The link between traits such as personality and cognitive style and vulnerability to depression is well established. A range of measures have been robustly associated with depression including neuroticism, Reference Martin1 dysfunctional attitudes Reference Jones, Scott, Haque, Gordon-Smith, Heron and Caesar2 and low self-esteem. Reference Jones, Scott, Haque, Gordon-Smith, Heron and Caesar2 The link to depression occurring in relationship to childbirth has not been as extensively investigated and findings are less robust, but studies have reported evidence of association with neuroticism, Reference Verkerk, Denollet, Van Heck, Van Son and Pop3 introversion, Reference Verkerk, Denollet, Van Heck, Van Son and Pop3 perfectionism, Reference Mazzeo, Slof-Op't Landt, Jones, Mitchell, Kendler and Neale4 low self-esteem, Reference Beck5 and dysfunctional cognitions. Reference Moorhead, Owens and Scott6,Reference Church, Brechman-Toussaint and Hine7 It remains to be established, however, whether measures of personality and/or cognitive style predict vulnerability to postnatal episodes over and above their known association with depression in general. Identifying specific vulnerability factors would have both theoretical and clinical importance. For example, in addition to giving important clues about aetiology, they could allow identification of women at high risk of postnatal depression and indicate those women in whom early intervention may be of benefit. They may also influence the development of psychotherapies specific to the postpartum context, and may predict adherence with, and response to, other treatment approaches such as medication.
In this study we address two questions: (1) does personality and/or cognitive style differ in women with a history of postnatal depression compared with healthy controls; and (2) do measures of personality and/or cognitive style distinguish women with a history of postnatal depression from women with recurrent major depressive disorder who have not experienced perinatal episodes.
Method
Samples
Two samples are included in this study: (1) a patient sample (parous women with major recurrent depression, who were not in an episode of depression when recruited and assessed, divided into two subsamples of (a) having a history of postnatal depression, and (b) not having an episode of depression in relation to childbirth); and (2) a healthy female control sample.
The patient sample was recruited as part of our ongoing research programme to investigate genetic and non-genetic determinants of major affective disorders, which uses systematic and non-systematic recruitment methods. Patient records of community mental health teams (CMHTs) across the UK are systematically screened to identify patients with major affective disorders, and, at the discretion of the responsible medical officer, all patients deemed suitable for inclusion are invited to participate. Invitations are sent to patients only when, in the opinion of the CMHT, they do not currently meet diagnostic criteria for a major depressive episode. Additionally, patient volunteers are recruited non-systematically via advertisements for participants with affective disorders in local general practitioner surgeries, local media and via patient support organisations (Depression Alliance and MDF The BiPolar Organisation). Patients are included in our research programme if they meet the following criteria: capable of giving voluntary informed written consent; aged 18 years or over; meet DSM–IV, 8 ICD–10 9 and Research Diagnostic Criteria (RDC) Reference Spitzer, Endicott and Robins10 for a major affective disorder; and, because of the fact that they are recruited for molecular genetic studies, UK/Ireland White ethnicity. Patients are excluded if they: have only experienced affective illness in relation to, or as a consequence of, alcohol or substance misuse or dependence; have only experienced affective illness as a consequence of medical illness or medication; or are an intravenous drug user with a lifetime diagnosis of dependency. Across our whole research programme, 44% of suitable patients identified via CMHTs have refused to participate and we have been unable to make contact with a further 14%.
To be included in the study reported here, patients must also be parous women meeting DSM–IV, 8 ICD–10 9 and RDC Reference Spitzer, Endicott and Robins10 criteria for major recurrent depressive disorder. Additional exclusion criteria are: an organic brain disorder or other cognitive problem that impedes ability to complete questionnaires; or biologically related to another study participant. Our final eligible sample for the study reported here is 379 parous women with recurrent major depressive disorder, with 39.3% (n = 149) recruited systematically.
