Public hospitals provide medical assistance to specific communities and a defined geographic region, serving its entire population. Unlike private hospitals, general hospitals must provide care to all patients and always maintain their main objective to treat people, both during routine operation and during an emergency and a disaster. Whether the disaster is natural or human-caused, the hospital’s operation level must be adapted to new demands that may involve approaches and resources that are not required during a routine operation. 1
A hospital’s operating modes can be categorized as routine, mass-casualty, and interim states that require procedures and resources exceeding those of routine operation. In times of disaster, new medical needs can arise, depending on the nature of the event. For instance, during wartime, the majority of patients seeking hospital facilities present with weapon injuries or collapsing infrastructure injuries. In a bioterrorism event, infectious diseases are rampant, requiring the medical teams to both treat patients and attempt to prevent further spread of the contagious agents. Regardless of the nature of the event and the needs, the medical staff must be prepared for a sudden increase in demand for service that could overwhelm the functional capacity and safety standards of the hospital. 2
The hospital is obligated to fulfill 2 goals: First is to be able to sustain itself against the sudden rise in demand for medical support, and aid given depends on the nature of the disaster. The second goal is to continue support for patients already hospitalized 2 and for others arriving at the hospital, regardless of the disaster. The importance of the second goal may decrease if the disaster escalates, at which point staff could consider outsourcing the care of non-critical patients to appropriate alternative treatment sites (eg, home care for low severity illness and chronic-care facilities for long-term patients). The aim of this paper is to describe the principles and the methods for hospital operation in the event of a disaster-level event. We describe the structure and methods for handling prolonged disaster-level events and the adjustments that can be made in the case of lower intensity events.
Every resident of Israel benefits from health care that is insured under the National Insurance Law, which determines a uniform health services, provided by 4 sick funds. The Israeli hospital system consists of governmental hospitals, public hospitals, and hospitals belonging to sick funds, which provide medical services to patients according to contracts with the sick funds. Private hospitals in Israel do not have emergency departments and treat patients in outpatient settings only. With the exception of private hospitals, all hospitals must continue functioning during a sudden influx of patients, especially wartime, and therefore regularly prepare for such disasters, with government and Home Front Command (HFC) support; the command is responsible for civil defense: preparing the civilian population for a conflict or disaster, assisting the population during the crisis, and contributing to post-crisis reconstruction.
This paper aims to describe the principles of general hospital operation in the event of a disaster-level event, the methods to be applied during prolonged disaster-level events, and the adjustments that can be made in the case of lower-intensity events.
MEDICAL SURGE-RELATED CHALLENGES THAT A HOSPITAL MIGHT FACE
Every general hospital must be able to enlarge its patient capacity on short notice to absorb an abrupt increase in demand. Reference Berger, Körner and Bernstein3 A mass-casualty event can differ from 1 region to another and can be natural, accidental, or human-caused. Examples of such events include aerial traffic accidents, mass exposure of harmful chemicals, bioterrorist attack, military conflicts, and natural disasters such as earthquakes, hurricanes, and floods. In such situations, absorbing and treating the sudden flux of casualties evacuated from the disaster area become the hospital’s main challenge. Reference Berger, Körner and Bernstein3 The extension of patient capacity on short notice demands switching to an operation mode that enables admitting and treating a high number of new patients in a short period of time. In another scenario, for example, war zone or earthquakes, the hospital itself might be damaged by the disaster. Reference Merrill, Orr and Chen4 In such a case, as long as the medical center is still operational, it is duty-bound to continue treating those already in its care, as well as those needing assistance in the surrounding area. In consideration of this possibility, Israel’s hospitals have been reinforced against missile attacks to enable continual activity. Reference Shasha5 Maintained hospital functionality in such scenarios can be challenging Reference Gallagher, Richardson and Forbes6 and largely relies on administrative skills and preparedness of hospital executives to lead and find solutions for unexpected and constantly arising challenges.
MANAGEMENT OF EMERGENCY CHALLENGES AT ZIV MEDICAL CENTER
Ziv Medical Center (ZMC) 7 is the northernmost publicly funded hospital in Israel. It is located in Safed, close to both the Syrian and Lebanese borders (30 km and 11.2 km, respectively; Figure 1). 7 ZMC personnel has extensive experience with both wars and mass-casualty emergency incidents. The hospital staff treated roughly 1600 soldiers and civilians during the 2006 Lebanon War, during which the medical center was hit directly by a missile fired by enemy forces. 8 Despite this, it continued functioning throughout the 33-day course. ZMC staff treated more than 1500 wounded Syrian refugees with multi-trauma war injuries. Reference Zarka and Lerner9

FIGURE 1 Ziv Medical Center in the North of Israel.
