Introduction
First-episode psychosis (FEP) is characterized by functional impairments in social, occupational, and independent living activities and is a crucial period for early intervention to improve long-term prognosis [Reference Griffiths, Wood, Fowler, Freemantle, Hodgekins and Jones1, Reference Segura, Mezquida, Martínez-Pinteño, Gassó, Rodriguez and Moreno-Izco2]. Achieving functional remission in FEP is a core clinical objective [Reference Andreasen, Carpenter, Kane, Lasser, Marder and Weinberger3], yet recovery rates vary over the course of the illness [Reference Chang, Kwong, Chan, Jim, Lau and Hui4–Reference Rojnic Kuzman, Makaric, Bosnjak Kuharic, Kekin, Madzarac and Koricancic Makar6], with long-term functioning impairments present even in patients in clinical remission [Reference Robinson, Woerner, McMeniman, Mendelowitz and Bilder7–Reference Austin, Mors, Secher, Hjorthøj, Albert and Bertelsen9]. Several factors are believed to influence functioning in FEP patients, including genetic variability [Reference Segura, Mezquida, Martínez-Pinteño, Gassó, Rodriguez and Moreno-Izco2], negative symptoms [Reference Mezquida, Cabrera, Bioque, Amoretti, Lobo and González-Pinto10–Reference Puig, Baeza, De La Serna, Cabrera, Mezquida and Bioque12], cognitive performance [Reference Sánchez-Torres, Moreno-Izco, Lorente-Omeñaca, Cabrera, Lobo and González-Pinto13, Reference Stouten, Veling, Laan, van der Helm and van der Gaag14], and cognitive reserve (CR) [Reference Amoretti and Ramos-Quiroga15, Reference Sánchez-Torres, Amoretti, Enguita-Germán, Mezquida, Moreno-Izco and Panadero-Gómez16].
Genetic variability is a potential modulator of prognosis in FEP [Reference Segura, Mezquida, Martínez-Pinteño, Gassó, Rodriguez and Moreno-Izco2] and is understood using polygenic risk scores (PRSs) [Reference Dima and Breen17]. PRSs aggregate the effects of many genetic variants across the human genome into a single score and are used to predict the genetic disposition for developing a given disease, including mental disorders [Reference Lambert, Abraham and Inouye18], while also overcoming certain limitations of candidate-gene strategies [Reference Segura, Mezquida, Martínez-Pinteño, Gassó, Rodriguez and Moreno-Izco2]. In fact, PRSs demonstrated good discriminative ability of case–control status in FEP individuals [Reference Segura, Mezquida, Martínez-Pinteño, Gassó, Rodriguez and Moreno-Izco2, Reference Santoro, Ota, de Jong, Noto, Spindola and Talarico19]. Schizophrenia and bipolar disorder PRSs have been linked to symptom severity, comorbid disorders, and cognitive impairments [Reference Mistry, Harrison, Smith, Escott-Price and Zammit20]. A significant positive correlation between PRS and the Positive and Negative Syndrome Scale (PANSS) but not overall functioning was found in a sample of FEP individuals [Reference Sengupta, MacDonald, Fathalli, Yim, Lepage and Iyer21]. Another study [Reference Hettige, Cole, Khalid and De Luca22] failed to find an association between schizophrenia PRSs and functioning. In both studies, the inclusion of patients at different illness stages with varying symptomatology and small sample sizes may have reduced power to identify small effects. The PRS for educational attainment (PRSEA) is based on the completed years of schooling and captures associated social, economic, and health outcomes [Reference Lee, Wedow, Okbay, Kong, Maghzian and Zacher23]. Lower educational attainment is associated with higher schizophrenia PRSs [Reference Escott-Price, Bracher-Smith, Menzies, Walters, Kirov, Owen and O’donovan24] and an overall higher frequency of copy number variants (CNVs) which are considered high risk for psychiatric disorders [Reference Saarentaus, Havulinna, Mars, Ahola-Olli, Kiiskinen and Partanen25]. Importantly, a higher PRSEA was associated with lower symptom severity and better functionality suggesting increased autonomy and better cognitive functioning [Reference Segura, Mezquida, Martínez-Pinteño, Gassó, Rodriguez and Moreno-Izco2], thus highlighting the potential protective properties of PRSEA.
CR has also been considered a protective factor and is understood as the brain’s ability to cope in response to pathology and delay the onset of the associated clinical, cognitive, and functional symptoms [Reference Anaya, Torrent, Caballero, Vieta, Bonnin and del26–Reference Stern30]. In various psychiatric populations, including FEP, higher CR has been associated with later onset age, greater insight, and reduced illness severity in terms of symptoms, particularly negative symptoms, better cognitive performance, and functioning [Reference Amoretti and Ramos-Quiroga15, Reference Amoretti, Bernardo, Bonnin, Bioque, Cabrera and Mezquida31–Reference Camprodon-Boadas, de la Serna, Baeza, Puig, Ilzarbe and Sugranyes34]. Individual differences in CR could explain why people with similar disorders differ in their levels of functioning [Reference Stern30, Reference Amoretti, Verdolini, Mezquida, Rabelo-da-Ponte, Cuesta and Pina-Camacho32, Reference Camprodon-Boadas, de la Serna, Baeza, Puig, Ilzarbe and Sugranyes34–Reference de la Serna, Andrés-Perpiñá, Puig, Baeza, Bombin and Bartrés-Faz36].
Research exploring PRSs and their associations with CR, clinical symptoms, and functioning following a FEP remains limited. Understanding the factors contributing to functional performance in FEP may contribute to early personalized intervention and person-focused therapy. The aim of this study was to investigate the mediating role of CR and clinical symptoms (negative and positive) on the interrelationship between genetic liability for educational attainment and functionality one-year post-FEP. We hypothesize that patients with higher PRSEA will have higher CR and less clinical symptoms, thus better overall functionality at one-year follow-up.
