Introduction
The emergence of the novel SARS-CoV-2 coronavirus pandemic (COVID-19) has triggered a series of cascading events echoing those following the Spanish flu of 1919 (Gavrilova and Gavrilov, Reference Gavrilova and Gavrilov2020). On 11 March 2020, the World Health Organization declared COVID-19 a global pandemic (Cucinotta and Vanelli, Reference Cucinotta and Vanelli2020). COVID-19 has been reported by Dong and Bouey (Reference Dong and Bouey2020) to be unique for several reasons: a) rapid transmissibility, b) uncertain incubation period, and c) the possibility of asymptomatic transmission. Several studies are beginning to reflect on and investigate the biopsychosocial aspects of COVID-19 (Moreno et al., Reference Moreno, Wykes, Galderisi, Nordentoft, Crossley, Jones and Chen2020). The pandemic has set off a chain of large-scale measures to curb its spread, including self-quarantine, school closure, and physical distancing across multiple social settings such as the workplace, public spaces, etc. (Lewnard and Lo Reference Lewnard and Lo2020). Thus, despite the predominantly biological nature of COVID-19, there are a multitude of psychosocial effects, including a marked increase in the stress and distress among the general public and healthcare workers (HCWs) alike (Otu et al., Reference Otu, Charles and Yaya2020).
As prevention and treatment for COVID-19 are still in their naissant stages, the general public and HCWs often seem to experience a fear of mortality and morbidity (Taylor et al., Reference Taylor, Landry, Rachor, Paluszek and Asmundson2020). The effects of shortage of protective medical supplies, medical staff, and hospital beds have further escalated the prevailing circumstances (Maia Chagas et al., Reference Maia Chagas, Molloy, Prieto-Godino and Baden2020; Zarocostas, Reference Zarocostas2020). The resulting psychological effects of COVID-19 among HCWs seem to almost dwarf the direct effects of Severe Acute Respiratory Syndrome of COVID-19, whereby many HCWs persist with intransigent and debilitating post-traumatic stress and major depressive disorders (Park et al., Reference Park, Park, Lee, Kim, Lee, Lee and Shin2020). In this regard, it would be essential to quantify the types of mental health outcomes among HCWs so that the appropriate groundwork for prevention and treatment could be contemplated (Vindegaard and Benros, Reference Vindegaard and Benros2020), the main reason being that compromised medical professionals have the potential to impact the quality of medical services at a time when readiness from their side is paramount (Vindegaard and Benros, Reference Vindegaard and Benros2020). While studies have emerged on the mental healthcare outcomes among ‘generic’ types of HCWs (Amerio et al., Reference Amerio, Bianchi, Santi, Costantini, Odone, Signorelli and Aguglia2020; Tu et al., Reference Tu, He and Zhou2020), little has been forthcoming reging primary healthcare workers (PHCWs) with a few exceptions (Amerio et al., Reference Amerio, Bianchi, Santi, Costantini, Odone, Signorelli and Aguglia2020). Halcomb et al. (Reference Halcomb, McInnes, Williams, Ashley, James, Fernandez and Calma2020) have examined the experience of nurses employed in primary healthcare (PHC) across Australia in a cross-sectional online survey. The majority of the cohort (n = 637) reported negative experiences during COVID-19 including the threat of termination. They felt that the pandemic had specifically heightened exposure to work-related risks due to the lack of availability of personal protective equipment. In terms of the quality of services being dispensed, a significant number of them felt like the quality of services had been severely dented by the pandemic. In India, George et al. (Reference George, Inbaraj, Rajukutty and de Witte2020) have explored the experience of community HCWs serving the marginalized sectors of society in rural India. This study reported exhaustion to be common among HCWs while fear of death or contamination with COVID-19 and being targeted or stigmatized by society were commonly reported. Contracting COVID-19 and the potential of it resulting in death have been documented among HCWs. By May 2020, in Spain, 40 921 healthcare professionals were confirmed to have COVID-19 infection, 53 of whom lost their lives to this disease (Muñoz and López-Grau, Reference Muñoz and López-Grau2020). In Oman, Al Ghafri et al. (Reference Al Ghafri, Al Ajmi, Anwar, Al Balushi, Al Balushi, Al Fahdi, Al Lawati, Al Hashmi, Al Ghamari, Al Harthi, Kurup, Al Lamki, Al Manji, Al Sharji, Al Harthi and Gibson2020) have conducted six focus group discussions among PHCWs. The themes that emerged from this qualitative study included an overwhelmed feeling of stress and exhaustion which appeared to be exacerbated by the prevailing lockdown, social distancing, and having to deal with death. It is not clear how these feelings of stress and exhaustion among PHWCs in qualitative studies fare when scrutinized using quantitative psychiatric tools. There is also the added issue of having no quantitative studies from emerging economies such as Oman.
