Impact statement
Due to the direct or indirect effects of the surroundings, delinquents are globally impacted by mental health difficulties. One global trend is increased aberrant behaviour caused by conflicts and other situations. As a result, mental health conditions, including posttraumatic stress disorder (PTSD), anxiety and depression, are increasingly prevalent. There are considerable long-term effects of poor mental health on deviant youngsters – those confined to institutions for rehabilitation and mental health needs. There is a significant difference between delinquency and the availability of mental health services (MHS). The vast global mental health treatment gap may be effectively addressed by integrating MHS into correctional settings. Offenders often get assistance from these activities and may be able to attend institutional and community-based therapy based on cognitive behaviour modification. Raising awareness and implementing community-based solutions may significantly lessen stigma, a lack of trust and the fear of unfavourable results. Governments, NGOs and other institutions can use individual, group and other platforms to satisfy juvenile offenders’ mental health needs. Notwithstanding the likelihood that these actions could benefit children, caution should be used when putting them into practice since they have not been tried in the real world.
Introduction
The statement is well known across the globe that Kashmir is a paradise on the earth due to its exceptional natural beauty, climate and geographical location (Malik et al., Reference Malik, Rashid, Ganie, Khuroo and Dar2015). J&K was a princely state (Hussain, Reference Hussain2021). Maharaja Hari Singh, the princely ruler, was granted permission to join India and Pakistan as independent nations in 1947. He was first apprehensive about joining India (Mohan, Reference Mohan1992; Farrell, Reference Farrell2002). He put off making a decision on Britain leaving the Indian subcontinent. However, he could not defend his princely kingdom from foreign invasion when the tribes from Pakistan’s northwestern areas attacked J&K. He ultimately asked the Indian government to provide the requisite military help (Jamwal, Reference Jamwal1998; Singh, Reference Singh2017; Snedden, Reference Snedden2021). India first ensured that until and unless the princely state formally acceded to India, it would be impossible to provide any military assistance (Abdullah, Reference Abdullah1964; Nawaz, Reference Nawaz2008). Under this condition, Maharaja Hari Singh signed the Instrument of Accession on 26 October 1947 (Rasool, Reference Rasool2014; Nath, Reference Nath2016; Paswal et al., Reference Paswal, Jafri and Fatima2020). India offered its armed support, and two-thirds of the princely J&K states were liberated from the tribals of Pakistan (Mangrio, Reference Mangrio2012; Kiss, Reference Kiss2013). These disputes led to the country’s 1965, 1971 and 1999 wars (Iqbal and Hussain, Reference Iqbal and Hussain2018). After that, in 1987, one political party was not happy with the election results, which produced a sense of resistance among the population, which termed into an armed struggle supported by Pakistan (Parlow, Reference Parlow2012; Majid, Reference Majid2018). Children in that armed conflict experienced both direct and indirect consequences of violence, such as unlawful recruitment into militant groups (Shah, Reference Shah2020), killings, gender-based violence (Kumar, Reference Kumar2016), illegal detentions (Ghosh, Reference Ghosh2020) and indirect impacts such as lack of access to essential services (Dhamija, Reference Dhamija2017). The trend remains, but after the 2008 agitation, the patterns of stone pelting increased (Guroo et al., Reference Guroo, Asif Ali Naikoo Guroo and Naikoo2018). The period between 2008 and 2016 was the victim of intensive protests in Kashmir; especially these protests were started from Amarnath Land Row, and a large number of protesters involved in street protests and stone pelting (Tremblay, Reference Tremblay2009; Parthasarathy, Reference Parthasarathy2020), and Burhan Wani militant commander was killed in 2016, which also led to severe agitation (Dhamija, Reference Dhamija2017). The role of the teenagers in the protest was vital due to the lack of opportunities, employment and critical economic conditions. In other ways, we can say it was the way to diffuse their frustration (Akmali, Reference Akmali2022). However, during the stone pelting and protests, physical injuries from bullets and tear gas shells peaked (Wei et al., Reference Wei, Ang, Nazir, Shah, Qureshi, Jain and Natarajan2022). On the other hand, the physical damages were recoverable, but psychological complications were also there, like fear of arrest, night raids and torture. To generate psychological fear among the teenagers, the security forces opted for new ways; they arrested the children who were part of anti-government activities, detained them and kept them in the side army camp, where they would beat them, and their cries could be spread around through loudspeakers to create ear among the youth (The Wire Staff, 2019; Haq, Reference Haq2020). The study stated that the continuity of this violent cycle creates mental health disorders that can lead to depression, PTS, anxiety distress and other mental health complications. Direct episodes of torture may lead to persistent depressive and traumatic conditions (Hassan and Shafi, Reference Hassan and Shafi2013). Another study’s most recent findings revealed that police officers, local health professionals, social workers and other NGOs who offer MHS are seeing an increase in the cases of various psychiatric disorders. The report also mentions the Ganderbal district, where more than 80% of cases were mental health-related, and 80% of patients had psychiatric disorders or had indicators (Syed and Khan, Reference Syed and Khan2017). In Kashmir, depression (41%), anxiety (28%) and PTSD (19%) are quite common (Muntazar: Kashmir Mental Health Survey Report 2015). Nearly 99.7% of the youth have exposure to conflict, 95.5% experienced psychological trauma, 60% suffer from somatic issues and 91% seem to suffer psychiatric problems. There is a high prevalence of PTSD (49%) among children, especially in areas where the intensity of conflict is very high, and this is due to regular encounters and strong resistance from civilians (Bhat and Imtiaz, Reference Bhat and Imtiaz2017). A critical African-based study shows that there are many factors behind getting good services, but there exists deficiency both of awareness and social stigma linked to trust. Still, health service seekers negatively perceive them (Rose et al., Reference Rose, Belus, Hines, Barrie, Regenauer, Andersen and Magidson2022).
Killings and mental health
The above bar chart shows that children experience mental distress when a loved one is killed. However, it has been observed that teenagers in Kashmir experienced mental health concerns during the 1990s owing to killings. The killing of friends during an encounter has been related to psychological issues among young people. The killings were higher between 1990 and 2007 than between 2008 and 2016 Figure 1. As a result, psychological issues were more common during both periods because the cycle of conflict continued, but between 2008 and 2016, injuries were high (Dar and Deb, Reference Dar and Deb2021).
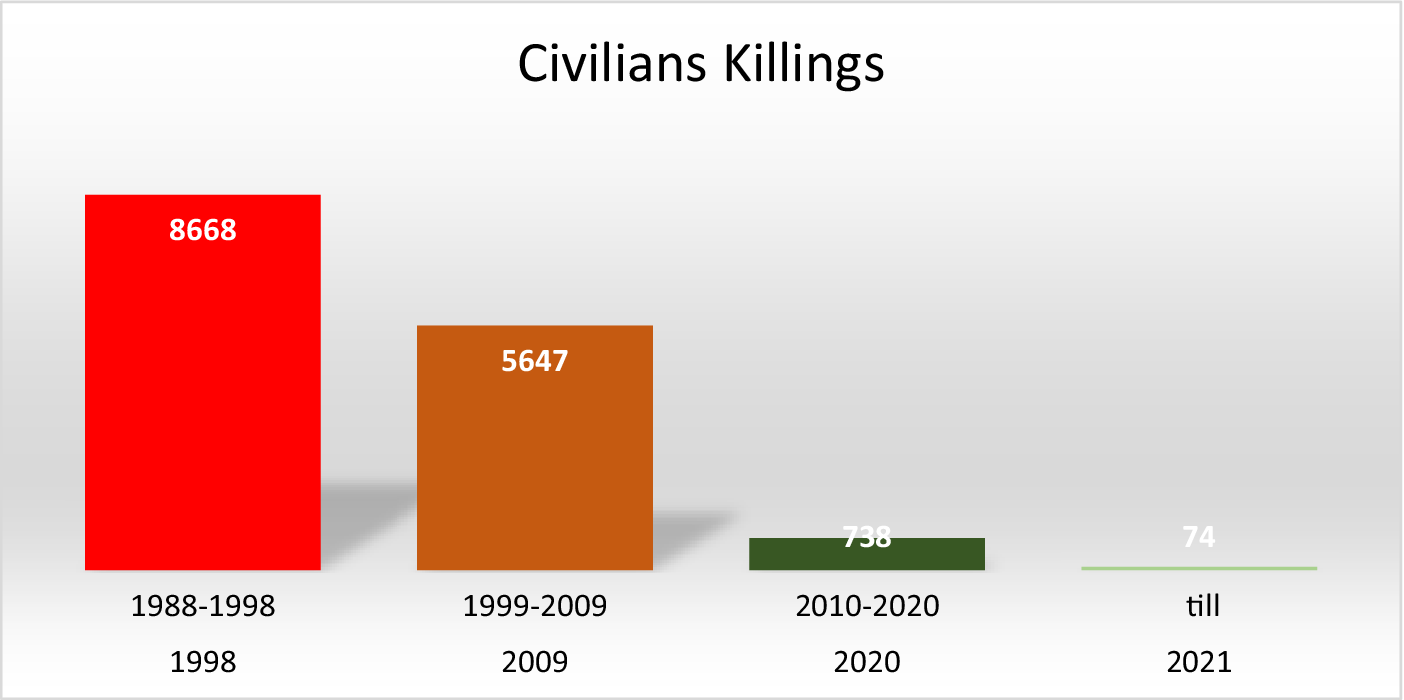
Figure 1. Civilian killings year wise in armed conflict. JKCCS, APDP and South Asia Terrorism Portal and Annual Report 2004–2005 (MHA-GOI).
Injuries and mental health
On the other hand, it has been observed that in the Kashmir region, the injured youth constantly lived in fear of being arrested; therefore, out of that worry, they choose not to go to a hospital for treatment. After 2008, the tendency was anticipated. As a result, many young people were experiencing mental health problems (Amin and Khan, Reference Amin and Khan2009). It has been observed that young people continue to experience phobias (Dar & Deb, Reference Dhamija2021). It was discovered that the injuries that occurred between 2008 and 2016 were specifically related to psychological conditions. In Kashmir, persons with severe injuries are more likely to have mental illnesses (Hussain et al., Reference Hussain, Dar, Qadri and Fatima2017; Dar and Deb, Reference Dar and Deb2021). Figure 2.

Figure 2. Injuries. JKCCS, APDP and South Asia Terrorism Portal.