Methods
Sample
A total of 335 FEP patients participated in the “Phenotype–Genotype Interaction: Application of a Predictive Model in First Psychotic Episodes” (PEPs based on Spanish acronym) [Reference Bernardo, Bioque, Parellada, Ruiz, Cuesta and Llerena37, Reference Bernardo, Cabrera, Arango, Bioque, Castro-Fornieles and Cuesta38], a collaborative project between various members of the Spanish Research Network on Mental Health (CIBERSAM) [Reference Salagre, Arango, Artigas, Ayuso-Mateos, Bernardo and Castro-Fornieles39]. This was a multicentre, naturalistic, prospective, longitudinal study. For comprehensive information regarding medication and sample diagnosis see Bioque et al. [Reference Bioque, Llerena, Cabrera, Mezquida, Lobo and González-Pinto40].
The PEPS study inclusion criteria were: (1) between 7 and 35 years at first evaluation; (2) < 12 months history of psychotic symptoms; (3) fluent Spanish, and (4) provide written informed consent. Exclusion criteria were: (1) intellectual disability according to DSM-IV-TR criteria; (2) history of head trauma with loss of consciousness, and (3) organic disease with mental repercussions.
Patients who provided blood samples for genetic analysis, passed the genetic quality control (see section: blood samples and genotyping), completed all assessments at one-year follow-up, were aged ⩾16 years old (chosen cut-off point as this is the age at which most scales report adolescent-adulthood results), had self-reported European ancestry, belonged to the non-affective psychotic disorder diagnostic category and, additionally, had all the information needed to calculate CR, were included. To control for the potential loss of sample, we focused on symptomatology and functional data for a period of 1 year. Supplementary Figure 1 depicts the selection process of the 162 patients with FEP.
The PEPs Project was approved by the Clinical Research Ethics Committee of all participating centers and was conducted in accordance with the ethical principles of the Declaration of Helsinki and Good Clinical Practice.
Written informed consent was obtained from all participants prior to inclusion in the study.
Assessments
Clinical, pharmacological, and sociodemographic assessment
Relevant sociodemographic, clinical, and pharmacological data were collected for all participants. Sociodemographic data included age, sex, and education. Pharmacological treatment was based on international consensus [Reference Gardner, Murphy, O’Donnell, Centorrino and Baldessarini41] and measured using chlorpromazine equivalents (CPZ). To calculate the duration of untreated psychosis (DUP), the number of days between the time taken from the initial onset of psychotic symptoms to beginning treatment for psychosis was calculated. The onset of psychotic symptoms was assessed with the Symptom Onset in Schizophrenia (SOS) scale [Reference Bernardo, Bioque, Parellada, Ruiz, Cuesta and Llerena37, Reference Mezquida, Cabrera, Martínez-Arán, Vieta and Bernardo42], explored via interviews with the patient, medical records, and interviews with relatives.
Diagnoses were established using the Structured Clinical Interview for DSM (SCID-I-II) [Reference First, Gibbon, Spitzer, Williams and Benjamin43, Reference First, Spitzer, Gibbon and Williams44] according to DSM-IV criteria. The PANSS scale [Reference Kay, Fiszbein and Opler45] was administered for the psychopathology assessment. Higher scores indicate greater symptom severity.
Although the PANSS is one of the most widely used measures of negative symptom severity, it has several limitations as it was not designed to evaluate negative symptoms exclusively [Reference Marder and Kirkpatrick46]. Thus, we also used the PANSS-Marder Factor Scores [Reference Marder, Davis and Chouinard47] as it has more restrictive criteria to assess positive and negative symptomatology. For the present study, the PANSS was solely used to understand the role of positive and negative symptoms in the sample as the literature has shown that CR is highly associated with negative symptoms only [Reference Amoretti, Bernardo, Bonnin, Bioque, Cabrera and Mezquida31], whereas functionality has been linked to both positive and negative symptoms [Reference Amoretti, Rosa, Mezquida, Cabrera, Ribeiro and Molina48]. The sum of the following items of the PANSS were used to calculate the Positive Symptom Factor (PS): delusions (P1), hallucinatory behavior (P3), grandiosity (P5), suspiciousness/persecution (P6), stereotyped thinking (N7), somatic concerns (G1), unusual thought content (G9) and lack of judgment and insight (G12); and for the Negative Symptom Factor (NS): blunted affect (N1), emotional withdrawal (N2), poor rapport (N3), passive/apathetic social withdrawal (N4), lack of spontaneity and conversation flow (N6), motor retardation (G7) and active social avoidance (G16).
Functional assessment
The Functioning Assessment Short Test (FAST) [Reference Rosa, Sánchez-Moreno, Martínez-Aran, Salamero, Torrent and Reinares49] evaluated overall functioning across the following six areas: autonomy, occupational functioning, cognitive functioning, management of personal finances, interpersonal relationships, and leisure time. Higher scores indicate poorer functioning.
The Premorbid Adjustment Scale (PAS) [Reference Cannon-Spoor, Potkin and Jed Wyatt50] evaluates the achievement of developmental goals prior to the onset of psychotic symptoms and was administered retrospectively to assess premorbid adjustment. Information was obtained from the patients themselves and parents/close relatives. All participants completed the childhood and adolescence elements of this scale. Higher scores indicate worse premorbid adjustment.
CR assessment
Premorbid intelligence quotient (IQ), educational attainment level, and lifetime participation in leisure, social, and physical activities are the three most commonly proposed proxy indicators of CR in psychiatry, particularly in FEP [Reference Amoretti, Bernardo, Bonnin, Bioque, Cabrera and Mezquida31–Reference Barnett, Salmond, Jones and Sahakian33, Reference Amoretti, Cabrera, Torrent, Mezquida, Lobo and González-Pinto35, Reference de la Serna, Andrés-Perpiñá, Puig, Baeza, Bombin and Bartrés-Faz36] and were used to assess CR in this study. Estimated premorbid IQ was evaluated with the Vocabulary subtest of the Wechsler Adult Intelligence Scale-III [Reference Wechsler51] as a measure of crystallized intelligence. The total number of participants’ completed years in education, as well as parents’ educational level, were used to assess educational attainment level. The scholastic performance domain of the PAS scale was used to evaluate lifetime participation in leisure, social, and physical activities and by enquiring about involvement in social activities, their self-rated capacity to take part in physical activities and satisfaction with hobbies. Higher scores indicate better performance. A “Cognitive Reserve Score” was created via a Principal Components Analysis (PCA) for each subject with completed data for the three core proxy indicators.