The control participants are a subsample of participants who had originally been recruited to the GENESiS (Genetic Environmental–Nature of Emotional States in Siblings) study. Reference Sham, Sterne, Purcell, Cherny, Webster and Rijsdijk11 This study recruited over 34 000 individuals through general practices in England and Wales. Index participants were individuals registered with these practices in the age range 18–55 years who had no current serious medical illness or disability. Participants included as controls in our research programme had scores on the Sham Composite Index of liability to depression and anxiety (‘G’) Reference Sham, Sterne, Purcell, Cherny, Webster and Rijsdijk11 that were in the lowest 20% of the GENESiS population. ‘G’ comprises responses to the following self-report measures: General Health Questionnaire (12-item version; GHQ–12); Reference Goldberg, Gater, Sartorius, Ustun, Piccinelli and Gureje12 short form of the Neuroticism subscale from the Eysenck Personality Questionnaire (EPQ–N); Reference Eysenck and Eysenck13 and two subscales from the Mood and Anxiety Symptoms Questionnaire (MASQ), Reference Watson, Clark, Weber, Assenheimer, Strauss and McCormick14 which measure levels of anxious arousal (MASQ–AA) and high positive affect (MASQ–HPA). Participants selected for our programme were additionally screened using a standardised semi-structured telephone interview administered by trained psychiatrists or psychologists. None had a personal or family history of psychiatric illness (defined as having consulted a healthcare professional, or having received a diagnosis or treatment from a healthcare professional for a mental health problem). Of the control participants in our programme, there were 173 women who comprised the healthy control sample for this study.
Psychiatric assessments
Patients in our research programme are interviewed face to face, usually in their own homes, by trained psychiatrists or psychologists using the Schedules for Clinical Assessment in Neuropsychiatry (SCAN) Reference Wing, Babor, Brugha, Burke, Cooper and Giel15 and psychiatric/general practice case notes are reviewed. These data are combined for each participant to form a written case vignette. Best-estimate lifetime diagnoses are made according to DSM–IV, ICD–10 and RDC. The vignettes are also used to rate other key clinical variables (including age at onset, number of illness episodes, history of psychosis, number of psychiatric admissions) and women are asked pregnancy by pregnancy about episodes of depression occurring in relationship to childbirth. Although a complete SCAN interview is not carried out for each perinatal episode, questions are asked about depressive symptoms to establish whether the episode met DSM–IV criteria for major depression and to establish the approximate week of onset pre- or post-delivery. Each patient is diagnosed, and has key clinical variables including postnatal episode status rated independently by at least two members of the research team and consensus is reached. Interrater reliability is high. This has been formally assessed using 20 cases and resulted in mean kappa statistics of 0.85, 0.83 and 0.80 for DSM–IV, ICD–10 and RDC diagnoses respectively. Mean kappa statistics for other key clinical variables (categorical) ranged from 0.81 to 0.99. Mean intraclass correlation coefficients for other key clinical variables (continuous) ranged from 0.91 to 0.97.
Definition of postnatal episodes
Only parous women, and therefore those who had an opportunity to experience an episode of postnatal depression, were included in the analysis. An episode of postnatal depression was defined as an episode of DSM–IV major depression with onset within 6 weeks of delivery (PND group) – corresponding to our recent finding that familiality of postnatal depression is maximised between 6 and 8 weeks. Reference Forty, Jones, Macgregor, Caesar, Cooper and Hough16 A wider definition of perinatal depressive episode was employed in defining the group of women who had not suffered with an episode of postnatal depression. Women in the non-postnatal depression group (NPND group) had given birth but had not experienced the onset of a major depressive episode either during their pregnancy or within 6 months of delivery. The PND group comprised 143 women and the NPND group comprised 131 women. The remaining 105 parous women in our sample were excluded from further analyses as they had an episode onset either during pregnancy or between 6 weeks and 6 months after delivery. Figure 1 summarises the women included in the patient groups.
