Effective suicide prevention initiatives rely on identifying factors involved in vulnerability and risk and provide opportunities for intervention. Although addiction and misuse of alcohol, prescriptions and illicit drugs are key risk factors for suicide, Reference Brady1–Reference Walsh3 the interaction between lifetime substance misuse and misuse at death is less well-documented. To develop and implement successful interventions for suicide prevention, it is important to know what role substance misuse and impaired reasoning and perception play, not only as integral to the life of an individual, but also at the time of considering and acting on suicidal thoughts. Reference Cherpitel, Borges and Wilcox4,Reference Hufford5
Illicit substance misuse is strongly associated with suicidal acts, even when the method does not involve drug overdose. Reference Darke, Duflou and Torok6 Moreover, dependent substance misusers record higher prevalences of all major risk factors for suicide than the general population, Reference Darke, Duflou and Torok6 in the forms of psychopathology, family dysfunction, social isolation, and lower socioeconomic status. Reference Conner, Houston, Swogger, Conwell, You and He7–Reference O'Reilly, Rosato, Connolly and Cardwell9 One UK study Reference Jones, Gruer, Gilchrist, Seymour, Black and Oliver10 indicates that drug overdose deaths among drug misusers feature frequent contacts with services in the months leading up to the deaths, along with a high incidence of suicidal ideation and previous suicide attempts. However, this study was limited to drug overdose deaths alone, excluding hanging, which forms the majority of suicide deaths. Further to existing evidence on illicit drug misuse, combined alcohol and polydrug use in recreational settings has become a cause for concern in recent years. In the USA, it is estimated that 10% of the population are affected by alcohol or illicit drug use, with approximately 2% (3.2 million individuals) experiencing problematic polysubstance misuse. Reference Akbar, Baldacchino, Cecil, Riglietta, Sommer and Humphris11
The Adult Drinking Pattern survey reports that 23% of the Northern Ireland population drink more than the weekly drinking limits (with 18% described as hazardous drinking and 5% as harmful – the latter equating to alcohol dependence). Of those adults who drink alcohol (74%), 30% engage in at least one binge-drinking episode per week. 12 The Northern Ireland Crime Survey 2008/2009 reported a 3.8% prevalence for illegal drug use: here survey respondents had been asked whether they had ever taken diazepam/Valium which was not prescribed by a doctor. Reference Toner and Freel13 In contrast to the Drug Prevalence Survey findings which indicate higher use of sedatives and tranquillisers in women and older adults, the National Advisory Committee on Drugs (NACD) and Public Health Information and Research Branch (PHIRB) have reported that non-prescribed tranquilliser use was more common in men and younger age groups. 14 The Drug Misuse Database collects information on those presenting for treatment for their drug misuse (including those receiving services in prison). The latest report shows that 61% of drug users took two or more drugs. This proportion has been increasing again in recent years, up from 51% in 2009/2010 when it was at its lowest. Reference Hagell15
The UK-based Association for Young People's Health recently reported an increase in young people help-seeking for polydrug misuse. Reference Hagell15 Alcohol and drug use (both prescription and illicit) play a significant part in suicide in Ireland. Reference Tormey, Srinivasan and Moore16 A recent study detected drugs in 48% of cases of death by hanging with alcohol featuring in 55% of all suicides. Reference Tormey, Srinivasan and Moore16 Missing from this analysis was any link to drug and alcohol misuse prior to the suicide event. Therefore, although the existing knowledge base provides a clear picture of the relevance of substance misuse to suicide deaths, there remains a lack of appropriate data linkage for closer examination of the relationship between drug and alcohol misuse in life and at time of death. Matching general practitioner (GP) record data with standardised toxicology screening may support the development of interventions to prevent suicide.