Blood samples and genotyping
K2EDTA BD Vacutainer EDTA tubes (Becton Dickinson, Franklin Lakes, NJ) were used to collect blood samples, which were subsequently stored at −20°C prior to shipment to the central laboratory for further analysis. The MagNA Pure LC DNA isolation kit – large volume and MagNA Pure LC 2.0 Instrument (Roche Diagnostics GmbH, Mannheim, Germany) supported DNA extraction and DNA concentration was determined by absorbance (ND1000, NanoDrop, Wilmington, Delaware). Specifically, 2.5 μg of genomic DNA was sent for genotyping at the Spanish National Genotyping Centre (CeGen) using Axiom Spain Biobank Array (developed in the University of Santiago de Compostela, Spain).
PRS calculation
Genotyping data were submitted to the Michigan Imputation Server [Reference Das, Forer, Schönherr, Sidore, Locke and Kwong52], following the standard pipeline for Minimac4 software and setting a European population reference from build GRCh37/hg19, reference panel HRC 1.1 2016 and Eagle v2.4 phasing.
For PRS calculation, genome-wide association study (GWAS) summary results from the Social Science Genetic Association Consortium were obtained. Based on our previous study [Reference Segura, Mezquida, Martínez-Pinteño, Gassó, Rodriguez and Moreno-Izco2] we selected the PRSEA (1,131,881 individuals) [Reference Lee, Wedow, Okbay, Kong, Maghzian and Zacher23], measured as the number of years of schooling that individuals completed. Higher scores reflect the genetic liability for higher educational attainment. Duplicated and unknown strand GWAS summary single-nucleotide polymorphisms (SNPs) were excluded.
Quality control was performed with PLINK v1.07 [Reference Purcell, Neale, Todd-Brown, Thomas, Ferreira and Bender53]. Inclusion criteria for SNPs were minor allele frequency > 0.01, Hardy–Weinberg equilibrium p > 10−6, marker missingness <0.01, and imputation INFO >0.8. Pruning was done using a window/step size of 200/50 kb and r 2 > 0.25. Sample quality control included individuals with heterozygosity values within three standard deviations (SD) from the mean, a missingness rate of <0.01, matching chromosomal and database-labeled sex and relatedness π-hat <0.125.
The PRS were constructed using PRS-CS, a method that implements a high-dimensional Bayesian regression to perform a continuous shrinkage of SNP effect sizes using GWAS summary statistics and an external linkage disequilibrium (LD) reference panel [Reference Ge, Chen, Ni, Feng and Smoller54]. The LD reference panel was constructed using a European subsample of the UK Biobank [Reference Bycroft, Freeman, Petkova, Band, Elliott and Sharp55]. For the remaining parameters, the default options as implemented in PRS-CS were adopted.
A genetic principal component analysis (PCA) was performed to control population stratification [Reference Patterson, Price and Reich56] by means of the SNPRelate package, and the first 10 components were used as covariates in the statistical analyses including PRS.
Statistical analysis
The normality of continuous variables was tested using the Kolmogorov–Smirnov and Shapiro–Wilk tests. The confounding effect on functionality of discrete variables was analyzed using a t-test and Pearson’s correlation coefficient was used for continuous variables. Before testing the mediation hypothesis, we tested the relationship between mediators and the outcome variable using Pearson’s correlation coefficient.
Mediation analysis tested whether the effect of a causal variable (PRSEA) on an outcome variable (functionality, FAST scale score) is affected by one or more mediator variables (CR, NS, PS, and Marder PANSS Factor Scores) at one-year follow-up. The relationship between variables is described by three effects: (1) Total effect (c), the association between causal variable and outcome variable; (2) Direct effect (c’), the effect of the causal variable on the outcome variable, when controlling for the mediator variables; and (3) Indirect effect, the effect of the causal variable on the outcome variable via the mediator variable [Reference Hayes and Rockwood57]. Two mediation models were explored. A parallel mediation model explored the relationship of PRSEA with functionality through CR, NS, and PS. A serial mediation model tested a causal chain of the three mediators: CR, NS, and PS. Based on clinical knowledge, we propose that genetic predisposition for educational attainment may be linked to higher CR, which in turn decreases clinical symptomatology and therefore increases functionality (PRSEA > CR > Clinical symptoms > Functionality) [Reference Segura, Mezquida, Martínez-Pinteño, Gassó, Rodriguez and Moreno-Izco2, Reference Mezquida, Cabrera, Bioque, Amoretti, Lobo and González-Pinto10, Reference Amoretti, Verdolini, Mezquida, Rabelo-da-Ponte, Cuesta and Pina-Camacho32]. For each model, we obtained the total effect, the direct effect, and the total indirect effect of all mediator variables, as well as the indirect effect of each individual mediator or serial path.
The statistical significance of the indirect effect was tested with a nonparametric bootstrapping approach (5000 iterations) to obtain 95% confidence intervals. In these analyses, mediation is considered significant if the 95% bias-corrected for the indirect effect does not include 0.
Analysis was performed using the PROCESS function V.4.1 in SPSS V.22. The model 4 (model as a parameter in the PROCESS function) was used for the parallel mediation model, and model 6 for the serial mediation models. To control for population stratification, all models were fitted by the first 10 principal components of the PCA analysis. Model fit statistics were also reported using the following: a Comparative Fit Index (CFI) (satisfactory > 0.90), a Root Mean Square Error of Approximation (RMSEA) (satisfactory < 0.05), and a Standardized Root Mean Square Residual (SRMR) (satisfactory < 0.08) [Reference Kline58]. The fit indices were derived using the R package lavaan [Reference Rosseel59].
Results
Table 1 shows the characteristics of the sample with 70% male and a mean age of 24.7 (SD = 5.4). The mean dose of antipsychotic medication was equivalent to 577.8 (SD = 489.5) mg/day of CPZ, and the mean DUP was 98.7 (SD = 128.2) days (14 weeks approximately).
