Introduction
A primary goal in palliative care is to ensure a high quality of life for persons with palliative care needs, which involves taking psychosocial, spiritual, and physical dimensions into account (World Health Organization/Worldwide Palliative Care Alliance, 2014). The World Health Organization (WHO) in 2018 reported that, globally, 40 million people are terminally ill, and millions of others not imminently dying need palliative care. However, 86% of those in need of palliative care do not receive the needed care, and access is unequal on the basis of age, diagnosis, and home location (Lindskog et al., Reference Lindskog, Tavelin and Lundström2015; World Health Organization/Worldwide Palliative Care Alliance, 2014; World Health Organization, 2018). Still, within palliative care, dignity-conserving care must be provided in various contexts for all persons who need it (Chochinov, Reference Chochinov2007).
Core values of dignity-conserving care are dignity, kindness, and respect, and remembering to “care for” the person. A healthcare professional's attitude, behavior, compassion, and use of dialog are important components of dignity-conserving care (Chochinov, Reference Chochinov2007). Dignity is central for persons experiencing difficulties with an illness (Brennan, Reference Brennan2017). It has been described that in healthcare, persons have dignity when they are able to live in agreement with their principles and values (Barclay, Reference Barclay2016). Persons who have problems with a failing body can be vulnerable and can lose control over their body and their immediate environment, which naturally impacts their ability to uphold standards and values (Barclay, Reference Barclay2016), leading to loss of dignity (Barclay, Reference Barclay2016; Kennedy, Reference Kennedy2016). Loss of dignity is a reality for many older persons and persons who are seriously ill (Gallagher et al., Reference Gallagher, Li and Wainwright2008; van Gennip et al., Reference van Gennip, Pasman and Oosterveld-Vlug2015), affecting between 4% and 11% of older and ill people in non-cancer populations (Chochinov et al., Reference Chochinov, Johnston and McClement2016), and reported as a significant problem for patients with cancer (Hack et al., Reference Hack, Chochinov and Hassard2004). Further, dignity has been recognized as a human right (Hemati et al., Reference Hemati, Ashouri and AllahBakhshian2016; Johnston et al., Reference Johnston, Flemming and Narayanasamy2017a).
Interventions to conserve dignity can contribute to improved palliative care (Johnston et al., Reference Johnston, Papadopoulou and Östlund2017b) but their value to a person's health, and how they can be evaluated in a proper manner must be further explored to find out the most optimal setup of an intervention and how it should best be implemented to maintain a person's dignity. Previous studies (Johnston et al., Reference Johnston, Flemming and Narayanasamy2017a, Reference Johnston, Papadopoulou and Östlund2017b; McIlfatrick et al., Reference McIlfatrick, Connolly and Collins2017) raise the importance of interventions aiming to conserve severely ill persons’ dignity and of evaluating their effectiveness before implementing them in care (Lendon et al., Reference Lendon, Ahluwalia and Walling2015). In the future, healthcare will be based not so much on activities, but rather on outcomes (Department of Health, 2010). Outcome assessment has been defined as “research aimed at assessing the quality and effectiveness of health care as measured by the attainment of a specified end result or outcome … ” (Jefford et al., Reference Jefford, Stockler and Tattersall2003, p. 110). Outcome research is important to provide information that inform patient decisions, guide healthcare professionals, and inform health policy decisions (Jefford et al., Reference Jefford, Stockler and Tattersall2003). Thus, research on this topic and consideration of relevant outcomes are central to implement new interventions. This will enable healthcare providers to assess the strength of evidence (Bland, Reference Bland2015). Today, outcomes targeting dignity-conserving care need to be further explored and clarified. Previous reviews have focused on: dignity therapy (DT) and its effects (Fitchett et al., Reference Fitchett, Emanuel and Handzo2015; Donato et al., Reference Donato, Matuoka and Yamashita2016; Martínez et al., Reference Martínez, Arantzamendi and Belar2017; Xiao et al., Reference Xiao, Chow and Liu2019), overviews of psychological/psychosocial interventions (Hulbert-Williams et al., Reference Hulbert-Williams, Beatty and Dhillon2018; Teo et al., Reference Teo, Krishnan and Lee2018; von Blanckenburg and Leppin, Reference von Blanckenburg and Leppin2018; Warth et al., Reference Warth, Kessler and Koehler2019), evidence of existential interventions (Bauereiβ et al., Reference Bauereiβ, Obermeier and Özünal2018), interventions with biographical approaches (Hesse et al., Reference Hesse, Forstmeier and Mochamat2019), personal narrative interventions (Roikjær et al., Reference Roikjær, Missel and Bergenholtz2019), and death anxiety interventions (Grossman et al., Reference Grossman, Brooker and Michael2018). These reviews did not have a clear focus on outcomes studied within dignity-conserving care, and without such overviews, it could be difficult to introduce this type of care within palliative care.