Physical, mental torture, sexual and verbal torture and conflict
Conflict in Kashmir and torture are inextricably linked (Barad., 2020). Physical, mental, sexual and verbal torture always remain unnoticed (Qutab, Reference Qutab2012), but it peaked in 1990 as per data in the bar graph (Petersen and Wandall, Reference Petersen and Wandall1995). However, the trend declined in 2017 in Kashmir (Lalwani and Gayner, Reference Lalwani and Gayner2020). Figure 3.

Figure 3. Physical, mental torture, sexual and verbal torture. JKCCS, APDP and South Asia Terrorism Portal.
Overall, mental health has been equally impacted by all factors. However, during the 1990s insurgency’s early stages, the general worry of the community was felt, and direct mental illness later began to afflict people (Naik, Reference Naik2016). Until 2000, killings enhanced mental health problems among the population (Dar and Deb, Reference Dar and Deb2021). Even still, they were frequently injured during the subsequent street protests, and the killing of local militants contributed to widespread emotional damage among the population (Ul Hassan et al., Reference Ul Hassan, Sekar and Raj2017). Additionally, between the 2008 and 2016 protests, torture is not publicly acknowledged (Naik, Reference Naik2015; Deol and Ganai, Reference Deol and Ganai2018).
The existing system of child protection
J&K Juvenile Justice (Care and Protection of Children) Act 2013
The J&K Juvenile Justice (Care) Act (J&K JJ Act) is an act that the state passed to codify and amend the law relating to juveniles in conflict with the law, to children in need of care and protection and to juveniles in need of proper care, protection and treatment to meet their developmental needs, for the adjudication and disposition of matters in the best interest of the children and for their utmost restoration (J&K JJ Act 2013). According to the J&K JJ Act 2013, children below 18 years of age have been involved in many offences (Feierman and Shah, Reference Feierman and Shah2007). There is still a chance that minors who committed less severe crimes might be apprehended, and the police have the authority to determine whether doing so would be in the juvenile’s best interest (Qadir, Reference Qadir2022). The JJ Act is poorly recognised or adequately implemented, leading to many juveniles engaging in activities that violate the law (Shah and Policy, Reference Shah and Policy2019). While the J&K administration has introduced and passed punitive rules like the Armed Forces Special Powers Act (AFSPA) and Public Safety Act (PSA), it has little regard for juvenile justice or legal protection of minors. The security services flout all juvenile justice norms while unlawfully detaining, assaulting and benefitting from these despicable actions (Gupta, Reference Gupta2021). Children are implicated in an offence, and police abduct them rather than turning them over to Juvenile Justice Board (JJB) and giving custody to a stranger, putting the child at risk of being tortured, sexually abused and imprisoned (Qadir, Reference Qadir2021). On the other hand, parents of minors have limited access to meet. In case of an emergency, they can meet. In addition, the mobility of the juveniles is restricted only within the OH; the official always keeps them watching.
Implementation
J&K have limited correctional homes, one each in Srinagar and Jammu (Ministry of Women and Child Development, 2019). However, both correctional houses need proper infrastructure suitable for such children as counselling facilities. In addition, the staff lack skills and training (Bhat and Mir, Reference Bhat and Mir2016; Shah, Reference Shah2020). A thorough execution of the J&K JJ Act 2013 and the Regulations of 2014 was sought in the petition Tanvi Ahuja v. State of J&K. The PIL stated that the state had not established a Child Welfare Committee (CWC) or JJB. The case determined CWC and JJB in the state in response to the petition. The state had never followed the JJ Act of 2015 requirements. India abolished its prior juvenile law to implement the requirements of the UNCRC into its national legislation and to protect children’s rights (Bajpai, Reference Bajpai2018). It enacted the Juvenile Justice (Care and Protection of Children) Act in 2000 (Mehta, 2008). In addition to offering a regulatory structure for adolescents’ safeguarding, management and reintegration to meet their cognitive concerns, this Act calls for an exceptional approach to avoiding and curing delinquent behaviour. In deciding cases involving youth violence, it adheres to the maxim of what is in the children’s best interests. The juvenile law was passed in India, but because of its unique legal connection, it did not apply to J&K (Muncie, Reference Muncie2008). Though it took a while, the J&K eventually passed a juvenile justice law distinctive from the JJA in India. In 1997, the state of J&K passed the JJA of India from the previous year, and it has been effective till 2013. The J&K approved the JJA that India enacted in 2000 in 2013. This demonstrates how seriously J&K takes adolescents (Shah, Reference Shah2020; Jasrotia and Sunandini, Reference Jasrotia and Sunandini2022).
Individual care plan
In the J&K JJ Act of 2013, there is no mention of an individual care plan, while the JJ Act of India 2015 discussed the individual care plan. The J&K JJ Act requires such certification of establishments working with children who need care or protection (J&K JJ Act of 2013). The JJ Act of 2015 emphasised individual care plans and required registration of all childcare facilities (JJ Act 2015). The national government abrogated Article 370 on 5 August 2019 (Chandrachud, Reference Chandrachud2019), and the Juvenile Justice (Care and Protection of Children) Act 2015 became applicable to J&K in 2021. There is optimism that minors will get more significant advantages which were not enlisted in the J&K JJ Act 2013. That national law will ensure that the individual care plan holistically makes child growth possible and teaches about the child’s past. Through direct child participation, they can discuss future objectives, emotional well-being, individual health, academic and entertainment needs. A thorough plan encompasses every person’s developmental, psychological and intellectual development (Shah, Reference Shah2020; Jasrotia and Sunandini, Reference Jasrotia and Sunandini2022).
Government initiatives for the youth
The individual care plan can include the children’s future goals and preferences. The Government of India has also developed numerous rehabilitation programmes for these youths (Aslam and Sudan, Reference Aslam and Sudan2021). Additionally, the army has launched multiple missions for Kashmiri youth, like Sahi Rasta initiative (Zade, Reference Zade2017; Dongare, Reference Dongare2022). The political process in J&K is inactive after the revocation of Article 370 (Khan, Reference Khan2021) because the LG Administration, Government of India, directly manages and oversees the entire process (Warikoo, Reference Warikoo2010).
Theoretical framework (the ecological model)
When examining the perception of MHS among minor offenders, it is crucial to consider their difficult living conditions, family history, support and neglect. These factors contribute to youngsters breaking the law and acting disrespectfully towards others (Repetti et al., Reference Repetti, Taylor and Seeman2002).
Microsystem
A pattern of actions, societal roles and interpersonal communication often occurs in the direct vicinity where the individual is enmeshed, referred to as the microsystem (Bronfenbrenner, Reference Bronfenbrenner1994). Frequent encounters between juvenile offenders, individuals and groups within society are closely related to their misbehaviour. The next part will focus on four elements closest to the particular teenager at the microsystem level: youth traits, family connections, friendship affiliations and school attachment. Adolescent features, including socio-demographic characteristics (such as gender and age) and psychological factors (such as the capacity to exercise self-control), have been demonstrated to influence the likelihood of delinquency (Vanniasinkam, Reference Vanniasinkam2010; Agha et al., Reference Agha, Khan, Rehman and Zarif2012; Khan, Reference Khan2021).
Gender
Most academic research in Kashmir, Palestine and Syria has proven that male adolescents are substantially more likely than females to engage in deviant acts (Farrington et al., Reference Farrington, Ttofi and Piquero2016; Slone et al., Reference Slone, Lavi, Ozer and Pollak2017; Bhat, Reference Bhat2019). There are apparent differences between male and female teenagers in Kashmir (Parashar, Reference Parashar2009; Shekhawat, Reference Shekhawat2014). Males were shown to be more prone than females to participate in stone pelting, natural aggressiveness, self-centred behaviour and aberrant behaviour, according to the study’s findings, and also likely to hold deviant opinions and have unsavoury associates (Adenwalla, Reference Adenwalla2006; Shah et al., Reference Snedden2019; Ganie, Reference Ganie2021; Hassan, Reference Hassan2022). Compared to their female counterparts, male adolescents were more traditional and likelier to engage in aberrant behaviour (Roy, Reference Roy2008; Clarke, Reference Clarke2011).
Age
Several research conducted in Kashmir has shown positive results on the age influence on teenage delinquent behaviour and mental health (Anjum and Varma, Reference Anjum and Varma2010; Bhat et al., Reference Bhat, Khan and Sahaf2017; Hassan, Reference Hassan2021). On the other hand, studies have observed a significant positive relationship between age and frequency of deviance. Western studies have proposed that the prevalence of juvenile offending follows an age–crime curve that rises rapidly during early adolescence, peaks in mid-late teenage years and steadily declines after that period (Grasmick et al., Reference Grasmick, Tittle, Bursik and Arneklev1993; Loeber et al., 2012; Gottfredson and Hirschi, Reference Gottfredson and Hirschi2022). According to most research, there is a clear correlation between early adolescence and increased aberrant behaviour and middle youth; however, this relationship weakens as children become young adolescents (Farrington, Reference Farrington1994; Farrington et al., Reference Farrington, Coid and West2009). However, in the context of Kashmir, similar trends have been observed (Elbakidze and Jin, Reference Elbakidze and Jin2015).
Self-control
According to J&K-based studies, self-control is a potent and accurate predictor of deviant and mental health issues (Ashiq, Reference Ashiq2015; Iqbal et al., Reference Iqbal, Janjua and Shams2020). Self-control is a steady interpersonal quality that may significantly reduce people’s urge to engage in some abnormal behaviour (Gottfredson et al., 1990). Research on 1,500 children has indicated that those who lack self-control are more likely to engage in offensive activities (Cutrín et al., Reference Cutrín, Gómez-Fraguela and Luengo2015). Moreover, other abnormal behaviours like snatching weapons (Kaura, Reference Kaura2017) and involvement in stone protests are a result of poor self-control (Kak, Reference Kak2010). Also, among youths in rural regions, a lack of self-control is strongly connected with interpersonal physiological aggressiveness (Var et al., Reference Var, Paul, Kumar and Shah2011; Fayaz, Reference Fayaz2019; Ganie, Reference Ganie2023). Low self-control linked to gang membership, violent behaviour (Naz et al., 2016), substance use, theft and crime among Jammu youth has been observed (Sharma et al., Reference Sharma, Kumar and Sharma2022).
