Introduction
The rapid growth of the oldest segment of the world population (‘the oldest-old’, age 80/85+) will result in rising numbers of oldest-old people with dementia in need of care, as well as rising numbers of oldest-old people (most often spouses) providing this care (Carers Trust, 2015; Alzheimer's Association, 2017). As oldest-old individuals, these care-givers have a high likelihood of experiencing ageing-related changes (e.g. frailty, multi-morbidities) (Hudson and Goodwin, Reference Hudson and Goodwin2013) that result in unique care-giving challenges and support needs. However, data on these unique age-related challenges and needs, and how care-givers manage them, is scant, meaning that evidence-based support may not be sensitive to their unique issues.
To better understand this subgroup, we conducted a narrative gerontology study exploring oldest-old care-givers' age and ageing-related experiences. In our first analysis (reported in Arbel et al., Reference Arbel, Cameron, Trentham and Dawson2023), we explored care-givers' perceptions of how age and ageing shape their care-giving experiences. Our findings suggested that oldest-old care-givers experience challenges providing care because of physical, cognitive or sensory decline; having fewer friends who can provide practical support; having less energy for non-care-giving activities (e.g. leisure activities, self-care), and experiences of ageism in the health-care system. Our second analysis (the focus of this paper) focused on how oldest-old care-givers manage these age and ageing-related care-giving challenges.
Literature review
While much has been written in the care-giving literature about how care-givers manage care-giving, most of this literature is not specific to oldest-old care-givers. Age-group specificity is an important consideration, as research suggests that patterns of coping and adaptation evolve and change throughout the lifecourse, and as people age. Reasons for these changes include: (a) developmental changes (e.g. maturation in coping behaviours or loss or adaptive capacities; Folkman et al., Reference Folkman, Lazarus, Pimley and Novacek1987); (b) life experiences (e.g. success in coping with past adversities can be interpreted as evidence of competence in mastering current adversities; Pearlin and Skaff, Reference Pearlin and Skaff1996); (c) changes in the nature and quality of stressors (e.g. reduction in stressors related to work and increase in stressors related to illness; Pearlin and Skaff, Reference Pearlin and Skaff1996); (d) changes in resources (e.g. age-related decrease in social resources; Lang et al., Reference Lang, Rohr, Williger, Fingerman, Berg, Antonucci and Smith2011); and (e) changes in success criteria (in younger ages success in life often refers to family, work or work–life balance while later adulthood is more often directed toward issues of autonomy, everyday competence and wellbeing; Lang et al., Reference Lang, Rohr, Williger, Fingerman, Berg, Antonucci and Smith2011). These changes, along with cohort differences (e.g. in dealing with difficulties; Folkman et al., Reference Folkman, Lazarus, Pimley and Novacek1987; Pearlin and Skaff, Reference Pearlin and Skaff1996), may result in differences in how younger-old and oldest-old people manage care-giving challenges. Because of these differences, research findings regarding coping or adaptation in younger-old care-givers may not be applicable to oldest-old care-givers.
Few studies describe management strategies used specifically by oldest-old spousal care-givers of people with dementia. These studies describe a wide array of strategies used by care-givers including: changing perceptions of their partner, in relation to the disease and keeping a sense of humour (Harris et al., Reference Harris, Adams, Zubatsky and White2011); living ‘one day at a time’, staying connected to the outside world to take their minds off things in the house (Black et al., Reference Black, Schwartz, Caruso and Hannum2008; Hammond-Collins et al., Reference Hammond-Collins, Peacock and Forbes2014); religious beliefs and practices (Black et al., Reference Black, Schwartz, Caruso and Hannum2008; Harris et al., Reference Harris, Adams, Zubatsky and White2011; Sodowsky, Reference Sodowsky2012); receiving social support from neighbours, caretakers, and people at support groups and conferences (Daniels et al., Reference Daniels, Lamson and Hodgson2007); and receiving formal supports and services (Black et al., Reference Black, Schwartz, Caruso and Hannum2008; Egset and Myklebust, Reference Egset and Myklebust2011; Sodowsky, Reference Sodowsky2012).
While this research is illuminating, it does not offer insight into how care-givers manage the specific age and ageing-related challenges often experienced by oldest-old care-givers. A better understanding of how oldest-old care-givers manage ageing-related care-giving challenges will enhance our understanding of this unique group of care-givers and ultimately help guide the development of social and health-care services that are age-sensitive and support care-givers as they age. Thus, the purpose of this study was to explore how oldest-old spousal care-givers of people with dementia manage ageing-related care-giving challenges. The objectives were: (a) to explore the strategies used by care-givers to manage ageing-related care-giving challenges, and (b) to explore facilitators and barriers to strategy use (i.e. internal or external conditions or resources that care-givers perceive as hindering or supporting their ability or willingness to use different strategies).
Theoretical framework
Two theories informed our conceptualisation of management strategies. The first was the selective optimisation with compensation (SOC) model (Baltes and Carstensen, Reference Baltes and Carstensen1996), developed in the field of gerontological research. The model specifies three processes – selection, optimisation and compensation – that together embrace a multitude of psychological mechanisms and behavioural strategies that enable people to attain their goals and adaptively respond to everyday demands, despite experiencing increasing ageing-related vulnerabilities and losses (e.g. sensory, cognitive or interpersonal; Baltes and Carstensen, Reference Baltes and Carstensen1996; Lang et al., Reference Lang, Rieckmann and Baltes2002) (for description, see Table 1).
Table 1. Theoretical constructs description

Notes: SOC: selective optimisation with compensation model (Baltes and Carstensen, Reference Baltes and Carstensen1996). Stress-coping theory: transactional theory of stress and coping (Lazarus and Folkman, Reference Lazarus and Folkman1984).
The SOC model has rarely been used in care-giving research. We chose to incorporate it in our theoretical framework because it provides an ageing perspective to strategy use, which is congruent with our research purpose. Baltes and Carstensen (Reference Baltes and Carstensen1996), in describing the model, do not provide a definition for the term strategy. As this term is used in research in a variety of ways, for the purposes of this study, we define SOC-related strategies as goal-directed behaviours used to accomplish a task, to achieve a purpose or to enhance success in an activity (Toglia et al., Reference Toglia, Rodger and Polatajko2012). This definition is congruent with the SOC model's emphasis on the role of strategies to master goals and optimise functioning, in the presence of age-related decline (Baltes and Carstensen, Reference Baltes and Carstensen1996).
The second theory that informed our conceptualisation of management strategies was the transactional theory of stress and coping (Lazarus and Folkman, Reference Lazarus and Folkman1984) (hereafter stress-coping theory). Coping strategies refer to the specific efforts, both behavioural and cognitive, that people use to master, tolerate, reduce or minimise stressful events (Monteiro et al., Reference Monteiro, Santos, Kimura, Baptista and Dourado2018). Coping strategies within this framework have been traditionally conceptualised into two major categories: emotion-focused strategies and problem-focused strategies (for description, see Table 1). Care-giver coping has been identified as central to understanding care-giving outcomes and has received a lot of attention in the care-giving literature (Hawken et al., Reference Hawken, Turner-Cobb and Barnett2018).