Method
Data collection
We examined all deaths in Northern Ireland determined to be suicide by the Coroners Service for Northern Ireland between 1 March 2007 and 28 February 2009. Data collection was carried out between January and November 2011, initially from the Coroner Service for Northern Ireland (CSNI) and linked to associated data extracted from GP records. Two researchers extracted this data and a comprehensive database was established in SPSS. To ensure interrater reliability, 10 CSNI files and 10 GP records were initially examined by both researchers (K.G. and S.M.), followed by discussions to ensure that the variable label definitions were robust. Additional methodological details have been published elsewhere. Reference Mallon, Rosato, Galway, Hughes, Rondon-Sulbaran and McConkey17
Data preparation
Histories of help-seeking for substance misuse were extracted from the GP records. Because of the lack of standardisation in GP terminology classifying this information proved a challenge – for example, terms included: history of alcohol misuse; alcohol dependency syndrome; heavy drinker; substance dependence; ‘benzo addiction’; addicted to painkillers; and opiate dependence. Although it was not possible to consistently classify substance misuse as either a current or historical issue, reference to relapse of historical substance misuse appeared frequently, although not in a systematic manner suitable for coding. For this analysis, both the alcohol and drug misuse data were (separately) summarised into two dichotomous variables noting any form of help-seeking for either alcohol misuse or substance misuse (prescription or illicit drugs). For this reason, the term substance misuse necessarily encompasses substance dependence throughout the paper.
Evidence of alcohol and substance misuse at the time of the suicide were obtained from the pathology report in the coroner records. Blood alcohol levels were dichotomised according to the drink-driving limit (>80 mg per 100 ml). In line with the literature, this cut-off represents an accepted standard level defining impaired cognition and functioning. Reference Cherpitel, Borges and Wilcox4 Where blood toxicology screening was carried out, the pathology report listed any detected substances (either illicit or prescription drugs) with a note referring to whether or not the detected levels of prescription drugs fell within the ‘therapeutic range’ – a value generated after accounting for the list of current medications prescribed to the individual by their GP. By this, a dichotomous variable signifying drug misuse was generated with values: none detected; or non-therapeutic levels of prescription drugs or any level of illicit drugs detected.
Other variables included in the analysis were: presence of a mental health diagnosis; whether or not there had been previous suicide attempts; indication of a history of help-seeking for alcohol misuse; history of help-seeking for substance misuse (prescription and illegal drugs); treatment status at death; locale of residence (whether urban or rural); whether or not the individuals were prescribed drugs at the time of death; and method of suicide (hanging, overdose, other).
Fifty-four per cent of the deaths (218/403) were subject to drug toxicology screening. The pathologist can use discretion in making any decision to order toxicology screening – this was based on information obtained from the police, witness reports and evidence gathered from the scene (for example, whether the individual was known to misuse substances or whether prescription drugs were found). Procedurally, an additional factor in the decision to order a toxicology screening has been the time-lag for toxicology results to be provided by the laboratory. In England, Wales and Northern Ireland, the decision is also ‘subject to the authority of the Coroner who may feel that such investigations may not be necessary to assist in the determination of the cause of death’ (J. Crane, personal communication, 2014). Almost half the cohort was not subject to toxicology screening for substance misuse beyond alcohol, therefore, we examined the characteristics of those who were subject to toxicology screening for substance misuse to explore the relationship between drug misuse in life and in death by suicide. It is important to examine the differences between those who were screened and those who were not, to assess any patterns involved in the decision to screen, beyond the reported circumstances of the death.
Statistical analyses
Descriptive statistics are presented, including chi-squared tests for significant differences between groups within the cohort (bivariate analyses). Significant variables were entered into a logistic regression model (multivariate analyses) to assess the relevance of individual characteristics to the decision to screen for misuse of substances at the time of death.
Ethical approval
Ethical approval for the study was obtained from the UK Office for Research Ethics Committees Northern Ireland (ORECNI), with access to personal confidential data in both the coroners' records and the GPs' records granted via the ‘research exemption’ within Section 33 of the Data Protection Act 1998.