According to the World Health Organization (2020), ‘primary care can play a significant role in the COVID-19 response by differentiating patients with respiratory symptoms from those with COVID-19, making an early diagnosis, helping vulnerable people cope with their anxiety about the virus, and reducing the demand for hospital services’. Lying at the southern tip of the Arabian Peninsula, Oman reported its first two cases of COVID-19 on 24 February 2020, (Khamis et al., Reference Khamis, Al Rashidi, Al-Zakwani, Al Wahaibi and Al Awaidy2020). Due to these factors, the Ministry of Health increased surveillance measures at the ports of entry, instituted health promotion and education activities with capacity building, and training activities for HCWs became an integral part of regular medical practice. The Ministry of Health ensures the provision of universal free healthcare for all Omani citizens and PHC constitutes the ‘backbone’ of its compartmentalized healthcare system divided into primary, secondary, and tertiary care (World Health Organization, 2017). Thus, it appears that the essential functions of PHC generally include identification and early diagnosis as reported elsewhere (Muñoz and López-Grau, Reference Muñoz and López-Grau2020). According to the National COVID-19 Surveillance System conducted from February to April 2020 (Al-Rawahi et al., 2021), there were 2,443 confirmed cases of COVID-19. The overall first-time testing rate for this period was 85.17% with a positivity rate of 53.1%. Asymptomatic cases accounted for approximately 16% of the sample. The death rate was 0.32 per 100 000 people.
The overall national positive ratio was 5.7%, ranging from 2.2 to 7.1% across different regions of the country with the regions of higher population density being the most affected. During these prevailing circumstances, it is not clear how COVID-19 has impacted the PHCWs in the region of Oman where COVID-19 was most endemic, i.e. the governorate of Muscat. At the time of this study, the number of those identified to have COVID-19 in the Muscat governorate had quadrupled. This was accompanied by high recovery rates and a low number of deaths (Khamis et al., Reference Khamis, Al Rashidi, Al-Zakwani, Al Wahaibi and Al Awaidy2020). According to the database of the Ministry of Health (2020), the highest number of confirmed cases (n = 8852) and deaths (n = 167) within Oman were reported from the capital city of Muscat, accounting for approximately 80% of the total cases in the country (Khamis et al., Reference Khamis, Al Rashidi, Al-Zakwani, Al Wahaibi and Al Awaidy2020). To date, there is no report on the mental health outcomes among PHCWs in this region. Hence, this study aimed to determine the rate and covariates of depressive symptoms among PHCWs in the Muscat governorate.
Methods
Setting and participants
This cross-sectional study was conducted among PHCWs working in all PHC centers across the Muscat governorate. Being one of the 11 administrative regions of the country of approximately 4.5 million residents (World Health Organization, 2017), the Muscat governorate also includes the capital city of Muscat. It has been divided into six administrative areas or ‘wilayats’: Al Amerat, Bawshar, Muscat, Mutrah, Qurayyat, and As Seeb. The present study was conducted among all PHC centers (n = 35) that fall under the Directorate General of Health Services for the Muscat governorate (Alghafri et al., Reference Alghafri, Al Harthi, Al-Ajmi, Al-Farsi, Craigie, Bannerman and Anderson2020). HCWs not working within the presently defined region of interest (Muscat governorate), not fulfilling the present criteria for HCS (e.g allied health, nurse, physician), and those doing observerships as allied health professionals, nurses, and medical students were all excluded from the present study.
Sample size
The required sample size was calculated with an assumption that the proportion of PHCWs with psychological co-morbidity is 35%, based on an earlier report (Lai et al., 2019). To reach the power of 80%, and a significance level of 5%, 200 participants were required to complete this study. To allow for the appropriate analysis of the various subgroups, it was necessary to increase the sample size to reach the upper limit of 300 participants in the PHC setting.
Data collection
The study was conducted from 10 May to 10 June 2020. With existing constraints on ‘traditional’ modes of data collection, the study was conducted online using an electronic Google questionnaire. Electronic study proformas were disseminated through mobile phone applications (WhatsApp) and emails to all PHCWs working in the Muscat governorate. Multiple prompts were sent via messaging software to encourage them to participate. Duplicate entries were curtailed by restricting users with the same IP (Internet Protocol) address from accessing the survey on more than one occasion. The system was equipped to prompt the participants to proceed with finishing the unanswered portions of the study instrument. Incomplete study surveys could not be submitted to the system.
All administrative divisions running PHC services across the Muscat governorate fall under the umbrella of the Director-General of Health Services in the Muscat governorate. Therefore, the process of recruitment and contacting the PHCWs was first initiated at the Director-General of Health Services in the Muscat governorate. Since the onset of the pandemic, all PHC facilities followed service delivery protocols and guidelines to meet the updated case definitions. A regional operational team headed by the Director-General of Health Services in the Muscat governorate bore the administrative, logistical, and clinical responsibility of managing COVID-19 cases. Data management of suspected and confirmed cases and their contacts were managed by the outreach team.