Methods
Approach
This study utilised a narrative gerontology approach (Kenyon et al., Reference Kenyon, Clark and De Vries2001; de Medeiros, Reference de Medeiros2014) which examines ageing as it is experienced and expressed in the stories of older persons (Kenyon et al., Reference Kenyon, Clark and De Vries2001). The narrative gerontology approach recognises that people create their personal stories and make sense of their lives within broader narrative structures and social contexts. People's lifestories are shaped by four interrelated dimensions: the personal or intrapersonal dimensions which involves the creation and discovery of meaning within each of us uniquely; the interpersonal dimension which refers to how our lifestories are shaped by and entwined with lifestories of other individuals (e.g. family, friends, intimate partners); the socio-cultural dimension which refers to social meanings that are associated with ageing and the lifecourse within a given cultural context; and the structural dimension that encompasses social policies, power relations and economic realities that pertain to a given society (Kenyon et al., Reference Kenyon, Clark and De Vries2001).
Design
This study utilised a multiple, semi-structured interview design. We chose a conversational interview style over other methods of narrative data collection (e.g. unguided life histories, diaries and journals), so as to evoke thinking about the phenomenon from different perspectives (stemming from previous research, our theoretical framework and previous interviews in this study), to deepen care-givers' reflections (with probes) as the conversation proceeded and to elicit reflections that may go beyond initial awareness (Polkinghorne, Reference Polkinghorne2007).
Multiple interview sessions help elicit deeper insight into participants' experiences by supporting the development of rapport between the interviewer and the participants, and by enabling the interviewer and participant to reflect between interviews, and revisit important issues in following sessions (de Medeiros, Reference de Medeiros2016).
Participants
This study included oldest-old spousal care-givers of people with dementia, which we defined as people who provide care and assistance (at home or in an institution) to partners who need support due to debilitating physical, mental or cognitive dementia symptoms (Canadian Caregiver Coalition, 2013). Care-givers in the Greater Toronto and Hamilton areas were recruited via convenience sampling, including grassroots recruiting methods (e.g. word-of-mouth referrals, flyers) and key agency contacts at local community agencies (e.g. the Alzheimer's Association). Interested care-givers contacted the research lab by phone, and underwent a phone screen to determine eligibility. Care-givers were included if they were age 80+, and self-identified as actively involved in care-giving for a spouse with dementia, on a daily or weekly basis, for any duration, and in any care setting (e.g. home, retirement home, long-term care facility (LTC)). Care-givers were excluded if their partner's dementia was a result of stroke, traumatic brain injury or multiple sclerosis, or if they provided care less than once per week. Participants were recruited from October 2019 to January 2020 concurrently with data collection and analysis until meaning saturation was achieved (i.e. a comprehensive understanding of the issues was reached and further interviews were not anticipated to provide new insights; Hennink et al., Reference Hennink, Kaiser and Marconi2017).
Context
As the sample includes only care-givers from two metropolitan areas in Ontario, Canada, narratives described below must be read as contextually limited to this region and the aforementioned time period. Canada has a universal health-care system (Medicare) meaning that core medical and hospital services are taxation-based and publicly funded. However, administration and service delivery are highly decentralised, and supports available differ between provinces and districts (Martin et al., Reference Martin, Miller, Quesnel-Vallée, Caron, Vissandjée and Marchildon2018). In Ontario, people with dementia may be eligible for services such as a personal support worker several hours per week, home-making support, nursing care and/or adult day programmes (Ministry of Health, 2022). The eligibility and level of care is determined and monitored by a case manager and is tailored to the condition of the spouse with dementia and not the care-giver (National Institute on Ageing, 2020). In addition to government support, charitable organisations offer funded supports for people with dementia (e.g. friendly visiting) and for care-givers (e.g. care-giving support groups). Privately funded services (out-of-pocket) are also available from for-profit or not-for-profit companies such as organisations that offer supplemental home support.
Despite the availability of publicly and privately funded services for care-givers in Canada (and especially in urban areas), studies show that Canadian care-givers often do not access supports because of a general lack of awareness of available supports and how to access them. Further, criteria for access to publicly funded services have been viewed as overly restrictive (National Institute on Ageing, 2020) and inability to pay for home and community support services has been identified as a major access barrier for Canadians aged 65 years and older (Martin et al., Reference Martin, Miller, Quesnel-Vallée, Caron, Vissandjée and Marchildon2018).
Data collection
Data were collected through two to three in-depth, one-on-one, semi-structured interviews per care-giver, of approximately 90–120 minutes. Interviews were conducted in care-givers' preferred location (home or research institute). Background information on care-givers and care receivers was collected via a demographic questionnaire. Care-givers rated their spouse's competence in basic activities of daily living with the Physical Self-maintenance Scale and competence in instrumental activities of daily living with the Instrumental Activities of Daily Living Scale (Lawton and Brody, Reference Lawton and Brody1969). Scores on the Physical Self-maintenance Scale range from 0 (low function, dependent) to 6 (high function, independent). Scores on the Instrumental Activities of Daily Living Scale range from 0 (low function, dependent) to 8 (high function, independent) for women or from 0 to 5 for men. These data were collected to characterise the sample and identify factors that may be shaping care-givers' experiences that could be explored in the interview. The scales are widely used to assess functioning in people with dementia and have established validity and reliability (Lawton and Brody, Reference Lawton and Brody1969; Graf, Reference Graf2008; Koyfman and Finnell, Reference Koyfman and Finnell2019).
Narrative data were collected through semi-structured interviews that included broad, open-ended questions with a set of optional probes. The interviews addressed how age and ageing shaped care-givers' experiences (analysed separately and reported in Arbel et al., Reference Arbel, Cameron, Trentham and Dawson2023), and how they managed the challenges arising from age and ageing and care-giving (for sample questions, see Table 2; for the full interview guide, see the online supplementary material).
Table 2. Interview questions related to managing care-giving

In line with the narrative approach, the exact wording or order of the questions was not pre-determined to allow participants' stories to unfold in their own way and to allow the interviewer (IA, first author) to respond to the stories as they unfolded (de Medeiros, Reference de Medeiros2014). This dynamic interview style allowed for a joint creation of data.
Interviews were audio recorded and transcribed by a trained research assistant. Narrative summaries of each interview were written by IA. In these summaries, stories related to managing age-related care-giving challenges were put in the context of care-givers' larger care-giving story. Subsequent interviews began with reviewing the narrative summary, allowing participants to clarify any aspect of the summary, and responding to follow-up questions. All participants had two interviews. In three cases where issues needed to be further explored, a third interview was conducted. In total, 25 interviews were conducted.
Ethical considerations
The research protocol was approved by the research ethic boards at the University of Toronto and the Rotman Research Institute at Baycrest. Information about the study (e.g. the purpose, the process, and risks and benefits) was verbally provided to participants during the phone screen, and informed, written consent was obtained before beginning the first interview. Interviews were conducted in care-givers' preferred location to minimise time burden and accessibility challenges.