Results
Characteristics of the cohort
Individual characteristics of the 2-year cohort (n = 403) are described below. GP records were available for 90% (361/403). There were no significant differences by age or gender between those with available or missing GP records. Of the main cohort: males comprised 81% (325/403); age ranged between 11 and 83 years (with a mean of 39); 49% (196/403) were either married or cohabiting; 38% (155/403) were in paid employment; and 40% (161/403), 28% (111) and 32% (129) lived in urban, rural and intermediate areas respectively. In relation to health service access, 41% (148/361) had not been diagnosed with a mental health problem and 46% (167/361) were not in receipt of any secondary or tertiary health service treatment at the time of death. However, 82% (209/361) had consulted with the GP in the 12 months prior to the suicide, and of these 71% (209/296) had presented with mental health concerns. Overall, 50.4% (182/361) were in receipt of mental health-related prescriptions and 50% (181/361) recorded more than six consultations, with a mean of 5.7 for the help-seeking group (296/361).
Table 1 records the levels of help-seeking for alcohol and drug misuse problems in the cohort for (a) the 12 months prior to the suicide (23.6%, 84/356 and 12.8%, 46/360 respectively), (b) and over the lifespan (33.4%, 120/359 and 22.2%, 80/360 respectively).
Table 1 History of substance misuse help-seeking at general practice (n = 360)

| n | % | |
|---|---|---|
| Lifetime history of alcohol misuse help-seeking | ||
| Yes | 120 | 33.4 |
| No | 239 | 66.6 |
| Lifetime history of drug misuse help-seeking | ||
| Yes | 80 | 22.2 |
| No | 280 | 77.8 |
| Last 12 months help-seeking for alcohol misuse | ||
| Yes | 84 | 23.6 |
| No | 272 | 75.8 |
| Last 12 months help-seeking for drug misuse | ||
| Yes | 46 | 12.8 |
| No | 314 | 87.2 |
Blood alcohol reporting
All suicides – except a small number (four) where there was a significant time-lag between the suicide and either the death or the pathological examination of the body – were subject to blood alcohol examination. Overall, 51.6% (204/395) of the cohort tested positive for blood alcohol (with 93% of these recording levels >10 mg per 100 ml): of these, 39.2% (155/395) were over the UK drink-driving limit (80 mg/100 ml), with 27.1% (107/395) at more than twice the UK limit. Of those over the limit, 36.1% (56/155) had sought help for an alcohol-related problem in the 12 months prior to death. Figure 1 records the relationship between help-seeking for alcohol problems over the lifetime and the presence of alcohol at the time of the suicide. Of those over the limit 47.1% (64/136) had visited the GP for an alcohol-related problem, whereas 52.9% (72/136) had never sought such help. Of those not over the limit, 75.1% (166/221) recorded no history of help-seeking for alcohol misuse, whereas 24.9% (55/221) did. However, perhaps surprisingly, a smaller minority had sought help over concerns about alcohol misuse in the 12 months prior to death (10%; 22/221).

Fig. 1 Suicides in Northern Ireland (March 2007–February 2009): blood alcohol levels at the time of death, linked to lifetime help-seeking for alcohol misuse
Toxicology reporting of prescription and illegal drug misuse
Figure 2 records the relationship between toxicological screening for drug misuse at the time of the suicide and help-seeking for drug misuse over the lifetime: 37.6% (70/186) of those screened recorded positive results for drug misuse at the time of death. Of these 65.7% (46/70) did not seek help for drug misuse over their lifetime, whereas 34.3% (24/70) did. This relationship is mirrored to a large extent among those who tested negative for misuse: 24.1% (28/116) and 75.9% (88/116) respectively for those who did and did not seek help.