To the best of our knowledge, no overview has been conducted of research concerning outcomes studied after different interventions for dignity-conserving care. Hence, this integrative review aims to identify outcomes studied after different interventions in dignity-conserving care and to find out how these have been operationalized through various instruments.
Method
Design
This study has an integrative review design (Whittemore and Knafl, Reference Whittemore and Knafl2005) to allow for the inclusion of primary studies with a combination of diverse methodologies such as quantitative studies, mixed-methods, and study protocols.
Search strategy
Searches were undertaken in four databases: CINAHL, MEDLINE, PsycINFO, and Web of Science, and limited to the time period 1997–2019. A broad and inclusive approach was used in preliminary searches to scope out the field. Indexing terms were established, as well as key words for free-text searching. Free-text key words were only used as a complement to indexing terms. In Web of Science, only free-text key words were available. The searches were started in CINAHL, where terms related to dignity (e.g. synonyms such as “personhood”) and terms related to palliative care (e.g. synonyms such as “end of life care”) were combined with Boolean operators “OR” and “AND.” Moreover, the searches were limited to English language, peer-review, and “all adult” (aged ≥18 years) studies. Where needed, the combination of search terms in CINAHL was modified for MEDLINE, PsycINFO, and Web of Science. The search strategy (Table 1) was discussed with and validated by a librarian. The database searches identified 1,619 articles. In addition, a manual search was conducted (Whittemore and Knafl, Reference Whittemore and Knafl2005) by networking within the research group and searching through reference lists of the already included articles, generating a further 59 articles (giving a total of 1,678 articles).
Table 1. Search strategy

1 Subject heading;
2 MeSH term;
3 Thesaurus. The use of caps (“”) keep words together in a keyword search.
* The search-term was used with truncation.
Selection of articles
Inclusion and exclusion criteria (Table 2) were applied. The inclusion criterion “match the aim of the review” was applied to all titles by researcher A.S., and 758 articles were excluded (see Figure 1 and Table 3 for the selection process and search results). All inclusion and exclusion criteria were used on the titles and abstracts of the remaining articles by two researchers (A.S. and K.B.) separately before they compared their independent selections, discussed disparities, and reached agreement. To validate the selection process, researchers U.Ö. and C.W.H. reviewed a selection of preliminarily included or excluded articles. This process led to discussions among all the researchers about the selection criteria until consensus was reached. This process excluded 784 articles. Full-text papers were retrieved, read in full, and reviewed by researchers A.S. and K.B., leading to exclusion of 61 articles (75 articles remaining). After a validating discussion among all the researchers, 40 articles remained. There were 16 doublets, so the final selection included 24 articles. An updated search was done in February 2019, which added two more articles to the result (n = 26) (Tables 4 and 5).

Fig. 1. Flow chart of the literature search; PRISMA flow diagram (Moher et al., Reference Moher, Liberati, Tetzlaff and Altman2009)
Table 2. Inclusion and exclusion criteria for articles

Table 3. Search outcomes from diverse databases and sources

Table 4. Articles (n = 19) focusing on the DT intervention

DT, Dignity Therapy; CCC, Client-Centred Care; DfD, Desire for Death; DIS, Dignity Impact Scale; DS, demoralization syndrome; EQ-5D, EuroQoL 5 Dimensions; HADS, Hospital Anxiety and Depression Scale; HRQoL, Health-Related Quality of Life; M, Median; MND, Motor Neurone Disease; PDI, Patient Dignity Inventory; PUB, Purposelessness, Understimulation and Boredom scale; RCT, randomized controlled trial; SD, standard deviation; SoD, Sense of Dignity; SPC, standard palliative care; T1, T2, T3, time 1, 2 and 3 denoting different measurement points.
