Epidemiological studies have indicated that childhood obesity has increased dramatically during the past decades, both in developing and developed countries(Reference de Onis, Blössner and Borghi1–Reference Fan and Zhang6). No doubt, the widespread prevalence of obesity in children and adolescents, with its attendant health risks, has become an important public health concern(Reference Franks, Hanson and Knowler7–Reference Ng, Fleming and Robinson9). Although BMI remains the most frequently used anthropometric marker to screen for overweight and obesity, however, BMI has two problems: it does not distinguish between fat-free mass and fat, and it does not take any account of fat distribution. It has been recognised that individuals with normal BMI may have an excess of body fat; this condition has been recently described as normal-weight obesity, a risk factor for CVD(Reference De Lorenzo, Martinoli and Vaia10–Reference Romero-Corral, Somers and Sierra-Johnson12).
A number of studies have provided ample evidence that compared with general obesity (assessed by BMI), central obesity is associated with greater CVD risks(Reference Despres13,Reference Despres and Lemieux14) . Waist circumference (WC) is considered as a simple, available and inexpensive anthropometric measurement, giving relevant information about fat distribution and reflecting the degree of central obesity(Reference Daniels, Khoury and Morrison15,Reference Lee, Bacha and Gungor16) . Recently, the waist:height ratio (WHtR) has been suggested as an alternative measure to identify central obesity with a simple public health message ‘keep your waist circumference to less than half your height’(Reference McCarthy and Ashwell17,Reference Browning, Hsieh and Ashwell18) . In practice, adults with normal BMI may have a large WC or WHtR; this status is defined as normal-weight central obesity (NWCO)(Reference Gibson and Ashwell19,Reference Ashwell and Gibson20) . However, the health risks of these individuals are often neglected because of the label of normal BMI. So far, information on the prevalence of central obesity within normal category of BMI among children and adolescents is scant. In this article, based on a large sample, we report the prevalence of central obesity among normal-weight children and adolescents in Shandong, China.
Subjects and methods
The study was approved by the Ethical Committee of the Shandong Center for Disease Control and Prevention, Shandong, China.
Study population
Data for this study were obtained from the database of the survey on students’ constitution and health in Shandong Province, which is a school-based representative survey covering seventeen districts, implemented by the department of health and education in 2014. The sampling method was stratified multistage sampling based on selected schools. Briefly, three urban public schools (one each for primary school, junior high school and senior high school where located in cities) and three rural public schools (one each for primary school, junior high school and senior high school where located in towns) from each of the seventeen districts in Shandong were randomly selected and invited to participate in the study. From the selected schools, two classes in each grade were selected and all students of the selected classes were invited to join the study. All subjects were primary and secondary students, ranging from 7 to 18 years of age, and all were of Han ancestry that accounts for about 99·32 % of the total population in Shandong. All subjects were stratified by sex, age and the area of residence (urban or rural), the ratio of boy:girl and urban:rural approximately equalled to 1:1. Subjects had a medical examination before the measurements were taken. They were all in apparently good health, free from overt diseases and deformities. In this study, a total of 29 516 (14 226 boys and 15 290 girls) normal-weight children and adolescents (excluding underweight, overweight and obesity) aged 7–18 years were extracted from the database and included in the final analysis (Fig. 1).