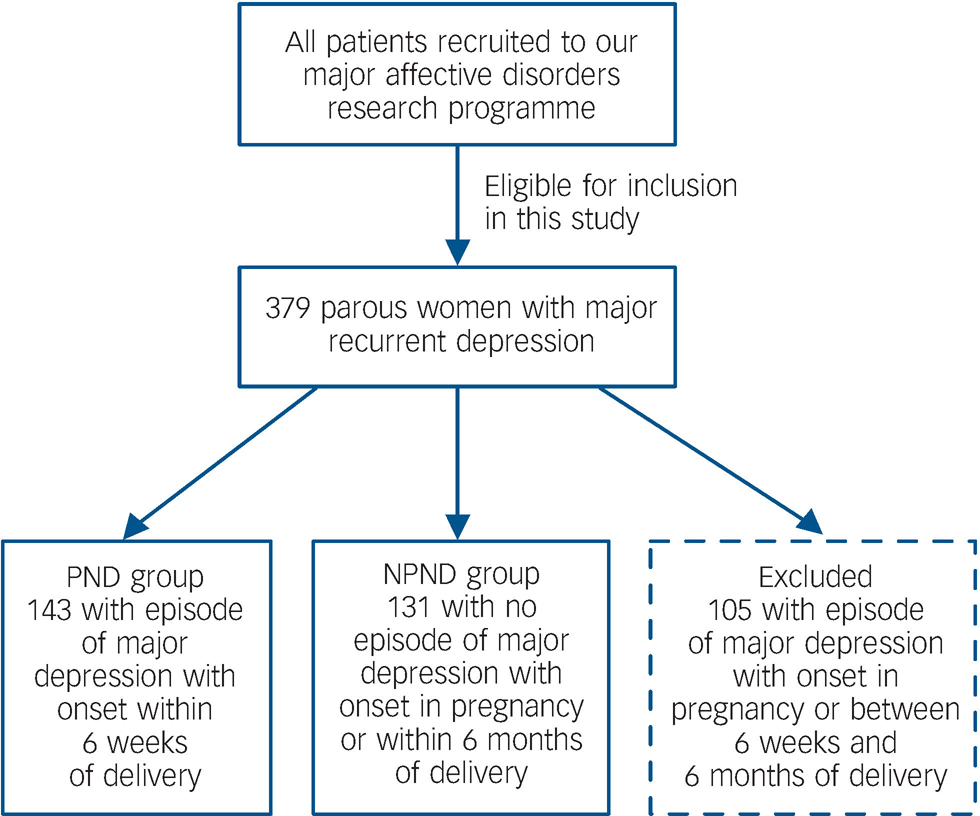
Fig. 1 Summary of participants included in the patient groups. PND, postnatal depression; NPND, non-postnatal depression.
Questionnaires
The following self-rated questionnaires, which all have demonstrated validity and reliability, were part of a larger pack of questionnaires administered to both patients and controls.
Rosenberg Self-Esteem Questionnaire (SEQ) Reference Rosenberg17
The SEQ measures trait self-esteem. It is a 10-item questionnaire comprising a positive and a negative subscale. Scores range from 5 to 20 on both subscales with high scores on the positive subscale reflecting high positive self-esteem and high scores on the negative subscale reflecting low negative self-esteem. Combining these subscales produces a total SEQ score (range 10–40), with higher total scores reflecting higher total self-esteem.
Dysfunctional Attitudes Scale (DAS) Reference Weissman and Beck18
The DAS measures underlying beliefs and attitudes. We used the 24-item version of the DAS. As well as a total score (range 24–168), the DAS gives three subscale scores (achievement, dependency and self-control) each ranging from 8 to 56. Higher scores indicate higher levels of dysfunctional attitudes.
Eysenck Personality Questionnaire (EPQ) Reference Eysenck and Eysenck13
We used the 90-item version of the EPQ. The EPQ gives scores for three personality dimensions: extraversion, neuroticism and psychoticism. Extraversion scores range from 0 to 21, neuroticism scores range from 0 to 23, and psychoticism scores range from 0 to 25.