The online questionnaire included information about the study and contained a consent clause for the participants to respond to before answering the questions through a Google link. The study survey was disseminated in both Arabic and English. The rationale for including both English and Arabic questionnaires stem from two interrelated reasons. First, despite the protracted exercises to translate the instrument into another language, its accuracy could still be undermined by certain subtle linguistic and conceptual misunderstandings that might not have been apparent during translation. Therefore, the study survey was given in both languages. Psychometric properties of the outcome measures solicited using the Arabic version of the Patient Health Questionnaire (PHQ-9) have been established to have high concordance with the English version and Arabic version in terms of the factor structures and internal reliability (Tau-equivalent reliability = 0.857) (AlHadi et al., Reference AlHadi, AlAteeq, Al-Sharif, Bawazeer, Alanazi, AlShomrani, Shuqdar and AlOwaybil2017) as well as among non-native PHCWs speaker of English (Indu et al., Reference Indu, Anilkumar, Vijayakumar, Kumar, Sarma, Remadevi and Andrade2018) Secondly, training for allied healthcare professionals, i.e. nurses and physicians, is provided in English. The education and teaching resources for HCWs generally follow an Anglo-American model (Muliira et al., Reference Muliira, Natarajan and Van Der Colff2017, Al Huseini et al., Reference Al Huseini, Al Alawi, Al Sinawi, Al-Balushi, Jose and Al-Adawi2019). HCWs are required to pass an English proficiency examination as a prerequisite for working with the Ministry of Health (Al Maqbali et al., Reference Al Maqbali, Al Omari, Slimane and Balushi2019). Hence, English is widely spoken.
Outcome measures
Depressive symptoms
Depressive symptoms were solicited using the PHQ-9 (Kroenke et al., 2001). The PHQ-9 appears to parallel semi-structured interviews in terms of its efficacy in identifying the presence of depressive symptoms (Levis et al., Reference Levis, Benedetti and Thombs2019). For the present study, factor analysis and reliability test results were analyzed. The factorability of the nine items of PHQ-9 was first scrutinized. The Kaiser–Meyer–Olkin measure of sampling adequacy appeared to exceed the threshold of 0.6 at a measure of 0.9. Bartlett’s test of sphericity (test of at least one significant correlation between two of the items studied) emerged as being significant (P < 0.001) (Tobias and Carlson, Reference Tobias and Carlson1969). The communalities of the items were all above 0.3. Communalities constitute a proportion of the item’s variance explained by the extracted factors. Such an outcome testifies to the view that each item shared some common variance with other items. With the emerging indicators, factor analysis appeared to be suitable for all nine items of the PHQ-9.
Within the background of the present research, principal components analysis was utilized to identify composite scores for the factors underlying the items of PHQ-9. Initial eigenvalues (statistical values used in deciding how many factors to extract in the overall factor analysis where values of ≥1.0 are considered statistically sound) (Dunn et al., 2014) indicated that only the first factor – ‘Little interest or pleasure in doing things?’ and ‘Feeling down, depressed, or hopeless?’ – explained 47.7% and 10.8% of the variance in the data, respectively. Cronbach’s Alpha emerged as 0.85 which, in turn, lent support to the adequate internal consistency of the scale.
Existing literature suggests vast variability for optimal cutoff scores of the PQH-9 (Manea et al., Reference Manea, Gilbody and McMillan2012). This study utilized a standard protocol – receiver operating characteristic (ROC) analysis – to establish optimal cutoff or specifically sensitivity and specificity of PHQ-9 (Al-Ghafri et al., Reference Al-Ghafri, Al-Sinawi, Al-Muniri, Dorvlo, Al-Farsi, Armstrong and Al-Adawi2014) for PHCWs in Oman. For the first phase, different strata of PHCWs (n = 75) were asked to fill the PHQ-9. For the second phase, 35 PHCWs were interviewed for the presence of depressive symptoms using Composite International Diagnostic Interview (CIDI) (World Health Organization, 1993). The researchers who performed the first phase and the second phase were ‘blinded’ to each other. Among the pooled scores from the CIDI and PHQ-9, the ROC curve was calculated to discriminate between the sensitivity and specificity for the PQH-9 for every possible threshold score. In the final analysis, a cutoff score ≥10 on the PQH-9 yielded the best compromise between sensitivity (80.6%) and specificity (94.0%).
Covariates
Various covariates (Table 1) were included in the online study proforma including sociodemographic variables such as gender, age and occupational type (‘allied health’, ‘nursing’, and ‘physician’). Participants were asked to indicate whether they had any persistent and pervasive medical [‘have at least one underlying physical health condition?’ (‘yes’, ‘no’)] or psychiatric conditions [‘Do you have positive family history of psychiatric disorders’ (‘yes’, ‘no’)]. Participants were also asked to indicate whether they were, at any capacity, in direct contact with positively tested COVID-19 patients.