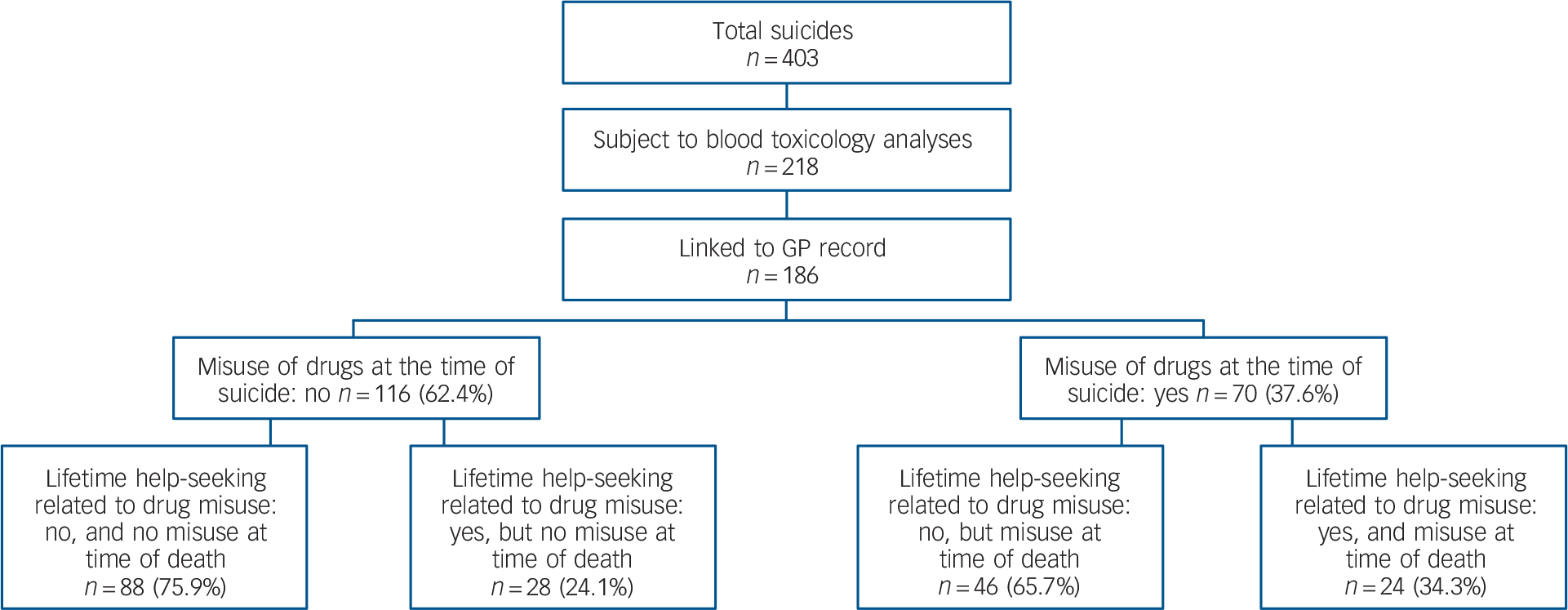
Fig. 2 Suicides in Northern Ireland (March 2007–February 2009): toxicology screeninga at the time of death, linked to lifetime help-seeking for drugs misuse.
GP, general practitioner.
a. A positive toxicology result is characterised either by the detection of illicit substances or the presence of prescribed substances used over and above the prescribed therapeutic level.
b. Results are for coroner's files and GP records combined.
Determinants of toxicology screening
Of the 403 suicide deaths, 54% (218/403) had been subject to blood toxicology testing. We found no differences in the likelihood of testing for gender, number of drugs prescribed, treatment status at death, mental health diagnosis, history of help-seeking for alcohol misuse, degree of rurality or prior suicide attempts. However, people with a recorded history of help-seeking for drug misuse (as reported by the GP) were more likely to be screened (χ2 (1 d.f., n = 360) = 11.5, P = 0.01), as were younger people. As age increased, toxicology screening was less frequently performed (χ2 (3 d.f., n = 403) = 28.6, P<0.01). In addition, the method of suicide was associated with the likelihood of screening. As expected, overdoses and ‘all other’ methods were screened more often than hangings.
Table 2 records (for those with GP records) the odds ratios (ORs) associated with factors thought to influence post-suicide blood toxicology screening in the cohort: these include gender, age, method of suicide and history of drug use. The pseudo-R 2 value (Nagelkerke R 2 = 0.21) indicates that the model is unlikely to explain more than 20% of the variance (e.g. toxicology screening carried out = yes, no). Death by drug overdose was the strongest predictor of blood toxicology screening (OR = 13.73: P<0.01, 95% CI 3.03–62.33). A history of drug misuse (OR = 2.05: P = 0.02, CI = 1.14–3.70) and age remained significant predictors: as age increased, the likelihood of toxicology screening dropped (Fig. 3) – with those aged 65+ one tenth as likely to be screened when compared with those less than 25 years (OR = 0.09: P<0.01, CI = 0.03–0.26).