Relationship with parents
Family had a significant influence on the lives of teenagers in J&K (Munshi et al., Reference Munshi, Iqbal, Rafique and Ahmad2008). Family history, support and neglect are crucial for their difficult living conditions (Repetti et al., Reference Repetti, Taylor and Seeman2002). A prolonged conflict between mother and father impacts children’s mental health for a long time because they have to stay with them for a long time; such action may affect them and cause developmental disorders (Vahedi et al., Reference Vahedi, Krug and Westrupp2019). A weaker bond between parents and children is associated with a greater propensity for delinquent behaviour (Hussain & Imtiyaz, Reference Hussain2016; Hussain, Reference Hussain and Imtiyaz2014). Another gender-based study on 640 Palestinian adolescents shows similar findings (Punamäki et al., Reference Punamäki, Qouta, Miller and El-Sarraj2011). Children who are not closely watched have a greater incidence of protest participation (Hussain et al., Reference Hussain, Dar, Qadri and Fatima2017). Children’s drive for independence and self-identity has been proven to make the controlling parenting style a source of conflict and miscommunication (Ayub et al., Reference Ayub, Poongan, Masood, Gul, Ali, Farrukh and Naeem2012). A study has examined how various family factors affected juvenile misbehaviour in J&K. Another study has indicated that teenagers of unemployed parents (Majeed et al., Reference Majeed, Dar, Kour and Shaban2020) display much greater rates of delinquency and violence because their parents lack parenting skills (Akhter et al., Reference Akhter, Hanif, Tariq and Atta2011). Similar findings affirm the concerns of an ineffective parenting style in J&K (Zhang et al., 1995; Amin, Reference Amin2011). Also, research has shown that difficult home situations with components like forceful parenthood, heated disagreements and parental abuse are favourable conditions for disruptive and delinquent behaviour (Fagan, Reference Fagan1995; Nisar et al., Reference Nisar, Ullah, Ali and Alam2015; Hussain et al., Reference Hussain, Dar, Qadri and Fatima2017).
Peer effect
In Kashmir, having delinquent friends is especially notable as a determinant of delinquency (Tremblay et al., Reference Tremblay, Masse, Vitaro and Dobkin1995). The loss of parental authority is a sign of shifting social patterns in teenagers’ life, from family bonds to peer interactions, due to ongoing conflict and frequent changes in recent decades (Malik and Bhat, Reference Malik and Bhat2022). Peer groups are a significant source and reinforcer of violent behaviour in adolescents (Ingram et al., Reference Ingram, Patchin, Huebner, McCluskey and Bynum2007b, Reference Ingram2011; Ferguson and Meehan, Reference Ferguson and Meehan2011). Another research has shown that teenagers who view their closest friends as deviant are likelier to participate in delinquency (Rokven et al., Reference Rokven, de Boer, Tolsma and Ruiter2017), increasing their propensity to protest, stone pelting in Kashmir and delinquency in Jammu (Mathur, Reference Mathur2016; Khanna et al., Reference Khanna, Behl and Kaur2020). Neighbourhood, peers and exposure to various conflict-related factors affect children’s mental health (Jaggers et al., Reference Jaggers, Prattini and Church2016). They are owing to low academic performance and a lack of rapport between teachers and adolescents (Suri, Reference Suri2014; Malla, Reference Malla2019; Dar & Deb, Reference Dar and Deb2020).
Mesosystem
The growing human is contained inside each of two or more microsystems that make up the mesosystem (Bronfenbrenner, Reference Bronfenbrenner1994). Adolescents’ peer interactions and academic achievement may impact their parental relationship experiences. These connections can help explain how delinquent behaviour works. Researchers have noted that teenagers with poor parental connection and limited self-control are considerably more prone to use aberrant coping mechanisms when faced with stressful situations (DuBois et al., Reference DuBois, Eitel and Felner1994; Laursen and Collins, Reference Laursen and Collins2009; Ardelt, Reference Ardelt2010). On the other hand, adolescents who have disruptive peers exhibit more delinquent behaviour and less self-control (Hussain, Reference Hussain2012; Sharma and Marimuthu, Reference Sharma and Marimuthu2014; Azim, Reference Azim2019).
Exosystem
The exosystem, depicted as a surrounding scope encompassing the interconnections between various engagements or circumstances, is where the developing person is only actively engaged in one encounter or circumstance (Bronfenbrenner, Reference Bronfenbrenner1994).
Socioeconomic conditions
Socioeconomic disadvantage potentially contributes to increased delinquent involvement (Anjum & Verma, 2010; Rashid and Waddell, Reference Rashid and Waddell2019). A Kashmir-based study shows that economic constraints are significantly associated with minors’ substance abuse and delinquent behaviour (Dabla, Reference Dabla2012; Vishwakarma, Reference Vishwakarma2021). Findings depict that the absence of bread earners is significantly associated with delinquency and mental health problems (Sameena et al., Reference Sameena, Rauf, Tabish and Khan2016); parents going to work can lead to inadequate supervision of their children, contributing to the development of delinquent behaviour among the minors (Flanagan et al., Reference Flanagan, Auty and Farrington2019). Studies on adolescents confirm that family economic condition is directly proportional to the prevalence of delinquency in J&K (Van der Westhuizen and Swart, Reference Van der Westhuizen and Swart2015; Bhorat et al., Reference Bhorat, Thornton and Van der Zee2017). Several studies in Kashmir demonstrate that young people participate in numerous protests and terrorist activities due to their poor socioeconomic condition (Anjum & Verma, 2010; Narain, Reference Narain2016; Singh, Reference Singh2019).
Community
Children are embedded in the community; underprivileged circumstances might encourage delinquent behaviour and affect children’s mental health (Garbarino et al., Reference Garbarino, Kostelny and Dubrow1991; Boyd et al., Reference Boyd, Jones, Quinn, Gale, Williams and Lateef2022). In Kashmir, due to community-based violence and street protests (Ganie, Reference Ganie2023), another study has proved that contact with extremist groups, fear of raids and arrests foster more excellent deviant behaviours among minors (Dar et al., Reference Dar and Deb2020). Exposure to poor conditions like frequent protests, the impact of neighbourhood, encounters and participation in militants’ funerals are more likely to evoke psychological stress in adolescents, which in turn contributes to an increased likelihood of deviant behaviour in Kashmiri youth (Mushtaq, Reference Mushtaq2012; Dhamija, Reference Dhamija2017; Malik, Reference Malik2018). Neighbourhood impacts more; youths spend the most time within the community (Durlak and DuPre, Reference Durlak and DuPre2008). What kind of attitude does the community have? In other words, we can say that they are very much familiar with the environment of their community (Brooks-Gunn et al., Reference Brooks-Gunn, Duncan, Klebanov and Sealand1993). So, it is easy for them to abstract the particular condition. They can act comfortably (Johnson, Reference Johnson2005). In 2016 there were 65 gun-snatching incidents (Mohanty, Reference Mohanty2018).
Mental Health facilities
The studies on the mental health of children who conflict with the law need to be more concentrated (Teplin et al., Reference Teplin, Abram, McClelland, Dulcan and Mericle2002). There is, however, limited research on the treatment of young patients with psychiatric issues (Mushtaq and Fatima, Reference Mushtaq and Fatima2016). Multiple factors are responsible for the cause of various mental health disorders among children who conflict with the law; they require mental health attention, or they need MHS (Almanzar et al., Reference Almanzar, Katz and Harry2015) as it is well understood that mental health of the general population of Kashmir started to suffer after 1987 when resistance started against the government. Children, elders and women have experienced many traumatic incidents during the insurgency (Naik, Reference Naik2016). To ensure that suitable therapies are offered to such children (Henggeler et al., Reference Henggeler, Melton, Brondino, Scherer and Hanley1997), it is crucial to understand how juvenile offenders feel about the effectiveness of mental healthcare. OH officials offer mental health assistance to detained youngsters after bail or during detention (Swank and Gagnon, Reference Swank and Gagnon2016). However, evidence indicates that these services’ efficacy is dubious (Malla et al., Reference Malla, Margoob, Iyer, Joober, Lal, Thara and Mansouri2019). The inadequacy of services provided while juvenile delinquents are in OH is simply a forerunner to the ineffectiveness of various interventions once they return home (Zeola et al., Reference Zeola, Guina and Nahhas2017; Shah, Reference Shah2020). The strategies to cope with such kinds of mental disorders commonly adopted by the people in Kashmir are spiritual practices and other community-based approaches. In other words, not only the elders or adults are entitled to such techniques. The involvement of teenagers is also expected (Aqeel et al. Reference Aqeel, Rohail, Ahsan, Ahmed and Saad2017). This division of responsibilities between health and rehabilitative services, as well as the absence of intersectoral coordination in providing these services, can be associated with adverse effects for the discrepancy in the delivery of health and rehabilitation aids (Storm et al., Reference Storm, Fortuna, Gill, Pincus, Bruce and Bartels2020).
Macrosystem
The macrosystem level considers elements of the larger environment, including cultural values, way of life and opportunity structures that eventually impact the social structures and activities at the immediate system level (Bronfenbrenner, Reference Bronfenbrenner1994). In particular, where Kashmiri culture and religion are strong influences, boys and girls are treated differently throughout establishing gender roles (Parlow, Reference Parlow2011; Behera, Reference Behera2016; Gabel et al., Reference Gabel, Reichert and Reuter2022; Kazi, Reference Kazi2022; Nisar, Reference Nisar2023). Kashmir has a substantial gun culture which immediately affects the young (Tremblay, Reference Tremblay1996; Parashar, Reference Parashar2011). Many teenagers under the influence join various militant groups (Hilali, Reference Hilali1999; Oberoi, Reference Oberoi, Lamiaye, Satu, Wirsing and Malik2004; Ahmad and Hussain, Reference Ahmad and Hussain2011). However, when fighting with forces, many young individuals perish (Ahmad and Balamurgan, Reference Ahmad and Balamurgan2020). Due to strong religious feelings, many will refer to it as a sacrifice (Devadas, Reference Devadas2018). Often different militant organisations publicly exhibit their weapons (Whitehead, Reference Whitehead2022), directly affecting young people. Children can view it as a distinctive aspect of the culture. Their behaviour may be abnormal due to that culture (Jamwal, Reference Jamwal2003; Dorjay, Reference Dorjay2016; Shah and Policy, Reference Shah and Policy2019). According to numerous studies, there is a significant chance that children from families where delinquency has a history may grow up to be classified as delinquents (Egalite, Reference Egalite2016; Kaiper-Marquez et al., Reference Kaiper-Marquez, Stickel and Prins2021). Intense community shaming and reconciliation will likely cause labelled persons to feel humiliated once they are reintegrated into the community in such a collective society, which may drastically lower their identity. Such minors are more prone to deviance and susceptible to mental health concerns (Sharpe, Reference Sharpe2015; Stuewig et al., Reference Stuewig, Tangney, Kendall, Folk, Meyer and Dearing2015; Lageson, Reference Lageson2016; Schalkwijk et al., Reference Schalkwijk, Stams, Stegge, Dekker and Peen2016).