Data analysis
Data were analysed thematically within QSR International's NVivo qualitative data analysis software (version 12). To identify common themes of managing age-related care-giving challenges, reflected in care-givers' stories, we conducted what Polkinghorne (Reference Polkinghorne1995) termed a thematic analysis of narrative data (rather than a narrative analysis). The thematic analysis was theoretical, meaning that the development of the themes themselves involves interpretative work, and the analysis produced is theorised (Braun and Clarke, Reference Braun and Clarke2006). The two theoretical frameworks described above, the SOC model (Baltes and Carstensen, Reference Baltes and Carstensen1996) and the stress-coping theory (Lazarus and Folkman, Reference Lazarus and Folkman1984), guided our analysis. Concepts from these frameworks guided our identification of stories related to managing, and our interpretation and coding of these stories. Initial interpretations were made by IA and then discussed with the research team. Changes to the themes were made iteratively over a number of meetings.
Rigour
Steps taken to improve rigour were guided by Polkinghorne's work on validity issues in narrative research (Polkinghorne, Reference Polkinghorne2007). Polkinghorne suggests there are two major validity threats in narrative research. The first arises because the stories people tell about their experienced meaning are not a mirrored reflection of their experienced meaning. Reasons for this include limitations in people's willingness to reveal their self-explorations to others (especially to strangers), and in their ability to reflect on meanings outside their awareness. To address this threat, we chose a multiple interview design so that participants would gain confidence and trust in the interviewer over multiple sessions. The second validity threat relates to the difference between the storied text and the interpretation of the text by the researchers. To attend to this threat, we created our interpretations iteratively (during data collection, in between sessions), and the interviewer began each interview by sharing our emerging interpretations with the participants. Participants were then able to provide feedback and clarify questions that arose during the interpretative portion of the analysis.
Results
Participant characteristics
The study included 11 care-givers (eight wives, three husbands), with an average age of 84.5. All care-givers were white and identified as being in heterosexual marriages. All but one couple (late-life remarriage, 8.5 years) were married over 50 years and had one to three children together. With one exception, all care-givers reported having at least one chronic health condition. All care receivers had chronic health conditions in addition to dementia. Care-givers living with their spouses (N = 8) reported that their spouses were highly dependent on others for instrumental activities of daily living (Instrumental Activities of Daily Living Scale scores ranged from 0 to 3), and low to moderately dependent on others for basic activities of daily living (Physical Self-maintenance Scale scores ranged from 2 to 4). Care-givers caring for spouses who lived in LTC (N = 3) reported that their spouses were highly dependent on others for instrumental and basic activities of daily living (all scored 0 on both scales) (for details, see Table 3).
Table 3. Care-givers' characteristics

Notes: 1. Self rated physical health was assessed with the following question: In general, how would you describe your physical health: excellent, very good, good, fair or poor? 2. Low mood was assessed with a question from the Patient Health Questionnaire (PHQ-9; Kroenke et al., Reference Kroenke, Spitzer and Williams2003): Over the last 2 weeks, how often have you been bothered by the following problem – feeling down, depressed or hopeless: not at all, several days, more than half of the days, nearly every day. SwD: spouse with dementia. LTC: long-term care facility.
Key findings from the thematic analysis: themes and corresponding facilitators and barriers
Care-givers' stories of how they managed ageing-related care-giving challenges centred around four main themes: (1) adjusting goals to lessen care-giving demands and to mitigate stress (selection/problem-focused coping); (2) using alternative means to reach goals and to mitigate stress (compensation/problem-focused coping); (3) enhancing capacities to care and mitigate stress through engagement in non-care-giving activities (optimisation/problem-focused coping); and (4) choosing positive attitudes and perspectives to lessen emotional distress (emotion-focused coping). In the next section, each of the themes, subthemes and strategies described by care-givers (objective 1) are presented with the corresponding facilitators and barriers to using the strategies (objective 2). Findings are summarised in Table 4.
Table 4. Management strategies and corresponding facilitators and barriers
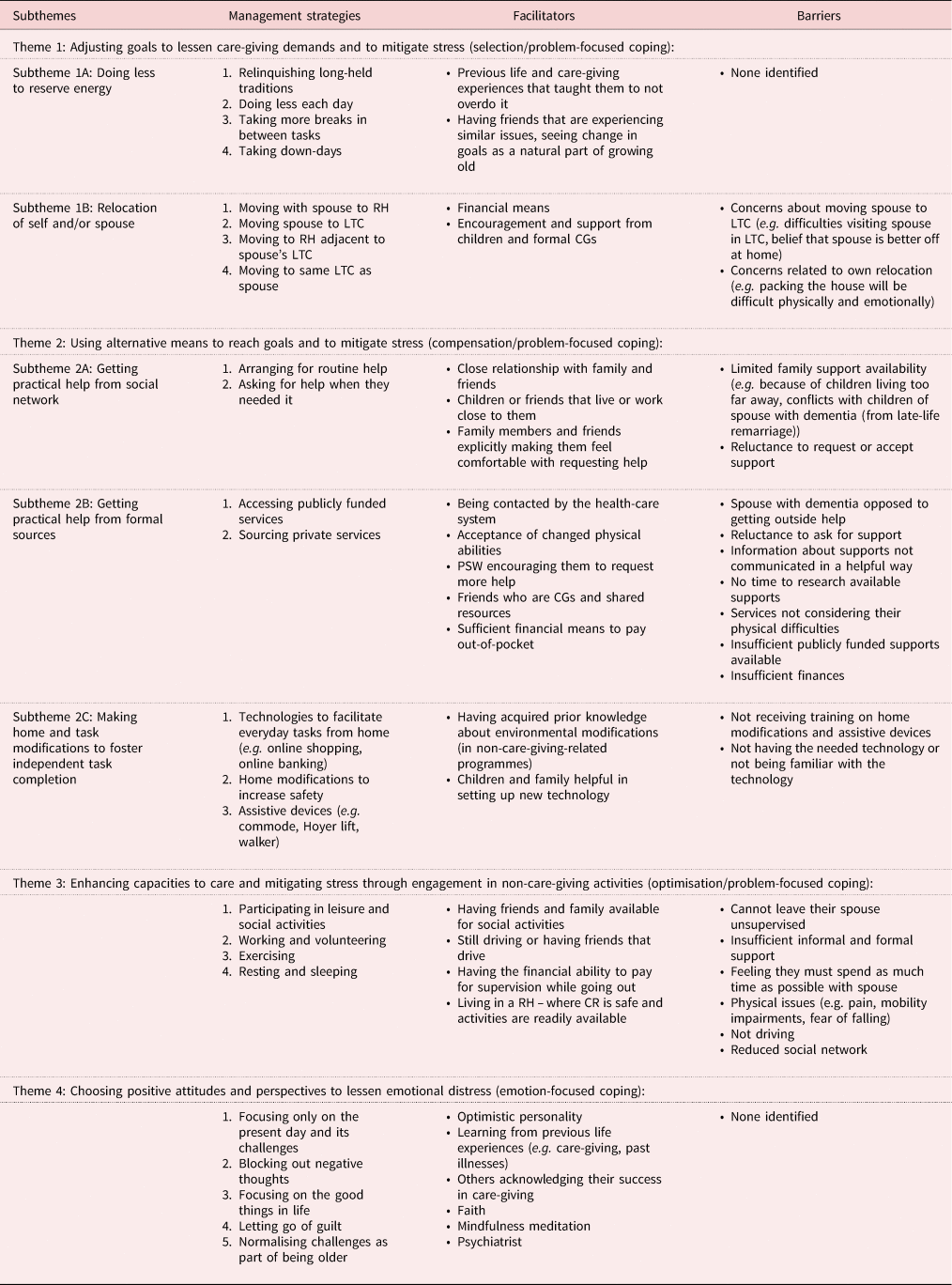
Notes: CG: care-giver. CR: care receiver. LTC: long-term care facility. RH: retirement home. PSW: personal support worker.