Table 5. Articles (n = 7) focusing on interventions for dignity-conserving care, other than DT
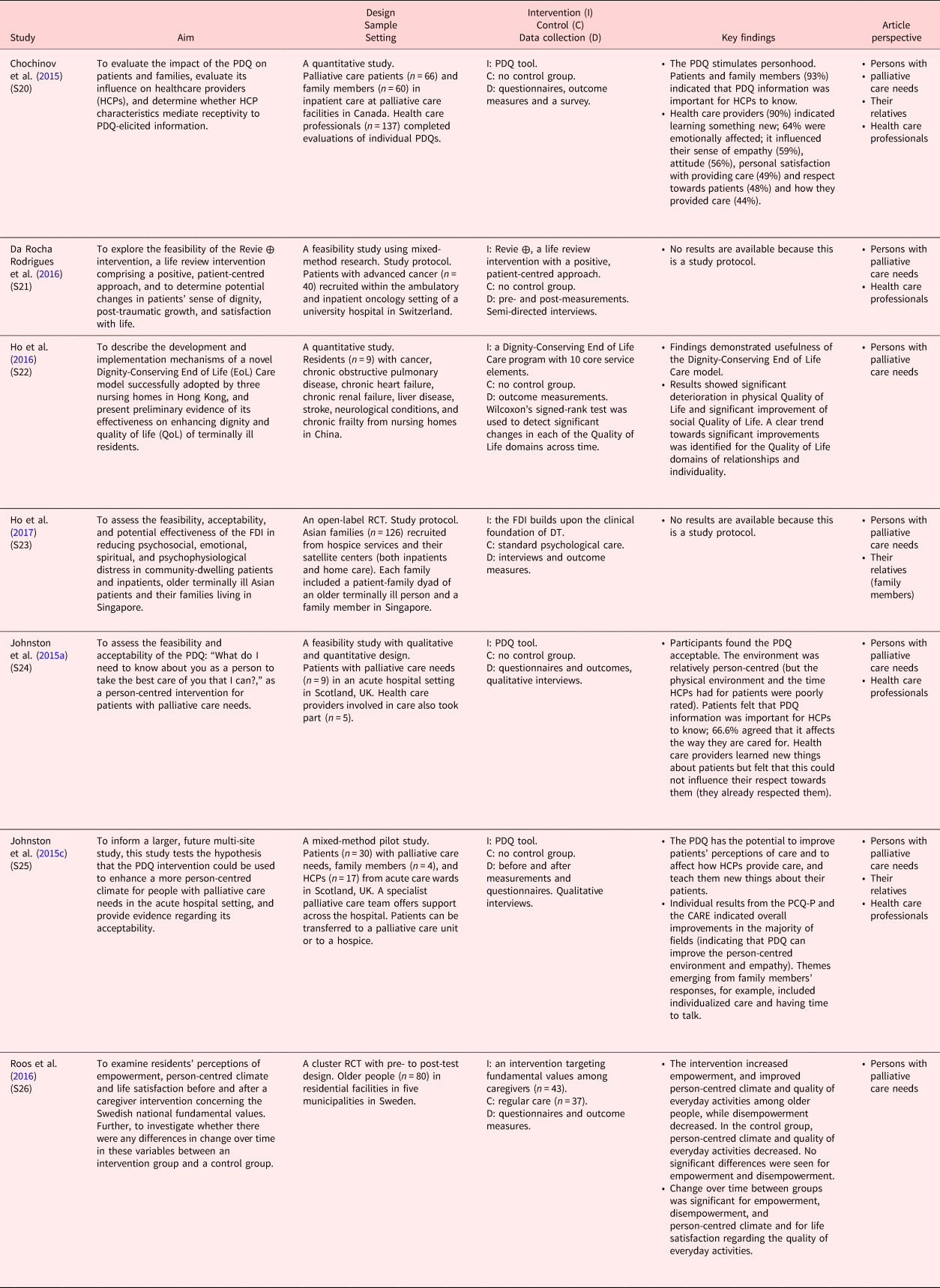
CARE, the Consultation And Relational Empathy measure; DT, Dignity Therapy; EoL, End of Life; FDI, Family Dignity Intervention; HCP, Health Care Professional; PDQ, Patient Dignity Question tool; QoL, Quality of Life; RCT, randomized controlled trial.
Data analysis
Based on Whittemore and Knafl's (Reference Whittemore and Knafl2005) recommendation, an analysis for mixed or qualitative method research, thematic synthesis (Lucas et al., Reference Lucas, Baird and Arai2007) was chosen to analyze the text of identified articles and facilitate the structuring of data. Further, an abductive approach (Alvesson, Reference Alvesson2017) was used, which assumes empirical facts but does not reject theoretical beliefs in discovering patterns that generate a deeper understanding about outcomes. Themes of outcomes were created inductively, while cluster themes were created deductively. To identify themes, researchers A.S. and U.Ö. first read and reread the articles, and focused on manifest data regarding the aim. A.S. and U.Ö. analyzed five articles separately and then discussed them together to establish and validate what should be extracted from the articles. Further, all researchers were involved in the analysis of the articles. Data were inductively collated based on questions derived from the study aim: “What outcomes were studied?” and “How were outcomes operationalized?” This process resulted in seven themes. Further, the three main categories of Chochinov's dignity model (Illness-Related Concerns, the Dignity-Conserving Repertoire, and the Social Dignity Inventory; Figure 2; Chochinov, Reference Chochinov2002) were used as a grid to deductively gather results into cluster themes. Some themes could not be clustered to the three main categories, which generated a fourth cluster theme: “Themes regarding Overarching Dignity Issues” (Table 7). For trustworthiness, themes and cluster themes were validated through discussions within the research group. In the last step, an agreed synthesis was produced, reporting main results.

