently inactive older adults living within both the community and assisted living facilities.
Additionally, a small convenience pragmatic sub-sample of participants from one assisted living facility were recruited and hence results cannot be considered representative. Furthermore, men tend to decrease participation in leisure-time PA as they get older; whereas this dose-response is not seen among women (Amagasa et al., Reference Amagasa, Fukushima, Kikuchi, Takamiya, Oka and Inoue2017). Consequently, there is the possibility of gender bias given the higher number of female participants recruited. However, the sample size, participants’ ages and gender distribution are comparable to those reported in two recent studies examining barriers and facilitators to PA participation among older adults (Baert et al., Reference Baert, Gorus, Mets and Bautmans2015; Moran et al., Reference Moran, MacMillan, Smith-Merry, Kilbreath and Merom2015). Within these two studies the total number of participants was 15 (five male) and 40 (13 male), and the mean age of the respondents was 74 years, and 84 years, respectively. This compares to a total number of 34 participants (eight male) with a mean age of 78 years in the current study. Nevertheless, as well as exploring correlates of PA participation in relation to gender, functional status and age differences between the young–old (60–69 years), old–old (70–79 years) and oldest–old (80+ years) (Heo et al., Reference Heo, Chun, Kim, Ryu and Lee2017), future research should obtain additional participant characteristic data prior to the intervention including, participants’ current sedentary time and PA levels, history of PA, family history of PA, ethnicity, employment status and educational achievements as such have been shown to potentially affect the perceived barriers and facilitators to PA participation among older adults (Greaney et al., Reference Greaney, Lees, Blissmer, Riebe and Clark2016; Keadle et al., Reference Keadle, McKinnon, Graubard and Troiano2016).
Conclusions
Older adults acknowledged the benefits of PA, not only for health but also those relating to socialising, enjoyment, relaxation, and physical and psychological well-being. The themes of opportunities and awareness for PA participation, cost, transport, location and season/weather varied dependent upon living status. These findings suggest current living status to be a separate correlate of PA participation among older adults. This data can be used to further strengthen the design, delivery and recruitment strategies of both the target GHGA PA intervention programme and international PA intervention programmes among older adults. Future interventions should consider educational strategies to communicate the role of PA in gaining health benefits for all, reducing SB, and countering the negative implicit attitudes that may undermine PA within this population. Given the small sample of participants in the current study, further comparative research exploring the barriers and facilitators between assisted living and community dwelling, and active and inactive older adults on both national and international levels is warranted.
Acknowledgements
The authors express their deepest gratitude to all the participants involved. Edge Hill University institutional ethical approval number: # SPA-REC-2015-329.
Conflicts of Interest
No potential conflict of interest was reported by the authors.