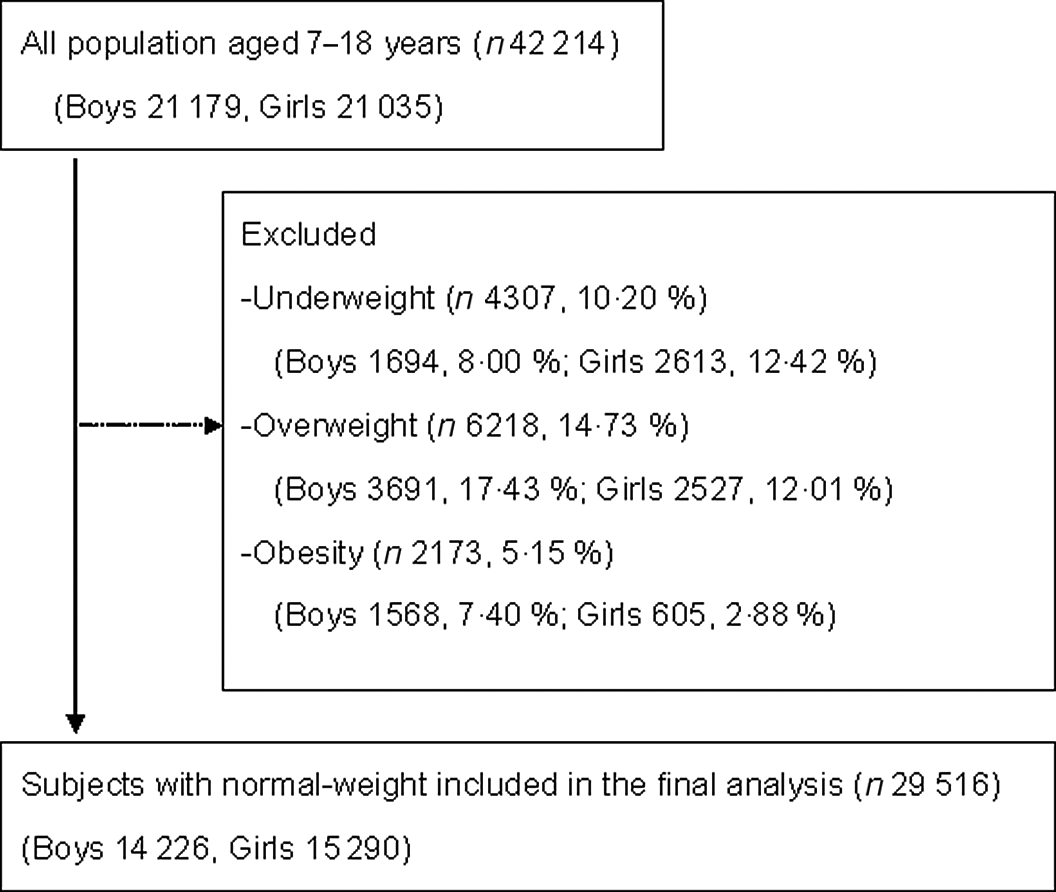
Fig. 1. Flow chart of recruiting participants.
Measurements and definitions
All measurements were performed by a team of trained health professionals in each of the seventeen districts using the same type of apparatus and followed the same procedures(21). Each professional is required to pass a training course for anthropometric measurement organised by the investigation team in Shandong. Height without shoes was measured using metal column height-measuring stands to the nearest 0·1 cm. Weight was measured using lever scales to the nearest 0·1 kg while the subjects wore their light clothes. BMI was calculated as weight in kg divided by the square of height in m (kg/m2). The category of normal weight was defined by the age- and sex-specific BMI cut-offs recommended by the International Obesity Task Force(Reference Cole and Lobstein22). WC was measured midway between the lowest rib and the superior border of the iliac crest with an inelastic measuring tape at the end of normal expiration to the nearest 0·1 cm. WHtR was calculated as WC divided by height. Central obesity was defined by the international age- and sex-specific WC cut-offs recently recommended by Xi et al.(Reference Xi, Zong and Kelishadi23) (see online Supplementary Appendix). Central obesity was also defined as WHtR ≥ 0·5(Reference McCarthy and Ashwell17).
Statistical analyses
The age- and sex-specific BMI quartiles of normal-weight children and adolescents were calculated, and all subjects within normal BMI category were reclassified into four subgroups (Q1–Q4), those in the upper fourth (Q4) were defined as ‘high-normal BMI’ and those in the lower fourth (Q1) were defined as ‘low-normal BMI’. Prevalence rates of central obesity were determined, and comparisons between different groups were made by the χ 2 test. All analyses were performed with the statistical package SPSS 11.5. Significance was defined at the 0·05 level.