Fig. 2. Harvey Chochinov's dignity model (Chochinov, Reference Chochinov2002) with permisson from the developer.
Results
The final study set comprised 26 articles (for study characteristics, see Tables 4 and 5; for included interventions, see Table 6). The findings are presented within four cluster themes and seven themes (Table 7 for overview of outcomes studied in research, see supplementary material). The cluster theme including the most outcomes was “Themes related to Illness-Related Concerns” (n = 19), while the “Themes related to the Social Dignity Inventory” covered the fewest of the studied outcomes (n = 3). Most of the reported outcomes have been studied, but outcomes reported in study protocols are proposed to be studied. To increase the readability of results, study numbers [e.g. Study 1 (S1)] are used (below and in Tables 4 and 5) instead of references for each included article.
Table 6. Description of dignity care interventions included in the integrative review (n = 6)

Tf, Theoretical framework; DT, Dignity Therapy; FDI, Family Dignity Intervention; PDQ, Patient Dignity Question tool; RCT, randomized controlled trial.
Table 7. Overview of cluster themes (n = 4) and themes (n = 7) of studied outcomes in dignity-conserving care

Themes related to Illness-Related Concerns
Performance, symptoms and emotional concerns
This theme included studied outcomes related to performance, symptoms, and emotional concerns. The outcome “Performance status” was studied after the implementation of DT and operationalized using the Palliative Performance ScaleS5 or the Palliative Performance Scale version 2 (PPSv2)S10. Further, post-DT, “Symptoms” as an outcome were studied using the Edmonton Symptom Assessment System (ESAS)S5,S19 including both emotional symptoms and physical symptoms, while “Symptoms and concerns” were studied using the Structured Interview for Symptoms and Concerns (SISC)S5, S10. Additionally, by using heart rate variabilityS23, a biomarker reflecting cardiovascular regulation, investigators planned to study “Psychophysiological wellbeing” as an outcome following the Family Dignity Intervention (FDI), while “Distress” was studied post-DT and operationalized through the Distress Thermometer, a 0–10 Likert scale that has been validated in cancer populationsS19. Moreover, investigators planned to study emotional concerns after DT implementation through the outcome “Affective states,” operationalized through the Positive and Negative Affect Schedule (PANAS),S15 and “Psychological wellbeing,” through the 20-item Life Closure Scale (LCS)S15. The outcome “Psychological distress” was studied post-DTS5, S6, S7, S9, post-FDIS23, and post-implementation of the Dignity-Conserving End-of-Life Care ProgramS22. It was proposed to be operationalized through the Geriatric Depression ScaleS6, the Distress ThermometerS7, or the Patient Health Questionnaire-9S23 or was operationalized through the Hospital Anxiety and Depression Scale (HADS)S9, the SISCS5, or the McGill Quality of Life QuestionnaireS22. Moreover, “Depression” was studied after DT and was further proposed to be operationalized using the HADSS5,S9, S10, S12, S13, S15, S17, the 15-item Geriatric Depression ScaleS8, the second edition of the 21-item Beck Depression InventoryS11, or the Zung Self-Rating Depression ScaleS16. Another outcome within this theme, proposed or studied after DT, was “Anxiety” which was operationalized through the HADSS5, S9, S10, S12, S13, S15, S17.
End-of-life and existential aspects
This theme included studied outcomes relating to end-of-life and existential aspects. “End-of-life psychological experiences” as an outcome of DT were studied using demoralization syndrome (DS) criteria, the Desire for Death scale, and the Patient Dignity Inventory (PDI)S14. Further, “Palliative care needs” as an outcome was proposed or studied through the Palliative care Outcome Scale (POS)S7, S9, and “Goals of care and treatment preferences in end of life” were studied using the Hypothetical Advanced Care Planning Scenario (H-CAP-S)S19, both post-DT. Additionally, existential outcomes were studied after DT: “Sense of life closure” was proposed through the use of the LCSS15 or studied through the Herth Hope Index (HHI)S9. “Existential wellbeing” was studied through the Functional Assessment of Chronic Illness Therapy — the 12-item Spiritual Well-Being Scale (FACIT-sp.)S3, and “Existential distress” was studied using the SISCS5, and in another study on five individual items (anxiety, sense of suffering, desire for death, lack of wellbeing, and perceived loss of dignity)S11 each one scored on a range from 0 to 6. “Purposelessness” as an outcome was further studied and operationalized through the Purposelessness, Understimulation and Boredom (PUB) scaleS16, while outcomes such as “Will to live” and “Desire for death” were studied and operationalized with the will-to-live visual analog scale included in the ESASS4, S5 and the Desire for Death Rating Scale (DDRS)S14, all after DT.