Table 2 Logistic regression model predicting the odds of a toxicology report being carried out (n = 360)

| Variables in the model (pseudo-R 2 = 0.21) | Odds ratio | P | Significance | 95% CI |
|---|---|---|---|---|
| Gender | ||||
| Female | 1.00 | |||
| Male | 1.34 | 0.33 | 0.74–2.41 | |
| Age, years | ||||
| <25 | 1.00 | |||
| 26–44 | 0.28 | <0.01 | ** | 0.14–0.55 |
| 45–64 | 0.16 | <0.01 | ** | 0.08–0.33 |
| >65 | 0.09 | <0.01 | ** | 0.03–0.26 |
| Drug misuse | ||||
| No record by GP | 1.00 | |||
| Record of drug misuse | 2.05 | 0.016 | * | 1.14–3.70 |
| Method | ||||
| Hanging | 1.00 | |||
| Overdose | 13.73 | <0.01 | ** | 3.03–62.33 |
| Other | 1.83 | 0.05 | 0.99–3.35 | |
**, significant to P<0.01; *, significant to P<0.05.

Fig. 3 (a) Likelihood of toxicology results being requested by age. (b) Detection of substance misuse at time of death by age.
Among those cases for which a toxicology report was available, we examined the results of the screening to ascertain whether the chances of a positive result differed according to age. Almost two-thirds (61.3%) of the tests were negative (that is, the quantity of drugs detected was within therapeutic range) with no significant difference across age. Figures 3(a) and (b) show that although age is a predictor of toxicology screening being carried out (suicide deaths are significantly less likely to be screened for blood toxicity, as age increases), it appears that there is no difference in the detection of misuse of prescription drugs or illegal drugs across age groups (χ2 [6 d.f., n = 218] = 3.08, P = 0.80).
Discussion
As part of a larger research initiative, this paper examines the relationship between substance misuse in life and misuse at death in a cohort of 403 suicides occurring over 2 years in Northern Ireland. This is the first time in a UK setting that primary care help-seeking data for lifetime substance misuse has been linked to toxicology reports of substance misuse at the time of the suicide.
The frequency of substance misuse (of alcohol, prescription drugs and illicit substances) at suicide in this cohort reflects earlier research. Reference Cherpitel, Borges and Wilcox4,Reference Tormey, Srinivasan and Moore16 Findings relating to alcohol showed a pattern of help-seeking in many of those who recorded significant alcohol levels at death. However, the relationship between substance misuse in life and misuse at death is not correlated to the degree that might have been expected. The overlap between histories of help-seeking and substance misuse is not simple: some of those with a history of substance misuse show no evidence of use at the time of death, and some with no history of help-seeking record positive results at death.
The negative blood results at the time of death among those with a history of help-seeking have implications for the frequently sited role of reduced inhibitions and impulsivity as mechanisms associated with substance misuse as a risk factor for suicide. Reference Lamis and Malone8,Reference Pompili, Serafini, Innamorati, Dominici, Ferracuti and Kotzalidis18–Reference Conner and Duberstein20 Some mechanisms associated with substance misuse as a risk factor for suicide may remain even in periods of abstinence. Mediating factors such as personality traits, life events and comorbid (potentially undiagnosed) mental health problems are relevant, particularly where the substance misuse may have provided emotional regulation. Reference Conner and Duberstein20 This requires further investigation. The positive toxicology results coupled with a history of associated help-seeking suggest that, despite help-seeking, there may be unmet need that could be addressed more effectively by services. Support services that can communicate, integrate and facilitate concurrent approaches to treatment of comorbid mental health problems and substance use disorders would be an ambition worth pursuing.