Results
The prevalence of central obesity among normal-weight children and adolescents by sex and age groups in the sample is shown in Table 1. On the whole, using the WC cut-offs, the total prevalence of central obesity was 9·90 (95 % CI 9·41, 10·39) % for boys and 8·11 (95 % CI 7·68, 8·54) % for girls (sex difference P < 0·01). Specifically, significant sex difference was observed in the age groups of 7–9, 10–12 and 13–15 years (P < 0·01). Using the threshold of WHtR, the total prevalence of central obesity was 2·97 (95 % CI 2·69, 3·25) % for boys and 2·44 (95 % CI 2·20, 2·68) % for girls (sex difference P < 0·01). Boys in the low age groups (aged 7–9 and 10–12 years) had a higher prevalence of central obesity than girls (P < 0·05); instead, boys in the high age group (aged 16–18 years) had a lower prevalence of central obesity than girls (P < 0·01).
Table 1. Prevalence of central obesity among normal-weight children and adolescents
(Percentages and 95 % confidence intervals)
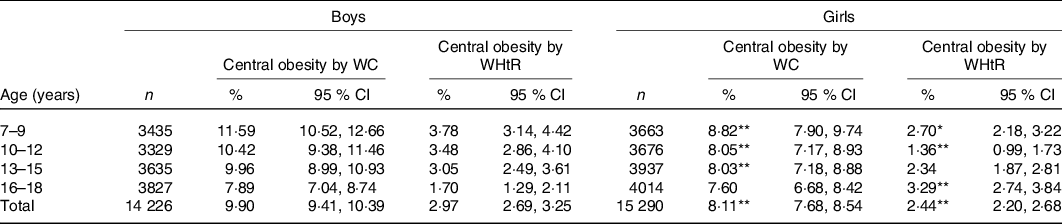
WC, waist circumference; WHtR, waist:height ratio.
* P < 0·05, ** P < 0·01 (sex difference).
As shown in Fig. 2, urban boys had a higher prevalence of central obesity (assessed by both WC and WHtR) than rural boys (P < 0·01). For girls, the urban–rural difference in the prevalence of central obesity was observed when assessing by WC and not observed when assessing by WHtR.
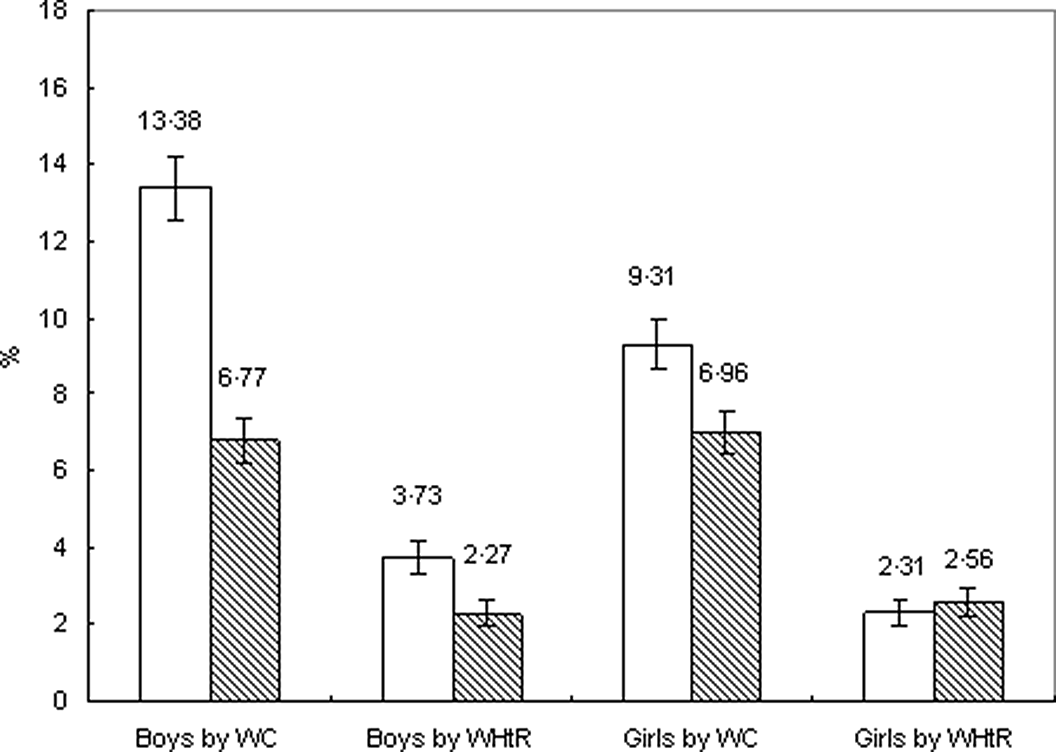
Fig. 2. Prevalence of central obesity among normal-weight children and adolescents categorised by urban–rural and sex. ![]() , Urban;
, Urban; ![]() , rural. WC, waist circumference; WHtR, waist:height ratio.