Theme 1: Adjusting goals to lessen care-giving demands and to mitigate stress (selection/problem-focused coping)
This theme included stories about changes that care-givers made to their care-giving goals (the care-giving-related tasks they aimed to perform or the environment in which they performed them) in order to lessen care-giving demands and to mitigate stress. The theme included two subthemes: doing less to reserve energy (1A) and relocation of self and/or spouse (1B).
Subtheme 1A: Doing less to reserve energy: ‘I don't go overboard the way I have done in the past’
Care-givers spoke of how they reduced the number of tasks they performed to reserve their energy (which they perceived as more limited compared to when they were younger) for tasks that were most pertinent to them, and how they lowered their expectations of themselves accordingly. Care-givers did this by relinquishing long-held traditions (e.g. going to the cottage for the summer), doing less each day (e.g. not bathing their spouse today), taking more breaks in between tasks and taking ‘down-days’ when needed.
Yesterday, at my daughters', usually that wears us both out. ’Cause we take the bus, and it's a long trip for us. Then the time there with her is always exciting and lots going on. And then home again. I always know that the following day, I won't do much. (P2, wife care-giver)
Reducing activities and pacing themselves, especially after busy days, helped care-givers conserve their energy so they could better regain care-giving duties in the days to come.
Facilitators to their willingness or ability to use these strategies included previous care-giving experiences that had showed them that they can accomplish much more if they don't overdo it, and perceiving the need to slow down as a normal part of ageing:
When I think of my older friends … they all need down-time. They all say, oh I had a busy day today, tomorrow I am going to stay home, and not do anything at all. So I'm not alone with that. It is just the natural process, I think. (P2, wife care-giver)
Seeing their peers also needing rest days helped normalise care-givers' decision to pace themselves, as this care-giver described. No barriers to this strategy were identified.
Subtheme 1B: Relocation of self and/or spouse: ‘All these things are taken care of’
Care-givers' stories included illustrations of how relocation of themselves and/or their spouse was utilised to lessen the demands of care, when the demands of care exceeded their abilities, or in anticipation of this happening. Care-givers discussed moving with their spouse to a retirement home when symptoms began, in preparation for the future, moving their spouse to LTC, moving to a retirement home adjacent to spouse's LTC and moving to the same LTC as their spouse.
Moving with their spouse in preparation for the future was perceived by care-givers and their family as a wise choice and relieved them of many care-giving tasks (e.g. cleaning, meal preparation), making their life easier:
When we bought, we were embarrassed to tell people that we moved to [retirement home]. I was only 64, [husband] was only 68 … our kids loved it, kids thought we were terrific; we were looking down the road … Our friends thought we were crazy … Now today, I hear the other story. ‘You were so smart to move into that place, and it's so wonderful’, and now there's a waiting list to get in. (P4, wife care-giver)
For this care-giver, having her sceptical friends finally acknowledge the wisdom in her decision to relocate early, strengthened the value of this strategy.
Care-givers talked about moving their spouse to LTC as a last resort, when caring at home, or at a retirement home, was no longer possible or safe for them and their spouse. Care-givers noted that by moving their spouse to LTC, they were able to focus more energy on taking care of themselves, which supported them in taking care of their spouse: ‘the solution was for her to go away so that I could repair myself so that I could look after her that way’ (P6, husband care-giver).
Care-givers who placed their spouse on a waiting list for LTC in anticipation of changes noted that this helped relieve some of their concerns about the future, when they would no longer be able to care for their spouse at home.
Moving to a retirement home adjacent to spouse's LTC or into the same LTC as their spouse was perceived by care-givers to make their life much easier, because it made visiting on a regular basis much easier:
I don't have to worry to get the car … or get a bus to go up there, and wonder what the weather is like. Is it slippery? … It's [the move] removed pressure on me without any doubt. It's made my life easier that way. (P7, husband care-giver)
Moving closer to his wife's LTC was perceived by this care-giver as a good strategy, because it eased logistical challenges like travel and weather concerns, making visiting safer and less stressful.
Facilitators to relocation decisions included having the financial means to do so and having others (children, personal support workers) observe and validate their struggles, as illustrated in the following quote: ‘I can remember my daughter saying to me, Dad if you don't let her go, you'll kill yourself caring for her’ (P6, husband care-giver).
Barriers to moving their spouses to LTC included insufficient finances (‘All we have is the house. We'll have to sell the house just to get him into a home’; P11, wife care-giver), preferring to age with spouse at home (‘Home is home, and I think [you should stay] as long as you can stay, and get the help that you need’; P8, wife care-giver), believing that no one can accommodate the needs of their spouse like they can, and fearing the separation on an emotional and logistical level: ‘I'm not that young either anymore. How am I going to get there? I have no car. It involves walking to the bus. Can I do that in the winter? Can I go over there? Can I see him?’ (P2, wife care-giver). This quote underscores care-givers' logistical concerns when contemplating the relocation of their spouse to LTC. The prospect of daily travel alone, especially when thinking about the snowy Canadian winter, elevated their anxiety.
Barriers to care-givers moving themselves included concerns that the move would require too much effort from them and their families, and that getting rid of their valuables and mementos will have an emotional toll on them. Care-givers also expressed concerns that they would not identify with residents of a retirement home and would not enjoy the ‘regimen’ in the LTC (P6, husband care-giver).
Theme 2: Using alternative means to reach goals and to mitigate stress (compensation/problem-focused coping)
This theme included stories about changes that care-givers made to the means by which they achieve their goals (i.e. how they performed care-giving tasks), so that they can continue meeting their goals/perform desired tasks and/or so that they can experience less stress as they do so. This theme included three subthemes: getting practical help from social network (2A), getting practical help from formal sources (2B), and making home and task modifications to foster independent task completion (2C).
