Allergic and respiratory diseases are complex, heterogenous and common disorders, especially in children. In the last decades, prevalence has increased and now seems to be stabilising in westernised countries.(Reference Asher, Rutter and Bissell1,Reference García-Marcos, Asher and Pearce2) Although there is an important genetic component in the aetiology of allergic and respiratory disorders, this rapid increase suggests an effect of environmental and behavioural changes such as a switch in dietary habits.(Reference Burbank, Sood and Kesic3) Many nutrients are involved in immunoregulatory pathways, giving the diet an important role in the regulation of chronic inflammation.(Reference Guilleminault, Williams and Scott4) As allergic mechanisms include immune system dysregulation and asthma is characterised by a chronic inflammation of airways and oxidative stress, it has been hypothesised that inadequate antioxidant intakes and the inflammatory potential of the diet may be involved in the aetiology of allergic disorders and asthma.(Reference Allan, Kelly and Devereux5)
Early life represents a key window of vulnerability and opportunity for health later in life.(Reference Barker6) Both the prenatal inflammatory potential of the diet and antioxidant intake may contribute to the maturation of the fetal immune system and lungs.(Reference Devereux and Seaton7) Thus, the maternal diet during pregnancy might be a potential area of interest for the prevention of allergic and respiratory disorders in offspring. Some antioxidants or nutrients with anti-inflammatory effects, such as vitamin D, E and Zn, have been associated with a lower risk of childhood allergic and respiratory diseases in epidemiological studies,(Reference Nurmatov, Devereux and Sheikh8–Reference Martindale, McNeill and Devereux13) but results remain heterogeneous as other studies reported adverse effects(Reference Tuokkola, Lamminsalo and Metsälä14) or no association,(Reference Nwaru, Erkkola and Ahonen15) and clinical trials of supplementation have failed to demonstrate beneficial effects.(Reference Allan, Kelly and Devereux5,Reference Yepes-Nuñez, Brożek and Fiocchi16) Most observational studies have focused on specific nutrients without considering the interaction between them, but as foods and meals are complex matrices of multiple nutrients, studying them together may offer a more realistic approach.(Reference Hu17) Moreover, although allergic and respiratory diseases frequently coexist in children,(Reference Anto, Bousquet and Akdis18) a comprehensive approach, considering the multimorbidity of allergic and respiratory diseases, has rarely been considered.
Tools have been developed to assess the antioxidant activity of dietary compounds through the dietary total antioxidant capacity (DTAC),(Reference Serafini and Del Rio19) as well as the global inflammatory potential of the diet with the dietary inflammatory index (DII) designed by Shivappa et al. (Reference Shivappa, Steck and Hurley20) The total antioxidant capacity of diet during pregnancy has never been studied in relation with allergic and respiratory diseases in children, although five recent studies have investigated the role of a pro-inflammatory maternal diet with allergic and respiratory diseases in children. Two of these studies reported a higher risk of asthma(Reference Chen, Lyons and Navarro21) or early wheezing(Reference Hanson, Rifas-Shiman and Shivappa22) in children, whereas the others found no association.(Reference Venter, Palumbo and Sauder23–Reference Sivula, Puharinen and Hantunen25) Lower lung function was also associated with a pro-inflammatory maternal diet in two studies.(Reference Hanson, Rifas-Shiman and Shivappa22,Reference Mensink-Bout, van Meel and de Jongste24) However, these studies mainly focused on respiratory health, and outcomes were considered separately.
We aimed to investigate the associations between the antioxidant and inflammatory potential of the maternal diet with allergic and respiratory multimorbidity in children.
Methods
Study design
We analysed data from ELFE study (Etude Longitudinale Française depuis l’Enfance), a longitudinal nationwide French birth cohort. The cohort design has been described elsewhere.(Reference Charles, Thierry and Lanoe26) Briefly, 18 329 mother–child pairs were included from a random sample of 320 maternity units in mainland France. Enrolment began in 2011 and was divided into four periods to consider seasonal variability: 1 to 4 April; 27 June to 4 July; 27 September to 4 October; and 28 November to 5 December. Inclusion criteria were mothers ≥18 years old, giving birth to liveborn singletons or twins at ≥ 33 weeks of gestation, with no plan to leave metropolitan France in the next 3 years.
Ethics
This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects/patients were approved by the Advisory Committee for Treatment of Health Research Information (Comité Consultatif sur le Traitement de l’Information en matière de Recherche dans le domaine de la Santé, approval number n°10.623), the National Data Protection Authority (Commission Nationale Informatique et Libertés, approval number n°910504) and the National Committee for Statistical Information. Written informed consent was obtained from both parents or only from the mother, informing the father to his right to object to the participation of his child.
Maternal diet
Information on maternal dietary intake in the last 3 months of pregnancy was collected by a self-administrated 125-item food frequency questionnaire (FFQ), designed for the pregnant French population(Reference Kadawathagedara, Ahluwalia and Dufourg27) and completed at inclusion in maternity units. Daily consumption frequencies estimated with the questionnaire were multiplied by portion size(Reference Hercberg, Deheeger and Preziosi28) to obtain daily food and drink intakes, and nutrient intakes were estimated by crossing daily food intakes with the SU.VI.MAX food composition database.(Reference Hercberg29) Mothers who did not answer the questionnaire, had more than ten missing items or had suspected extreme under- or over-reporting (total daily energy intake <933 kcal/d – 3rd percentile or >5072 kcal/d – 97th percentile) were excluded from the study.