Regarding those who had misused substances at the time of death but had no history of help-seeking, a proportion will have selected misuse of available medications as an opportunistic method of choice for suicide, Reference Sinyor, Howlett, Cheung and Schaffer21 and may have no history of substance misuse; others may have accessed an alternative source of support or they may not have recognised their needs, therefore not yet sought help. Population-based data suggest a significant time lag of 16 years (median) in seeking treatment for alcohol misuse in the Northern Ireland context. Reference Bunting, Murphy, O'Neill and Ferry22
The primary limitation of the data is that pathology results for use and misuse of prescription and illicit drugs at the time of death were only available for approximately half the cohort: no information was available for 46% of suicides occurring in Northern Ireland. Compounding this limitation is the apparent bias in ordering blood toxicology analysis: although young people are over three times as likely to be screened for illicit substance misuse than those in middle age (45–64 years), they are perhaps slightly less likely to have misused prescription or illicit drugs. A second limitation concerns the possibility that some of the cohort had experienced substance misuse problems but did not seek help from their GP (and therefore this ‘misuse’ will be lost to the current analysis). This is likely to be particularly relevant to illicit drug misuse, because of associated criminality and fear of exposure or stigma. Reference Gilchrist, Moskalewicz, Slezakova, Okruhlica, Torrens and Vajd23 The analysis uses a binary classification for reported substance misuse where, for example, a trace of cannabis and a non-therapeutic level of prescribed medication are classified similarly, when in reality they are likely to produce different levels of impaired reasoning and perception. This classification means that we are unable to quantify the misuse or the impact it may have had on the circumstances surrounding the death. However, assessing reasoning and perception, to include for example reduced inhibitions and impulsivity due to substance misuse, in a suicide cohort is confounded by not only polydrug use but also pre-existing mental health problems.
Two important points emerge from this study. First, to capitalise on prevention programmes that address the role of alcohol and substance misuse in suicide it is important to better understand the mediating factors involved in substance misuse and suicide, including the role of impaired reasoning and perception at the time of a suicidal act. Second, this information must be considered in the context of existing concerns about prescription, alcohol and illicit drug misuse over a person's lifetime, in relation to intervening where suicidal thoughts are pervasive.
It is also important that the potential role of polypharmacy in suicide is explored and considered, particularly in relation to the psychoactive chemicals used in psychiatry, which affect the state of a person's emotional faculties at the time of a suicide attempt. Reference Moncrieff24 In this cohort, high levels of psychiatric polypharmacy were observed requiring further analyses. Such analyses would be enhanced by the availability of blood toxicology results for all suicide deaths. However, there are notable contextual difficulties and challenges that result in these limitations on the data that is available. In Ireland, professional guidelines for pathologists state that every death by suicide should be subject to toxicology screening. Reference Tormey, Srinivasan and Moore16 There are no similar guidelines in the UK. Neither jurisdiction is subject to specific guidelines that would target the almost unlimited number of drug and poison analyses that could be carried out. Importantly, the Irish guidelines 25 suggest that such analyses should be mandatory where the cause of death cannot be clearly established from the post-mortem. Herein lies a fundamental difficulty in the use of coroners' data as a tool for developing interventions for the prevention of suicide.
The task of the coroner is to determine cause of death. This is reflected in the increased frequency with which toxicology screening is ordered in the case of suspected overdose. In hangings (the method used in 76% of suicides in this cohort), the biological cause of death is asphyxiation, and within an exclusively medical approach to cause of death the associated sociopsychological context surrounding suicide may be diminished. Reference Tormey26 For example, despite expectations to the contrary, a prior suicide attempt (particularly drugs overdose) did not independently predict the ordering of a toxicology report. Thus, previous behavioural actions related to intent to die do not feature in the decision to order toxicology screening because they are largely irrelevant to the cause of death. As a result of this procedural convention, the full extent of substance misuse in the psychosocial sequelae of suicide remains unknown. To make best use of the information collected when a suicide occurs, a sea change in medical forensics may be required, to realign the process towards a biopsychosocial model for examining and understanding suicide.
Acknowledgements
The authors thank the Coroner's Service for Northern Ireland and Health & Social Care (HSC) Business Services Organisation for their help in accessing the data analysed in this paper. We also thank NIAMH (Northern Ireland Association for Mental Health) for their support of the study. The analysis and opinions expressed represent the views of the authors. The funders and those who provided access to the data had no role in the study design, data analysis, decision to publish or preparation of the manuscript.








eLetters
No eLetters have been published for this article.