Table 1. Main sociodemographic, functional, and clinical features of the FEP sample at study entry (N = 162)
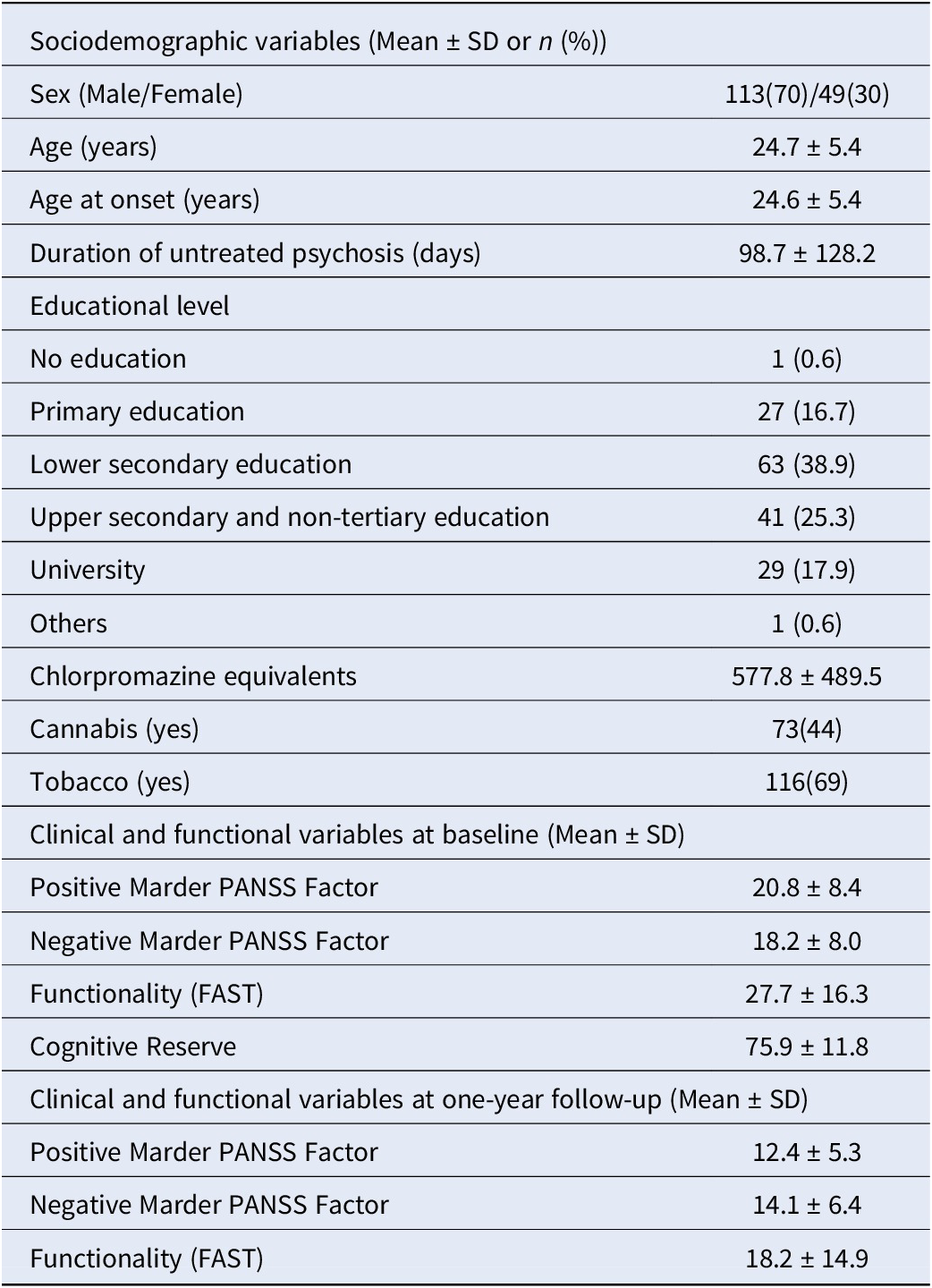
Abbreviations: FAST, Functioning Assessment Short Test; PANSS, Positive and Negative Syndrome Scale.
Functionality, measured using the FAST total score, was negatively correlated with PRSEA (r = −0.21, p = 0.004) and CR (r = −0.23, p = 0.003), and positively correlated with NS (r = 0.69, p < 0.001) and PS (r = 0.56, p < 0.001), indicating that higher PRSEA and CR are associated with better functional outcome. In contrast, higher levels of NS and PS are correlated with worse functional outcome. As these correlations were significant, the conditions required to perform mediation analysis were fulfilled.
The total effect of PRSEA on functionality was significant (β = −3.27, 95%CI [−5.62, −0.93], p = 0.006). In the parallel mediation model (Figure 1), the direct effect was not significant (p = 0.077), and a total indirect effect was present (β = −1.74, 95%CI [−3.27, −0.18], p < 0.05) (Table 2). None of the three mediators significantly mediated the relationship between PRSEA and functionality. Fitting indices also demonstrated that the model poorly fit the data (CFI = 0.30; RMSEA = 0.25; SRMR = 0.11).

Figure 1. Parallel mediation model. The mediating effect of three mediators (CR, PS, and NS) in the relationship between PRSEA and functionality. All presented effects are unstandardized. C′ is the direct effect of PRSEA on functionality. *p < 0.05, **p < 0.01, ***p < 0.001. Continuous lines denoted significant regression. CR, cognitive reserve; NS, negative symptoms; PRSEA, polygenic risk score for educational attainment; PS, positive symptoms.
Table 2. Non-standardized total, direct, and indirect effects (total and of each individual mediator or path) of the two mediation models

Abbreviations: CI, confidence interval; CR, cognitive reserve; NS, negative symptoms; PRSEA, polygenic risk score for educational attainment; PS, positive symptoms. Significant differences (p<0.05) marked in bold.