Mental health services, stigma and trust
Ample studies discuss the relationship between stigma and MHS among teenagers. Stigma is linked with the mentally ill, which could harm their growth, development, self-esteem, daily activities and seeking appropriate treatment (Hinshaw, Reference Hinshaw2005; Kaushik et al., Reference Kaushik, Kostaki and Kyriakopoulos2016). Trust in counsellors or those who assist MHS is widely ignored in the stigma studies (Gilburt et al., Reference Gilburt, Rose and Slade2008). The study of MHS has also paid little attention to trust (Brown et al., Reference Brown, Calnan, Scrivener and Szmukler2009; Gaebel et al., Reference Gaebel, Muijen, Baumann, Bhugra, Wasserman, Van der Gaag and Zielasek2014). However, if we talk about interpersonal relations between the service seeker and the service provider, trust plays a vital role (Terrell and Terrell, Reference Terrell and Terrell1984; Bucci et al., Reference Bucci, Seymour-Hyde, Harris and Berry2016). Because it is a matter between two individuals primarily, on the other hand, stigma may be from the social side as well as self-stigma. In addition, trust remains ignored in the MHS domain (Gilburt et al., Reference Gilburt, Rose and Slade2008). This is unexpected because the interaction between service providers and clients of MHS is thought to be the most crucial process (Brown and Calnan, Reference Brown and Calnan2013). A psychologist has established a concept called trust level theory. The efficiency of the systems as a result of how the processes interact is said to be determined mainly by trust level. According to Gibb, trust is an innate, unplanned emotion similar to passion (Gibb, 1997). However, factors include the trustworthiness of the healthcare providers’ patient-centeredness, the assurance that policies will not negatively impact individuals, the healthcare professionals’ skill, the care benchmark and the flexibility and coexistence of the services concerning spreading knowledge, accessibility, privacy and possible vulnerability (Blomqvist, Reference Blomqvist1997; Straten et al., Reference Straten, Friele and Groenewegen2002; Thompson et al., Reference Thompson, Hupcey and Clark2003; Shou et al., Reference Shou, Guo, Zhang and Su2011). The majority stress the optimistic acceptance of a vulnerable situation in which the truster believes the trustee will care for the truster’s interests (Hall et al., Reference Hall, Dugan, Zheng and Mishra2001, p. 615). A crucial component of trust is the belief in loyalty, competence, fairness, privacy and general reliance (Hall et al., Reference Hall, Dugan, Zheng and Mishra2001). On the other hand, we will talk about stigma and MHS; stigma is a significant obstacle behind MHS (self and public stigma) and enhancing mental health problems (Polaha et al., Reference Polaha, Williams, Heflinger and Studts2015). The study shows that children who conflict with the law experience stigma and a determined-to-trust deficit, making their mental health more pathetic (Naik, Reference Naik2016; Mir and Bueno de Mesquita, Reference Mir and Bueno de Mesquita2022). Though stigma is thought to prevent mental healthcare participants from rehabilitating, the exact intermediary procedures within MHS providers are still unknown (Mezey et al., Reference Mezey, Youngman, Kretzschmar and White2016). As engagement among individuals and professionals is a core component within MHS and trust is viewed as a central aspect of this communication, trust may be considered a relatively essential intermediate factor connecting stigma to the effects of MHS (Walsh et al., Reference Walsh, Scaife, Notley, Dodsworth and Schofield2011).
Conceptual framework
Individual-level variables cannot fully explain adolescent behaviour (Loeber and Farrington, Reference Loeber and Farrington2000; Anderson et al., Reference Anderson, Cesur and Tekin2015) because communities defined by geography (Shannon et al., Reference Shannon, Hankins, Shelton, Bosse, Scott, Block and Nicolas2021) and conflict (Yule et al., Reference Yule, Stuvland, Baingana and Smith2003; Slone and Shoshani, Reference Slone and Shoshani2022), and groups determined by gender, school and income, appear to exhibit consistent, non-random patterns of teenage problem behaviours (Loeber and Farrington, Reference Loeber and Farrington2000; Anderson et al., Reference Anderson, Cesur and Tekin2015), parent’s profession in the earlier research (Chang et al., Reference Chang, Wang and Tsai2016). Several studies have shown that a child’s environment may function as a potential cause or a shield against delinquency (Ferrell, Reference Ferrell1997; Nation et al., Reference Nation, Crusto, Wandersman, Kumpfer, Seybolt, Morrissey-Kane and Davino2003), mental health (Betancourt and Khan, Reference Betancourt and Khan2008; Williams and Thompson, Reference Williams and Thompson2011) and behaviour issues (Margoob et al., Reference Margoob, Rather, Khan, Singh, Malik, Firdosi and Ahmad2006; Thabet et al., Reference Thabet, Karim and Vostanis2006; Ayub et al., Reference Ayub, Poongan, Masood, Gul, Ali, Farrukh and Naeem2012). Consequently, we constructed an integrated model that accounts for the influences of microsystems, mesosystems, exosystems and macrosystems on adolescents. They may experience various psychological issues due to the environment, which may indirectly or directly contribute to the development of deviant behaviour (Lambie and Randell, Reference Lambie and Randell2013). Afterwards, these minors moved to correctional settings. They could be hesitant to use mental health treatments because of stigma and mistrust, as depicted in Figure 4. We came up with hypotheses regarding the stigma associated with MHS. In particular, the latter model hypothesises that aberrant youths need more faith in guidance counsellors and, despite this, in OH staff members. Children reportedly feared confidentiality would be violated since the visiting counsellor might tell JJB or other officials everything.

Figure 4. Conceptual framework. The framework aims to explain how ecosystems can affect children from a micro to a macro level since they interact directly and indirectly. Suppose an issue arises, for instance, at the macro or family level, both circumstances have the potential to influence how minors behave. As a result, individuals can develop mental health issues or act inappropriately.
Objectives and rationale of the study
Objectives
-
1. To learn about the socioeconomic situation of the children who are in conflict with the law in J&K.
-
2. To understand the stigma associated with children who are in conflict with law and are housed in correctional settings.
-
3. To understand the fear of unforeseen repercussions among juvenile delinquents in J&K.
-
4. To understand the trust in service providers among the children who are in conflict with the law.
Rationale of the study
The rationale behind choosing this particular area is because it has yet to be given much attention (Noor and Llah, Reference Noor and Llah2015; Bhat et al., Reference Bhat, Singh, Surmal, Singh, Shivgotra and Musarella2021). However, the prevalence of mental disorders among delinquents is high in Kashmir (Hassan, Reference Hassan2021). Nonetheless, Kashmir has a high rate of mental illness among offenders (Goldstein et al., Reference Goldstein, Olubadewo, Redding and Lexcen2005; Housen et al., Reference Housen, Lenglet, Ariti, Shah, Shah, Ara and Pintaldi2017; Paul and Khan, Reference Paul and Khan2019). The researcher has discovered through literature review that specific issues of young people who were in trouble with the law and had spent time in correctional homes in J&K are not extensively documented. The lack of study and effective intervention in this area leaves juvenile mental health issues exposed and stigmatised for a very long period. It should be mentioned that the social welfare authorities, academic planners, healthcare authorities and social workers are unaware of the psychological concerns that offensive children experience due to a lack of appropriate and reasonable engagement with the issues. As a result, individuals are unable to manage their problems consistently. This study recognises this as a significant societal issue in J&K and tries to provide practical, participant-friendly solutions for the target group in correctional settings. This proposition would benefit policymakers, government representatives, ICPS (Mission Vatsalya), social welfare administrators, psychologists and social workers to put new guidelines and plans into action for the welfare of delinquents.
Operational definitions of anti-social activities
-
1. In this study, anti-social activity is a disturbance in the social order through noisy protests and disruption of day-to-day activities. Protest leads to closing all business activities (Bhat, Reference Bhat2019; Hassan, Reference Hassan2022).
-
2. Anti-social activities are actions taken by an individual or a group that violate social laws and ethical standards.
-
3. The term “anti-social activities” describes a collection of actions that may undermine the regular function of life and affect essential community service delivery.
Method
Study design
The study aimed to examine adolescents’ perceptions of mental healthcare. Due to interviews producing open-ended replies, this research used a qualitative methodology, and the sample size was restricted to 15 individuals. The study permitted a comprehensive face-to-face examination and analysis. There was no defined standard instrument. Thus, questions were focused on the literature’s primary topics. The researchers expected that participants’ replies would indicate that using MHS carries a stigma, such as being seen as weak by peers. Moreover, authorities may see these youngsters as weak. It was also suggested that delinquents might fear unforeseen repercussions while reporting the need for mental health assistance, such as losing their candidacy for school enrolment or missing employment opportunities. These adolescents may also be seen as fragile by both authorities and peers. In addition, the study hypothesised that youngsters in legal peril do not trust counsellors or OH authorities. As the counsellor is also accountable to the JJB, there is a concern that confidentiality may be compromised.
Sampling
Srinagar and Jammu districts have the highest number of delinquents in J&K (Hassan, Reference Hassan2022; Jasrotia and Sunandini, Reference Jasrotia and Sunandini2022). However, 15 youngsters were picked using the snowball sampling method from the districts of Srinagar (eight) in the Kashmir division and Jammu (seven) in the Jammu division. The participants were between 10 and 18 years old. The adolescent must have spent at least three months in a correctional facility, and all participants were bailed out.
Data collection
Before the interview, participants’ demographic information was gathered via a questionnaire. The demographic questionnaire covered age, educational level, family profession, family status (APL or BPL), parent education and participation in delinquent behaviours. All demographic questionnaire items were close-ended, and participants had 10 min to respond. The questions for the interview were open-ended. In addition, it was anticipated that this study would inspire more research into establishing guidelines for such juvenile delinquents. Before conducting the interviews, the researchers provided a debriefing to describe the purpose of the study and evaluated the eligibility of the children to be interviewed. The aberrant youngsters signed a permission form.