Beck Depression Inventory (BDI) Reference Beck and Steer19
The BDI assesses the presence and/or severity of current depressive symptoms. It comprises 21 items and total scores range from 0 to 63.
Procedure
The procedure for systematically recruited patients and volunteer patients was identical. After the semi-structured interview, the questionnaires were left with patients to rate and return to the team (stamped, addressed return envelopes were provided). They were given written instructions to complete all of the questionnaires at the same time within 1 week of receiving them. If the questionnaires were not returned after 1 month, a reminder letter was sent out, along with another copy of the questionnaires and return envelope. If the questionnaires were still not returned after a further 2 weeks, a reminder telephone call was made.
The control participants received the questionnaires via post following their telephone interview. Otherwise, the procedure was identical to that outlined above.
This study received all necessary national research ethics service approval.
Statistical analysis
The three groups (PND group, NPND group and control group) were compared for age using one-way analysis of variance (ANOVA), followed by post hoc comparisons using the Tukey Test. Differences in key clinical variables between the PND and NPND groups were examined using independent samples t-tests or chi-squared tests.
The distributions of the questionnaire scores in each of the groups approximated to normal, thus the groups were compared on the BDI, and all cognitive style and personality measures using univariate one-way ANOVAs, followed by the Tukey Test. One-way univariate analyses of covariance (ANCOVA) were then carried out with possible confounders (age, BDI scores) included as covariates. The PND and NPND groups were compared using one-way ANCOVA with age, BDI scores and all clinical variables that differed between the two groups as covariates.
All analyses were undertaken using SPSS (version 14.0) for Windows.
Results
Sample characteristics
As shown in Table 1, the NPND group was significantly older (mean age 53 years) than both the PND and control groups (mean age 47 and 49 years respectively). The two patient groups scored significantly higher on the BDI (measuring current levels of depressive symptomatology) than the control group (mean BDI scores of 17, 17 and 3 respectively).
Table 1 Age and Becks Depression Inventory (BDI) scores of the three groups

| PND group | NPND group | Control group | |
|---|---|---|---|
| n | 143 | 131 | 173 |
| Age, in yearsa | |||
| Mean (s.d.) | 47.01 (11.72) | 52.53 (11.61) | 48.85 (8.88) |
| 95% CI | 45.08-48.95 | 50.53-54.54 | 47.50-50.19 |
| Range | 23-79 | 26-83 | 25-61 |
| BDI scoreb | |||
| Mean (s.d.) | 17.20 (12.47) | 17.27 (11.18) | 2.74 (2.80) |
| 95% CI | 15.12-19.27 | 15.34-19.21 | 2.31-3.16 |
| Range | 0-51 | 0-49 | 0-17 |
Table 2 summarises the clinical features of the patient groups. The PND and NPND groups were well matched on number of episodes of depression, number of psychiatric hospital admissions, number of deliveries, and history of psychosis. The NPND group had a significantly older age at illness onset (mean age 30 years), defined as age at first clinically significant functional impairment due to affective illness, than the PND group (mean age 23 years).
Table 2 Clinical features of the patient groups
| PND group | NPND group | |
|---|---|---|
| n | 143 | 131 |
| Number of episodes of depression | ||
| Mean (s.d.) | 4.97 (2.61) | 4.38 (2.65) |
| 95% CI | 4.48-5.35 | 3.91-4.84 |
| Range | 2-16 | 2-15 |
| Age at illness onset, yearsa | ||
| Mean (s.d.) | 23.07 (6.61) | 30.03 (11.40) |
| 95% CI | 21.93-24.21 | 23.04-32.03 |
| Range | 11-39 | 10-61 |
| History of psychotic symptoms, n (%) | ||
| Never present | 124 (86.7) | 119 (90.8) |
| Present | 15 (10.5) | 12 (9.2) |
| Not known | 4 (2.8) | - |
| Number of admissions | ||
| Mean (s.d.) | 0.79 (1.20) | 0.81 (1.58) |
| 95% CI | 0.57-0.98 | 0.51-1.06 |
| Median (IQR) | 0.00 (1.00) | 0.00 (1.00) |
| Range | 0-6 | 0-10 |
| Number of deliveries | ||
| Mean (s.d.) | 2.46 (1.06) | 2.26 (1.02) |
| 95% CI | 2.27-2.65 | 2.09-2.44 |
| Range | 1-6 | 1-6 |
Comparison of personality and cognitive style between the groups
Mean scores for each of the groups on each of the personality and cognitive style measures are presented in Table 3. Compared with the control group, the PND group showed significantly lower levels of self-esteem and extraversion, and significantly more dysfunctional attitudes, neuroticism and psychoticism. There were no significant differences on any of the measures between the PND and NPND groups.