Table 1. Sociodemographic and depressive symptom status of primary healthcare workers according to age group

^ Chi-square test; PHQ-9:Patient Health Questionnaire (range from 0 to 27): without depressive symptoms <10; with depressive symptoms ≥10;
* two missing.
Ethical approval
The study was approved by the Regional Research and Ethical Review Committee, Directorate General of Health Services (Ref: MH/DGHS/DPT/528/2020/12 April 2020), Ministry of Health, Muscat, Oman. As per international best practice, the study ensured the anonymity of respondents who were explicitly informed that their participation was voluntary and were requested to provide consent online before the commencement of the study. If undue distress was experienced by the participant while responding to the mood scale/sensitive questions, without compromising the required anonymity, the contingent measures were in put in place for counseling and if needed, referral to mental health specialists was also provided.
Statistical analysis
Descriptive statistics, including percentage, mean, and median were used to describe the basic sociodemographic features of the PHCWs. Depressive symptoms of each worker were measured by the PHQ-9 scores; those with scores equal to/above 10 were considered as having depressive symptoms, else they were considered to be functioning without depressive symptoms. In the univariate analysis, each sociodemographic factor was compared to two groups of PHCWs using a chi-square test and Fisher’s exact test. Multivariate logistic regression was used to determine risk factors associated with depressive symptoms in PHCWs after adjusting for all sociodemographic factors. IBM SPSS 23 was used to conduct the analysis and the level of significance of each test was set at 5%.
Results
Table 1 shows the results for demographics and the associations between the age groups among PHCWs. Among the total number of those who fulfilled the study eligibility criteria (n = 600), the response rate was 72% (n = 432). They had an average age of 39.2 years (SD = 7.8 years), ranging from 25.0 to 75.0 years. Participants were then divided into three age groups (≤34, 35–39, and 40+ years) with almost equal proportion in order for us to be able to explore any relationship between age category and other demographic factors. Results showed a significant association between different age groups and professions, having at least one underlying physical health condition and depressive symptom status. In the age group of 40+ years, there were more physicians (59.4%, n = 70, P < .001) having at least one underlying physical health condition (32.2%, n = 55, P = 0.001) than the other two groups. In contrast, there were more PHCWs aged below 34 years (24.6%, n = 34, P = 0.038) who endorsed depressive symptom status as compared to the two other groups (age 35–39 years:14.6%, n = 18; age 40+ years: 15.2%, n = 26).
Table 2 shows the results for demographics and the associations/differences between depressive symptoms among all PHCWs. A total of 78 out of 423 subjects (18.1%) were considered to have depressive symptoms. In the univariate analysis, there was no significant association found between depressive symptoms and profession (allied health versus physician: P = 0.528; nurse versus physician: P = 0.504), personal psychiatric history (P = 0.210), family history of psychiatric disorders (P = 0.828), and direct involvement with COVID-19 patients (P = 0.755). However, results show that PHCWs who were younger (≤34 years) were more likely to have depressive symptoms than older workers (40+ years, P = 0.039) and female workers were more likely to have depressive symptoms than male workers (P = 0.018). Workers who reported at least one underlying physical health condition were more likely to have depressive symptoms than those without medical problems (P = 0.008). In the multivariate analysis, after adjusting for all factors, the logistic regression model showed that being 34 years of age or below (OR = 2.079, P = 0.021) and having at least one underlying physical health condition (OR = 2.216, P = 0.007) were factors contributing significantly to depressive symptoms among the PHCWs.