Procedures
The participants were individually questioned. Researchers made use of field notes. For the participant, the interview lasted 30 min at maximum. In some cases, it reached 45 min. A separate setting was chosen for the interview to ensure the participants’ comfort during the procedure.
Data analysis
Thematic analysis, which is open-ended, dynamic and can provide additional insight, led the data analysis to further our knowledge of how children form their opinions of MHS (Bloomberg, Reference Bloomberg2012). Getting familiar with the participant data involved transcribing, reading and rereading the transcriptions, making notes and creating emergent themes by systematic coding of interesting features across the entire data set, compiling information pertinent to each code, looking for themes by organising codes into potential themes and collecting information pertinent to each prospective theme (Booysen et al., Reference Booysen, Mahe-Poyo and Grant2021). Ultimately, data analysis and drafting of the findings have been through an iterative procedure, with the authors debating and commenting on the data analysis (Bloomberg, Reference Bloomberg2012; Gergen and Gergen, Reference Gergen, Gergen, Reason and Bradbury2008).
Results
A review of issues found while analysing the data will subsequently happen – exposition of the 15 children involved in aberrant activities like stone pelting, robbery, rape and murder.
Parents’ education
Regarding parental education, four fathers were educated up to the 10th grade. Six fathers have less than a 10th-grade education; three fathers never went for studies; two parents attended college. Eight of the mothers had education levels below the tenth grade. Seven did not go to school.
Socioeconomic status
Few respondents self-identified as below the poverty line (BPL), despite most respondents’ socioeconomic status falling into this category. Teenage delinquency and income seem to be related in some way (Hassan et al., Reference Hassan, Adindu and Cyril2020). Notably, just one parent worked in the public sector, and 13 were labourers. The majority of fathers and mothers were lower-class income earners. The majority of lower-income households reported making do with their little incomes. One delinquent was an orphan, whose father had died (Table 1).
Table 1. Demographic profile of the respondents

Note: Males aged 10 to 18 were enrolled in the average 8th to 12th grade. Nine respondents identified as Muslims, eight from Srinagar and one from Jammu, while the remaining identified as Hindus from Jammu. Eight individuals who participated in stone pelting were from Srinagar, while others committed offences from Jammu.
Offence repatriation frequency
According to the respondents’ revealed information on the frequency of offence recurrence, one respondent committed a crime seven times, two minors committed a crime three times and four others engaged in aberrant behaviour four times. Also, five children engaged in offensive conduct twice (Table 2).
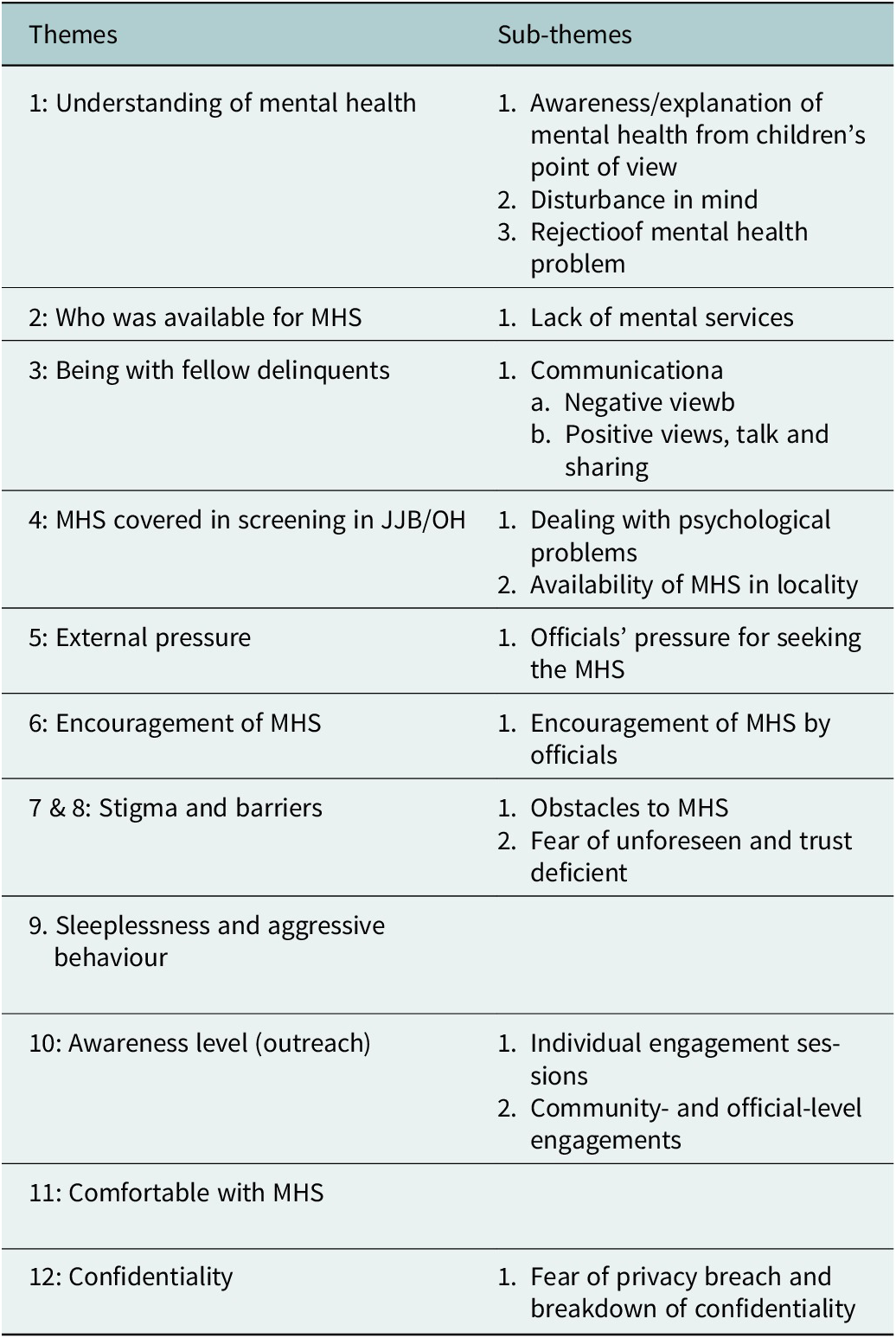
Table 2. Themes
Theme 1: Understanding of mental health
Sub-theme: Awareness/explanation of mental health from children’s point of view
The concept of mental health was seen differently by children. Others characterised mental health differently, dismissing any issues and offering a medical explanation for their symptoms instead.
-
1. “When someone is disturbed, they are said to be mental.”
-
2. “I believe that before becoming insane [Pagal Panthi], I was quite aware; my brain was blocked.”
Sub-theme: Disturbance of mind and rejection of mental health problem
Despite their linguistic barriers, several respondents could link explicitly “disturbed” with their mental health. These statements were fairly lucid and would be understandable. Although some children could express their issues plainly, others did it in a more ethereal manner. This may have resulted from simple language difficulties or represent specific regional viewpoints. They could interpret their experiences and show profound understanding by attributing the situation to the brain. Even when specifically questioned, several children denied having mental health issues These individuals tended to attribute the reason to somatic symptoms.
-
3 “Respondent claims that even though I have a headache and sore eyes, I am not ill. It’s very typical among the others.”
-
4 “I don’t suffer from any mental illnesses. I recognise the spooky dream. Sometimes, I skipped sleep.”
These responders describe their mental state in various ways. For instance, several respondents blamed their health issues on particular physical rather than disturbance of the mind. As the interviewer pressed for further information, he was sure he had no mental health issues. The responder shared this rejection of mental health issues.
-
5 “I’m not a mental problem.”
-
6 “I refuse to go to the counsellor to be among the mentally ill children.”
Even after admitting mental health issues, individuals continued to have unfavourable opinions on their own and others’ psychological health. It is common for young individuals to discuss mental health negatively (Oral et al., Reference Oral, Ramirez, Coohey, Nakada, Walz, Kuntz, Benoit and Peek-Asa2016).
Theme 2: Who was available for MHS
Sub-theme: Lack of MHS
Most of the respondents said no MHS were offered in the OH. Few stated they were told a counsellor was available to talk to them. One said, for example:
The office of the OH suggested that we consult the counsellor if we needed assistance, but I hardly saw any counsellor while in the OH. They mentioned that a counsellor has been on duty, and you might approach them for counsel if necessary. If you notice someone battling, see what you can do to encourage them to seek MHS. I attended a medical camp, but none of the psychiatric came there; I consulted with the psychiatrist with the help of my family. If we complain about our mental health problems, we must follow many steps during the consultation procedure.
Narrative of another teenager:
One of the participants shared that they did not provide direct services, but sometimes the official from the OH came and asked whether they required any help; you can ask us, but there was no explicit mention of MHS. If you are facing any problems, you can share them with us. Most of the time, they conducted medical camps, but no psychiatrist or counsellor. However, no one considered that we were distressed.
Who was accessible to the convicts about the connected MHS was the topic of the associated MHS. After analysis, we can say there was a lack of MHS.
Theme 3: Being with fellow delinquents
Sub-theme: Negative view regarding communication
“Why do I have to know anyone? Being alone is better since no one will give you support when things go difficult.”
“Since you’re not doing it in a group but are going to communicate to one individual alone, one must have communicated with them individually.”
In another interesting finding, a few respondents said they never talked to anyone about their offence.
Sub-theme: Positive view regarding communication
“It’s a great idea to talk to anyone, as one of the participants said, particularly with family and friends. It may help to resolve a tough problem.”
One respondent said that “talking to others is delightful, especially mates”.
“When you are there, you interact with your friends who are with you and just your friends. You truly don’t want to share your troubles with your family. Talk to everyone there who is experiencing it with you.”
Most minors felt more at ease speaking with others who understood their issues or had comparable experiences. Most importantly, most adolescents felt at ease communicating with peers inside the OH compared to the counsellor.
Theme 4: MHS covered in screening in JJB/OH
Sub-theme: How to deal with psychological problems
Very few stated that they were briefed about dealing with various psychological stressors while returning from the OH, but not profitably or professionally.
“Counsellor advised to play games, calm anger, talk to parents about difficulties, and not ponder too much before leaving OH.”
“They discussed facing your emotions rather than ignoring them, not ignoring problems, and the need to seek counselling or support from a mental health professional if you are struggling.”