Themes related to the Dignity-Conserving Repertoire
Essential life values
This theme included outcomes relating to hope, meaning, and spirituality. The outcome “Hope” was studied or proposed to be through the HHI after DTS2, S15, while “Hopefulness” was proposed or studied through the same instrument (HHI) after DTS1, S6, S7, S8, S9 or the FDIS23. Another outcome was “Meaning in life,” which investigators proposed to study through the use of the Life Evaluation Questionnaire, the 5-item Appreciation of Life subscale, the 8-item Contentment subscale, and the 8-item Social Integration subscaleS15 (after DT), or through a modified Cancer Coherence scaleS23 (after FDI). Moreover, the outcome “Spirituality” was studied using the GES (Grupo de Espiritualidad de la Sociedad Española de Cuidados Paliativos) questionnaireS17 or the Dignity Impact Scale (DIS)S18 post-DT, while “Spiritual wellbeing” was studied through the FACIT-sp., post-DTS1, S2, S5, or proposed to be studied that way post-FDIS23.
Aspects of personal strength and coping
Some of the studied outcomes could be related to personal strength and coping. The outcome “Self-efficacy” was proposed as a mediating or moderating factor through the General Self-Efficacy (GSE) scaleS15, while “Resilience” was proposed to be studied through the Connor–Davidson Resilience Scale (CD-RISC)S15 or was studied with the Brief Resilient Coping Scale (BRCS)S17 (all after DT). In addition, the outcome “Empowerment” was studied through the Empowerment Scale (after the intervention targeting fundamental values)S26, and the outcome “Post-traumatic growth” was proposed by using the Post-traumatic Growth Inventory (PTGI) after administering the Revie ⊕ interventionS21. Investigators proposed to use “Psychological adaptation” as an outcome with the LCSS15, while “Death acceptance” was studied through the Terminal Illness Acknowledgement (TIA) questionnaireS19, both after DT.
Themes related to the Social Dignity Inventory
Aspects of care tenor and social support
This theme included aspects of care tenor and social support. The outcome “Person-centred care climate” was studied after the implementation of the Patient Dignity Question (PDQ) toolS24, S25 and an intervention targeting fundamental valuesS26, and further operationalized through the Person-centered Climate Questionnaire-Patient (PCQ-P) including three subscales measuring: a climate of safety, a climate of everydayness, and a climate of hospitality. Moreover, the outcome “Empathy” was studied and operationalized through the Consultation And Relational Empathy (CARE) measureS25 or the Empathy questionnaireS20 for healthcare professionals after administering the PDQ. “Social support” was another outcome studied post-DT; it was operationalized through the Duke-UNC-11 Functional Social Support QuestionnaireS17, focusing on confidential support (support for communicating intimate feelings) and affective support (support for positive empathy). In one study, investigators proposed a modified version of the Inventory of Social SupportS23 to study the same outcome after FDI.
Themes regarding Overarching Dignity Issues
Some themes were classifiable under more than one of the three main categories in Chochinov's dignity model (Chochinov, Reference Chochinov2002); for this reason, we considered them to reflect more broad or overarching dignity-related concerns.