Table 2. Sociodemographic data of primary healthcare workers according to depressive symptom status
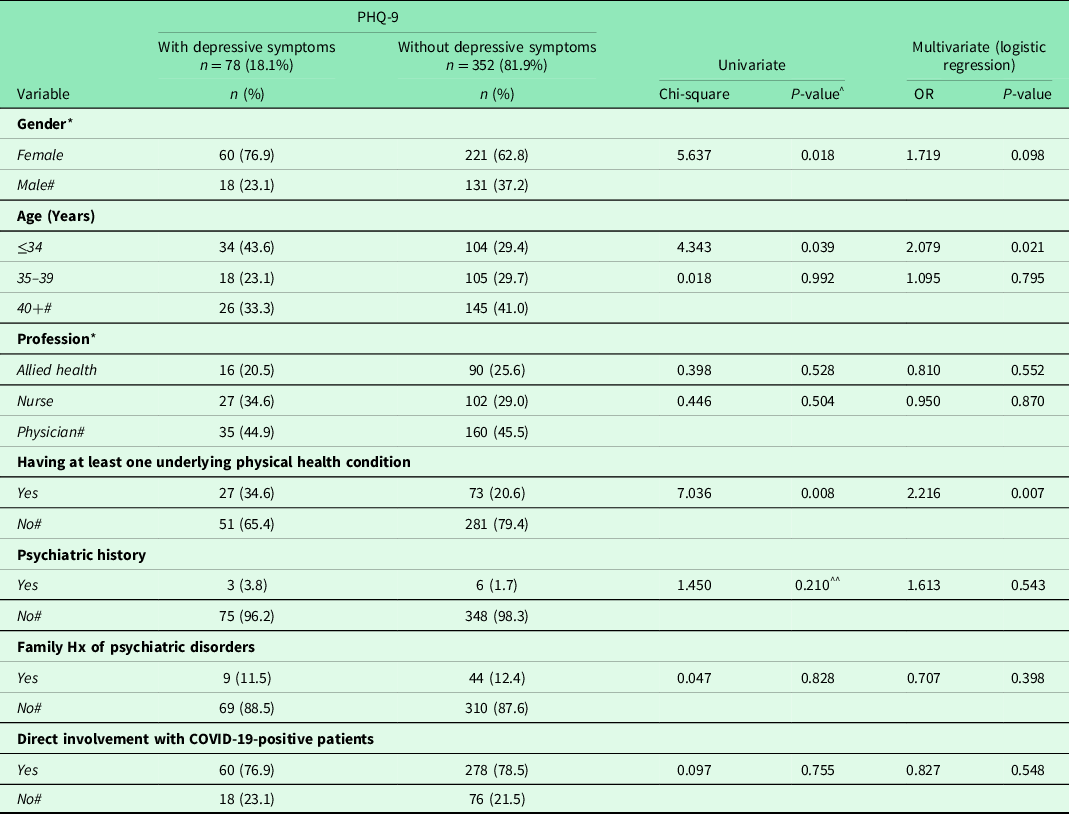
^Chi-square test; ^^Fisher’s exact test; OR = odds ratio; # = reference point;
* two missing; PHQ-9, Patient Health Questionnaire (range from 0 to 27): with depressive symptoms <10, with depressive symptoms ≥10; Hosmer & Lemeshow test (chi-square = 1.996, P = 0.981); sensitivity = 57.7%, specificity = 66.0%, overall = 64.5%.
Discussion
To date, this is the first quantitative examination of the rate of depressive symptoms among PHCWs in the Muscat governorate during the COVID-19 pandemic. A previous qualitative study conducted during the pandemic indicated that stress and its sequalae are common among PHCWs in the Muscat governorate (Al Ghafri et al., 2020). The current study suggested that 18.1% of the PHCWs showed depressive symptoms. The cohort operationalized as PHCWs consisted of allied HCWs, nurses, and physicians. The multivariate logistic regression which aimed to explore the impact of each factor on depressive symptoms adjusted by other factors together suggested that being of younger age (34 years or below) and having at least one underlying physical health problem appears to contribute significantly to having depressive symptoms.
Before the 1980s, Oman was labeled as a ‘hermit kingdom’ due to its isolation from the rest of the world and rudimental healthcare services (Peterson, Reference Peterson2004). In the 1980s, with the discovery of hydrocarbons, the initial phase of PHC focused on dispensing child immunization, reducing child mortality and heightening maternal care in a country gripped by malnutrition, communicable diseases, and environmentally transmitted infectious and communicable diseases (Al-Mandhari et al., Reference Al-Mandhari, Alsiyabi, Al Rabhi, Al-Adawi, Al-Adawi, Braithwaite, Mannion, Matsuyama, Shekelle, Whittaker and Al-Adawi2018). More recently, with the rise of noncommunicable diseases in the country, which entail continuity of care as well as the persisting challenge of communicable diseases, PHC centers have cropped up across all regions of the country (Al-Mahrezi and Al-Kiyumi, Reference Al-Mahrezi and Al-Kiyumi2019). In addition to the physical presence of PHC centers, concerted efforts were made to increase the number of HCWs with limited success as PHC is predominantly catered to by non-specialized staff. Al-Mahrezi and Al-Kiyumi (Reference Al-Mahrezi and Al-Kiyumi2019) have stated that the existing man power serving PHC falls short of international best practice. Generally, in emerging economies, the PHC setting has been reported to often have inadequate staff, excessive workload, financial strain, inadequate supervision, frequent conflicts among healthcare professionals, stressors in their private life, and a lack of social support (Zarei et al., Reference Zarei, Ahmadi, Sial, Hwang, Thu and Usman2019, Dugani et al., Reference Dugani, Afari, Hirschhorn, Ratcliffe, Veillard, Martin, Lagomarsino, Basu and Bitton2018). Due to these factors, PHC tends to exhibit high rates of turnover and those in the field are often prone to high risk of depressive disorders, poor job performance, and high rates of absenteeism (Al-Makhaita et al., Reference Al-Makhaita, Sabra and Hafez2014). In Oman, Al-Hashemi et al. (Reference Al-Hashemi, Al-Huseini, Al-Alawi, Al-Balushi, Al-Senawi, Al-Balushi, Jose and Al-Adawi2019) examined occupational burnout using the Maslach Burnout Inventory among PHCWs in an urban city of Oman, Muscat. This study reported a 6.3% prevalence of burnout and longer working hours was found to be strongly associated with the development of depressive symptoms. Given the precarious circumstances owing to COVID-19, scant attention has been directed towards determining the rate and covariates of depressive symptoms among PHCWs. PHC centers have a catchment area of approximately 1.442 million people distributed along 3,500 km2. The compartmentalized healthcare system in Oman requires service users to utilize these widespread PHC centers as the first point of contact for medical services. Within such background, the question remains regarding the mental health outcomes of PHCWs during what has already been labeled ‘a once-in-a-century pandemic’ (Gates, Reference Gates2020).