ZMC serves more than 250 000 residents of the Upper Galilee and the Golan Heights. 7 Its patients tend to be of a lower socioeconomic status, who benefit from publicly funded health care. Its geographic location is a high-risk earthquake region Reference Zaslavsky, Shapira and Arzi10 and is vulnerable to bad weather (such as snow) and lacks evacuation routes. ZMC’s proximity to enemy borders demands that the hospital staff be ready for several possible mass-casualty scenarios, such as wars and chemical attacks. In addition, the proximity of ZMC to the war zone in Syria makes it the default evacuation destination for refugees, some of them with severe injuries, and mass-casualty incidents from the Syrian Civil War. The geographic location of ZMC in Safed in the north, on a mountain, makes the hospital and its area vulnerable to bad weather (such as snow) with a lack of evacuation routes.
The staff must be prepared and trained to implement 1 of many disaster plans, dictated by the nature of the event. Maintaining efficient and effective functionality during a crisis proves to be a challenge not only for the medical staff, but for the administration as well. For this purpose, an established system needs to be in place for handling events of all kinds. The system must follow clear protocols and still be sufficiently flexible to address unique and unexpected challenges that may arise. Before discussing the system’s more flexible aspects, the threats and needs common to different disaster types will be discussed.
THE CONSTANTS BETWEEN DIFFERENT EVENTS
A hospital’s main mission at any time is to supply medical support to those in need. As a disaster unfolds, a gap between the available and the necessary resources evolves as the hospital switches its mode of operation. The priority in times of emergency is to adapt to the situation and appropriately allocate resources in order to close that gap as soon as possible. Reference Zaslavsky, Shapira and Arzi10
In any single mass-casualty event, the first-response requires a collection of information concerning the nature of the crisis, the estimated number of casualties, the severity of their condition, and the exact time and location of the event. This information is then used by the medical staff to evaluate the new demands, prepare the hospital, and estimate the time necessary to transport the casualties to the hospital. Because an ongoing event is dynamic in nature, the allocation of resources must be continually reassessed and adjusted accordingly.
Thereafter, the staff’s capabilities to meet the demands presented by the specific event must be evaluated. These capabilities differ if disaster strikes in the middle of the day versus at night or on the weekend. For example, in trauma, blood supply is critical to the treatment of casualties, but it is not as necessary in the case of bioterrorism.
A system has been created at ZMC that is not dependent on the nature of the event and includes specific units that can be adapted to suit different complications. This system comprises 5 separate units that are overseen by the Board Table: the Hospital Multi-Component Emergency Center (HMCEC).
THE HOSPITAL MULTI-COMPONENT EMERGENCY CENTER