Aspects of dignity and gratitude
The theme “Aspects of dignity and gratitude” was seen as a broad theme featuring in Illness-Related Concerns, the Dignity-Conserving Repertoire, and the Social Dignity Inventory. The outcomes “Sense of dignity” (after both DTS14 and FDIS23) and “Dignity-related distress” (after DTS1, S2, S3, S5, S6, S7, S8, S9, S10, S17 and the Revie ⊕ interventionS21) were reported in several articles as studied or proposed using the PDI. Other outcomes studied within this theme post-DT were “Gratitude” and “Appreciation of life,” proposed to be operationalized through the Gratitude Questionnaire Six-Item Form (GQ-6)S15 (measuring the experience of gratitude, forgiveness, and spiritual transcendence) or through the 5-item Appreciation of Life subscale and one subscale of the Life Evaluation Questionnaire.S15
Aspects of quality of life
Another theme with a broad focus on dignity issues was “Aspects of quality of life.” The “Quality of life” was studied after administering DT, FDI, and the Dignity-Conserving End of Life Care Program. It was operationalized or proposed through the Amyotrophic Lateral Sclerosis Assessment Questionnaire-5 (ALSAQ-5)S1, a Quality of Life Scale (measuring the quality of life and satisfaction with the quality of life)S4, S5, S6, S7, S8, S9, S19, and the EuroQoL 5 Dimension (EQ-5D) instrumentS6, S7, S8, S9 and also by two items from the European Organization for Research and Treatment of Cancer Quality of Life C30 (EORTC-QLQ-C30) QuestionnaireS17. Further, the “Quality of life” was proposed or studied through the McGill Quality of Life QuestionnaireS22 or through the WHO Quality of Life Scale-8S23. The outcome “Satisfaction with life” was proposed after the implementation of the Revie ⊕ intervention using the Satisfaction with Life ScaleS21 or studied after the intervention targeting fundamental values with the Life Satisfaction Questionnaire (the LSQ)S26. “Health-related quality of life” was another outcome studied (after DT) within this theme through the use of the EORTC Quality of Life Questionnaire-C15-PAL (15 items for palliative care)S10 or the Functional Assessment of Chronic Illness Therapy-Palliative Care version 4 (FACIT-Pal)S11. Investigators also proposed to study “Nursing home quality of life” through the Nursing Facilities Quality of Life scale after the implementation of the Dignity-Conserving End of Life Care ProgramS22.
Discussion
This integrative review identified outcomes that were grouped under seven themes and four cluster themes (Table 7). All identified outcomes could be related to Chochinov's dignity model (Chochinov, Reference Chochinov2002). To be able to maintain or enhance a person's dignity, outcomes related to all three main categories are suggested to be studied together to provide high-quality dignity-conserving care. Otherwise, there is a risk that some part of a person's dignity could be unconfirmed. Loss of dignity has been related to different factors: symptom and existential distress, dependency, absence of peace of mind, and a lack of social support (Rudilla et al., Reference Rudilla, Galiana and Oliver2016). This strengthens the assumption of using a broad focus on outcomes while evaluating dignity-conserving care. This review identified “Themes related to Illness-Related Concerns” as the most common cluster theme, implying the need for a broader perspective also including outcomes related to the other cluster themes, “Themes related to the Dignity-Conserving Repertoire” and “Themes related to the Social Dignity Inventory.” Other studies also recommend the use of a holistic approach to studying outcomes (Evans et al., Reference Evans, Benalia and Preston2013; Akpan et al., Reference Akpan, Roberts and Bandeen-Roche2018), which implies that outcomes identified within “Themes regarding Overarching Dignity Issues” have to be considered in order not to get a too one-sided picture of the concerns of persons with palliative care needs. Previously, Patient-Reported Outcome Measures (PROMs) that were specifically developed to address dignity-conserving care and that are recommended for researchers and clinicians were identified (Johnston et al., Reference Johnston, Flemming and Narayanasamy2017a) to be the PDI (Chochinov et al., Reference Chochinov, Hassard and McClement2008) and the Missoula-VITAS Quality of Life Index (Byock and Merriman, Reference Byock and Merriman1998). In this review, we identified “Dignity-related distress” operationalized through the PDI, as an outcome frequently studied when evaluating dignity-conserving care. By contrast, the Missoula-VITAS Quality of Life Index was not used in any of the studies, suggesting that this instrument may need more attention. Instead, other instruments measuring aspects of quality of life were identified in this review, for example, the McGill Quality of Life QuestionnaireS22 (Cohen et al., Reference Cohen, Sawatzky and Russell2017) which has shown strong psychometric properties and has previously been recommended (Selman et al., Reference Selman, Siegert and Harding2011).