“When I was sent there, I was anxious and afraid, but no one asked me about my condition.”
No professional counselling was given to the minors.
Sub-theme: Availability of MHS in locality
“Amm, I notice that there are no essential health services in my neighbourhood, and I’ve never heard of any MHS there. No doctor of for mind.”
“I never see a doctor for other diseases. To take treatment, our people go to the city. Doctor-related to mind is the secondary option.”
The rest said that officials asked that all services be accessible in your localities, and most responded similarly. The comments reveal insufficient screening for mental health problems. So no services were available in the neighbourhood.
Theme 5: External pressure
The external pressure encompasses staff members’ security, influencing juvenile delinquent’s mental health and seeking HMS.
Sub-theme: Officials’ pressure for seeking MHS
Most of the youngsters stated that they did not have such kind of pressure from the side of the officials, and officials were never very serious about MHS. Nearly half of the youngsters stated that the officials should have done something or taken the lead to enhance MHS. The rest of the children told that officials thought they were not serious if they felt they needed any benefits such as MHS.
One of the children stated that it is the responsibility of the children in the OH to push the officials to promote MHS. It needs an hour because most of us suffer from various kinds of stress and strain.
MH is not a non-topic of discussion with authorities. I’ve never actually talked about it with anyone else. I never really bothered discussing it, or nobody ever brought it up. We hardly seldom get together and discuss officials. Even if no one doesn’t care, there are situations when sharing information with them might have unexpected effects. We don’t think about that discussion much.
Children were not encouraging MHS after analysing the theme, although they sometimes needed to be urged more. Few believed that occasionally the government promoted MHS, but it was the responsibility of the children to avail them – no direct mention of pressure from the side of the OH staff.
Theme 6: Encouragement of MHS
Sub-theme: Encouragement of MHS by officials
“Particularly, authorities showed little concern about pains and made no effort to MHS. They request to take a pill, leave, and go to bed.”
“If we reveal everything, they’ve been pushing only the other things, ultimately affecting your future. Nobody is discussing mental health.”
“Somehow, when I was unhappy and in a bad attitude, authorities recommended that I visit a counsellor.”
“So, it’s like, not simply to speak to them because they don’t, they don’t listen as they listen, but they’re not hearing since the only thing they are looking to is, I don’t know, I honestly find it pointless talking to officials.”
The researcher found inconsistent responses from various staff members.
“Many don’t care, so yes, that’s the case.”
Some respondents believed that officials need more awareness of difficulties in OH. As such, they think they need to be better placed to support them adequately.
“These are youths with multiple problems that nobody else is conscious of since they believe they are okay and all that, but which must be dealt with because, you know.”
Maybe they would because they have not known, but they would not ask you questions if they see you in a bad state.
“Indeed, because they avoid discussing that particular psychological condition, they speak about how others make fun of them, but there must be other reasons to feel anxious.”
Some respondents felt unsupported in coping with issues because they believe others are prejudiced against offending actions.
Most respondents claimed no support for promoting MHS. Children claimed that although there was no promotion of MHS, we could communicate with other teenagers in the OH when things get difficult or stressful. We may enjoy conversing with others in any way. And if we communicate with one another, our chances of finding alleviation from this type of condition improve. However, most teenagers fear sharing their matters with others because they worry about their future, whether they will be accepted at a school or find jobs, and that their privacy would be violated. After analysing the theme, there needed to be more encouragement. Few felt that sometimes officials encourage MHS, but they feel it is up to the children to get them.
Themes 7 & 8: Stigma and barriers
Sub-theme: Obstacles to MHS
Children stated that they have to consult with a psychiatrist or counsellor to cope with a particular situation; with that, some children said no one can understand the actual problem of anyone. They have to deal with it themselves. Few of them were unaware of the obstacles to MHS.
From most respondents’ responses, it was found that there was a stigma attached, which was not openly acknowledged since they did not discuss their direct experiences.
For instance, one said: “Do not be encouraged; simply speak to someone if you need help. Do not let it increase. Just discuss it with someone like a friend. Everyone in the room was believed to have psychological issues or abnormalities. Just let someone know about it.”
Juveniles do not trust counsellors, so they are also comfortable sharing their problems with mates and unnoticed stigma.
“Because we are supposed to put up everything that goes along with being juvenile offenders, we thought we were weak if we went and spoke to someone about mental health.”
Self-stigmatisation: Low self-esteem and low confidence may stop them from seeking services.
The theme in this question dealt with stigma. Most of them fear of their career and did not want to see them as weak.
According to one respondent, children are outgoing, sincere and honest. He said, for instance:
I’m not sure. It doesn’t appear to be bad. Our correctional home inmates dealt with things in a rather transparent manner. Just be real and sincere. Now we’ll be able to see whether you’re stalling. One such man murdered his girlfriend after suffering a total mental collapse. We won’t hold him responsible. He’s not to blame. Another issue would arise if you claimed to have been traumatised while not seeing anything. No one should encounter any issues as long as you are being true and honest. The only thing I can think of is that.
Sub-theme: Fear of unforeseen repercussions and trust deficient
Fear
Due to responses that have led them to lose significant associations like close friends or even partners, most respondents preferred to refuse having mental illnesses. This behaviour may be prompted by fear of the condition.
I will tell you about my experience in the observation home. Several staff members tell us that we have nothing, and the people trying to assist us to get weary and hostile after dismissing you. I get the notion that others say, “There comes, everyone was biased, neglecting, since if he gets into a dilemma, he could abuse others.” That, I believe, has not been favourable for me.
Discrimination
Respondents stated that counselling them was as if they cannot cope except in rare cases. On the other hand, most of the children thought these unfavourable presumptions were connected to discriminatory actions.
Even if you are OK, there is no confidence. If officials will come to meet with the counsellor to inquire about a problem, I would prefer not to meet anyone and want to be silent and stay alone. They don’t think I’m real, which makes me feel awful. Because of it, they may share my details with other board members. What a coincidence I had a problem; later on, it may create more problems for my carrier.
Fear of unforeseen repercussions and trust deficient
“While I was in OH, few police officers never stopped saying I was criminal after all others said: ‘me that he is a criminal, he is the bad guy.”
A few individuals shared their experiences obtaining mental healthcare and the advantages they received. A lack of awareness about the kinds of support accessible to them and how to access those appeared to be an obstacle to receiving help, as did fear of being negatively judged and for lack of trust.
Theme 9: Sleeplessness and aggressive behaviour
Most indicated they could not cope with stress and anxiety, although they reported sleeping problems. Some of them narrated they repeated the offence. “We fear the arrest or JJB will send back to the OH. So, we have a fear, and we cannot sleep.”
“[In the OH] all children were in one room. It was just like a gaol, although we couldn’t sleep.”
Respondents stated they had less stress since returning from OH because they were with their families, and few of them got admission to the school. Most of them said they had difficulties with nightmares:
Unpleasant dreams had occurred due to anxiousness, although they occurred more when I initially returned home. Yet the overwhelming sense of anxiety kept me awake at night, and sometimes it only did so when I was reminded of what I had done. Hardly a day goes by that I don’t think about it or particular events that took place there, thus.
We fear arrest or the Juvenile Justice Board will send them back to the observation home. So, we have a fear, and we can’t sleep. With that, in the observation home, we don’t have any services related to games, and there is only one room; all children are in one room. It was just like a gaol.
Theme 10: Awareness level (outreach)
Sub-theme: Individual engagement sessions
Based on very few participants, one-on-one engagement sessions to initiate therapy would benefit those returning from OH. According to respondents.
“It will be preferable if the counsellor arranges individual counselling. One will feel more ease to discuss difficulties, which will assist with solving problems.”
“Yet, it could be challenging to get us to attend supportive relationships since we might claim that we don’t believe. So, additional initiatives must be undertaken to let know that counsellors are available.”
Others narrated that there is a lack of awareness regarding MHS and that if someone goes for MHS, he will be considered mentally ill. One child narrated as such:
“When anyone went for help related to mental health, most of the neighbours considered them pagal (mad). People will hesitate to talk; everyone will see with doubt and fear that he/she can harm us.”
Society as well as officials must have awareness related to mental disorders and MHS. Then it will be easy for teenagers to avail of MHS comfortably.
Once upon a time, I shared everything with a counsellor and all other officials related to my aberrant behaviour. After a few days, some other offices came to me and asked about my behaviour, so how can we trust them? We can only trust over parents and friends; at least we will be safe.
Sub-theme: Community- and official-level engagements
It was found that most respondents needed to be made aware of the MHS.
“Such services must be because they can help us understand the difference between reality and our actions.”
Still, with that, one of the respondents narrated: “Is ka kush nhi bn piye, is say dar lagta ha, jha pagal ha, is ka kush nhi ban sakta. Ise liye ma ghar say bhair nhi niklta hospital b nhi jata hou.”
“Pagal” word is ubiquitous in Indian societies for those with mental illnesses or psychological problems (Murthy et al., Reference Murthy, Dasgupta, Chaturvedi and Chaturvedi2020).
Theme 11: Comfortable with MHS
Most participants agreed that having one-on-one meetings to begin services would help them feel more at ease with MHS. One said, for instance:
It all comes down to the fact that I dislike psychiatry. I’m not sure I really get how it is with them. Someone telling me how I feel irritates me. I, too, find that group thing annoying. I don’t particularly appreciate talking to huge gatherings of people. I like speaking with a select group rather than many individuals.
However, respondents felt uncomfortable with group therapy but were more comfortable with individual therapy.
Theme 12: Confidentiality
Sub-theme: Fear of privacy breach and breakdown of confidentiality
More immediate access, yes. You don’t need to tell your mates that you’re simply going in to talk to someone. It would be useful. In my opinion, many inmates know that it should be kept private, but because you are still being watched, it is still there. I believe that this is a mental barrier that prevents them from speaking to someone.
Another respondent: “Well, I guess you would have to be with us to understand all this. Hard to talk with somebody that’s never been there.”
According to one respondent:
I’m not sure. It doesn’t appear to be bad. Our correctional home inmates dealt with things in a rather transparent manner. Just be real and sincere. One such of friend murdered his girlfriend after suffering a total mental. We won’t hold him responsible. He’s not to blame. Another issue would arise if you claimed to have been traumatised while not seeing anything. No one should encounter any issues as long as you are being true and honest. The only thing I can think of is that.
Others believed that everything would be OK if one were honest and trustworthy. Most of the respondents expressed concern that confidentiality would not be maintained. Delinquents feared that confidentiality would be violated.