Subtheme 2A: Getting practical help from social network: ‘When I can't do something, I phone them up’
Care-givers' stories illustrated how they asked for help from their social network for tasks they could not manage on their own (‘heavy things’, like lifting wheelchairs) or for tasks with which they were not familiar, often because their spouse used to handle them (e.g. home maintenance, finances, cooking):
My son and daughter-in-law are helpful frequently, but it's not on any, not on any regular basis. If I need something fixed or if I can't work the computer for some reason or another, or if I need a few minutes to go out and do something or whatever … they are there for emergency stuff. (P9, wife care-giver)
Care-givers' stories illustrated how they perceived their family's assistance as valuable, but not available to them on a regular basis. However, some care-givers did arrange for routine help from family members (e.g. taking their spouse out for lunch once a week, providing cooked food several times a week). Care-givers described this routine help with a lot of appreciation because of how busy they perceived others to be, as illustrated in this quote: ‘I'm so happy for that, and I'm grateful because she's a lawyer, she's busy’ (P8, wife care-giver).
Facilitators for care-givers' willingness to ask for support included having family members they felt ‘close’ to, who lived and/or worked close by, or who made it explicit that they welcomed their requests: ‘and she said to me “there's nothing wrong with asking one of us to come and take you to the doctor.” She said … “we could make time”’ (P8, wife care-giver).
Barriers to getting help included limited availability of social supports because friends were also ageing and dealing with their own problems, or because family lived far away. Several care-givers described strenuous relationships with their children that compromised the availability of family support. One unique illustration was provided by a wife care-giver in a late-life remarriage who was rejected by her husband's children:
His son was sort of open a little bit to the marriage. But the two daughters, furious. [They thought I was] marrying him for the money … Very rude, very hostile towards me … And even 8.5 years later, there's still a little hostility. (P10, wife care-giver)
This rejection meant that family support was very limited, chiefly provided by her own daughters, who lived in a different province and offered primarily emotional support from afar.
Another barrier to getting practical support from their social network was care-givers' reluctance to ask for or to accept support for several reasons, including not wanting to burden others, or upset their spouse, perceiving their independence as a source of pride, and not being used to asking others for help:
We always gave help, we never took help … I don't like needing people … I like to be able to take care of it myself. It's gonna be me first and only asking somebody if there's no other way. (P8, wife care-giver)
Care-givers' narratives portray their internal struggle with seeking or accepting family support. On one hand, they deeply appreciate assistance when received, but on the other hand, a strong sense of self-reliance and a reluctance to burden others often make asking for help a last resort.
Subtheme 2B: Getting practical help from formal sources: ‘It's time now that I need help’
This subtheme included stories of how care-givers obtained practical help from publicly funded or private services. Most care-givers reported that at some point in time, they realised that they needed routine help beyond that which could be provided by friends and family members. Strategies included accessing publicly funded services and sourcing private services when publicly funded services were insufficient.
Publicly funded services were sometimes offered to care-givers whose spouses were discharged from the hospital or had received a dementia diagnosis. These care-givers were contacted by a care co-ordinator and if their spouse was found eligible, they could accept funded services such as a personal support worker for several hours a week. Some care-givers were offered such services but turned them down because they were still managing on their own. One care-giver spoke of how she maintained regular contact with the care co-ordinator, to ensure that this help would be available to her, when the need arose:
I just think it is important that even if you're younger and you think, I can handle this very well, to make connections that if something unexpected happens, that you are not all of a sudden facing a mountain you cannot climb. (P2, wife care-giver)
This care-giver recognised the immense value in taking a proactive approach to maintain connections with formal service providers, particularly in preparation for unforeseen challenges.
Care-givers who were not contacted by care co-ordinators sourced publicly funded services primarily after learning about them from friends and family members who were also care-givers, or who worked in the health or social service sector: ‘I wouldn't have known about it [a day centre for people with dementia]. My social worker told me also, but I first learned about it from my friend's sister-in-law … somebody experienced. Somebody who is dealing [with dementia]’ (P8, wife care-giver). This quote illustrates a common narrative among care-givers who spoke of discovering publicly funded services ‘by chance’, often through informal networks like friends and family members with lived care-giving experiences.
Care-givers sourced private services (for which they paid out-of-pocket) in addition to publicly funded services, when they felt that publicly funded supports were insufficient. Some care-givers hired personal support workers from private agencies, but most could not afford this and arranged for more affordable support through their personal networks. Several care-givers were in the process of hiring a live-in formal care-giver.
Facilitators for getting help from formal sources (publicly and privately funded) included having sufficient finances, having older friends with care-giving experience who provided information about resources, having personal support workers recommend they get more help, which made them feel better about using public resources, and accepting their changed physical abilities:
I've come to realise that … perhaps going back to ageing, perhaps I've come to realise that I can't. I'm not as agile as I was. I can't bend down and get stuff out of the dryer and fold it because my shoulders hurt. And so on and so on. (P6, husband care-giver)
Care-givers' narratives depicted the significant role that their evolving perceptions of their own physical limitations played in their readiness to seek support. For some, the willingness to accept support only emerged when they recognised and made peace with their own limitations.
Barriers to getting practical help from formal sources were many. Some care-givers were reluctant to ask for or to accept publicly funded support because they believed that they should not ‘take advantage’ of, or ‘abuse the system’ unless it was absolutely necessary. If they were ‘healthy enough’, or they had ‘enough resources’, then they ‘should be the person responsible’ for their spouse (P3, wife care-giver). Otherwise, they might be depriving somebody else of this support. Care-givers were reluctant to get private support because they ‘are not from a generation that is used to paying for help’ (P8, wife care-giver) or because ‘entering into a commercial transaction’ of care seemed like a failure on their part (P6, husband care-giver).
Other barriers included the spouse with dementia being opposed to external help, having insufficient finances, supports not being communicated in a helpful way (‘I think I was told stuff, but it just went over the top of my head at the time’; P9, wife care-giver), or feeling overwhelmed by the amount of care-giving tasks and feeling that utilising a new service would just be another task to manage. Finally, care-givers identified that criteria for accessing publicly funded services for people with dementia did not consider their own physical difficulties.
Subtheme 2C: Making home and task modifications to foster independent task completion: ‘There are things we can manage on our own’
This theme included stories about modifications that care-givers made, either to the way they perform specific care-giving tasks or to the physical environment in which the task was performed, so that they could continue to perform the task independently. Care-givers discussed using technologies to facilitate everyday tasks from home (e.g. online shopping or banking), making (minor) home modifications to increase safety (e.g. by removing rugs, installing bars in the shower, installing motion alerts on the front door) and using assistive devices (e.g. commode, walkers or Hoyer lift used to transfer patients from spot to spot (e.g. bed to chair, chair to toilet, etc.)).
Facilitators reported by care-givers for home and task modifications included learning about environmental modifications (e.g. in a fall prevention programme that they themselves attended due to their own issues), and having children or grandchildren help them set up and use technologies (e.g. online grocery shopping): ‘my daughter said to me yesterday “mom, for the winter I will sign you up for grocery delivery, so that you can order your groceries, I don't want you to trek papa all the way to the shopping centre”’ (P2, wife care-giver). Care-givers’ stories, as illustrated in this quote, highlighted the valuable role of family involvement in facilitating home and task modifications, especially for technological solutions that they were less adept at using.