It was not unexpected that “Dignity-related distress” (used in 13 of the articles) and “Quality of life” (used in 16 of the articles) were among the most studied outcomes identified, as these concepts are concrete and central in palliative care (Ho et al., Reference Ho, Chan, Leung, Fong and Tong2014; World Health Organization, 2018). These outcomes have also been listed by other researchers as essential (Reference Johnston, Flemming and NarayanasamyJohnston et al., Reference Johnston, Flemming and Narayanasamy2017a; Akpan et al., Reference Akpan, Roberts and Bandeen-Roche2018). Therefore, health organizations must enable healthcare professionals to emphasize aspects such as these. Healthcare professionals need to know how their patients experience dignity and their quality of life; and if they do not know this, their ability to provide their patients with optimal palliative care could be questioned. Providers of healthcare need to constantly remind themselves to focus on other aspects besides the patient's illnesses — and to see the whole person. It is relevant to mention that a meta-analysis has concluded that psychosocial interventions are effective in improving the quality of life and reducing emotional and existential distress (Warth et al., Reference Warth, Kessler and Koehler2019). Studies with a moderate to the high level of evidence have presented an increased sense of dignity, will to live, and sense of purpose outcomes after DT (Donato et al., Reference Donato, Matuoka and Yamashita2016). However, effects of DT on dignity and quality of life (Xiao et al., Reference Xiao, Chow and Liu2019) as well as on physical and emotional symptoms (Fitchett et al., Reference Fitchett, Emanuel and Handzo2015) have been inconsistent. DT has shown efficacy in anxiety and depression outcomes in patients with high levels of psychological distress (Martínez et al., Reference Martínez, Arantzamendi and Belar2017). These outcomes are important and useful — showing that dignity-conserving care could be beneficial for persons with palliative care needs. However, to avoid bias, it is always essential to choose outcomes and measurements that are sensitive to the intervention and to use validated instruments (Bland, Reference Bland2015). This was lacking in several of the studies and together with a small sample, the design could be questioned.
There is also a need to evaluate effects of other interventions for dignity-conserving care, as one intervention may not be suitable for everyone, and as today tailored care is advocated for, also to use other outcomes for example relating to the care tenor (e.g. person-centered climate). It has been reported that a person with an illness that suffers from multidimensional problems, benefits from a person-centered approach (Grassi et al., Reference Grassi, Mezzich and Nanni2017), and that a holistic approach (McCance et al., Reference McCance, McCormack and Dewing2011) is suitable for enhancing dignity (Chochinov, Reference Chochinov2007).
Further, outcomes within the “Themes related to the Dignity-Conserving Repertoire” can be crucial to evaluate, as it has been reported that loss of dignity is a risk factor for a person's wishing to hasten death (Monforte et al., Reference Monforte, Crespo and Rodríguez2018), which suggests great suffering for that person. Although there are ethical challenges when preserving dignity at the end of life, for example regarding inadequate organization for good palliative care (Brodtkorb et al., Reference Brodtkorb, Skisland and Slettebø2016), healthcare must assist in trying to prevent people from encountering such suffering. This can, for example, be managed by using relevant outcomes. Further, if healthcare does not give focus to outcomes within “Themes related to the Social Dignity Inventory,” for example, empathy, there may be a risk of increasing a person's suffering. It has been stated that insufficient empathy can create a poor connection between the nurse and the patient (Cross, Reference Cross2019). Patients have described empathy as a response that acknowledges and attempts to understand an individual's suffering (Sinclair et al., Reference Sinclair, Beamer and Hack2017). Moreover, both empathy and compassion have been reported by patients as having a positive effect on their care experiences (Sinclair et al., Reference Sinclair, Beamer and Hack2017). Attentive nursing care, including paying attention to the person's expressed emotions and narratives, is valuable for providing comforting care (Höglander et al., Reference Höglander, Eklund and Eide2017). Thus, outcomes within the cluster theme “Themes related to the Social Dignity Inventory” must be considered and studied to a greater extent than they have been studied thus far; otherwise, we cannot expect persons’ dignity to be well maintained.
In this review, rare outcomes have been identified, such as “gratitude” and “empowerment.” As palliative care is often associated with suffering and grief (Chochinov et al., Reference Chochinov, Kristjanson and Hack2007; Aoun et al., Reference Aoun, Breen and O'Connor2012), identifying these outcomes may present researchers with a challenge to consider investigating outcomes that are not too obvious. It has been recognized that with a grateful attitude, people may become less fearful of death because they may have a sense that life has been well lived (Lau and Cheng, Reference Lau and Cheng2011). Persons with palliative care needs have also reported feeling appreciative about their accomplishments and about important people in their life (Hall et al., Reference Hall, Goddard and Speck2012), supporting the idea that gratitude could be an important outcome for them. Furthermore, empowerment has been defined as “a process of promoting and enhancing people's ability to meet their own needs and to mobilize the resources necessary to feel control over their lives” (Roos et al., Reference Roos, Silén and Skytt2016, p. 2). It has been described that a sense of control contributes to enhancing a person's dignity (Guo and Jacelon, Reference Guo and Jacelon2014), and perceived loss of control is a risk factor for losing dignity (Monforte et al., Reference Monforte, Crespo and Rodríguez2018). Consequently, empowerment is an important outcome to study when caring for persons with palliative care needs. Relatives and healthcare professionals have responded about the importance of “empowering” patients (McClement et al., Reference McClement, Chochinov and Hack2007; Johnston et al., Reference Johnston, Östlund and Brown2012; Montross et al., Reference Montross, Meier and De Cervantes-Monteith2013), while persons receiving dignity-conserving care have reported having gained “new insights” (Hall et al., Reference Hall, Goddard and Speck2012) and having the “motivation to achieve things” in the time they have left (Hall et al., Reference Hall, Goddard and Speck2013).