Dietary total antioxidant capacity
The cumulative antioxidant capacity of the diet was estimated by calculating the dietary total antioxidant capacity (DTAC)(Reference Serafini and Del Rio19) obtained by using two Italian databases(Reference Pellegrini, Serafini and Colombi30,Reference Pellegrini, Serafini and Salvatore31) which estimate the antioxidant capacity of 156 plant-based foods, beverages and spices with three different in vitro assays: the Trolox equivalent antioxidant capacity (TEAC), the total radical trapping antioxidant parameter (TRAP) and the ferric reducing-antioxidant power (FRAP). Fifty-five items from the FFQ were matched with their corresponding antioxidant value. If one item corresponded to various foods, the average of the available antioxidant values was calculated (i.e. the item ‘strawberries and raspberries’ was attributed to the mean of the antioxidant values for strawberries and raspberries, see online Supplementary Table S1). Three different versions of the DTAC score were calculated to ensure consistency between the different in vitro measurement methods.(Reference Serafini, Villano and Spera32) The score for each participant was calculated by summing the product of the antioxidant capacity of each food multiplied by its daily intake. The greater the score, the higher the antioxidant capacity of the diet. Since antioxidant capacity through coffee consumption was responsible for 41 %, 45 % and 57 % of the TEAC, FRAP and TRAP version of the DTAC score and was highly correlated with the scores (Pearson, all r > 0·93, online Supplementary Table S2), and daily coffee consumption is highly heterogenous (median = 4·9 ml, 90th percentile = 250 ml), we chose to calculate versions of the DTAC scores excluding coffee. All versions of the DTAC score were adjusted for total energy intake with the residual method.(Reference Willett, Howe and Kushi33)
Energy-adjusted dietary inflammatory index
The inflammatory potential of the maternal diet was assessed using an energy-adjusted dietary inflammatory index (E-DII), a comprehensive indicator of anti-inflammatory and pro-inflammatory components of the diet. The index was obtained using the literature-based inflammatory weights of twenty-eight dietary components calculated by Shivappa et al. according to their anti-/pro-inflammatory potential (effect on IL-1β, IL-4, IL-6, IL-10, TNF-α and C-reactive protein) (online Supplementary Table S3) and ranges from –0·795 to 0·373.(Reference Shivappa, Steck and Hurley20) More precisely, the index of each participant was calculated as follows: (i) the energy-adjusted daily intake of each nutritional component was calculated using the residual method,(Reference Willett, Howe and Kushi33) (ii) a z-score was calculated (by subtracting the mean in our population from the energy-adjusted daily intake and dividing by the standard deviation of our population), (iii) to reduce right skewness, z-scores were converted into percentile scores and (iv) percentile scores were multiplied by 2 and subtracted by 1, so they could range from –1 to 1. Subsequently, each percentile score was multiplied by the inflammatory weight and then summed to obtain the overall E-DII score for each participant, ranging theoretically from –7·79 to +7·79. The higher the score, the more pro-inflammatory the potential of the diet; the more negative the score, the greater the anti-inflammatory the potential of the diet.
Allergic and respiratory multimorbidity
Allergic and respiratory multimorbidity clusters were derived by latent class analyses in a previous study.(Reference Delvert, Charles and Leynaert34) Briefly, based on information collected by phone interviews to parents at different times between 2 months and 5·5 years, ever food allergy, ever rash, ever night cough, ever wheeze, ever medication for asthma, ever medical consultation for asthma, ever allergic conjunctivitis up to 5·5 years and allergic rhinitis at 5·5 years were used for the construction of clusters. Five clusters were identified with the following characteristics (online Supplementary Table S4):
-
‘asymptomatic’ (43 %, n 4841), children with few allergic and respiratory symptoms
-
‘early wheeze without asthma’ (34 %, n 3785), children with a high prevalence of night cough and wheeze in early life, but without medical consultation for asthma
-
‘asthma only’ (7 %, n 829), children with respiratory symptoms, including medication and consultation for asthma, and a low prevalence of other allergies
-
‘allergies without asthma’ (7 %, n 804), children with a high prevalence of food allergy, eczema, allergic conjunctivitis and rhinitis, but few respiratory symptoms
-
‘multi-allergic’ (9 %, n 987), children with a high prevalence of both allergic and respiratory symptoms.
Covariates
Maternal and household characteristics were collected at inclusion and at 2 months of age, and child’s sex was extracted from the medical records. Maternal characteristics used as covariates in our analyses were age (<25, 25–29, 30–34 and ≥35 years), education level (upper to lower secondary, upper secondary, intermediate, 3-year university degree and at least 5-year university degree), migration history (immigrant, second-generation immigrant and born in France to French parents), smoking status (never smoker, smoker before pregnancy, smoker in early pregnancy and smoker throughout pregnancy), number of older children in the household (no siblings, one sibling and ≥2 siblings) and family history of allergy (asthma, allergic rhinitis or eczema in at least one parent or sibling; yes/no). Household characteristics included monthly household income by consumption unit (≤750€, 751–1111€, 1112–1500€, 1501–1944€, 1945–2500€ and >2500€), living area (urban and rural) and region (Paris region, Paris Basin – East, Paris Basin – West, North, East, West, South-West, South-East and Mediterranean). Self-reported height and weight were used to calculate pre-pregnancy BMI (<18·5, 18·5–24·9, 25–29·9 and ≥30 kg/m2), and physical activity during pregnancy was assessed with the Pregnancy Physical Activity Questionnaire (PPAQ; per point).(Reference Chasan-Taber, Schmidt and Roberts35)
Study sample
After exclusion of children whose parents withdrew consent (n 57), random selection of one twin (n 287), exclusion of children not followed up until the age of 5·5 years or without data available for allergic and respiratory multimorbidity clusters (n 6739), and mothers with missing, incomplete or implausible food intakes (n 1567), 9679 mother–child pairs remained and were included in the main analyses (Fig. 1). Among them, 740 had missing values for at least one covariate.