The HMCEC (Figure 2) is ZMC’s 5-unit mass emergency response system created to manage mass-casualty events of all scales and types. When an unexpected incident occurs, the hospital director (HD) activates the HMCEC and recruits the entire staff assigned to the different units. The system enables first-responders to divide a mass-casualty event into smaller, well-defined missions that can be handled by separate teams of specialists. Each has its own duties and contributes uniquely to the achievement of the hospital’s stated mission.
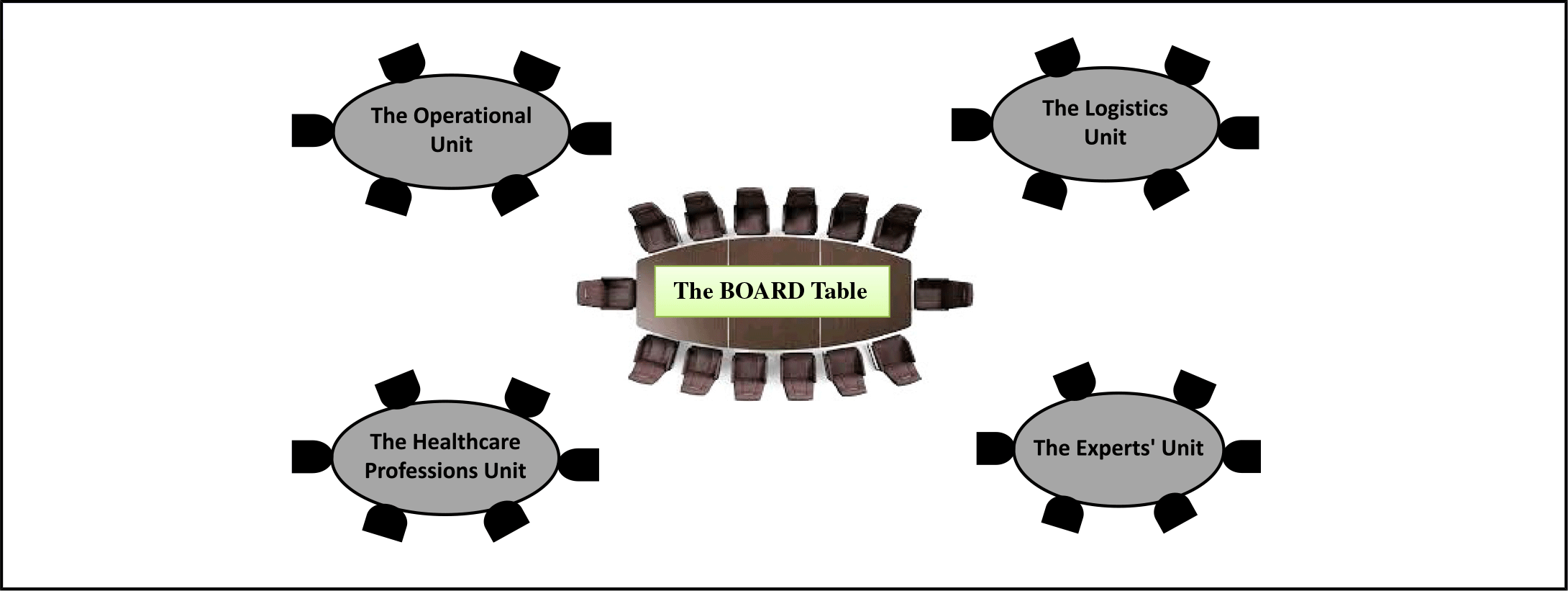
FIGURE 2 Diagram of the HMCEC at Ziv Medical Center.
The HMCEC Units
-
1. The Board Table: The central unit of the HMCEC, comprising the hospital’s board, which convenes to set priorities and to execute HD decisions.
-
2. The Operational Unit: Deals with medical and professional aspects of an emergency event and allocates professional staff as necessary.
-
3. The Logistics Unit: Deals with logistics demands and provides additional staff.
-
4. The Health Care Professions Unit: Deals with hospital laboratories and pharmacy, and other services directly supporting the relief efforts.
-
5. The Experts Unit: The role of this unit is dependent on the nature of the event and, as such, is the most flexible component of the HMCEC.
To simplify the operation in times of an emergency, the HMCEC is the only system activated by the ZMC administration. The assembled staff gathers in a protected location, with each unit having its own room as a base of operation. The units are connected by different command and control systems, such as phones, e-mail, and a command and control system that enables information to flow from the departments to the units and between the units and the Board Table.
The Board’s Roles and Structure
The board head (BH) is responsible for the different roles of the board. The first role is to evaluate the severity of the situation and to set priorities accordingly. In order to properly fill this role, the different units must provide the Board Table with the data and information necessary to draw a clear picture of the situation, the potential future scope of the event, and relevant issues and dilemmas to be resolved. The data are collected by the teams on-site and in the hospital, as well as by other corresponding organizations and services, such as the Israel Fire and Rescue forces, the Israel Police, the Israel Emergency Medical Services, and the HFC. When enough data have been collected and the scope of the disaster is fully understood, a plan of action for the immediate and near future is formulated (Figure 3).

FIGURE 3 Function of the Board.
When assessing the disaster, a list of the needs for the present disaster and possible future complications is prepared by the board members. Suggestions for conceivable solutions are discussed before being presented to the HD. Whatever decision that the HD makes becomes the plan of action and is delivered to the response teams. The head of the board is responsible for writing and publishing the plan of action in writing with precise, well-understood objectives and distributing it to the response teams. Later, follow-up board actions take place in order to confirm whether their decisions have been properly implemented. Besides dealing with the current problems, the BH has to consider new and future issues and suggest ways for resolving future challenges, in order to preserve the hospital’s functional continuity. The board acts continuously in a cycle of assessing and updating the status of the event, prioritizing decisions, and suggesting possible solutions to the HD. The plan of action might be amended and updated according to any changes made during the process.