“So, the staff and counsellor are utterly unfathomable to me.”
“As every aspect of OH is different here. It seems that OH differs for each individual. I don’t believe that if I have a problem, just my parent or another person can assist me.”
As compared to service providers, children demonstrated more confidence in parents. A deeper-seated mistrust of health MHS is complicating things further.
“I don’t trust this counsellor. Thus, I need to be more comfortable.”
“Even though I do not believe others, I retained my difficulties secret from myself and won’t disclose them to anybody else.”
Respondents talked about privacy breach and confidentiality. Trust presents still another obstacle to appropriate service participation. Distrust may cause a person to feel unsafe. These juvenile delinquents had a severe problem with trust.
The most crucial factor is trust. Thus, I would recommend counselling since I really valued their assistance and, honestly, really needed help at the time because I was in such a mess. Keeping things private would never benefit you.
As many children having trouble with the law reported they did not like attending their sessions and that the therapies were ineffective; it is probably not unexpected that the overall perception of MHS was negative.
“I like a few moments to sit while counsellors perform counselling because I don’t enjoy disturbance. With that, one needs to attend individual sessions to develop trust.”
“I lost my father, I had many issues, and I talked about many of them with staff members, but they didn’t assist me.”
Dealing with these individuals requires caution since their attitudes towards MHS could deteriorate if they believe their issues are getting worse. Some juveniles had unpleasant reactions to what is being done, including an in-depth evaluation and description of the problems. This defines the psychiatric profession and calls for much scrutiny. Despite the participants’ general pessimism about using services and reluctance to go, some saw benefits. These children have also discussed trust and stigma.
Discussion
Child delinquency, family income and educational level are directly correlated (Rekker et al., Reference Rekker, Pardini, Keijsers, Branje, Loeber and Meeus2015; Garbarino and Plantz, Reference Garbarino and Plantz2017; Lochner, Reference Lochner2020). The researcher believed the participants in the research would provide comments revealing that the use of MHS would be correlated with stigma, as suggested by a review of literature. The thematic review showed that out of a total of 15 respondents, most believed that MHS was stigmatised (Tully et al., Reference Tully, Hawes, Doyle, Sawyer and Dadds2019). The remaining expressed concern that receiving MHS after leaving the OH would either prevent them from being hired or be problematic for getting a job. They may face problems getting admission to the school (Evans et al., Reference Evans, Pelletier and Szkola2018; Townsend et al., Reference Townsend, Musci, Stuart, Heley, Beaudry, Schweizer and Wilcox2019). These findings somewhat corroborate the notion that youngsters who run afoul of the law experience stigmatisation when they seek mental healthcare after leaving the OH (Milin et al., Reference Milin, Kutcher, Lewis, Walker, Wei, Ferrill and Armstrong2016; Zola et al., Reference Zola, Ilyas and Yusri2017). Studies have found that OH does not have enough MHS (Underwood and Washington, Reference Underwood and Washington2016; Paul and Khan, Reference Paul and Khan2019). However, it was interesting that most aberrant children interviewed claimed no stigma associated with obtaining MHS. But most minors claimed they had not sought treatment despite exhibiting symptoms (Thompson et al., Reference Thompson, Morris, Thompson and Morris2016) and various psychological symptoms (Firmin et al., Reference Firmin, Luther, Lysaker, Minor and Salyers2016). The lack of seeking treatment supports the hypothesis that a stigma is attached (Stringer and Baker, Reference Stringer and Baker2018; Lievesley et al., Reference Lievesley, Harper and Elliott2020). Even so, delinquents found it easier to talk about their difficulties with associates (Rafedzi et al., Reference Rafedzi, Abrizah, Yu and Abrizah2016). It was determined that most individuals did not experience any official pressure to be less than candid about their mental health issues. The children’s responses to other questions, however, were intriguing since they suggested there might be unspoken pressure from officials to refrain from seeking counselling or other required interventions (Ricciardelli et al., Reference Ricciardelli, Carleton, Mooney and Cramm2020). A few aberrant teenagers claimed they were engaged in several illegal actions and would be wrong if they told anyone about their time in the OH and, with that, their involvement in several illicit pursuits. This is intriguing since the younger hinted that if people judged him as a bad guy, he would not develop into a strong man and could not accomplish anything in the future. Another teenager claimed he did not want to use MHS because the officials always view with prejudice, interfering with their schooling (Snyder, Reference Snyder2015) and possibly their careers. If children stopped getting mental healthcare while in an observation home, their chances of finding employment might decrease (Chan, Reference Chan2019). The stigma might also intensify (Moore et al., Reference Moore, Stuewig and Tangney2016).
The final hypothesis was that aberrant teenagers lack trust in counsellors. It was hypothesised that children feared there would be breaches in confidentiality because the counsellor who was coming may share everything with the JJB or other officials (Gibbs et al., Reference Gibbs, Walters, Lutnick, Miller and Kluckman2015). The study’s finding matches this hypothesis as the teenagers failed to go for the services, expressed a fear of being noticed by the various officials of the observation home, and many shared that they would feel more agreeable with their family and friends. Many aberrant children said they would share their problems with family members (Kapetanovic et al., Reference Kapetanovic, Boele and Skoog2019), but it has been seen that they are comfortable talking with friends (Lee et al., Reference Lee, Liu, Patacchini and Zenou2021). However, following a comprehensive examination of the data, it appears there is a bad stigma linked to obtaining psychological help, such as being labelled as a wrong person. Evidence did not explicitly support each assumption. It was also clear that youngsters who broke the law feared consequences, such as losing their jobs and having a counsellor with the JJB violate their privacy (Todres, Reference Todres2022; Math et al., Reference Math, Gowda, Basavaraju, Manjunatha, Kumar, Enara, Gowda and Thirthalli2019; Birchley et al., Reference Amin and Khan2017). However, the stigma, unexpected repercussions and privacy intrusions were not explicitly addressed by these youngsters.
Role of social workers
Juvenile offenders often experience remorse and humiliation due to “their different delinquent behaviours” (Stuewig and McCloskey, Reference Stuewig and McCloskey2005; Hoffman and Duschinski, Reference Hoffman and Duschinski2020). These emotions may significantly discomfort individuals and exacerbate mental health conditions in that age category. Understanding the psychological effects of obtaining mental health treatment may inspire reforms to serve this demographic better. It is crucial to realise that stresses in correctional facilities have been demonstrated to impact psychological health while inmates are away from home and after they return (Fazel et al., Reference Fazel, Doll and Långström2008; Tasca et al., Reference Tasca, Turanovic, White and Rodriguez2014). To effectively treat minors with MHS, it is vital to understand their particular requirements. This research offers three separate contributions to the field of social work. While dealing with children who have had a challenging reintegration, “psychiatrists, physicians, or nurses need to be aware of the delicate nature of reintegration” at the micro level (Baglivio et al., Reference Baglivio, Wolff, Piquero, Greenwald and Epps2017). This study investigated children’s attitudes and beliefs in understanding what must be changed to improve mental health treatment. Such children may benefit from MHS and social work assistance, and the aberrant children see these services as beneficial (Whitney and Peterson, Reference Whitney and Peterson2019). This study will provide social workers insights into constructively interacting with the target population and developing a strong therapeutic bond. According to studies, abnormal teenagers prefer to talk about their issues and activities, and processing these experiences may be beneficial (Hartwig and Myers, Reference Hartwig and Myers2003; Vyas, Reference Vyas2016). This research will assist social workers in understanding MHS-seeking hurdles and facilitating transformation. As a result, services may be delivered successfully. Understanding the proper services is crucial since “the prevalence of mental health disorders connected to stress and adaptation indicates a need to build community-based service resources to manage and assist the afflicted persons” (Wells et al., Reference Wells, Miranda, Bruce, Alegria and Wallerstein2004; Sellers, Reference Sellers2015; Rijo et al., Reference Rijo, Brazão, Barroso, da Silva, Vagos, Vieira and Macedo2016). Social workers can promote change due to this study to ensure that these children’s needs are adequately met. Taking care of youngsters’ emotional factors at OH will result in fewer stressed people who will perform better in the future (Abrams, Reference Abrams2013; Covington and Bloom, Reference Covington and Bloom2014). Through community-based programmes and activities, children participate in many forms of delinquency; social workers may restrict such activities (Davidson & Wolfred, Reference Davidson and Wolfred1997; Phillips, Reference Phillips1997; Henggeler, Reference Henggeler2016). This research has generated information at the policy level that would enable efficient methods for identifying mental health issues and developing interventions for the targeted group. Limited studies are currently available to frame policy about effectively encouraging access to and delivering mental health treatment for such youngsters (Hassan, Reference Hassan2021). Last but not least, this research was necessary because social workers need to figure out how to connect with adolescents who have encountered psychiatric problems (Goldkind, Reference Goldkind2011).
Directions for research, policy and practice in social work
To ensure that all juvenile offenders get the care they need, the study was designed to catalyse further investigation. Further investigation is required to determine what obstacles prevent such adolescents from obtaining MHS and what initiatives might benefit counselling those who engage in delinquency. This research made the social work field aware of the stigma these minors face when they seek treatment, whether overtly acknowledged or not. It assisted in identifying the obstacles individuals confront while seeking assistance.
Law enforcement agencies and NGOs
To connect delinquents with different skill development programmes, authorities may establish neighbourhood facilities for leisure activities, such as playgrounds and indoor games. To increase awareness and to conduct different events, the police and Community Based Organisations may work together (Dar and Mir, Reference Dar and Mir2013; Maqbool and Khan, Reference Maqbool and Khan2020). NGOs may bridge the gap between service providers and those who need assistance, support research capacity building and increase outreach to the community (Rather and Margoob, Reference Rather and Margoob2006).
Family and educational institutions and other allied institutions
Schools may play a crucial role in preventative and intervention initiatives by enlisting the help of experts, such as social workers, psychiatrists, counsellors and physicians (Waxman et al., Reference Waxman, Weist and Benson1999; van Os et al., Reference Van Os, Guloksuz, Vijn, Hafkenscheid and Delespaul2019), and multidisciplinary teams to create strategies for teaching children and parents about the value of family ties in prohibiting the development of delinquents. The professional team might also make a strategic plan (including community outreach, counselling, leadership training and team building) to lessen the trouble of some behaviours and support the child’s improvement (Smith et al., Reference Smith, Banegas, Acquati, Chang, Chino, Conti and Yabroff2022).