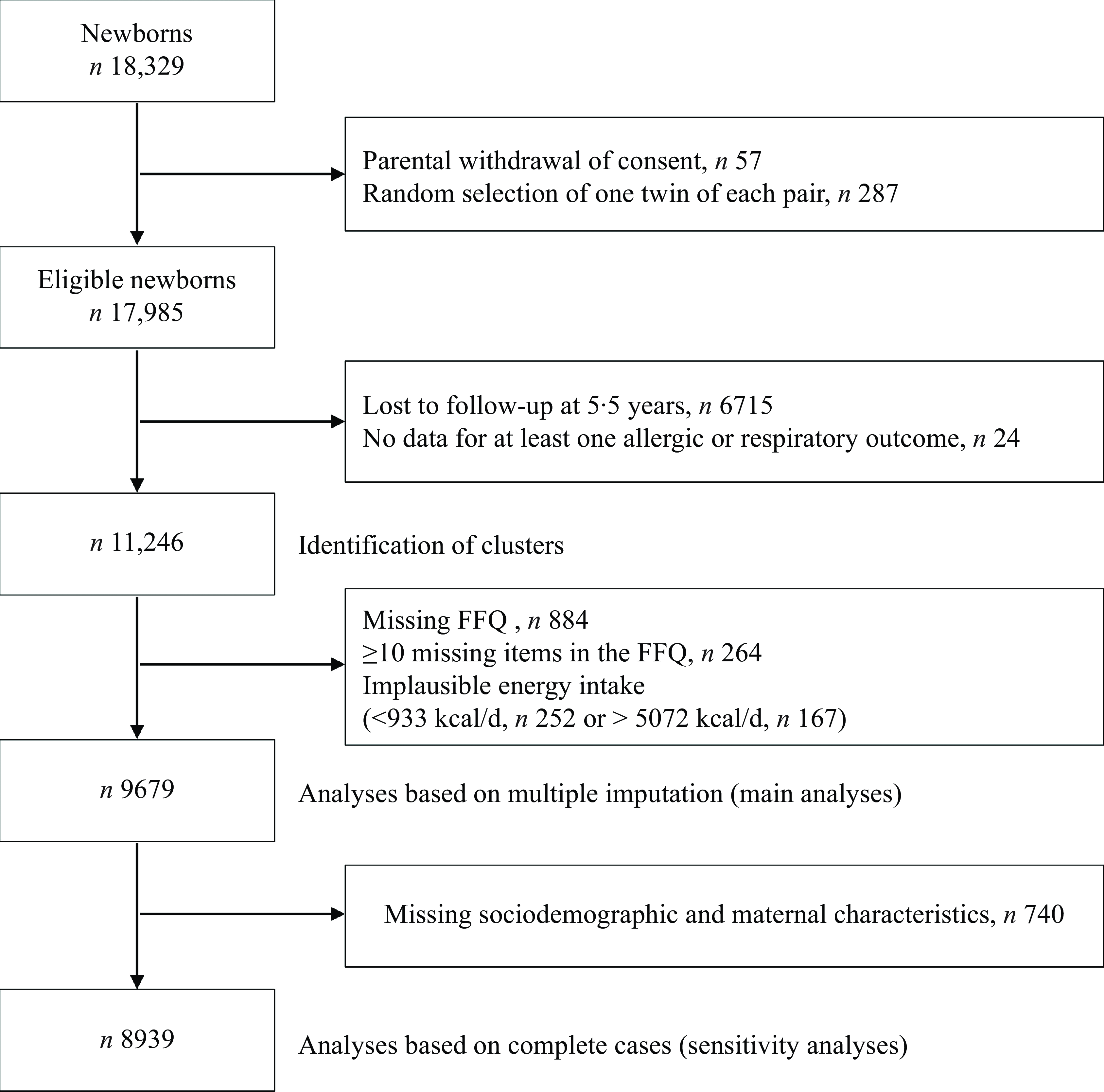
Figure 1. Flow chart of the study population.
Statistical analysis
Characteristics of mother–child pairs included in the study population were compared with excluded pairs using Student’s t tests for continuous variables and Pearson’s χ 2 tests for categorical variables.
Pearson’s correlations were calculated between the different versions of the DTAC to assess consistency.