Barriers that care-givers mentioned included not receiving proper training about how to use assistive devices (e.g. Hoyer lifts), not having the needed technology for online services (e.g. computer, smartphone) or not being familiar with using the desired technology (which some care-givers attributed to their age).
Theme 3: Enhancing capacities to care and mitigating stress through engagement in non-care-giving activities (optimisation/problem-focused coping): ‘If you don't do things for yourself, you'll find deterioration’
This theme encompasses care-givers' active pursuit of non-care-giving activities, including leisure and social activities, work and volunteering, exercise, rest and sleep. These activities serve dual purposes: for some, they provide a means to stay connected with the world and keep their minds sharp, as exemplified in the quote: ‘[Working] keeps me current … I'm in the world with other people, and with business. You know, keeps me sharp … keeps me thinking’ (P4, wife care-giver). For others, these activities offer a brief respite from care-giving, helping them relieve some of their stress:
That's what you have to do … go out and meet people and do things … The care-giver has got to go out and get that pressure off him and get his mind directed elsewhere … I'd say it's essential. If not, you're gonna find deterioration. (P7, husband care-giver)
Care-givers' narratives underscore the vital role of non-care-giving activities in preserving their wellbeing and sustaining their care-giving capacity.
Facilitators that care-givers discussed included having the financial ability to pay for supervision, driving (‘Thankfully, I can still drive. I have a car, and I can still drive … that gives me freedom’; P4, wife care-giver), and having family members or friends who encouraged and even ‘pushed them’ to do things out of the house. Care-givers who were experiencing physical limitations noted that it was helpful to have friends who still drive and/or friends who are more physically capable. Care-givers who lived with their spouse in a retirement home noted that they were able to engage in their own activities because it was safe enough to leave their spouse alone unsupervised, and that the activities offered at the retirement home (e.g. game nights, movie nights) made it easier for them to maintain a life outside care-giving.
Barriers reported included feeling guilty about not being with their spouse (‘I could probably take more time off and let somebody else, but I do have a kind of guilt, that I know he's better off when I'm here’; P4, wife care-giver) and insufficient help (‘People say “you've got to get out more, you've got to do more things”. Well fine, how? It's not possible’; P9, wife care-giver). Some care-givers had difficulties engaging in out-of-home activities because of reasons they attributed to their ageing (e.g. lack of energy, pain, mobility difficulties and comorbidities). Care-givers felt that these difficulties made going out ‘so hard it's not worth it’ (P8, wife care-giver). A few care-givers reported being less active as their social circle had ‘faded away’ (P5, wife care-giver), some friends had died or were dealing with health issues of their own.
Theme 4: Choosing positive attitudes and perspectives to lessen emotional distress (emotion-focused coping): ‘If I don't laugh then I'll have to cry’
This theme included stories about how care-givers managed the emotional distress that arose from ageing-related care-giving challenges by choosing attitudes and perspectives that made them feel better. Care-givers discussed focusing on the day and ‘its own problems’ (P2, wife care-giver), blocking out thoughts that made them sad, focusing on the good things in their life, letting go of guilt and accepting their situation as a normal part of ageing, as illustrated in the following quote: ‘We grow with age into our age. Whatever comes we accept it as being part of our life, right? … It's just simply a matter of attitude’ (P2, wife care-giver).
Facilitators to choosing a positive attitude included having an optimistic personality, previous life experiences (e.g. past care-giving experiences, past illnesses) that had taught them adaptive skills, faith, therapy to manage guilt and practising mindfulness meditation. No barriers to this strategy were identified.
Ageing-related facilitators and barriers
Although not an aim of the study, this analysis also illuminated facilitators and barriers to strategy use that care-givers attributed to ageing. Table 5 outlines ageing-related facilitators and barriers described by care-givers, categorised across the four dimensions proposed by Kenyon et al. (Reference Kenyon, Clark and De Vries2001): intra-personal, inter-personal, socio-cultural and structural dimensions (as described in the methodology approach section).
Table 5. Ageing-related facilitators and barriers

Discussion and implications
To our knowledge, this is the first study to focus on how oldest-old spousal care-givers of people with dementia manage ageing-related care-giving challenges and concerns. Specifically, this study aimed to explore the strategies used by oldest-old care-givers to manage ageing-related care-giving challenges and the facilitators and barriers to using these strategies. The results illustrate the myriad of strategies used by oldest-old care-givers to attain their care-giving goals (i.e. complete their desired care-giving tasks) despite experiencing ageing-related challenges, and to mitigate the stress arising from these challenges.
The strategies used by care-givers centred around four main themes which aligned with the SOC model and the stress-coping theory which guided our analyses: (1) adjusting goals to lessen care-giving demands and to mitigate stress; (2) using alternative means to reach goals and to mitigate stress; (3) enhancing capacities to care and mitigate stress, through engagement in non-care-giving activities; and (4) choosing positive attitudes and perspectives to lessen emotional distress. Care-givers' stories also illuminated numerous facilitators and barriers to their use of these strategies.
Many of the strategies used by care-givers in this study are not unique to oldest-old spousal care-givers of people with dementia or to managing age-related care-giving challenges. For example, the use of formal and informal support, relocation of spouse to LTC and use of emotion-focused strategies have all been widely identified and discussed in the care-giving literature (see review by Hawken et al., Reference Hawken, Turner-Cobb and Barnett2018). The following section discusses new insights about strategies used by oldest-old care-givers to support their care-giving role alongside ageing.
Strategy use (objective 1)
Strategies related to relocation of self (e.g. relocation with spouse to a retirement home or relocation to a retirement home following spouse's relocation to LTC) were identified by care-givers as a means to lessen care-giving demands. The few care-givers who relocated did so proactively (in anticipation of future challenges), and deemed it extremely valuable. However, more care-givers talked about the concerns that prevented relocation. Self-relocation has not been widely addressed in the care-giving literature, but our findings are consistent with gerontological literature that suggests that proactive relocations (also termed proactive moves (Pope and Kang, Reference Pope and Kang2010) or anticipatory moves (Kahana et al., Reference Kahana, Kahana and Lee2014)), are potentially valuable, but less common among older adults, compared to crisis-driven reactive moves. The many reservations held by care-givers in this study about relocating (e.g. practical concerns, concerns about losing meaningful objects, concerns about losing freedom and negative age stereotypes about older people) align well with previous gerontological research (Lofqvist et al., Reference Lofqvist, Granbom, Himmelsbach, Iwarsson, Oswald and Haak2013). Because of these reservations, older people typically prefer to stay at home for as long as possible, and relocate only after exhausting all other options, such as modifying their current residential environments or adapting the activities they perform (Pope and Kang, Reference Pope and Kang2010; Golant, Reference Golant2011; Lofqvist et al., Reference Lofqvist, Granbom, Himmelsbach, Iwarsson, Oswald and Haak2013; Perry and Thiels, Reference Perry and Thiels2016). However, gerontological research also suggests that relocation in anticipation of changes can help older individuals lessen the stressors and challenges associated with ageing, optimise functioning and maintain autonomy for longer (Kahana et al., Reference Kahana, Kahana and Lee2014; Perry and Thiels, Reference Perry and Thiels2016). Proactive/anticipatory moves may be particularly valuable for oldest-old care-givers of people with dementia who can anticipate a deterioration of both their spouse's ability and their own abilities. As evidence about care-giver relocation is scarce, future research can continue to explore proactive/anticipatory relocation in older care-givers (e.g. how does relocation shape care-giving experiences and outcomes compared to home care, what facilitates a proactive move in oldest-old care-givers, is there an optimal time to start thinking of relocation?). If proactive relocation is found beneficial to the care-giving experience, these data may contribute to the design of interventions that support older care-givers in considering and/or executing such transitions.