The board comprises the HD, the deputy director, and the BH. Additionally, the Operational Unit, the Logistics Unit, the Health Care Professions Unit, and the Experts Unit all have representatives on the board. The hospital security, public relations, and communication units are also represented on the board. There are several external members on the board as well, including Ministry of Health (MoH) and HFC representatives. In Israel, publicly funded hospitals, such as ZMC, are under the authority of the MoH and must report to it regularly. As such, these 2 organizations are represented at the Board Table as well, in order to address gaps in resources to the proper authorities and coordinate with other hospitals and organizations during a disaster. 2 Because the hospital functions directly under the MoH, the board must regularly report its status. HFC supports the hospital in times of war and other emergencies, by law, and in certain situations even directing the hospital about protection and hospital missions. The HFC representative provides the board with information relevant to the hospital, supports it with manpower, and coordinates with the army and all other emergency services. In certain cases, representatives of the Israel Police, the Israel Fire and Rescue Services, and Israel Emergency Medical Services might sit at the Board Table as well. It is important to note that the board may take direct command concerning certain critical issues while cooperating with 1 of the units, often with the Operational Unit. For example, when an unusually high number of casualties arrive at the Emergency Department and the hospital cannot handle all of them, input is needed from the board for the solution. It would be more efficient for the Operational Unit to work directly with the board concerning this issue rather than wait for the board to come to a decision on its own. The board records and archives its decisions and activities for the debriefing process and possible reference, in case of a similar event in the future.
The Units
Each HMCEC unit operates separately. They can be located in the same building, but each is in a different room or in the same hallway but at independent stations.
The Operational Unit collects data about both the event and the hospital. More specifically, it collects data about the number, medical status, hospitalization necessities, and so on, of the casualties. The Operation Unit monitors the status (staff, number of patients, available beds, supply of medications, and so on) of the medical departments in the hospital. It constantly updates on the status of the hospital’s emergency departments and operation theaters. This group is also in charge of setting hospital admission and discharge criteria and prioritizing clinical and operational interventions, according to available treatment capacity and severity of the patient conditions. 2 It is important to remember that, besides the disaster’s immediate needs, the existing medical services offered by the hospital under routine operation (eg, emergency care, urgent operations, maternal and child care) are still operational as usual and need to be managed in parallel with the switch to the hospital’s emergency response plan. 2 As the responsibilities of this unit are key to the successful operation of the medical center, in times of intensive activity, for example, sudden arrival of a large number of casualties to the emergency room, the board may fill the unit’s role as well.
Depending on the situation and the size of the hospital, this unit can be divided into 2 smaller units, one dealing with operational matters and the other with staff allocation.
The Logistics Unit maintains infrastructure, establishes shelters, and distributes equipment and supplies to support the disaster relief efforts. This unit includes employment agency representatives to enable the smooth and rapid recruitment of additional workforce, as necessary, and other logistical services, such as engineering and maintenance, nutrition, water, fuel, laundry, cleaning, and waste management. The Logistics Unit obtains these resources from outside of the hospital, arranging transportation and coordinating supply lines. This unit reinforces structures for medical use. The unit must also handle all matters related to the staff, including availability, working hours, transportation, legal aspects concerning employee change in the case of a disaster, and care of children of staff members. 8
The Health Care Professions Unit includes representatives from different health care sectors, such as the hospital pharmacy, the laboratories, the blood bank, respiratory therapy, social workers, and X-ray technicians. This unit organizes the staff for the different needs, such as the allocation of social workers to comfort and support victims’ families and send others to occupy the information center 8 that provides anxious families with information about their loved ones. Moreover, it collects data from the distressed relatives about their missing loved ones. In addition, it monitors other critical resources, for example, blood supplies in trauma and antibiotics inventory in bioterror events.
The Experts Unit composition depends on the nature of the disaster. In the case of a bioterror attack, the experts would be specialists in infectious diseases. When the disaster involves the mass spillage of chemicals, different experts would be needed for different chemical agents. The role of this group is to assist in determining the hospital’s operation policy for diagnosis, treatment, exposure, and so on. The professionals comprising this unit provide advice to the staff according to the data gathered and according to instructions given by the MoH. The Experts Unit acts to learn from the current status and provides a new understanding of the situation through a professional perspective. When an emergency event is declared, the hospital’s director activates the HMCEC, and an evaluation of the situation begins. Suitable professionals are assigned to the Experts Unit. For example, in a sudden outbreak of a war, the Experts Unit studies the different types of injuries and extracts data from the casualties in order to learn the exact nature of the weapons used. The unit then transfers this information to the army, which can use this information for better preparedness and protection. If during the war, an event of a different type emerges, such as a chemical weapon strike, experts in diagnosis and treatment of such cases will be added to the unit. This group is the most flexible component of the HMCEC system, and it acts as the professional advisory committee to the hospital’s director.