Missing covariates were assumed to be missing at random, and multiple imputation was performed by generating five independent datasets with the Fully Conditional Specification method (FCS, MI procedure, FCS method, online Supplementary Table S5). Potential confounders were identified from the literature, and a directed acyclic graph was constructed to select covariates (online Supplementary Fig. S1). Multinomial logistic regressions were performed between the different versions of the maternal DTAC or E-DII scores and allergic and respiratory multimorbidity clusters (reference: ‘asymptomatic’ cluster). First unadjusted models were run and then models were adjusted for all covariates identified in the directed acyclic graph (maternal age at delivery, level of education, household income, migration status, smoking status during pregnancy, pre-pregnancy BMI, physical activity during pregnancy, number of older children, living area, region and family history of allergy), plus variables related to study design: maternity unit size and period of enrolment (corresponding to the season), child sex and daily energy intake. Interactions between dietary scores and family history of allergy, child’s sex and maternal smoking status during pregnancy were tested, and analyses were stratified if P-value < 0·05. Analyses were first performed with the imputed datasets and then replicated in the complete-case sample to verify consistency. We chose to present the associations with DTAC scores without the coffee component in our main analyses. Analyses with DTAC scores including coffee are presented in the supplementary material (online Supplementary Table S6).
The design of the ELFE cohort enables calculation of weights to correct for selection bias; thus, weights with truncation were calculated based on the inclusion procedure and biases related to non-consent and attrition(Reference Siméon36) and also included margin calibration from the state register’s statistical data and the 2010 French National Perinatal study(Reference Blondel, Lelong and Kermarrec37) on the following variables: age, marital status, migration status, education level, primiparity and region. Additional analyses were performed based on the weighted sample.
All analyses were carried out with SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Subject characteristics
Mothers included in the study sample were older at delivery (31·6 v. 29·9 years), had a higher level of education (24·3 % v. 14·0 % with at least a 5-year university degree), higher household income per consumption unit (1755 v. 1448 euros/month), were less frequently primiparous (43·1 % v. 46·4 %) and less frequently smoked throughout pregnancy (12·6 % v. 20·5 %) compared with excluded mothers. Included children more frequently belonged to families with a history of allergies (53·1 % v. 44·8 %) and were more frequently born in the summer or spring (42·1 % v. 38·6 %). Characteristics of included mother–child pairs are presented in Table 1.
Table 1. Sociodemographic characteristics of the 9679 included mother–child pairs from the ELFE cohort
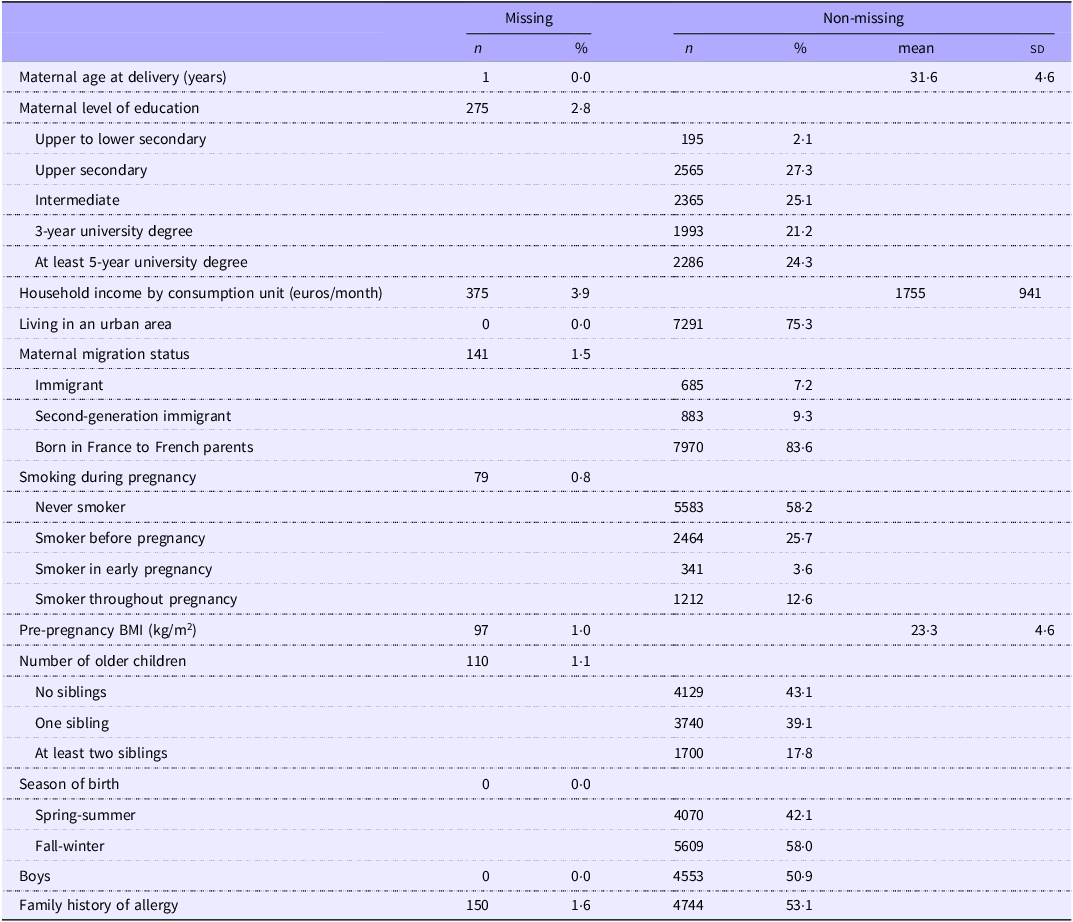
BMI, body mass index.