The present study found 78 out of 432 or 18.1% of PHCWs to have an above cutoff (≥ 10) score on the PHQ-9. In studies that have used the PHQ-9 during the COVID-19 outbreak among 100 nurses in Wuhan, China, Tu et al. (Reference Tu, He and Zhou2020) reported 46% having depressive symptoms. Among PHCWs in Genoa, Italy, Amerio et al. (Reference Amerio, Bianchi, Santi, Costantini, Odone, Signorelli and Aguglia2020) reported that 22.9% of the sample appeared to score ≥10 on the PHQ-9. Some studies have reported the rate of depressive symptoms among the different spectrums of frontline HCWs using various instruments. In Hubei province in China, Lai et al. (2019) reported 50.4% of the sample as having depressive symptoms. In Singapore, Tan et al. (Reference Tan, Chew, Lee, Jing, Goh, Yeo, Zhang, Chin, Ahmad, Khan, Shanmugam, Chan, Sunny, Chandra, Ong, Paliwal, Wong, Sagayanathan, Chen, Ying Ng and Sharma2020) reported 8.9% of the sample to be having depressive symptoms. Overall, all the studies considered so far have suggested that poor mental health outcomes are common among HCWs (Pappa et al., Reference Pappa, Ntella, Giannakas, Giannakoulis, Papoutsi and Katsaounou2020). Indeed, adverse mental health outcomes in PHCWs, including depressive symptoms, have been an area of concern in the literature and its rate often outstrips the rate found in the general population (Holmes et al., Reference Holmes, O’Connor, Perry, Tracey, Wessely, Arseneault, Ballard, Christensen, Cohen Silver, Everall, Ford, John, Kabir, King, Madan, Michie, Przybylski, Shafran, Sweeney, Worthman, Yardley, Cowan, Cope, Hotopf and Bullmore2020). The possible reasons for these mental problems may be associated with work-related stressors and the resultant occupational burnout. A recent cross-sectional study from Iran reported that 53% of PHCWs were burned out during the COVID-19 period (Jalili et al., 2020). Similarly, a systematic review reported higher rates of burnout among physicians, specifically on indices of emotional exhaustion (0–86.2%), depersonalization (0–89.9%), and low personal accomplishment (0–87.1%) (Rotenstein et al., Reference Rotenstein, Torre, Ramos, Rosales, Guille, Sen and Mata2018). Other reasons could be attributed to worrying about the risk of infection, especially with the shortage of protective equipment (Jalili et al., 2020). Additionally, social isolation, particularly when PHCWs are required to undergo prolonged quarantine, and fear of contaminating their significant other are some of the many potential factors that could trigger stress and distress among PHCWs during the ongoing crisis (Kisely et al., Reference Kisely, Warren, McMahon, Dalais, Henry and Siskind2020). Moreover, uncertainties of impending death faced by critically ill patients could further exacerbate the challenges of the situation (Chen et al., Reference Chen, Liang, Li, Guo, Fei, Wang, He, Sheng, Cai, Li, Wang and Zhang2020). It was interesting to note that physicians and nurses exhibited higher rates of depressive symptoms compared to allied health workers. This could be attributed to the fact that physicians and nurses, by the nature of their job, are more likely to have a direct encounter with COVID-19 patients. This supports the contention that frontline HCWs, rather than non-frontline HCWs, are often more prone to stress and distress (Alshekaili et al., Reference Alshekaili, Hassan, Al Said, Al Sulaimani, Jayapal, Al-Mawali, Chan, Mahadevan and Al-Adawi2020).