Table 3 Cognitive style and personality scores in the three groups
| PND group | NPND group | Control group | |
|---|---|---|---|
| Rosenberg Self-Esteem | |||
| Questionnaire | |||
| n | 132 | 128 | 170 |
| Total scorea | |||
| Mean (s.d.) | 23.99 (5.97) | 24.92 (6.31) | 34.18 (3.66) |
| 95% CI | 22.96-25.02 | 23.82-26.03 | 33.63-34.74 |
| Positive subscalea | |||
| Mean (s.d.) | 12.74 (2.96) | 13.05 (3.09) | 16.92 (3.73) |
| 95% CI | 12.23-13.25 | 12.51-13.59 | 16.63-17.22 |
| Negative subscalea | |||
| Mean (s.d.) | 11.25 (3.56) | 11.88 (3.80) | 17.26 (2.39) |
| 95% CI | 10.64-11.86 | 11.21-12.54 | 16.90-17.62 |
| Dysfunctional Attitudes | |||
| Scale | |||
| n | 133 | 129 | 170 |
| Total scoreb | |||
| Mean (s.d.) | 98.18 (24.90) | 93.74 (29.01) | 71.92 (17.25) |
| 95% CI | 93.91-102.45 | 88.69-98.80 | 69.31-74.53 |
| Achievementb | |||
| Mean (s.d.) | 31.69 (11.44) | 30.09 (12.33) | 19.51 (7.97) |
| 95% CI | 29.73-33.65 | 27.94-32.23 | 18.30-20.71 |
| Dependencyb | |||
| Mean (s.d.) | 35.72 (9.07) | 33.56 (10.46) | 25.52 (7.08) |
| 95% CI | 34.17-37.28 | 31.74-35.38 | 24.45-26.59 |
| Self-controlb | |||
| Mean (s.d.) | 30.77 (8.24) | 30.10 (9.64) | 26.89 (7.65) |
| 95% CI | 29.35-32.18 | 28.42-31.78 | 25.74-28.05 |
| Eysenck Personality | |||
| Questionnaire | |||
| n | 141 | 130 | 173 |
| Extraversiona | |||
| Mean (s.d.) | 9.13 (5.58) | 9.16 (5.30) | 14.83 (4.91) |
| 95% CI | 8.21-10.06 | 8.24-10.08 | 14.10-15.57 |
| Neuroticismb | |||
| Mean (s.d.) | 17.04 (4.84) | 16.98 (4.88) | 5.14 (3.67) |
| 95% CI | 16.24-17.85 | 16.14-17.83 | 4.59-5.69 |
| Psychoticismb | |||
| Mean (s.d.) | 3.30 (2.50) | 2.92 (2.18) | 2.02 (2.07) |
| 95% CI | 2.89-3.72 | 2.54-3.29 | 1.71-2.33 |
These data were further analysed using ANCOVA. The three groups were compared on all measures controlling for age and BDI scores. The inclusion of the covariates did not alter the findings. The PND and NPND groups were compared controlling for age, BDI scores and the clinical variable that differed between the two groups, age at illness onset. Again, the inclusion of the covariates did not alter the findings.