The Interactions Between the Board Table and the Units
At ZMC, each unit has defined duties and goals and must manage these responsibilities and others according to the guidelines of the BH and the HD. As mentioned, all of the units have representatives on the Board Table in order to keep the board and the HD up-to-date with the status of the hospital, the disaster, and the actions taken. The board meetings are a simple and effective tool for the exchange of data and information between all of the separate units and the board. The decisions made by the Board Table are transferred as directives to the units, who then execute them on both the hospital grounds and at the disaster site. Feedback is then given to the board, including the actions taken, the effects they had on the hospital’s operation, and new challenges that arose.
The board must coordinate between the 4 units and assign new responsibilities according to the continuously updated assessment of the situation. The board meeting protocol is sent to all units with new directives, with each group managing its ongoing task list and keeping the board informed concerning the status of its current missions.
DISCUSSION
When an event escalates into an emergency, unexpected obstacles escalate with it and need to be resolved if a hospital is to function efficiently and effectively. With the nature of the crisis hard to predict, hospitals must always be prepared for any event, whether it is a war, a natural disaster, a terror attack, or any other scenario. The span of these scenarios depends on the country and its challenges. The first priority of any medical center during such an event is to provide medical support to those currently hospitalized within its walls, as well as to all new casualties. To ensure an effective response, the hospital must show proper care in planning for any kind of disaster. An indispensable part of this readiness is the system that enables the hospital’s administration to save as many lives as possible and to reduce disability in case of an emergency. ZMC, a hospital with much experience in dealing with emergencies, developed a system and a methodology to aid the hospital’s operation in any events of emergency and war alike. HMCEC is the only system at ZMC, allowing for a similar response structure over several types of events but still providing enough flexibility to make changes, depending on the nature of the event. Keeping the same system and the same general plan of action for any event helps the staff develop a method and terminology needed for such stressful events and builds trained, resilient, and capable teams. When this system is implemented in drills or during unfortunate events, the staff is prepared to face different challenges using the method and structure to handle them effectively. The flexibility of the system allows the board at ZMC to make the necessary changes in order to adapt to any event. Currently, ZMC staff has not faced the emergency needed to test the model in the field in their area. They performed drills simulating war situations in the Galilee area, as well as drills simulating bioterrorism and chemical weapon attacks. ZMC staff continues to implement the HMCEC method during training and reports that this system enables them to manage different scenarios effectively. With the sole aim of saving lives and providing medical support to all in need during catastrophes, the HMCEC could very well be the system necessary to help achieve that very mission. This system provides the administration of the hospital with several advantages in handling such a catastrophe:
-
1. Clear and defined responsibilities for different subgroups (units)
-
2. Division of the mission into submissions, delegated to each subgroup
-
3. Creation of expertise in specific aspects of emergency challenges
-
4. Simultaneous tackle of various aspects of the disaster situation
-
5. The hospital director’s ability to choose to directly deal with the most critical problem(s), while others handle the routine problems
-
6. Flexibility in the degree of centralization of handling the event
-
7. Frequent reassessment and decision-making
-
8. Familiarity of the staff with the program structure and its implementation in different scenarios and the options for changing and adapting it to suit the uniqueness of specific scenarios
Our Experience
ZMC staff has not yet been faced with an emergency to test the model. It has performed drills simulating war situations in the Galilee area, as well as drills simulating bioterrorism and chemical weapon attacks. More specifically, we have tested the model under 2 different conditions. First, we tested the model in 3 wide-scale training exercises conducted by first-response forces simulating armed conflict on Israel’s northern border. In each exercise, ZMC was required to respond to a variety of complex crises, such as mass-casualty events, missile strikes on the hospital, and a lack of resources. During all 3 drills, the model proved very effective, ensuring that each unit clearly understands its mission and carries it out effectively. This allowed all units to thoroughly manage all aspects of the tasks simultaneously while keeping the board and hospital administration informed of critical issues that required their intervention. A possible challenge discovered over the course of the exercises was the lack of computer communication between the different components and the administration – such as a command and control system. As a result, the staff developed a reliance on standard communication methods, such as cell phones, that may not be available in an emergency.
Second, the model was partially tested when extreme weather struck the area around the hospital. All units were gathered to discuss the predicted weather and the challenges that it was expected to bring. Once the first round of discussions was concluded, the units were sent to assess their capacities. This information was then sent back to the Board Table for review. Following this, the command structure was scaled down to a situation room dealing mostly with the transportation of employees to and from the hospital. In this operation, the greatest challenge, once again, was the exchange of information between the different units. We recommend that an emergency computer and communications system be developed to allow for the exchange of information between units, precluding the need to rely on landline or cellular technology.
CONCLUSION
ZMC staff continues to implement the HMCEC method during training and reports that this system enables them to effectively manage a range of scenarios.