Existing literature on the magnitude of medical complications among HCWs has not received due attention. In contrast, the literature is replete with studies on the magnitude of burnout and poor mental outcomes (Rotenstein et al., Reference Rotenstein, Torre, Ramos, Rosales, Guille, Sen and Mata2018). The proportion of PHCWs in this study with depressive symptoms and concurrently underlying physical health conditions amounted to 23.1% of the sample and 34.6% of them had elevated scores in PHQ-9. A national study from the USA showed that 3–11% of HCWs were reported to have at least one underlying physical health condition (CDC COVID-19 Response Team, 2020). Speculations to account for such a link are therefore warranted. Firstly, it is not clear whether their physical illnesses are likely to trigger psychological burden since there is widespread literature suggesting that physical illnesses tend to impact mental disorders and vice versa (Prince et al., Reference Prince, Patel, Saxena, Maj, Maselko, Phillips and Rahman2007). Secondly, with the availablility of data suggesting that people with preexisting illnesses are more prone to having poor prognostic indicators after contracting COVID-19 (CDC COVID-19 Response Team, 2020), the knowledge of such an association may heighten the stress surrounding untimely demise and the resulting existential crisis. This, in turn, could be an antecedent to the development of depressive symptoms (Ventegodt et al., Reference Ventegodt, Kandel, Neikrug and Merrick2005). More studies are therefore warranted to shed light on the link between having underlying physical health conditions and mental health outcomes.
This study suggests that age is one of the contributory factors for having depressive symptoms. Specifically, the PHCWs whose mean age was less than or equal to 34 were more likely to have depressive symptoms than older cohorts. Previous studies have aligned with the view that age has a relationship with depressive symptoms (Hayasaka et al., Reference Hayasaka, Nakamura, Yamamoto and Sasaki2007; Sun et al., Reference Sun, Sun, Jiang, Chen, Li, Ma, Wei, He and Zhang2020). There are not many plausible explanations that could account for the present relationship between age and depressive symptoms but speculations abound.
It is possible that younger HCWs are more inclined to more openly sharing their mental distress compared to the older generations. Thus, it is possible that older HCWs are less likely to admit to having depressive symptoms due to sociocultural beliefs surrounding such symptoms. There are also increasing trends of mental health awareness on popular social media platforms by large-scale influencers that younger generations are more exposed to, leading them to be more aware of many mental health conditions (Pavlova and Berkers, Reference Pavlova and Berkers2020). In traditional Omani society, emotional distress is often equated with ‘weakness of character’ which, in turn, causes an individual to be viewed negatively (Eloul et al., Reference Eloul, Ambusaidi and Al-Adawi2009). However, such a view may have changed with the onset of modern education. Recent studies have suggested that depressive symptoms are a lot less stigmatized than before (Corrigan, Reference Corrigan2016). Therefore, studies are needed to shed light on whether there is a generation gap in attitude towards and having depressive symptoms. Related to this, more research is needed to analyze sociocultural beliefs and practices in order to support the mental health of healthcare professionals involved in infectious disease care. Placing the mental health of healthcare professionals at the forefront of infectious diseases is an issue worldwide and support must be tailored to global standards while remaining sensitive to the unique cultural characteristics of each country. A society like Oman is often described to be more collectivistic in nature. Collectivism as a sociocultural practice encourages one to develop a ‘collective’ or ‘group’ mindset (Al-Adawi, Reference Al-Adawi and Jeffrey2006). Studies from collectivistic societies have suggested that shame is often implicitly used to promote conformity and cultural values. Interestingly, when distress occurs, the tendency is to externalize blame since distress such as depressed mood is not perceived to owe its origins to intrapsychic conflict. Some have suggested that rather than targeting intrapsychic conflict as it is done in western psychotherapeutic intervention, the focus should be geared toward social relationships and utilizing the facets of ‘ethnotherapy’ (Gadit, Reference Gadit and Reed2004) rather than psychotherapy. More studies are warranted in this regard.
Some salient aspects of these results are discussed here. First of all, it is intriguing that nurses are less likely to have depressive symptoms. A previous study among general frontline versus non-frontline HCWs has suggested that factors that contribute to the development of psychosocial distress include lack of experience and age (Alshekaili et al., Reference Alshekaili, Hassan, Al Said, Al Sulaimani, Jayapal, Al-Mawali, Chan, Mahadevan and Al-Adawi2020). Further exploration of such sociodemographic factors is warranted as this would have the potential to help in the development of best practices in addressing the distress among PHCWs. The second issue that is salient in this study is the preponderance of females in the study cohort (281/432) and the relatively high percentage of depressive symptoms among them, although not significant in multivariate analyses. Widespread education and empowerment of women in Oman have resulted in ‘effeminization’ of HCWs (Mohamed et al., Reference Mohamed, Abdulhadi, Al-Maniri, Al-Lawati and Al-Qasmi2018). According to Mansour et al. (Reference Mansour, Al-Awadhi, Al Nasiri and Al Balushi2020), women in Oman constitute slightly more than 30% of the workforce. Despite the participation being skewed towards a lower figure, overall education and rapid modernization triggered by the surge in oil revenues in the past decade have resulted in the pronounced empowerment of women (Randeree Reference Randeree2012). It appears that females outshine their male counterparts on many indices of education, and females were more likely to excel in higher education (Mansour et al., Reference Mansour, Al-Awadhi, Al Nasiri and Al Balushi2020).