Discussion
Postnatal mood disorders
Mood disorders occurring in relationship to childbirth are an important public health issue with suicide now a leading cause of maternal death in the UK. Reference Jones and Craddock20 Postnatal or postpartum depression are terms that have gained widespread use over the past 40 years and the concept has undoubtedly had positive effects in reducing stigma and in the development of clinical services for women who become ill at this time. However, the scientific validity of the concept of postnatal depression has been questioned over the past decade as evidence emerged to suggest that childbirth is not associated with increased rates of depression Reference O'Hara, Zekoski, Philipps and Wright21–Reference Cox, Murray and Chapman23 and that in clinical presentation and response to treatment, postnatal depression does not differ from depression occurring at other times. Reference Cooper, Jones, Dunn, Forty, Haque and Oyebode24 Nevertheless, findings are inconsistent and the literature is far from clear.
Other studies have suggested that in a subgroup of women who experience postnatal depression there is a specific association between childbirth and the onset of depression Reference Cooper and Murray25 and that the postnatal period may indeed be a period of increased risk for depression when analyses take account of other known risk factors for depression. Reference Eberhard-Gran, Eskild, Tambs, Samuelsen and Opjordsmoen26,Reference Munk-Olsen, Laursen, Pedersen, Mors and Mortensen27 In addition, we have recently demonstrated that a vulnerability to postnatal triggering is familial and therefore potentially influenced by genetic factors. Reference Forty, Jones, Macgregor, Caesar, Cooper and Hough16 If some women have a particular vulnerability to postpartum episodes of depression, identifying putative risk factors for postnatal depression will increase the clinician's ability to prospectively identify those at high risk and also contribute to research on stress–vulnerability models of mood disorders.
Studies that have been carried out so far suggest considerable overlap between the risk factors for postnatal depression and for depression in general. Reference O'Hara and Swain28 However, it is important that studies determine what factors may specifically increase an individual's susceptibility to postnatal episodes – be they biological or psychosocial.
Personality and cognitive style
One line of research that has proved very productive in increasing understanding of stress–vulnerability models of depression is the study of premorbid traits. There is robust evidence that personality traits, especially high premorbid levels of neuroticism Reference Martin1 and abnormalities of cognitive style such as stable negative self-esteem Reference Jones, Scott, Haque, Gordon-Smith, Heron and Caesar2,Reference Scott, Stanton, Garland and Ferrier29 are associated with vulnerability to depression. We examined whether personality and/or cognitive style predict vulnerability to postnatal episodes of depression as it is plausible that the transition to motherhood is a particular challenge for some women (e.g. those with low self-esteem). Reference Moorhead, Owens and Scott6
Our findings suggest that women with a history of major depression associated with childbirth demonstrate characteristic depressogenic profiles with lower self-esteem (greater negative evaluation of self, and less positive evaluation of self), higher levels of dysfunctional attitudes (greater need for achievement, greater dependency on others, and greater need for control of self), and higher levels of neuroticism compared with healthy controls. These findings are consistent with previous studies of women with postnatal depression and of women who experience recurrent (non-postnatal) depression compared with healthy controls. Reference Verkerk, Denollet, Van Heck, Van Son and Pop3–Reference Beck5,Reference Church, Brechman-Toussaint and Hine7
The present study then extended the analysis to explore whether any of these personality and cognitive measures has a specific association with postnatal depression over and above the robustly demonstrated associations with vulnerability to depression in general. We did not find any unique cognitive or personality characteristics that differentiated between women with recurrent major depressive disorder who did or did not have a history of postnatal depression. This suggests that future studies of postnatal depression should incorporate this three-group design to distinguish between factors that influence the depression diathesis in general and the puerperal onset in particular. Study designs that do not include a non-postnatal depression group and simply demonstrate differences between women with postnatal depression and healthy controls cannot demonstrate specificity for depression triggered by childbirth and erroneous conclusions may result.