The serial mediation model hypothesizes a causal chain linking the three mediators in a specified order and direction flow. We propose that PRSEA may be linked to higher CR, which in turn decreases clinical symptomatology and therefore increases functionality (Figure 2). Results show that the three mediators in the abovementioned causal order fully mediate the relationship between PRSEA and functionality, as no direct effect was observed whereas the total indirect effect was significant (Table 2). Among the seven paths that could be inferred from the model, only the path including CR and NS as mediators was significant according to 5000 bootstrapped samples. Fitting indices indicated that the model fits the data satisfactorily (CFI = 1.00; RMSEA = 0.00; SRMR = 7.2 × 10−7).
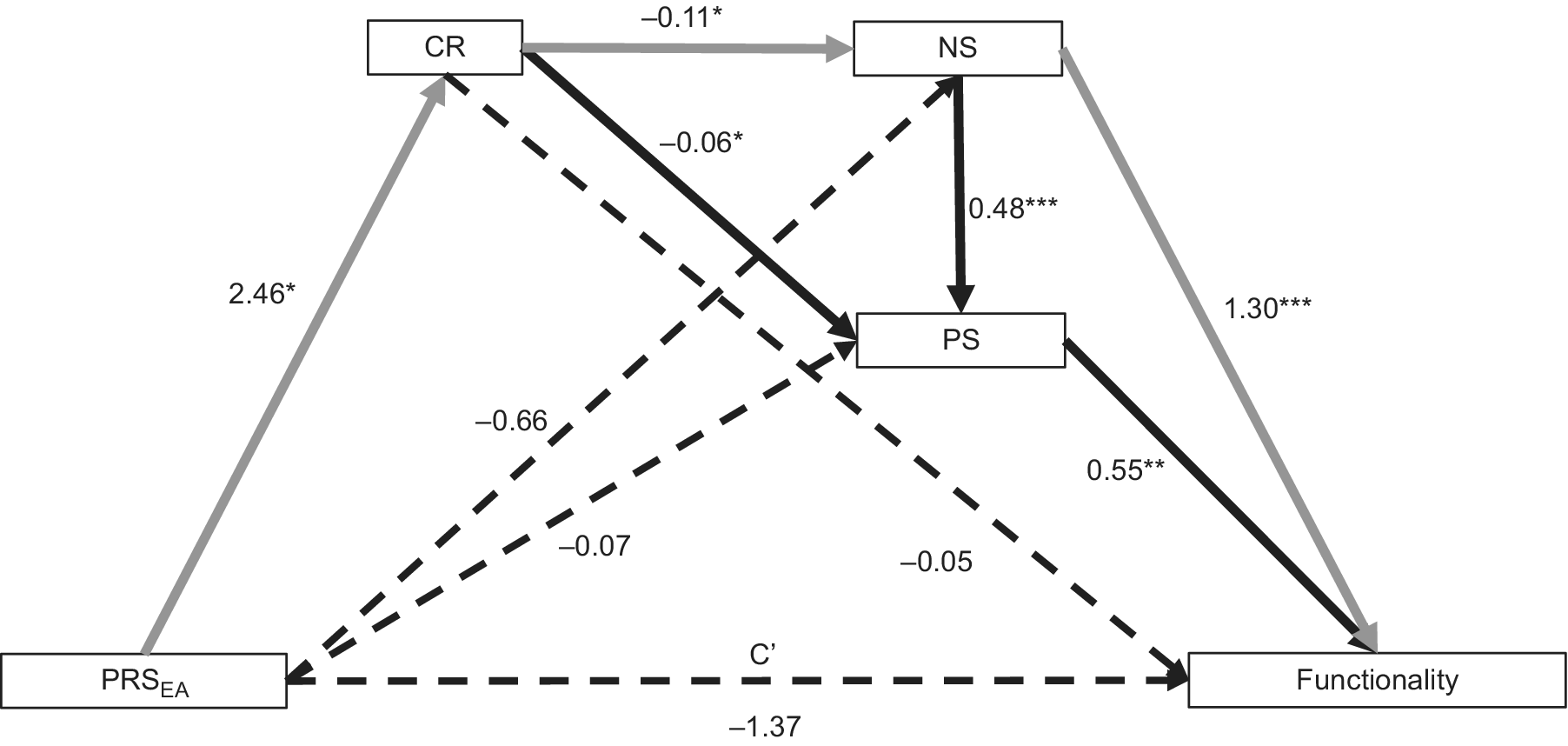
Figure 2. The serial mediating effect of CR, PS, and NS in the relationship between PRSEA and functionality. All presented effects are unstandardized. C′ is the direct effect of PRSEA on functionality. *p < 0.05, **p < 0.01, ***p < 0.001. Continuous lines denoted significant regression. Gray lines represent path with significant indirect effect. CR, cognitive reserve; NS, negative symptoms; PRSEA, polygenic risk score for educational attainment; PS, positive symptoms.
Discussion
The main finding of this study is that the serial mediation model demonstrated that CR and clinical symptoms, more specifically NS, mediate the relationship between PRSEA and functionality at one-year follow-up. To the best of our knowledge, this is the first statistical model describing this causal chain of events, improving our understanding of previously observed clinical findings. Based on this causal relationship between variables, a parallel mediation model poorly fit the data. Our results provide evidence for the role of genetic liability in the cognitive and clinical aspects of FEP, further supporting findings for the association between PRSEA (and not psychological PRSs) and cognition, illness course, and functioning [Reference Segura, Mezquida, Martínez-Pinteño, Gassó, Rodriguez and Moreno-Izco2]. In our serial model, a causal chain (PRSEA > CR > Clinical symptoms > Functionality) was found.