Maternal energy-adjusted dietary inflammatory index and dietary total antioxidant capacity and child allergic and respiratory multimorbidity
None of the tested interactions (see methods section) reached the level of significance of P < 0·05. Maternal E-DII and DTAC scores in our study population are described in Table 2.
Table 2. Nutritional characteristics of the 9679 included mothers from the ELFE cohort
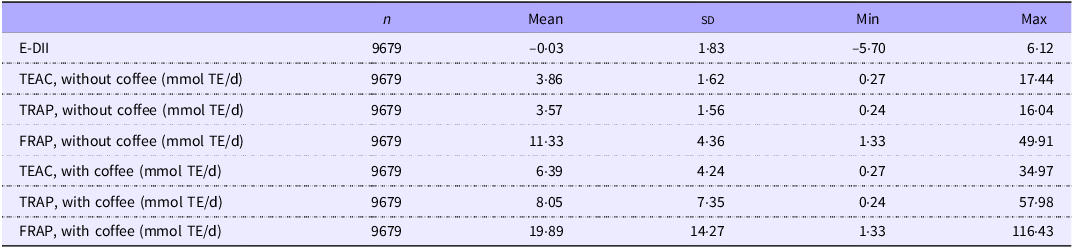
E-DII, energy-adjusted dietary inflammatory index; TEAC, Trolox equivalent antioxidant capacity; TE, Trolox equivalents; TRAP, total radical trapping antioxidant parameter; FRAP, ferric reducing-antioxidant power.
Dietary total antioxidant capacity without coffee
The three versions of the DTAC excluding coffee were highly correlated (Pearson, all r > 0·97, online Supplementary Table S2), and the two most contributing items were fruit juices and tea. In unadjusted analyses (Table 3), the maternal DTAC was negatively associated with the risk of belonging to the ‘early wheeze without asthma’ cluster in children, consistently in the three versions of the score. The associations remained significant in adjusted models with the TEAC (aOR (95 % CI) = 0·95 (0·90, 0·99) per sd, P = 0·02), and a similar trend was observed with the TRAP (aOR (95 % CI) = 0·96 (0·91, 1·01) per s d, P = 0·08) and FRAP (aOR (95 % CI) = 0·95 (0·91, 1·00) per s d, P = 0·05). Additional analyses on the complete-case sample and the weighted sample showed similar associations (Table 3).
Table 3. Associations between the DTAC scores (excluding coffee) of maternal diet during pregnancy and allergic and respiratory multimorbidity clusters in children of the ELFE study
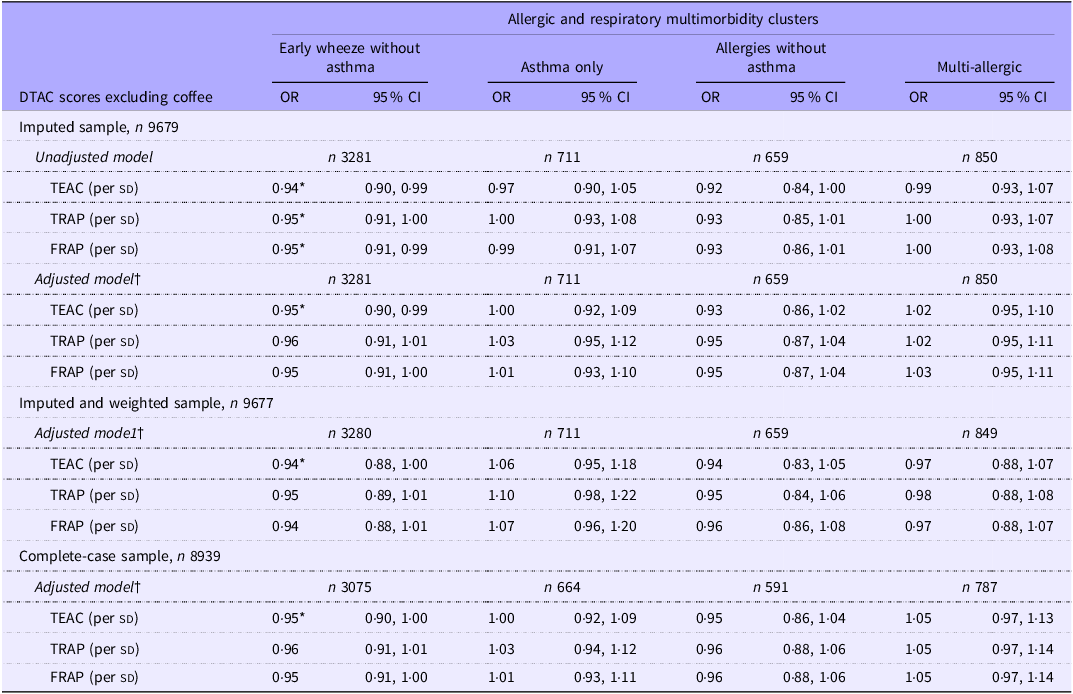
DTAC, dietary total antioxidant capacity; TEAC, Trolox equivalent antioxidant capacity; TRAP, total radical trapping antioxidant parameter; FRAP, ferric reducing-antioxidant power.
Each score was considered in a separate model.
Cluster of reference: ‘asymptomatic’.
OR (95 % CI) from multinomial logistic regressions.
* P < 0·05.
† Models were adjusted for maternal characteristics (age at delivery, level of education, household income, migration status, smoking status during pregnancy, pre-pregnancy BMI, physical activity during pregnancy, number of older children, living area (urban/rural), region, total energy intake), child characteristics (sex and family history of allergy) and study design characteristics (period of enrolment and size of maternity unit).