Strengths
Our samples were large and post hoc power calculations, undertaken using nQuery Advisor (version 4.0) for Windows, showed that on all of the questionnaire measures our sample size had >99% power to detect at the 0.05 level the difference in means between the three groups. The patients in this study were: narrowly defined – they met lifetime diagnostic criteria according to three widely-used psychiatric classification systems; well characterised – illness data were collected using a validated semi-structured interview and case-note review, and a range of clinical variables, including puerperal status, were rated using consensus method, with excellent interrater reliability; and representative – a large percentage were systematically ascertained. The control group was unaffected and selected for a low risk of developing a mood disorder.
Limitations
Our results must be interpreted in light of a number of limitations. First, this is a cross-sectional study so we cannot determine whether the differences in personality and cognitive style observed in the women with depression are a cause of recurrent depressive episodes or the psychological sequelae of this experience. For example, elevated neuroticism scores in those with recurrent depression may represent trait vulnerability Reference Duggan, Sham, Lee, Minne and Murray30,Reference Fanous, Gardner, Prescott, Cancro and Kendler31 or merely reflect residual symptoms. Reference Farmer, Redman, Harris, Mahmood, Sadler and Pickering32 Prospective longitudinal studies are necessary if we are to determine whether there are any true differences between factors that influence a general depression diathesis and puerperal triggers in particular. For example, future studies of postnatal depression would ideally undertake cognitive and personality ratings from at least early pregnancy until up to a year postnatally and compare these with clinical outcomes.
We excluded women with onset of depression antenatally or between 6 weeks and 6 months after delivery to ensure our PND and NPND groups were as clean as possible. We chose the cut-off of 6 weeks after delivery for illness onset for the PND group on the basis of our own published work that familiality of postnatal depression is maximised when onset is between 6 and 8 weeks postpartum. Reference Forty, Jones, Macgregor, Caesar, Cooper and Hough16 A sensitivity analysis using later cut-offs might be most illuminating, although larger sample sizes are required to do this while retaining adequate statistical power. Consideration of women with antenatal onset of depression would be interesting and important, and future work should aim to explore this prospectively in a large sample of women with antenatal depression.
Furthermore, we have investigated only limited aspects of personality and cognitive style. There are a number of other measures such as coping styles, attributions, self-representations, attachment styles, novelty-seeking traits, affective temperaments and perfectionism, which may reveal differences between women vulnerable to postnatal triggering and those with no perinatal episodes of depression. It would also be important to incorporate measures that rate beliefs specifically related to motherhood Reference Moorhead, Owens and Scott6 rather than relying solely on general measures of cognitive style. Similarly, future work may benefit from including measures of social factors (e.g. relationship with partner) that may differentiate sensitivity to postnatal depression from sensitivity to depression at other times in life.
Other limitations need to be noted. For example, we have included patients recruited both systematically (via CMHTs) and opportunistically (via advertisements). Analyses repeated using only the former group, however, reveal an unchanged pattern of findings. There was a high refusal/non-response rate within our systematically ascertained group, which might have introduced responder bias. However, there was no difference in response rate between the PND and NPND groups, and any bias between patients and controls is likely to be conservative assuming that patients with higher levels of depressogenic cognitive style were those less likely to participate. Also, to maximise our power to detect differences, we used a control group selected for low risk of developing a mood disorder, so-called ‘supernormal’ controls. The measures of cognitive style examined here, however, were not used to define the control group, and it is unlikely that the differences we have found are accounted for merely by the selection of controls.
The link with childbirth is a challenge to our understanding of the aetiology of depression and has received very different explanations by those from divergent theoretical backgrounds. Biological explanations that implicate the massive hormonal fluctuations at this time vie with psychosocial explanations that emphasise difficulties in the role transition associated with motherhood. The perinatal period is a complex time with immense changes at the biological, psychological and social level, and it is therefore difficult to differentiate which factors in each of these domains play the most significant role in the onset of depressive episodes at this time. Our findings, however, suggest that personality and cognitive style alone do not identify women with a specific postnatal vulnerability.
Acknowledgements
We are indebted to all the mental health professionals who helped us to recruit patients for this work. We thank all the participants who so generously gave us their time and support.







eLetters
No eLetters have been published for this article.