In terms of CR, results indicate its potential genetic component. Genetic and environmental factors are both important in CR. Genetics determine individual aspects of functional brain processes, which can be influenced by the interaction of innate individual factors (e.g., in utero or genetically determined) as well as lifetime exposures. Conversely, environmental elements such as education, occupation, physical exercise, leisure activities, and social interaction are also influential [Reference Stern30, Reference Bora60, Reference Walhovd, Howell, Ritchie, Staff and Cotman61]. In this context, the protective effect of the genetics underlying cognitive features in the early progression of clinical manifestation after a FEP has been recently reported [Reference Segura, Mezquida, Martínez-Pinteño, Gassó, Rodriguez and Moreno-Izco2]. As such, FEP individuals with an increased genetic predisposition for better cognitive functioning could be more resilient to the stressful effects of the psychotic episode and have a better prognosis [Reference Segura, Mezquida, Martínez-Pinteño, Gassó, Rodriguez and Moreno-Izco2]. Equally, environmental factors are currently addressed in specific interventions enhancing CR in FEP and high-risk populations [Reference de la Serna, Montejo, Solé, Castro-Fornieles, Camprodon-Boadas and Sugranyes62]. Therefore, our results add to the previous research demonstrating the mediating effects of CR, while also including the genetic component and its influence in the relationship with clinical symptoms and functioning.
Regarding clinical aspects, different studies have shown that CR is closely linked with negative symptoms [Reference Amoretti, Bernardo, Bonnin, Bioque, Cabrera and Mezquida31, Reference Barnett, Salmond, Jones and Sahakian33] and only one study [Reference Amoretti, Rosa, Mezquida, Cabrera, Ribeiro and Molina48] has found a relationship between CR and positive symptomatology; the authors described that CR partially mediates the relationship between positive symptoms and functioning. Notably, negative and cognitive symptoms are indeed the primary predictors of functioning at different stages of psychotic disorders [Reference Green, Kern, Braff and Mint63, Reference Okada, Hirano and Taniguchi64], and appear to have a greater impact on functioning than positive symptoms [Reference Ventura, Hellemann, Thames, Koellner and Nuechterlein65, Reference Rabinowitz, Levine, Garibaldi, Bugarski-Kirola, Berardo and Kapur66]. Several studies of the PEPs project have established the role of CR as a mediator of clinical and cognitive symptoms, as well as functionality [Reference Amoretti, Bernardo, Bonnin, Bioque, Cabrera and Mezquida31, Reference Amoretti, Verdolini, Mezquida, Rabelo-da-Ponte, Cuesta and Pina-Camacho32, Reference Amoretti, Cabrera, Torrent, Mezquida, Lobo and González-Pinto35, Reference González-Ortega, González-Pinto, Alberich, Echeburúa, Bernardo and Cabrera67]. Amoretti and Ramos-Quiroga [Reference Amoretti and Ramos-Quiroga15] found that higher levels of CR predict a better prognosis following a FEP, reiterating the need to consider the genetic component of this disorder. Nevertheless, in this study, CR alone did not predict functionality. This may be due to its complex interplay with NS and PS which are believed to have a more direct impact upon functionality [Reference Mezquida, Cabrera, Bioque, Amoretti, Lobo and González-Pinto10]. Hence, CR may have a strong genetic basis which influences NS, PS, and functionality. Specifically, findings suggest that PRSEA may lead to higher CR which in turn is linked to lower NS and therefore better functionality following a FEP (e.g., PRSEA > CR > NS > Functionality). This finding is relevant for the application of PRS in personalized medicine which aims to improve early disease detection, as well as early prevention [Reference Vieta and Berk68] and personalized intervention methods [Reference Konuma and Okada69].
Certain limitations in the present study must be considered. Firstly, several constraints are associated with the use of the PANSS as it was not designed with the purpose of solely measuring negative symptoms [Reference Blanchard, Kring, Horan and Gur70]. To account for this, we used the PANSS-Marder Factor Scores [Reference Marder and Kirkpatrick46] which applies stricter criteria for assessing positive and negative symptomatology. Future studies may include specific scales to assess negative symptoms such as the Brief Negative Symptom Scale (BNSS) [Reference Kirkpatrick, Strauss, Nguyen, Fischer, Daniel and Cienfuegos71, Reference Mané, García-Rizo, Garcia-Portilla, Bergé, Sugranyes and Garcia-Alvarez72] to address this drawback. A similar limitation is seen in all studies measuring CR in psychiatric populations as at the time of conducting this study there were no validated tools to evaluate CR. The Cognitive Reserve Assessment Scale in Health (CRASH) [Reference Amoretti, Cabrera, Torrent, Bonnín, Del and Mezquida73] for adult population, and Cognitive Reserve Questionnaire for Adolescents (CoRe-A) [Reference Camprodon-Boadas, de la Serna, Baeza, Ilzarbe, Puig and Andrés-Perpiñá74] have since been designed and should be administered accordingly. Secondly, the limited sample size may increase the risk of reducing statistical power and the ability to detect small effects. As such, further research with larger sample sizes is required. Finally, the short follow-up period is a potential limitation in this study. Nonetheless, the present study is a naturalistic and multicentric study from the entire Spanish population and comprises the largest and best-characterized first-episode sample of the country. Additionally, the PRSs were calculated with the largest GWAS from international consortiums ergo the genetic variants have a greater capacity to capture the genetic susceptibility of the phenotypes explored. Furthermore, the specific PRS-CS method implemented ensures that the shrinkage of variant effect sizes allows the inclusion of all available SNPs in the PRSs and therefore avoids p-value thresholding.
Conclusions
This study provides a potential clinical explanation for the association between genetic predisposition for educational attainment and functional outcomes. We identified an influence of CR on NS in mediating the relationship between PRSEA and functioning in individuals with FEP. These results highlight the suitability and applicability of mediation models to explore the relationship between genetic and clinical data. Additionally, these results may be of significant clinical importance for two primary reasons. Firstly, we provide a clinical framework for clinicians by identifying a potential causal chain of events which can be part of the ongoing development of PRSs in precision psychiatry to further advance toward personalized interventions. Secondly, and based on these insights, the use of cognitive interventions could be recommended to enhance CR by focusing on mental stimulation (e.g., cognitive tasks), physical exercise, leisure activities, and social skills training [Reference de la Serna, Montejo, Solé, Castro-Fornieles, Camprodon-Boadas and Sugranyes62, Reference Willis and Hakim75]. This is clinically relevant given the importance of functional outcomes during the first years after a first-episode. To prevent severe forms of the disorder and a poorer prognosis, rapid identification, timing of treatment, and early interventions in first episode patients are key factors in determining their prognoses and functional outcomes.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1192/j.eurpsy.2023.2480.