Strategies related to enhancing capacities to care and mitigating stress, through engagement in non-care-giving activities, were rarely used by care-givers in this study. Care-givers spoke about wanting to engage in non-care-giving activities, but rarely being able to do so. Some care-givers selectively gave up valued activities to save energy and resources for their care-giving role. Care-givers who did report using such strategies deemed them as essential to their ability to provide care. Care-givers perceived these strategies as a potential means to maintain cognitive sharpness, physical strength and mental health, so as to delay expected ageing-related declines and to prolong their capacity to provide care. This expands on previous literature reporting that maintaining interests and hobbies, having time to themselves and partaking in activities external to care-giving can enhance positive adaptation for family care-givers of people with dementia (Teahan et al., Reference Teahan, Lafferty, McAuliffe, Phelan, O'Sullivan, O'Shea and Fealy2018). However, in this study, as in others (e.g. Mausbach et al., Reference Mausbach, Patterson and Grant2008), care-givers reported being very restricted in their ability to do this. In the care-giving literature, activity restrictions are typically attributed to the time spent on care-giving duties (Fancey et al., Reference Fancey, Keefe, Guberman, Barylak and Macleod2008; Mausbach et al., Reference Mausbach, Patterson and Grant2008) and researchers have suggested that care-givers be encouraged to use respite services in order to have time to participate in meaningful occupations, social roles and relationships (Kokorelias et al., Reference Kokorelias, Lu, Santos, Xu, Leung and Cameron2020). The findings of this study point to additional factors inhibiting this participation particularly related to care-givers' advanced age such as mobility impairments, driving cessation, loss of friends and reduced energy.
From an ageing perspective, if oldest-old care-givers are restricted in their ability to enhance or maintain their capacities via activity participation, this may affect not only their ability to provide care but also their ability to experience active and healthy ageing. Active ageing (Foster and Walker, Reference Foster and Walker2015) and healthy ageing (Beard et al., Reference Beard, Officer, de Carvalho, Sadana, Pot, Michel, Lloyd-Sherlock, Epping-Jordan, Peeters, Mahanani, Thiyagarajan and Chatterji2016) are the focus of two policy frameworks endorsed by the World Health Organization. Both frameworks encourage self-care and engagement in leisure and social activities as a means to maximise physical and mental capacities of older people (World Health Organization, 2002; Foster and Walker, Reference Foster and Walker2015; Beard et al., Reference Beard, Officer, de Carvalho, Sadana, Pot, Michel, Lloyd-Sherlock, Epping-Jordan, Peeters, Mahanani, Thiyagarajan and Chatterji2016). In light of these frameworks, we must ask ourselves whether the oldest-old care-giving population, a rapidly increasing subset of the ageing population, are fairly positioned to experience active and healthy ageing, and if not, how can we help them experience these? Future studies could explore how opportunities for older care-givers to participate in non-care-giving activities might be optimised, over and above providing time relief, and whether this would indeed result in healthier ageing for this population.
It is worth noting that these unique findings were largely elicited by constructs from the SOC model. The SOC model enabled us to conceptualise relocation-of-self as a selection-related strategy (i.e. selecting a less-demanding environment to live in, in which some care-giving tasks can be relinquished or more easily accomplished) and to explore whether relocation was made reactively or proactively in anticipation of future changes in care-givers' own competencies. Similarly, the SOC model provided a lens to think about participation in non-care-giving activities as a strategy not only to minimise stress (e.g. Ekwall et al., Reference Ekwall, Sivberg and Hallberg2007), but also as an optimisation-related strategy aimed at optimising physical and cognitive capacities needed to continue to meet care-giving demands alongside ageing. Future research can continue to examine the benefit/applicability of using the SOC model in research with oldest-old care-givers to provide an ageing lens to care-giving adaptation.
Facilitators and barriers to strategy use (objective 2)
Another unique contribution of this study was the comprehensive portrayal of facilitators and barriers across a wide array of strategies that care-givers identified. Previous research has primarily focused on facilitators and barriers to service utilisation and accessing formal and informal support (e.g. Brown et al., Reference Brown, Chen, Mitchell and Province2007; Brown and Chen, Reference Brown and Chen2008; Greenwood and Smith, Reference Greenwood and Smith2015). Together the studies identified a myriad of facilitators (e.g. past experiences, professional support to access services) and barriers (e.g. cost, lack of information, not wanting to bother others), which align well with those described by care-givers in this study. However, this study portrays facilitators and barriers to additional strategies, over and above the use of formal and informal supports (e.g. relocation of self, environmental adaptations). These data may inform the design of interventions to support oldest-old care-givers in facilitating using specific strategies. For example, insight into care-givers' concerns about relocating self and spouse could be beneficial for the design of interventions aiming to support relocation.
Unique insights into age-related barriers or facilitators were also provided by this study. Previous literature on older care-givers suggested that care-givers' (old) age can act as a barrier to obtaining formal or informal supports, because of generational-related reluctance to request or receive supports, lack of energy and stamina needed to access services, or having reduced social support due to friends ageing or dying (Pollitt et al., Reference Pollitt, Anderson and O'Connor1991; Greenwood et al., Reference Greenwood, Pound, Brearley and Smith2019). Our findings provide additional illustrations of how age can act as a barrier. For example, negative attitudes towards old age served as a barrier to relocation of self (not wanting to identify with other older adults) and to sourcing support from social networks (not wanting to appear dependent, despite experiencing significant challenges). Both of these can be linked to negative societal stigma about older adults as frail, ill, dependent and incompetent (Swift et al., Reference Swift, Abrams, Lamont and Drury2017). Care-givers also talked about their physical difficulties not being considered in eligibility criteria for formal services. A systematic lack of consideration of the unique needs of ageing bodies in dementia and/or care-giving services is a form of ageism (Richeson and Shelton, Reference Richeson, Shelton, Carstensen and Hartel2006; Swift et al., Reference Swift, Abrams, Lamont and Drury2017; Trentham and Neysmith, Reference Trentham and Neysmith2017). It is likely that the impact of negative social stigma and ageism on how oldest-old care-givers manage late-life care-giving is much greater than appears in these findings. The theoretical framework used in this study does not pay special attention to issues of ageism. It is possible that more specific theoretical perspectives are needed to illuminate ageism in care-giving research. For example, a theoretical perspective on coping with stigma (e.g. Miller and Kaiser, Reference Miller and Kaiser2001) or on adapting to, negotiating or resisting ageism and negative age stereotypes (see review by Richeson and Shelton, Reference Richeson, Shelton, Carstensen and Hartel2006) could yield more insight into ageism and negative age stereotypes in late-life care-giving. Findings from this study thus point to the need to explore further how these issues shape care-giving at an advanced old age. Such research may help identify places and situations in which ageism occurs in care-giving and identify ways in which ageism might be reduced, from the individual level to the structural level.