Psychoeducation
Psychoeducational therapies are those in which people with mental problems are provided knowledge. Psychoeducation might assist individuals in comprehending their issues, talking about them with others and adopting coping skills afterwards. The study’s main findings focused on stigma, help-seeking attitudes, help-seeking intentions and mental health literacy (Malla et al., Reference Malla, Margoob, Iyer, Joober, Lal, Thara and Mansouri2019; Pandya et al., Reference Pandya, Shah, Chauhan and Saha2020). On the other hand, it can play an essential role in Kashmir as the delinquents suffer from various psychological problems (Carpenter and Sugrue, Reference Carpenter and Sugrue1984). Psychoeducation was started in Kashmir in the 2000s through radio. As it was for the general population, the community responded excellently (Hamdani, Reference Hamdani2003). Individuals have found that sharing problems with others, using muscular relaxation exercises, fostering healthy family interaction and engaging themselves with activities were advantageous. Several persons said they found it highly beneficial to convey the ideas surrounding the myths and realities of psychological health. After seeing the broadcast, everyone in their family felt obliged to discuss their issues (Hamdani, Reference Hamdani2003). In the context of Kashmiri youth, information could be enhanced through psychoeducation, and comprehension would enable individuals with mental illnesses to cope with disorders better, improving prospects. Virtual psychoeducation has been more prevalent recently to improve access to resources like lectures and online modules (Kim et al., Reference Kim, Choi, Moon, Park, Hwang, Kim and Seok2020; Migoya-Borja et al., Reference Migoya-Borja, Delgado-Gómez, Carmona-Camacho, Porras-Segovia, López-Moriñigo, Sánchez-Alonso and Baca-Garcia2020).
Suggestions
-
1. MHS in Kashmir must be developed with community participation, awareness and mental health rehabilitation services.
-
2. For those living with persistent trauma, proper counselling services must be accessible.
-
3. Academicians, doctors and decision-makers must also develop strategies and regulations considering the particular demographic and mental health.
-
4. We advocate the creation of a comprehensive virtual MHS network for mental health issues. This strategy will increase the availability of services.
-
5. We should ensure availability of affordable MHS with prompt diagnosis and enhanced therapeutic follow-up.
Open peer review
To view the open peer review materials for this article, please visit http://doi.org/10.1017/gmh.2023.70.
Data availability statement
Not applicable due to the anonymisation of interview data.
Author contribution
M.M.A. led the search and screening of articles, interviews with respondents and data analysis. He drafted the initial and final manuscript and resolved inclusion criteria and data analysis; J.J. was integrally involved in theorising and research and contributed to the final paper.
Financial support
Central University of Kerala.
Competing interest
The authors declare none.
Ethical consideration
Before the interview, each participant completed an informed consent form after receiving a brief explanation of the study. The fact that participation was voluntary and that leaving at any time without consequence was made clear to participants. By coding the information from each participant, anonymity was protected. Most respondents were afraid because of the conflict in J&K; thus, data were carefully analysed as per their request. The method of data analysis chosen involved the researcher selecting coding themes from each question on behalf of the item and carefully examining the narratives and statements of respondents.
Consent for publication
Permission was obtained from each participant before the interview.
Limitations
The study’s limitations include its limited sample size and focus on children from specific neighbourhoods. Delinquent children made up the sample. Hence it was impossible to extrapolate the results of this research to the overall youth population.
Abbreviations
- APDP
-
Association of Parents of Disappeared Persons
- APL
-
above poverty line
- BPL
-
below poverty line
- ICPS
-
Integrated Child Protection Scheme (Mission Vatsalya)
- J&K
-
Jammu and Kashmir
- JJ Act
-
Juvenile Justice Act
- JJB
-
Juvenile Justice Board
- JKCCS
-
Jammu Kashmir Coalition of Civil Society
- MHS
-
mental health services
- NGOs
-
non-governmental organisations
- OH
-
observation home
- PTSD
-
posttraumatic stress disorder
- UNCRC
-
The United Nations Convention on the Rights of the Child


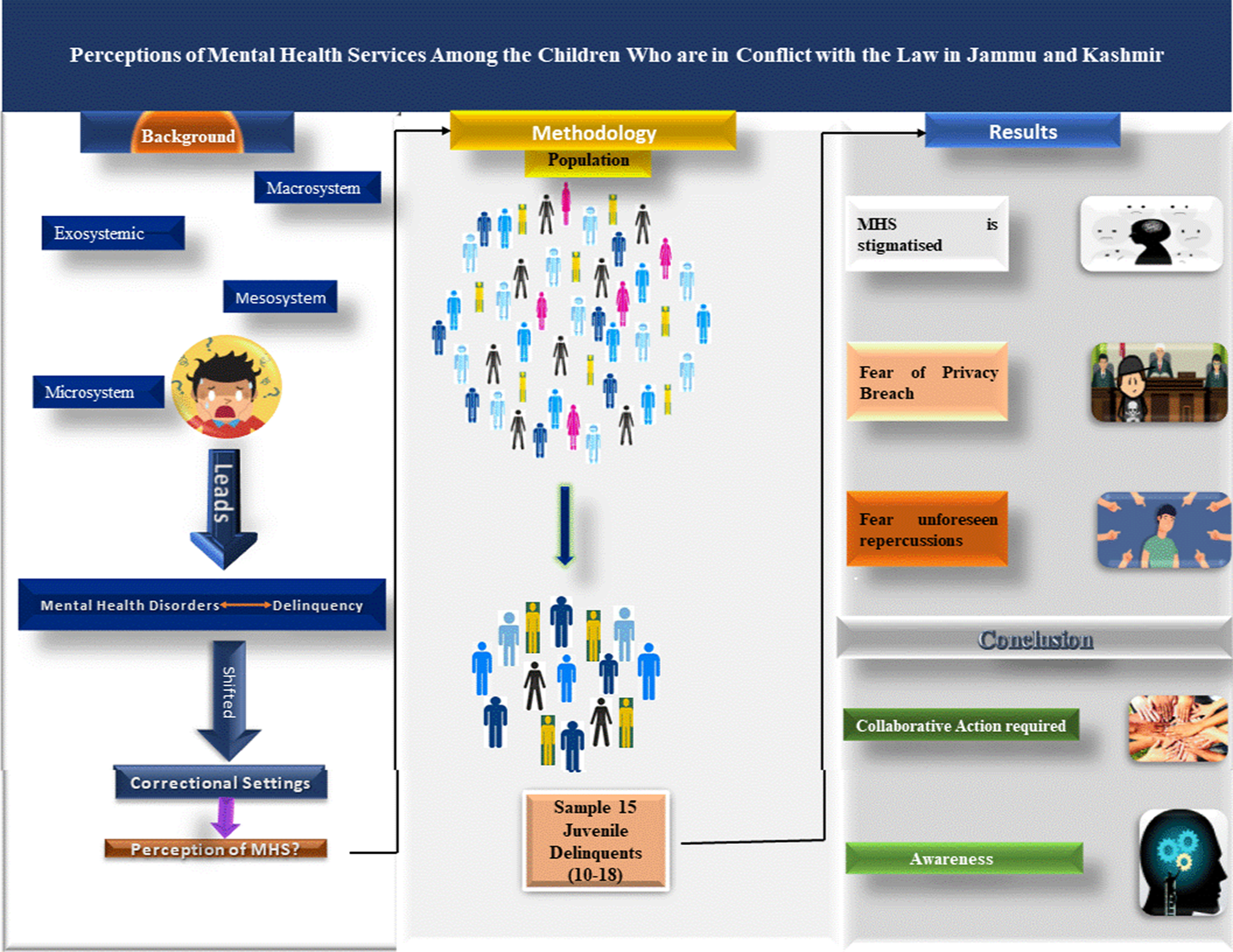




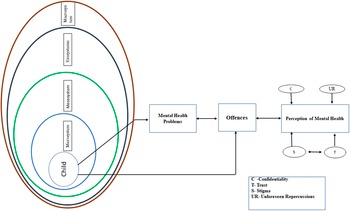
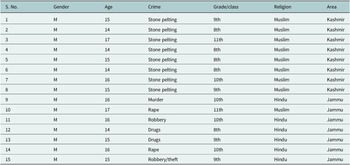
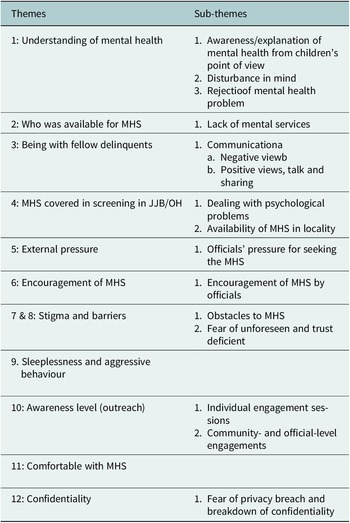

Comments
Mohd Manshoor Ahmed
PhD. Research Scholar
Department of Social Work
Central University of Kerala,
Tejaswini Hills,Periye (PO),
Kasaragod (DT), Kerala-671320
INDIA
Email: ahmed.ssw072106@cukerala.ac.in
Date: 05-01-2k23
Respected Editor,
We wish to submit an original research article entitled “Perceptions of Mental Health Services Among the Children Who are in Conflict with the Law in Jammu And Kashmir.” for consideration by Global Mental Health.
We confirm that this work is original and has not been published elsewhere, nor is it currently under consideration for publication elsewhere.
This paper finds that Jammu and Kashmir is a conflict zone, and generations over the decades have suffered. However, teenagers are also part of a particular society and are primary victims of a specific conflict, and part of the conflict also. Due to that, they adopt aberrant behaviour. After arrest, adolescents are shifted to correctional homes for rehabilitation. This is significant because there is much need to generate awareness among the children who conflict with the law regarding mental health services to eradicate stigma, mistrust, and discrimination. With that, authorities must have to do more also.
We believe this manuscript is appropriate for publication in the Global Mental Health. We have no conflicts of interest to disclose.
We appreciate your consideration of this manuscript.
Sincerely,
Mohd Manshoor Ahmed Dr Jilly John
PhD. Research Scholar Assistant Professor
Department of Social Work Department of Social Work
Central University of Kerala Central University of Kerala
Email: ahmed.ssw072106@cukerala.ac.in Email: jillyjohn@cukerala.ac.in