Many previous studies that have documented mental health outcomes among HCWs have utilized screening tools without establishing their psychometric properties (Amerio et al., Reference Amerio, Bianchi, Santi, Costantini, Odone, Signorelli and Aguglia2020; Tu et al., Reference Tu, He and Zhou2020). To lay the groundwork for the present study, protracted exercises were undertaken to establish the psychometric properties of the PHQ-9. The internal consistency of this tool was adequate. Factor analysis showed that the variability in scores contributed the most to the overall results. As there is no cut-off point to distinguish caseness from non-caseness, this study established a cutoff greater than or equal to 10 to yield the best compromise between sensitivity and specificity.
Limitations
There are several limitations to this study. First, the nature of this online survey (google survey) may have attracted individuals who were more technologically savvy. This may have restricted the participation of a large number of PHCWs who had no access to or experience with using online technology. Future studies with a larger sample size inclusive of staff from secondary and tertiary hospitals may be helpful. Second, compared to other studies, the presently observed rate of depressive symptoms appears to be lower compared to the international trend. In general, the rate of depressive symptoms appears to be lower in the Arabian Gulf (Eloul et al., Reference Eloul, Ambusaidi and Al-Adawi2009) especially in comparison to other studies where a larger percentage of health workers showed a pooled prevalence of 22·8% according to a recent systematic review and meta-analysis (Pappa et al., Reference Pappa, Ntella, Giannakas, Giannakoulis, Papoutsi and Katsaounou2020). The depressive symptoms might have been underreported due to mental health-related stigma. Therefore, social desirability could have accounted for the present lower rate. Third, the cohort operationalized as PHCWs consisted of allied HCWs, nurses, and physicians. It is not clear how allied HCWs are exposed to the stress and distress often encountered among nurses and physicians. The inclusion of allied HCWs should be considered one of the limitations of this study. Four, the current study focused only on depressive symptoms with no consideration of the presence of other psychological disorders. Follow-up studies exploring other mental illnesses and investigating the reversibility of symptoms with time are warranted (Alshekaili et al., Reference Alshekaili, Hassan, Al Said, Al Sulaimani, Jayapal, Al-Mawali, Chan, Mahadevan and Al-Adawi2020). Five, while the checklist for depressive symptoms underwent psychometric evaluations, it is well known that to adequately detect clinical depressive symptoms, semi-structured interviews based on the International Classification of Disease or the Diagnostic and Statistical Manual of Mental Disorders are essential. Six, during the time of stress, many people develop poor coping, adjustment disorder, or acute stress reactions including emotional disorders such as depressive symptoms. However, it is not clear whether the present snapshot view of the depressive symptoms has the potential to culminate in the development of chronic and debilitating psychiatric disorders. Longitudinal studies are therefore warranted. Lastly, the fact that there was a high response rate indicates a scarcity of non-responders. Such an occurrence, by default, constitutes one of the limitations of this study.
Conclusion
To date, few studies have explored the rate and covariates of depressive symptoms among PHCWs and none have emerged from the Arabian Gulf countries. The present study was conducted among PHCWs in the northern part of the country including the capital city, Muscat, where the bulk of the population resides. To lay the groundwork for the present study, the instrument for tapping into depressive symptoms was scrutinized for its applicability. The present study suggests that approximately 18% of PHCWs had depressive symptoms. The logistic regression model showed that age and having at least one underlying physical health condition were significantly associated with the development of depressive symptoms. Studies are therefore needed to assess whether the presently found rate of depressive symptoms is more related to the acute stress reaction of working during the pandemic or the culmination into full-blown psychiatric disorders in the future. In the meantime, it is essential to screen and identify PHCWs at risk of mental illness and refer them to the appropriate services. The integration of mental health services at the earlier stages of any crisis should be a cornerstone of the overall preparedness during crises with a particular focus on factors like age and having underlying physical health conditions.
Authors’ contributions
AA, TA, HA, and FA had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: AA, TA, HA, FA, and SH.
Acquisition, analysis, or interpretation of data: AA, TA, and FA.
Drafting of the manuscript: AA, TA, HA, FA, SA, SM, and MFC.
Critical revision of the manuscript for important intellectual content: AA, SA, and MFC.
Statistical analysis: SH, SA, and MFC.
Administrative, technical, or material support: AA, TA, HA, and FA.
Supervision: AA, TA, HA, and FA.
Financial support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of interest
The authors declare that there are no conflicts of/or competing interests.
Ethical standards
Written informed consent was obtained from all participants before data collection. The study and the details of consent were approved by both the Regional Research and Ethical Review Committee, Directorate General of Health Services (Ref: MH/DGHS/DPT/528/2020/12 April 2020), Ministry of Health, Muscat, Oman. This study adhered to the World Medical Association’s Declaration of Helsinki (1964–2008) for Ethical Human Research including confidentiality, privacy, and data management.
Consent for publication
Not applicable. However, consent for publication was obtained through ethics approval and consent to participate.
Availability of data and materials
This is a research article and all data generated or analyzed during this study are included in this published article.