In sensitivity analyses considering the DTAC scores with the coffee component, no association was found (online Supplementary Table S6).
Energy-adjusted dietary inflammatory index
In unadjusted analyses (Table 4), the maternal E-DII score was positively associated with the risk of belonging to the ‘early wheeze without asthma’ cluster (OR (95 % CI) = 1·05 (1·00, 1·10) per s d, P = 0·04) and the ‘asthma only’ cluster (OR (95 % CI) = 1·11 (1·02, 1·20) per s d, P = 0·01). After adjustment for potential confounders, the associations were slightly attenuated for the ‘early wheeze without asthma’ cluster (aOR (95 % CI) = 1·04 (0·99, 1·09) per s d, P = 0·14) and the ‘asthma only’ cluster (aOR (95 % CI) = 1·09 (1·00, 1·19) per s d, P = 0·05). These weak associations were consistently observed in sensitivity analyses, though the association with the ‘asthma only’ cluster was attenuated in the weighted sample (Table 4).
Table 4. Associations between energy-adjusted dietary inflammatory index (E-DII) score of maternal diet during pregnancy and allergic and respiratory multimorbidity clusters in children of the ELFE study
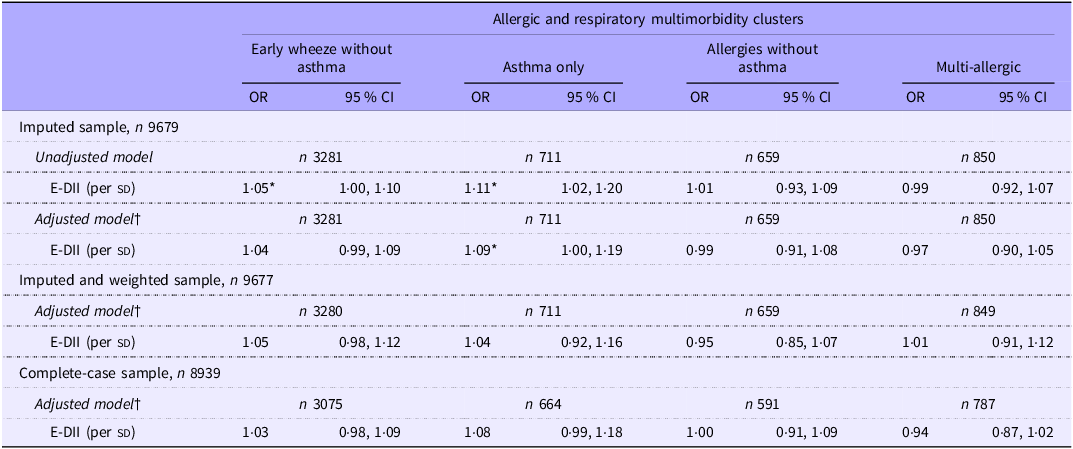
E-DII, energy-adjusted dietary inflammatory index.
Cluster of reference: ‘asymptomatic’.
OR (95 % CI) from multinomial logistic regressions.
* P < 0·05.
† Models were adjusted for maternal characteristics (age at delivery, level of education, household income, migration status, smoking status during pregnancy, pre-pregnancy BMI, physical activity during pregnancy, number of older children, living area (urban/rural), region and total energy intake), child characteristics (sex and family history of allergy) and study design characteristics (period of enrolment and size of maternity unit).
Discussion
In this large, longitudinal prospective study on 9679 mother–child pairs, two complementary approaches were used to assess the impact of the antioxidant and pro-inflammatory capacities of the maternal diet during the last trimester of pregnancy on offspring health. The antioxidant capacity of the maternal diet, from sources other than coffee, was associated with a lower risk of belonging to the ‘early wheeze without asthma’ cluster. The pro-inflammatory score of the maternal diet was associated with a higher risk of belonging to the ‘asthma only’ cluster and marginally associated with the ‘early wheeze without asthma’ cluster in children. All the identified associations had a limited effect size. No associations were observed with either score and the ‘allergies without asthma’ and ‘multi-allergic’ clusters.