Data availability statement
The data that support the findings of this study are available on request from the corresponding authors.
Acknowledgments
We are extremely grateful to all participants. This study is part of a coordinated-multicentre project, funded by the Ministerio de Economía y Competitividad (PI08/0208; PI11/00325; PI14/00612; PI18/00789), Instituto de Salud Carlos III – Fondo Europeo de Desarrollo Regional, Unión Europea, Una manera de hacer Europa, Centro de Investigación Biomédica en Red de salud Mental, CIBERSAM, by the CERCA Programme/Generalitat de Catalunya AND Secretaria d’Universitats i Recerca del Departament d’Economia I Coneixement (2021 SGR 01120), Departament de Salut de la Generalitat de Catalunya, en la convocatòria corresponent a l’any 2017 de concessió de subvencions del Pla Estratègic de Recerca i Innovació en Salut (PERIS) 2016–2020, modalitat Projectes de recerca orientats a l’atenció primària, amb el codi d’expedient SLT006/17/00345. M.B. is also grateful for the support of the Institut de Neurociències, Universitat de Barcelona. M.B. thanks the support of the Fundació La Marató de TV3 (202205-10). E.V. thanks the support of the Spanish Ministry of Science, Innovation and Universities (PI15/00283; PI18/00805; PI21/00787) integrated into the Plan Nacional de I + D + I y cofinanciado por el ISCIII-Subdirección General de Evaluación y el Fondo Europeo de Desarrollo Regional (FEDER); CIBERSAM; and the Comissionat per a Universitats i Recerca del DIUE de la Generalitat de Catalunya to the Bipolar Disorders Group (2021 SGR 1358) and the project SLT006/17/00357, from PERIS 2016–2020 (Departament de Salut), CERCA Programme/Generalitat de Catalunya. This work was supported by La Marató-TV3 Foundation Grant (202234-30). S.A. has been supported by Sara Borrell doctoral programme (CD20/00177) and M-AES mobility fellowship (MV22/00002), from the Instituto de Salud Carlos III (ISCIII), and co-funded by European Social Fund “Investing in your future.” This work was supported by La Marató-TV3 Foundation Grant (202234-32). G.F. received the support of a fellowship from “La Caixa” Foundation (ID 100010434). The fellowship code is LCF/BQ/DR21/11880019. M.F.F. received the support of a “Contratos predoctorales de formación en investigación en salud” (PFIS22) (FI22/00185) from the Instituto de Salud Carlos III (ISCIII). A.G.-P. thanks the support of the Spanish Ministry of Science, Innovation and Universities PI21/00713, PI18/01055 integrated into the Plan Nacional de I + D + I y cofinanciado por el ISCIII-Subdirección General de Evaluación y el Fondo Europeo de Desarrollo Regional (FEDER); CIBERSAM; and the Basque Government 2022111054. The study has been supported by a BITRECS project conceded to N.V. BITRECS project has received funding from the European Union’s Horizon 2020 research and innovation programme under the Marie Skłodowska-Curie grant agreement No. 754550 and from “La Caixa” Foundation. We also would like to thank the authors of the PEPs group who participated in the development of this manuscript, namely, Jairo González-Díaz (Barcelona Clinic Schizophrenia Unit, Hospital Clinic of Barcelona, Neuroscience Institute, University of Barcelona, August Pi i Sunyer Biomedical Research Institute [IDIBAPS], Barcelona, Spain; UR Center for Mental Health – CERSAME, School of Medicine and Health Sciences, Universidad del Rosario, Bogota DC, Colombia; Clínica Nuestra Señora de la Paz, Bogota DC, Colombia), Lydia Fortea (Barcelona Clinic Schizophrenia Unit, Hospital Clinic of Barcelona, Neuroscience Institute, University of Barcelona, August Pi i Sunyer Biomedical Research Institute [IDIBAPS], Barcelona, Spain), Alvaro Andreu-Bernabeu (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Department of Child and Adolescent Psychiatry, Institute of Psychiatry and Mental Health, Hospital General Universitario Gregorio Marañón, School of Medicine, Universidad Complutense, IiSGM, Madrid, Spain), Marta Ferrer-Quintana (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Department of Child and Adolescent Psychiatry, Institute of Psychiatry and Mental Health, Hospital General Universitario Gregorio Marañón, School of Medicine, Universidad Complutense, IiSGM, Madrid, Spain), Judit Selma (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Department of Psychiatry, Institut d’Investigació Biomèdica-Sant Pau [IIB-SANT PAU], Hospital de la Santa Creu i Sant Pau, Universitat Autònoma de Barcelona [UAB], Barcelona, Spain), Olga Martínez-Piera (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain), Iñaki Zorrilla (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Araba University Hospital, Bioaraba Research Institute, Vitoria-Gasteiz, Spain; University of the Basque Country [UPV-EHU], Bilbao, Spain), Itxaso Gonzalez-Ortega (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Araba University Hospital, Bioaraba Research Institute, Vitoria-Gasteiz, Spain; University of the Basque Country [UPV-EHU], Bilbao, Spain), Concepción De-la-Cámara (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Department of Medicine and Psychiatry, Zaragoza University, Instituto de Investigación Sanitaria Aragón [IIS Aragón], Zaragoza, Spain), Pedro M Ruíz-Lázaro (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Department of Medicine and Psychiatry, Zaragoza University, Instituto de Investigación Sanitaria Aragón [IIS Aragón], Zaragoza, Spain), Juan Nacher (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Neurobiology Unit, Program in Neurosciences and Interdisciplinary Research Structure for Biotechnology and Biomedicine [BIOTECMED], Universitat de València, Biomedical Research Institute INCLIVA, Valencia, Spain), Carlos Cañete (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Department of Psychiatry, Hospital Clínico Universitario de Valencia; Facultad de Medicina, Universidad de Valencia, Valencia, Spain; Biomedical Research Institute INCLIVA, Valencia, Spain), Laura Martínez-Sadurní (Hospital del Mar Medical Research Institute, MELIS Department, Universitat Pompeu Fabra, Barcelona, Spain), Georgina Benet (Hospital del