, rural. WC, waist circumference; WHtR, waist:height ratio.
The prevalence of central obesity in different subgroups categorised by BMI quartiles is shown in Table 2. For both boys and girls, the prevalence of central obesity increased with BMI percentiles; statistically significant differences were observed among the four groups (P < 0·01). Especially, children and adolescents in the ‘high-normal BMI’ group (Q4) had a much higher prevalence of central obesity than their counterparts in the ‘low-normal BMI’ group (Q1) (P < 0·01).
Table 2. Prevalence of central obesity among normal-weight children and adolescents categorised by BMI quartiles (Q)*
(Percentages and 95 % confidence intervals)
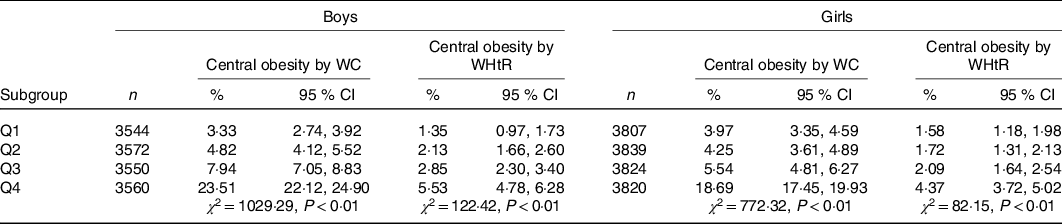
WC, waist circumference; WHtR, waist:height ratio.
* Q1, BMI < 25th; Q2, 25th ≤ BMI < 50th; Q3, 50th ≤ BMI < 75th; Q4, BMI ≥ 75th.
As shown in Fig. 3, children and adolescents aged 7–18 years in the ‘high-normal BMI’ group (Q4) had higher WC than those in the ‘low-normal BMI’ group (Q1) in all age groups (P all < 0·01), the range of differences being 5·6–9·8 cm for boys and 5·0–7·8 cm for girls, respectively. Similar difference in WHtR was also observed between Q4 and Q1 groups; children and adolescents in the Q4 group had higher WHtR than those in the Q1 group in all age groups (P all < 0·01) (see online Supplementary Appendix).