Dietary total antioxidant capacity
We reported an inverse association between a higher antioxidant capacity of the maternal diet and the risk of belonging to the ‘early wheeze without asthma’ cluster up to 5·5 years, with no association with other allergic and respiratory multimorbidity clusters. We chose to exclude coffee from the DTAC scores, as this component accounted for a high proportion of the scores, making it not possible to distinguish the potential beneficial effects of antioxidants in coffee from the deleterious effects of caffeine during pregnancy.(38) Moreover, the FFQ items were matched with an Italian database which does not necessarily reflect the concentration and bioavailability of antioxidants in French coffee which depend on type of coffee, type of beans, roasting method, etc.(Reference Yashin, Yashin and Wang39) The predominance of coffee in the DTAC scores has already been reported elsewhere and limits the investigation into other dietary sources of antioxidants.(Reference Villaverde, Lajous and MacDonald40–Reference Rossi, Tavani and Ciociola42) The total antioxidant capacity of the maternal diet has never been studied before in relation with allergic and respiratory diseases, but the FRAP has been related to a lower risk of preterm birth(Reference Sartorelli, Carvalho and da Silva Santos43) and the TEAC, FRAP and TRAP to a low birth weight and gestational diabetes.(Reference Daneshzad, Tehrani and Bellissimo44) A few studies have focused on the total antioxidant capacity of children’s diets, reporting an inverse association with allergic asthma,(Reference Gref, Rautiainen and Gruzieva45) asthma in children of non-smoking parents(Reference Rodríguez-Rodríguez, Ortega and González-Rodríguez46) and an association with a greater lung function at 16 years in asthmatic children at 8 years.(Reference Sdona, Hallberg and Andersson47) Studies on maternal intake of specific antioxidants have highlighted associations between a higher maternal intake of copper,(Reference West, Dunstan and McCarthy11) long-chain n-3 fatty acids,(Reference Sordillo, Rifas-Shiman and Switkowski48) Zn(Reference Bédard, Northstone and Holloway10,Reference Litonjua, Rifas-Shiman and Ly12) and vitamin E(Reference Litonjua, Rifas-Shiman and Ly12,Reference Martindale, McNeill and Devereux13) and a lower risk of impaired respiratory health in children. Maternal consumption of some antioxidant-rich foods such as fruit and vegetables or chocolate have also been associated with a lower risk of asthma in children with severe atopic dermatitis.(Reference Milewska-Wróbel and Lis-Święty49)
Energy-adjusted dietary inflammatory index
In our study, after adjustment for potential confounders, the inflammatory potential of the maternal diet was associated with an increased risk of belonging to the ‘asthma only’ cluster and marginally to the ‘early wheeze without asthma’ cluster. In a recent study, Venter et al. reported a positive association between the maternal DII score and the risk of asthma or wheeze at the age of 4 years, which was attenuated after adjustment, consistently with our results.(Reference Venter, Palumbo and Sauder23) In a meta-analysis of seven European birth cohorts, a higher maternal E-DII score was not associated with preschool wheeze or school-age asthma but was associated with a poorer forced vital capacity.(Reference Mensink-Bout, van Meel and de Jongste24) Hanson et al. also reported an association between the highest quartile of maternal DII score with poorer lung function in children, plus an association with an increased risk of an early wheeze trajectory between 1 and 9 years.(Reference Hanson, Rifas-Shiman and Shivappa22) Another study found that a higher E-DII score in the first trimester was associated with higher risk of asthma over the first 10 years of life.(Reference Chen, Lyons and Navarro21) A recent study found no association between the maternal DII and wheeze or eczema in the first year of life.(Reference Sivula, Puharinen and Hantunen25) Although there are some discrepancies, a pro-inflammatory diet during pregnancy has generally been associated with poorer respiratory health of the offspring, but no associations were reported with allergies, consistently with our results. In our cohort, as children were younger than 6 years old, the potential effects on lung function could not be investigated.
Asthma and allergy aetiology is particularly complex. Evidence suggests that neonatal programming of the immune system is influenced by environmental exposures,(Reference Campbell, Boyle and Thornton50) including maternal inflammation, that leading to impaired fetal immune system regulation or lung inflammation, which could make children more susceptible to develop allergies or asthma later in life.(Reference Krusche, Basse and Schaub51,Reference Lebold, Jacoby and Drake52) High consumption of antioxidants or anti-inflammatory compounds during pregnancy may decrease maternal oxidative stress, ensuring proper development of the fetal immune system and epithelium in the respiratory tract.(Reference Morales, García-Serna and Larqué53)
Strengths and limitations
Our study was conducted in the large nationwide ELFE birth cohort, giving our study several strengths, such as the possibility to adjust for multiple potential confounders selected with a directed acyclic graph, although residual confusion could not be excluded. Perinatal parameters such as the mode of delivery, breast-feeding duration and late introduction of food allergens may influence the risk of developing allergic and respiratory diseases. They have not been considered as potential confounders in our models, as they were posterior to the exposure. Our results remained similar after further adjustment for these factors (data not shown). However, the general population included in our analyses had a higher economic status than the general French population, but the calculation of weights corrected for attrition and non-participation and weighted analyses suggested that potential selection bias had little influence on our findings.
We used two complementary approaches to assess dietary maternal antioxidant and inflammatory potential, as the scores used consider food at different scales (food groups for DTAC and nutrients for E-DII), with different methods (one reflecting the literature and the other based on in vitro measurements), and their correlation coefficient is moderately high (Pearson, all |r| < 0·64, online Supplementary Table S2). For the DTAC, different versions were constructed as recommended in the literature to ensure robustness to differences in the estimation of the antioxidant capacity according to the in vitro method carried out.(Reference Serafini, Villano and Spera32) However, the DTAC construction includes the antioxidant potential of plant-based foods and beverages, without accounting for the oxidative potential of the diet. Studies including the balance between the oxidant and antioxidant potential of the diet, based both on plant-based and animal-based foods, may help confirm our results. For the E-DII, the construction followed the method developed by Shivappa et al.,(Reference Shivappa, Steck and Hurley20) except the standardisation of food intakes was made based on our own sample to be more representative of French pregnant women. In addition, as the FFQ was not specifically designed to measure the inflammatory potential, not all food components of the score were available in our study: 28 out of 45 were included, and some food components with a particularly high anti-inflammatory potential were missing (polyphenols, spices and condiments), which may explain the weak association observed, even though most studies did not include more food components in the literature.(Reference Chen, Lyons and Navarro21–Reference Mensink-Bout, van Meel and de Jongste24) Moreover, the E-DII score only reflects food intakes, and supplementation was not considered. Finally, the FFQ only covers the last 3 months of pregnancy, limiting recall bias; thus, our dietary scores reflect the maternal diet during late pregnancy and may not be representative of early or mid-pregnancy.