Mar Medical Research Institute, MELIS Department, Universitat Pompeu Fabra, Barcelona, Spain), Maria Serra-Navarro (Bipolar and Depressive Disorders Unit, Hospital Clinic of Barcelona, Institute of Neurosciences, IDIBAPS, University of Barcelona, Barcelona, Spain; Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain), Clàudia Valenzuela (Bipolar and Depressive Disorders Unit, Hospital Clinic of Barcelona, Institute of Neurosciences, IDIBAPS, University of Barcelona, Barcelona, Spain), Josefina Castro-Fornieles (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Department of Child and Adolescent Psychiatry and Psychology, 2017SGR881, Institut Clinic de Neurociències, Hospital Clínic Universitari, IDIBAPS, Department of Medicine, University of Barcelona, Barcelona, Spain), Immaculada Baeza (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Department of Child and Adolescent Psychiatry and Psychology, 2017SGR881, Institut Clinic de Neurociències, Hospital Clínic Universitari, IDIBAPS, Department of Medicine, University of Barcelona, Barcelona, Spain), Fernando Contreras (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Bellvitge University Hospital, IDIBELL, Barcelona, Spain), Teresa Bobes-Bascarán (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Servicio de Salud del Principado de Asturias [SESPA] Oviedo, Instituto de Investigación Sanitaria del Principado de Asturias [ISPA], Instituto Universitario de Neurociencias del Principado de Asturias [INEUROPA], Oviedo, Spain; Department of Psychology, Universidad de Oviedo, Oviedo, Spain), Leticia González-Blanco (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Servicio de Salud del Principado de Asturias [SESPA] Oviedo, Instituto de Investigación Sanitaria del Principado de Asturias [ISPA], Instituto Universitario de Neurociencias del Principado de Asturias [INEUROPA], Oviedo, Spain; Department of Psychiatry, Universidad de Oviedo, Oviedo, Spain), Rafael Segarra (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Cruces University Hospital, BioCruces Health Research Institute, University of the Basque Country [UPV/EHU], Vizcaya, Spain), Arantzazu Zabala (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Cruces University Hospital, BioCruces Health Research Institute, University of the Basque Country [UPV/EHU], Vizcaya, Spain), Ángeles Sánchez-Cabezudo (Instituto de Investigación Sanitaria Hospital 12 de Octubre [imas12], Madrid, Spain), Roberto Rodriquez-Jimenez (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Instituto de Investigación Sanitaria Hospital 12 de Octubre [imas12], Madrid, Spain; Universidad Complutense de Madrid [UCM], Madrid, Spain), Judith Usall (Parc Sanitari Sant Joan de Déu, Teaching, Research & Innovation Unit, Institut de Recerca Sant Joan de Déu, Sant Boi de Llobregat), Anna Butjosa (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Hospital Infanto-juvenil Sant Joan de Déu, Institut de Recerca Sant Joan de Déu, Esplugues de Llobregat, Barcelona), Edith Pomarol-Clotet (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; FIDMAG Germanes Hospitalàries Research Foundation, Barcelona, Spain), Maria Ángeles García-León (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; FIDMAG Germanes Hospitalàries Research Foundation, Barcelona, Spain), Ibáñez A (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Department of Psychiatry, Hospital Universitario Ramón y Cajal, IRYCIS, Universidad de Alcalá, Madrid, Spain), Ana M. Sánchez-Torres (Department of Psychiatry, Complejo Hospitalario de Navarra, Pamplona, Spain; IdiSNA, Navarra Institute for Health Research, Pamplona, Spain), and Vicent Balanzá (Biomedical Research Networking Center for Mental Health Network [CIBERSAM], Barcelona, Spain; Department of Medicine, University of Valencia, Valencia, Spain).
Financial support
The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Competing interest
E.V. has received grants and served as a consultant, advisor, or CME speaker for the following entities (unrelated to the present work): AB-Biotics, Abbott, Allergan, Angelini, Dainippon Sumitomo Pharma, Ferrer, Gedeon Richter, Janssen, Lundbeck, Otsuka, Sage, Sanofi-Aventis, and Takeda. M.B. has been a consultant for, received grant/ research support and honoraria from, and been on the speakers/advisory board of ABBiotics, Adamed, Angelini, Casen Recordati, Janssen-Cilag, Menarini, Rovi, and Takeda. N.V. has received financial support for CME activities and travel funds from the following entities (unrelated to the present work): Angelini, Janssen-Cilag, Lundbeck, and Otsuka. A.T. has received research support from Lundbeck and served as a speaker for Lundbeck and Angelini unrelated to the present work. G.M. received travel grants from Angelini and Janssen. C. D-l-C. received financial support to attend scientific meetings from Janssen, Almirall, Lilly, Lundbeck, Rovi, Esteve, Novartis, Astrazeneca, Pfizer, and Casen Recordati. I.B. has received honoraria or travel support to attend conferences from Angelini, Janssen, and Otsuka-Lundbeck; and grants from Instituto de Salud Carlos III, Spanish Ministry of Health. R.R.-J. has been a consultant for, spoken in activities of, or received grants from: Instituto de Salud Carlos III, Fondo de Investigación Sanitaria (FIS), Centro de Investigación Biomédica en Red de Salud Mental (CIBERSAM), Madrid Regional Government (S2010/BMD-2422 AGES; S2017/BMD-3740), JanssenCilag, Lundbeck, Otsuka, Pfizer, Ferrer, Juste, Takeda, Exeltis, Casen-Recordati, and Angelini. J.G.-D. is partly funded by a grant from Ministerio de Ciencia y Tecnologia – Republica de Colombia (Convocatoria 885/2020) and has been an advisor/speaker for, or received travel support from Janssen, Eurofarma, Servier, Sanofi, Lilly, and Pfizer. A.I. has received research support from or served as a speaker or advisor for Janssen-Cilag, Lundbeck, and Otsuka. The rest of the authors report no biomedical financial interests or potential conflicts of interest.
Ethical standard
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.







Comments
No Comments have been published for this article.