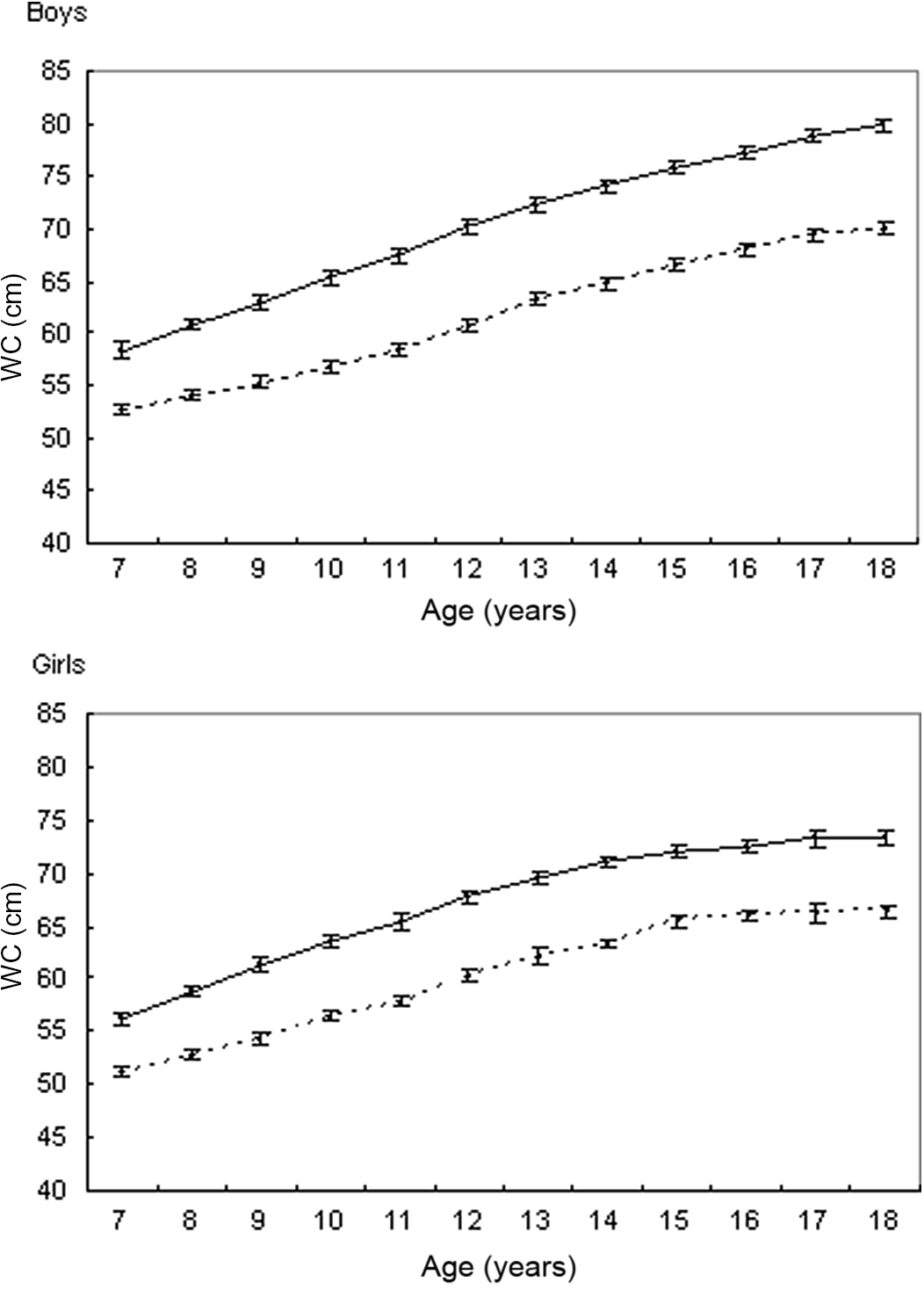
Fig. 3. Mean values (95 % CI) of waist circumference (WC) for children and adolescents in the ‘high-normal BMI’ (quartile 4) and ‘low-normal BMI’ (quartile 1) groups. ![]() , Quartile 1;
, Quartile 1; ![]() , quartile 4.
, quartile 4.
Discussion
The prevalence of central obesity in total population has been reported in numerous previous studies. However, information on the prevalence of central obesity within normal category of BMI is scant. To the best of our knowledge, this is the first study examining the prevalence of central obesity among normal-weight children and adolescents in Shandong, an important littoral province with a large population (more than 100 million) in East China. The major findings of this study were that the prevalence of central obesity as measured by WC was 9·90 % for boys and 8·11 % for girls; by WHtR was 2·97 % for boys and 2·44 % for girls. Our findings will provide scientific basis for developing monitoring and prevention strategies for childhood obesity in this region.