Another insight from this study is that ageing-related changes such as pain, mobility impairments, fear of falling, driving cessation or ageing friends can also act as barriers to engaging in non-care-giving activities as a means to enhance capacity to care and mitigating stress. As noted above, some care-givers talked about difficulties engaging in out-of-home activities (which we interpreted as an optimisation strategy, from the SOC model) because of reasons they attributed to their ageing. These care-givers' abilities to use optimisation strategies were inhibited by the same ageing-related changes they were trying to overcome. The notion of ageing-related barriers to using optimisation strategies is paradoxical since these strategies are aimed at managing ageing-related challenges. This paradox was previously identified by Freund and Baltes (Reference Freund and Baltes2002) and Ouwehand et al. (Reference Ouwehand, de Ridder and Bensing2007). They noted that while optimisation and compensation are meant to generate resources, they also consume a lot of resources and thus depend on the availability of resources, which themselves decline in old age. This makes optimisation and compensation strategies increasingly difficult to use. Ouwehand et al. (Reference Ouwehand, de Ridder and Bensing2007) suggested a very important adaptive strategy might be anticipating negative changes, and handling them proactively, at an early stage. This could help prevent greater ageing-related stressors from occurring, which in turn may help preserve resources needed for optimisation and compensation (Ouwehand et al., Reference Ouwehand, de Ridder and Bensing2007). It is possible that early interventions aimed at preventing some of the anticipated ageing-related care-giving challenges could also help care-givers maintain resources for longer, allowing them to utilise strategies for longer.
Assessing changes in care-givers' health and functional status alongside their spouse's dementia progression can help clinicians support care-givers in proactively planning for changes, rather than reacting to them when a crisis appears. This is especially important because anticipated changes in care-givers' health are not only a result of their ageing, but also of their spouse's disease progression. Research suggests that care-giving for more severely affected patients with Alzheimer's disease can increase care-givers' risk of comorbidities (Szabo et al., Reference Szabo, Lakzadeh, Cline, Palma dos Reis and Petrella2019). Further, future research on oldest-old care-givers can benefit if data on care-givers' physical, cognitive and emotional status, and their own ability to perform activities of daily living, are collected and used for sample description and an exploration of how these shape care-giving experiences.
The study sample included one wife caring for a husband from a late-life remarriage (married seven years before the onset of dementia). Her illustrations of barriers to receiving support from her husband's adult children align well with previous research (Sherman and Boss, Reference Sherman and Boss2007; Roberts and Struckmeyer, Reference Roberts and Struckmeyer2019). With growing numbers of older adults entering into late-life marriages which may be impacted by dementia (Roberts and Struckmeyer, Reference Roberts and Struckmeyer2019), purposefully including care-givers in late-life remarriages will be of value to the growing evidence base on oldest-old spousal care-givers of people with dementia.
Finally, our findings illustrate how ageing-related factors can also facilitate the use of some strategies. For example, being older and living through other care-giving and illness-related experiences facilitated care-givers in allowing themselves to slow down and do less to reserve their energy. Having an ageing social network meant that many other friends were experiencing similar issues and could share their knowledge of accessing formal supports. This aligns well with Donnellan et al. (Reference Donnellan, Bennett and Soulsby2017), who suggest that access to peers with shared experiences (whether through personal networks, community groups or care-giving support groups) can increase emotional and informational dimensions of support and reduce psychological distress, depressive mood and burden.
Though the study focused on oldest-old care-givers of people with dementia, the issues identified might be relevant to oldest-old spouses caring for people with progressive disabling physical conditions such as Parkinson's disease or multiple sclerosis. Future research can explore if and how caring for spouses with different conditions in late-life differs.
Limitations
This study has several limitations. Although efforts were made to recruit a diverse sample of care-givers, the final sample accrued was comprised only of white, Western European descendants, who were either born in Canada or emigrated over 60 years ago. Most care-givers identified as Jewish and the rest were either Christian or Agnostic. It is likely that some of the results are not applicable to care-givers from other groups. All care-givers identified as being in heterosexual relationships and all but one couple were in a long marriage. Care-givers in non-heterosexual relationships and late-life remarriages may have provided additional insights, particularly in relation to facilitators and barriers for strategy use. The study included primarily women care-givers. More research is needed to illuminate the ways that oldest-old men care-givers manage care-giving. Finally, the study is limited by the theoretical frameworks used (the SOC model and the stress-coping theory). Although we believe our analysis was rigorous, it is possible that issues not highlighted in these frameworks were missed or misinterpreted during data analysis and interpretation.
Conclusions
To summarise, this study aimed to explore how oldest-old spousal care-givers manage ageing-related care-giving challenges. The study provides a comprehensive portrayal of the strategies used by care-givers to attain their care-giving goals and to reduce stress. The study also provides an extensive description of the facilitators and barriers to the utilisation of specific strategies, and highlights those facilitators and barriers that care-givers attributed to age and ageing. With the use of a theoretical framework that combines constructs related to care-giving stress and constructs related to goal attainment amidst ageing-related changes, the study revealed unique nuances related to strategy use (or non-use) that had received limited attention in previous care-giving literature, but are particularly important to consider in the context of late-life care-giving and/or ageing in the care-giving role. By doing so, this study contributes to the small but growing evidence base on oldest-old care-givers, and provides a foundation for future work in this area. With the rapid growth of this care-giving subgroup, advancing this research is paramount to our ability to design interventions and services that are adapted to the unique situation of oldest-old care-givers, and that support them in managing their care-giving role.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0144686X23000673.
Acknowledgements
We wish to acknowledge Nan Greenwood, PhD, Faculty of Health, Social Care and Education, Kingston University and St George's University of London, London, UK and David Burne, PhD, Associate Professor at the University of Toronto, Factor-Inwentash Faculty of Social Work, University of Toronto, Toronto, Canada, for reviewing the manuscript and providing comments that greatly improved it. We also wish to thank Emily Wright, the research assistant who transcribed the data.
Author contributions
The manuscript was written by IA as part of her PhD research. DRD, BT and JIC, the supervisory committee, all made a substantial contribution to the conception and design of the study, the interpretation of results and revisions of the manuscript. All authors reviewed and approved the final version of the manuscript.
Financial support
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests
The authors declare no competing interests.
Ethical standards
The research protocol was approved by the research ethic boards at the University of Toronto (#37556) and the Rotman Research Institute at Baycrest (#19-14).