The findings of this review surprisingly do not include distinct outcomes of “communication,” although it was studied on an individual item through the SISCS10. Communication has been highlighted in previous studies (Johnston et al., Reference Johnston, Larkin and Connolly2015b; Werkander Harstäde et al., Reference Werkander Harstäde, Blomberg and Benzein2017) that have reviewed dignity-conserving care actions and have indicated that it is central to this type of care. Further, as poor communication can have a negative effect on a person's dignity (Guo and Jacelon, Reference Guo and Jacelon2014), this outcome must be considered when evaluating dignity-conserving care. Due to the lack of concrete communication outcomes in this review, an exploration of communication must in the future receive more attention and must be given equal emphasis in care and research. Not evaluating this outcome could jeopardize the delivery of high-quality care, as communication skills are required for dignity-conserving care (Johnston et al., Reference Johnston, Papadopoulou and Östlund2017b).
In summary, researchers can use this review for guidance while aiming to evaluate dignity-conserving care. The recommendation is to use outcomes presented within each cluster theme to receive a broad overview of a person's situation.
Limitations
Integrative reviews play an important role in evidence-based practice for nursing care (Whittemore and Knafl, Reference Whittemore and Knafl2005). This study used an integrative approach to include studies with different designs and methodologies. We do not claim to have included all relevant articles on the subject, but we used four databases and performed a manual search, which provided an extensive base of articles to explore. The search strategy included many doublets, indicating saturation. Trustworthiness was enhanced by using inclusion and exclusion criteria to identify relevant studies, as well as by discussions among all researchers about the criteria. Sometimes articles did not use the term “dignity-conserving care” but instead referred to “an intervention to enhance dignity.” These articles were also included as there still are not many dignity-conserving care interventions, and it was thought that they might provide valuable information.
Because our aim was not focused on designs or finding effects, a critical appraisal of articles was not accomplished. There is no agreed standard as to when to perform a critical appraisal of the quality of articles; according to Whittemore and Knafl (Reference Whittemore and Knafl2005), the quality appraisal should be done if fulfilling a meaningful purpose. It is most likely that a type 2 error (where real effects cannot be found even though they, in fact, exist) was made in several of the included studies. This proves that more studies with a more robust study design and including more participants are needed if effects are to be identified. For ethical considerations (Holstein et al., Reference Holstein, Parks and Waymack2011), articles only focusing on persons with dementia were excluded, as these persons can be considered as too frail and dignity-conserving care often includes reflective conversations requiring the ability to think clearly and to process dialogues.
Moreover, we found it challenging to assign some of the outcomes to an appropriate theme because outcomes often overlapped. This may be due to the complexity of the palliative care context; and according to Alvesson's (Reference Alvesson2017) themes in an analysis, cannot always be completely isolated.
Conclusions
Consideration of relevant outcomes is central to implementing new interventions. It is hoped that this study can be an important source for researchers evaluating dignity-conserving care, inspiring them to use a broad approach of outcomes or outcomes within “Themes regarding Overarching Dignity Issues.” Over and above outcomes within “Themes related to Illness-Related Concerns,” there is a need to give an equal and enhanced focus to outcomes within cluster themes “Themes related to the Dignity-Conserving Repertoire” and “Themes related to the Social Dignity Inventory” to increase or maintain the dignity of a person with palliative care needs. An increased focus on “Communication outcomes” within dignity-conserving care is highly desirable to help improve the care provided within palliative care today.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1478951520000139
Acknowledgments
The authors thank the Research School of Successful Ageing at Örebro University, Örebro, Sweden, which funded the research time of the first author Annika Söderman. The authors also thank Professor Eva Benzein for valuable input in planning this review.
Conflict of interest
The authors declare no conflict of interest.
Author Contributions
All authors took part in the study conception, design, drafting of the manuscript, writing, and final editing of the manuscript. The first and last author (A.S. and K.B.) were responsible for most of the data collection, while the first and second author (A.S. and U.Ö.) took main responsibility for the data analysis. All authors were involved in critical revision of the manuscript for important intellectual content.