Only a few studies have examined the prevalence of central obesity among normal-weight children and adults. Shirasawa et al.(Reference Shirasawa, Ochiai and Yoshimoto24) reported that the prevalence of central obesity (WHtR ≥ 0·5) among normal-weight ((BMI 18·5–24·9 kg/m2) Japanese middle-aged adults was 28·17 % (23·02 % for men, 38·83 % for women) during 2013–2014. Du et al.(Reference Du, Sun and Yin25) reported that the prevalence of central obesity (WC ≥ 90 cm for men and ≥80 cm for women) among Chinese adults with BMI < 25 kg/m2 increased from 11·9 % in 1993 to 21·1 % in 2009. Based on the International Obesity Task Force BMI categories and WHtR ≥ 0·5, a few studies have reported the prevalence of central obesity among normal-weight children and adolescents. For example, a study from Greece has found that among normal-weight children aged 7–9 years, the prevalence of central obesity was 3·4–6·8 % during 2010–2011(Reference Hassapidou, Tzotzas and Makri26). A national school-based health survey during 2010–2011 has also shown that among normal-weight Greek children (aged 9·9 (sd 1·1) years), the prevalence of central obesity was 12·0 %(Reference Grigorakis, Georgoulis and Psarra27). A study from Spain has shown that 7·5 % of children aged 6–11 years and 1·8 % of adolescents aged 12–17 years within the normal BMI category suffer from central obesity during 1998–2000(Reference Schröder, Ribas and Koebnick28). A study from Portugal has shown that 8·2 % of normal-weight children aged 6–10 years suffer from central obesity during 2013–2014(Reference Rodrigues, Padez and Machado-Rodrigues29). Together with the above studies, our findings suggest that central obesity was also evident among normal-weight children and adolescents.
Sex and urban–rural disparities in the prevalence of central obesity among normal-weight children and adolescents were observed in the study; this finding is in line with the distribution of obesity in the total population (including all categories of BMI) in China(Reference Song, Wang and Dong30,Reference Song, Ma and Wang31) . This can come about from a variety of reasons. For example, it may be related to the society’s traditional preference for sons particularly in rural areas, and boys are likely to enjoy more of the family’s resources(Reference Cui, Huxley and Wu32); it may also be related to the sex difference in satisfaction with their body image, evidence has shown that body image dissatisfaction is more prevalent in girls than in boys in China, more girls regard thinness as an ideal body shape than boys and boys prefer to have a larger body size than girls(Reference Li, Hu and Ma33). The differences in dietary habit and sedentary behaviour between boys and girls may partly explain the sex difference in obesity; evidence has shown that Chinese boys ate animal foods more frequently and fruits and vegetables less frequently than girls(Reference Shi, Lien and Kumar34); compared with girls, boys usually spent more time engaged in screen-time viewing (watching television/videos, using computers/tablets and electronic/mobile devices)(Reference Cai, Zhu and Wu35,Reference Duan, Hu and Wang36) . The differences in living conditions, lifestyle and dietary patterns may partly explain the urban–rural disparities in central obesity. In China, children and adolescents resident in cities generally have easier access to high energy foods and, as a result, had a higher consumption of energy-dense, animal-based foods and a lower consumption of fruit and vegetables than their counterparts resident in countryside(Reference Cui and Dibley37,Reference Zhang, van der Lans and Dagevos38) . In addition, it has been found that sedentary behaviours were more common among children and adolescents resident in cities compared with those in countryside(Reference Cai, Zhu and Wu35). Age differences in central obesity were also observed in the study, and the reason is still unclear; it may be related to the difference in lifestyle and dietary pattern between different age stages.