Our study is the first investigating the role of the total antioxidant capacity and of the pro-inflammatory potential of the maternal diet in relation with child respiratory and non-respiratory allergic disorders such as rash, food allergy, allergic conjunctivitis and rhinitis. We accounted for the interrelation and frequent concomitance of allergic and respiratory disorders in children by considering them together with multimorbidity clusters, which include most common allergic and respiratory disorders. As these respiratory multimorbidity clusters and our food scores were based on questionnaires, misclassification bias cannot be excluded, even if considering allergic and respiratory symptoms together helps to characterise phenotypes.
Conclusion
In this large French birth cohort, the antioxidant capacity of the maternal diet was associated with a lower risk of early wheeze without asthma in children up to 5·5 years. The pro-inflammatory potential of the maternal diet in late pregnancy was associated with poorer respiratory health in children. The associations reported are weak, suggesting the multifactorial origins of allergic and respiratory diseases. These results must be verified by other studies, to confirm that the maternal dietary antioxidant capacity may be a strategy to help reduce the important burden of respiratory disorders in childhood.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114524002642
Acknowledgements
The authors are grateful to scientific coordinators (B Geay, H Léridon, C Bois, MN Dufourg, JL Lanoé, X Thierry and C Zaros), the Respiratory Group (MC Delmas, A Deschildre, JC Dubus, MN Dufourg, B Leynaert, C Marguet, L Millon and C Raherison-Semjen), IT and data managers, statisticians (T Simeon, A Candea and S de Visme), administrative and family communication staff, study technicians (C Guevel, M Zoubiri, G Meyer, I Milan and R Popa) of the ELFE coordination team, as well as the families that gave their time for the study.
Part of this study was included in the InfaDiet project, funded by a grant from the French National Research Agency (ANR-19-CE36-0008). The ELFE survey is a joint project between the French Institute for Demographic Studies (INED) and the National Institute of Health and Medical Research (INSERM), in partnership with the French blood transfusion service (Etablissement français du sang, EFS), Santé publique France, the National Institute for Statistics and Economic Studies (INSEE), the Direction générale de la santé (DGS, part of the Ministry of Health and Social Affairs), the Direction générale de la prévention des risques (DGPR, Ministry for the Environment), the Direction de la recherche, des études, de l’évaluation et des statistiques (DREES, Ministry of Health and Social Affairs), the Département des études, de la prospective et des statistiques (DEPS, Ministry of Culture) and the Caisse nationale des allocations familiales (CNAF), with the support of the Ministry of Higher Education and Research and the Institut national de la jeunesse et de l’éducation populaire (INJEP). Via the RECONAI platform, it receives a government grant managed by the National Research Agency under the ‘Investissements d’avenir’ programme (ANR-11-EQPX-0038 and ANR-19-COHO-0001).
R. D., R. V., B. L. G. and A. B. contributed to the conception and design of the study. M. A. C., M. N. D., C. R., K. A. P., A. D. C. and B. L. G. participated in acquisition of data. R. D., R. V., B. L. G. and A. B. conducted the analyses and interpretation of data. R. D., R. V., B. L. G. and A. B. wrote the draft of the article. R. D., C. D., M. A. C., K. A. P., A. D. C., M. N. D., B. L., C. R., R. V., B. L. G. and A. B. revised the draft critically for important intellectual content and gave final approval of the version to be published.
R. Delvert has nothing to disclose. M.A. Charles has nothing to disclose. K. Adel-Patient received support from the Fondation pour la Recherche Médicale outside the present project. She is also an expert for the Human Nutrition Committee from the French public agency ANSES. A. Divaret-Chauveau, outside of the submitted work, reports grants from the French public agency ANSES, Don du Souffle, Novartis, ARAIRLOR, consulting fees for Sanofi, Stallergens, ALK, Aimmune Therapeutics, payment for presentations for Aimmune Therapeutics, Novartis, ALK, support for attending meetings from Mead Johnson, Nutricia, Aimmune Therapeutics, Novartis, ALK, stocks from Essilor Luxottica. M.N. Dufourg has nothing to disclose. B. Leynaert has nothing to disclose. C. Raherison, outside of the submitted work, reports contracts from Sanofi, payment for presentations from Novartis, AstraZeneka, GSK, support for attending meetings from Sanofi, AstraZeneca, Sanofi, participation on Advisory Board of Sanofi. R. Varraso has nothing to disclose. B. de Lauzon-Guillain received support for this manuscript from the French National Research Agency and, outside the present projet, grants from the Fondation pour la Recherche Médicale. She is also an expert for the Human Nutrition Committee from the French public agency ANSES. A. Bédard has nothing to disclose.
Data availability
Data described in the manuscript, code book and analytic code will not be made available because this study includes a substantial number of variables that, together, could be used to re-identify the participants based on a few key characteristics and then be used to have access to other personal data. Therefore, the French ethics authority strictly forbids making these data freely available. However, they can be obtained upon request to the ELFE principal investigator of ELFE. Readers may contact marie-aline.charles@inserm.fr for data requests. The analytic code will be made available.