Growing evidence suggests that NWCO is associated with greater CVD risks among children and adolescents(Reference Gibson and Ashwell19,Reference Ashwell and Gibson20,Reference Khoury, Manlhiot and McCrindle39) . In children aged 6–11 years, increased WC is associated with elevated blood pressure even when BMI is normal(Reference Pazin, Rosaneli and Olandoski40). Results from the Bogolusa Heart Study showed that 5·88 % of the normal-weight central obese children had the metabolic syndrome as compared with only 0·26 % of the normal-weight without central obesity; the former were 1·66, 2·01, 1·47 and 2·05 times more likely to have significant adverse levels of LDL-cholesterol, HDL-cholesterol, TAG and insulin than the latter(Reference Mokha, Srinivasan and Dasmahapatra41). In this study, we found central obesity exist in children and adolescents with a BMI in the currently accepted normal range. Especially, subjects in the ‘high-normal BMI’ subgroup had a higher proportion of central obesity. Unfortunately, the health risks of children and adolescents with NWCO may be missed when BMI is used alone as a measure of overweight and obesity. Therefore, together with previous studies(Reference Schröder, Ribas and Koebnick28,Reference Rodrigues, Padez and Machado-Rodrigues29) , we suggested that WC measurement should be included in clinical practice with a simple message ‘Keep your waist to less than half your height’.
The WHtR has gained increasing interest as a measure of central obesity, independent of sex and age, with a simple public health message ‘keep your waist circumference to less than half your height’(Reference McCarthy and Ashwell17,Reference Browning, Hsieh and Ashwell18) . For a long time, international WC cut-offs to define central obesity in children and adolescents have not yet been proposed(Reference de Moraes, Fadoni and Ricardi42). Fortunately, a set of international age- and sex-specific WC cut-offs, based on data from eight countries (Bulgaria, China, Iran, Korea, Malaysia, Poland, Seychelles and Switzerland), have just been established by Xi et al.(Reference Xi, Zong and Kelishadi23) in 2020. Using the WC cut-offs and WHtR ≥ 0·5, we examined the prevalence of central obesity among normal-weight children and adolescents. Unexpectedly, a wide disparity in the results of the two criterions was observed, and a significant difference was observed in all age groups (P < 0·01). We speculate that the 0·5 threshold of WHtR may be a bit high for children and adolescents or the new WC cut-offs may be a bit low. Further research is needed to find which approach (the current WC cut-offs or WHtR ≥ 0·5) should be prioritised as a recommendation in practice.
Despite including a large sample and using the international standards, our study has several limitations. First, the absence of detailed information concerning living environments, family economic conditions, dietary patterns and physical activity at the individual level limit our analysis of influence factors. Second, biochemical indicators (e.g. blood lipids and blood glucose) were not measured in the sample; an in-depth analysis on the potential health risks of children with NWCO could not be carried out. We plan to address these topics in the following studies and tracking the change trends in the prevalence of NWCO among children and adolescents in the future.
In summary, based on the international cut-offs of BMI, WC and WHtR, the profiles of central obesity among normal-weight children and adolescents were examined. The prevalence of central obesity as measured by WC was 9·90 % (boys) and 8·11 % (girls); by WHtR was 2·97 % (boys) and 2·44 % (girls). The health risks of children with NWCO may be missed when BMI is used alone as a measure, suggesting that it is meaningful to include WC in the clinical practice and to include the simple message ‘Keep your waist to less than half your height’.
Acknowledgements
Surveys on students’ constitution and health are conducted under the auspices of the department of education in Shandong Province, China. We thank all the team members and all participants. Special thanks to Mr. B Yu for providing access to the survey data.
This work was supported by grant no. 2014WS0376 from medical and health programme of Shandong, China.
Y. Z. designed the study and drafted the manuscript. J. C. and X. L. performed the data collection and analysis. All authors approved the final manuscript.
The authors declare that they have no conflicts of interest.
Supplementary material
For supplementary materials referred to in this article, please visit https://doi.org/10.1017/S0007114520004882








