Introduction
Primary headaches (PHA), including migraine, tension-type headache, and cluster headache are a common reason for emergency department (ED) presentations. Reference Locker, Mason and Rigby1 While there is concern that headaches may indicate underlying pathology (e.g., subarachnoid hemorrhage, tumor, temporal arteritis, and meningitis), the vast majority of these PHA presentations are for conditions considered “benign,” particularly migraine headaches, following failed home-based treatments. Reference Ramirez-Lassepas, Espinosa, Cicero, Johnston, Cipolle and Barber2,Reference Doretti, Shestaritc and Ungaro3 Although guidelines exist for management of secondary headaches such as subarachnoid hemorrhage, Reference Perry, Stiell and Sivilotti4 few management guidelines exist for diverse presentations of PHA. Furthermore, guidelines often do not address acute presentations and adherence to guidelines is low in the ED setting, leaving management largely to emergency physician (EP) and patient preferences. Reference Granato, Morelli, Cominotto, D’Acunto and Manganotti5 Consequently, variation in management (e.g., use of opioids and other agents), imaging ordering, and outcomes are substantial. Reference Vinson, Hurtado, Vandenberg and Banwart6–Reference Prevedello, Raja and Zane8
Increasing availability of computed tomography (CT) within the ED has led to a significant increase in CT ordering, despite the documented low likelihood of identifying clinically important findings among patients with suspected PHA. Reference Larson, Johnson, Schnell, Salisbury and Forman9–Reference Osborn, Alder and Mitchell11 While diagnostic image ordering for headache patients has risen in the ED, the prevalence of intracranial pathologies in CT and magnetic resonance imagining findings for these patients have declined. Reference Gilbert, Johnson, Larkin and Moore12 Increased CT ordering continues to drive concerns related to overuse, while failing to substantially influence treatment and resulting in clinically insignificant incidental findings, needless radiation exposure, ED congestion, and increased healthcare costs. Reference Prevedello, Raja and Zane8,Reference Osborn, Alder and Mitchell11,Reference Korley, Pham and Kirsch13,Reference Sodickson, Baeyens and Andriole14 Literature exploring drivers of CT ordering has highlighted the role of patient expectations or requests in increasing demand for unnecessary care, including imaging. Reference Embrett and Randall15–Reference Augustsson, Ingvarsson and Nilsen17 Additionally, factors associated with EPs’ perceptions regarding the appropriateness of ordering CT for patients with PHA presentations remain poorly understood.
This study assessed EPs diagnostic imaging decisions, particularly CT ordering for patients presenting with PHA, the circumstances in which CT ordering is perceived as appropriate, and barriers limiting its reduction for patients with PHA. Furthermore, the study explored drivers influencing EPs’ perceptions and attitudes towards the appropriateness of CT ordering for this patient population.
Methods
Study Design and Population
A cross-sectional study was conducted among EPs in Edmonton, Alberta, Canada, one of the largest urban centers in Western Canada, with a population of ∼1.5 million. Emergency Department services are provided at seven locations in the city and are publicly funded. Cumulatively, these EDs see nearly 10,000 headache presentations annually. 18
Study Procedures and Data Collection
A study questionnaire was developed by a multi-disciplinary research team composed of clinicians, methodologists, and psychologists, and reviewed by a convenience sample of EPs, including physicians who were practicing in other geographic areas in Canada (Appendix S1). The questionnaire included both 7-point Likert scale and open-ended questions about the medical management and diagnostic imaging practices, specifically CT, provided to patients with a variety of PHA presentations. Managing patients’ expectations towards CT ordering was also explored through questions about physicians’ comfort and practices of discussing risks of CT with their patients. Primary headache was defined as headaches that might be cluster, tension or migraine with no sign of underlying serious pathology (e.g., subarachnoid hemorrhage, meningitis, temporal arteritis).
A centralized list of all EPs practicing in Edmonton in 2017 was created by the study team. Emergency physicians from the centralized registry were contacted via email between March 22 and April 30, 2017. An initial email explaining the study purpose as well as providing ethics information was sent to the EPs by the principal investigator (BHR). Subsequently, the study questionnaire was sent to EPs via REDCap (Vanderbilt University, Nashville, TN, USA), an online secure data capture tool. Reference Harris, Taylor, Thielke, Payne, Gonzalez and Conde19 Two reminders for completion were sent via REDCap.
Data Analysis
Categorical data are reported as proportions and percentages. Open-ended questions were analyzed qualitatively using a general inductive approach. Reference Thomas20 Double reading of responses was undertaken. Responses were subsequently coded and then clustered into themes.
Multivariable logistic regression methods were used to examine the independent association between selected variables from the questionnaire and EPs’ perceptions regarding the appropriateness of CT ordering for patients with PHA after adjusting for other factors. For this analysis, EPs who considered CT scans for patients with PHA as frequently, sometimes, or occasionally appropriate were categorized as potential “intermediate CT users” and compared to those who believed CT scans were rarely or never appropriate for patients with benign headache (potential “low users”: reference group). The variables were chosen from the questionnaire as they characterized EPs’ general practice approach and were not specific to a clinical scenario or unique clinical presentation of PHA: female sex, years of practice, level of Emergency Medicine training, site of practice, and most common perceived barriers to limiting the use of CT scans. These barriers include the possibility of missing a severe condition, the fear or litigation if condition is missed, and patient request or expectation.
Results are reported as adjusted odds ratios (aOR) with corresponding 95% confidence intervals (CIs). Those with p<0.05 were considered statistically significant. Missing data were excluded from the analysis. Statistical analyses were conducted using the Statistical Package for the Social Sciences (SPSS, V.13.0, Chicago, Illinois) and STATA Release 16 (StataCorp LP, College Station, Texas, UAS).
Ethics
Ethics approval was obtained from the Health Research Ethics Board at the University of Alberta (Pro00062871). A study information sheet was provided to the EPs along with access to the REDCap link for completion. Questionnaire completion implied consent.
Results
A total of 198 email invitations were sent to EPs; five failed delivery notices were received. Resultantly, a total of 193 EPs received the study invitation and 73 completed the questionnaire (38%) (Figure 1). Study participants were mostly over 40 years of age (62%) males (70%) and practicing in the ED for less than 10 years (48%) (Table 1).
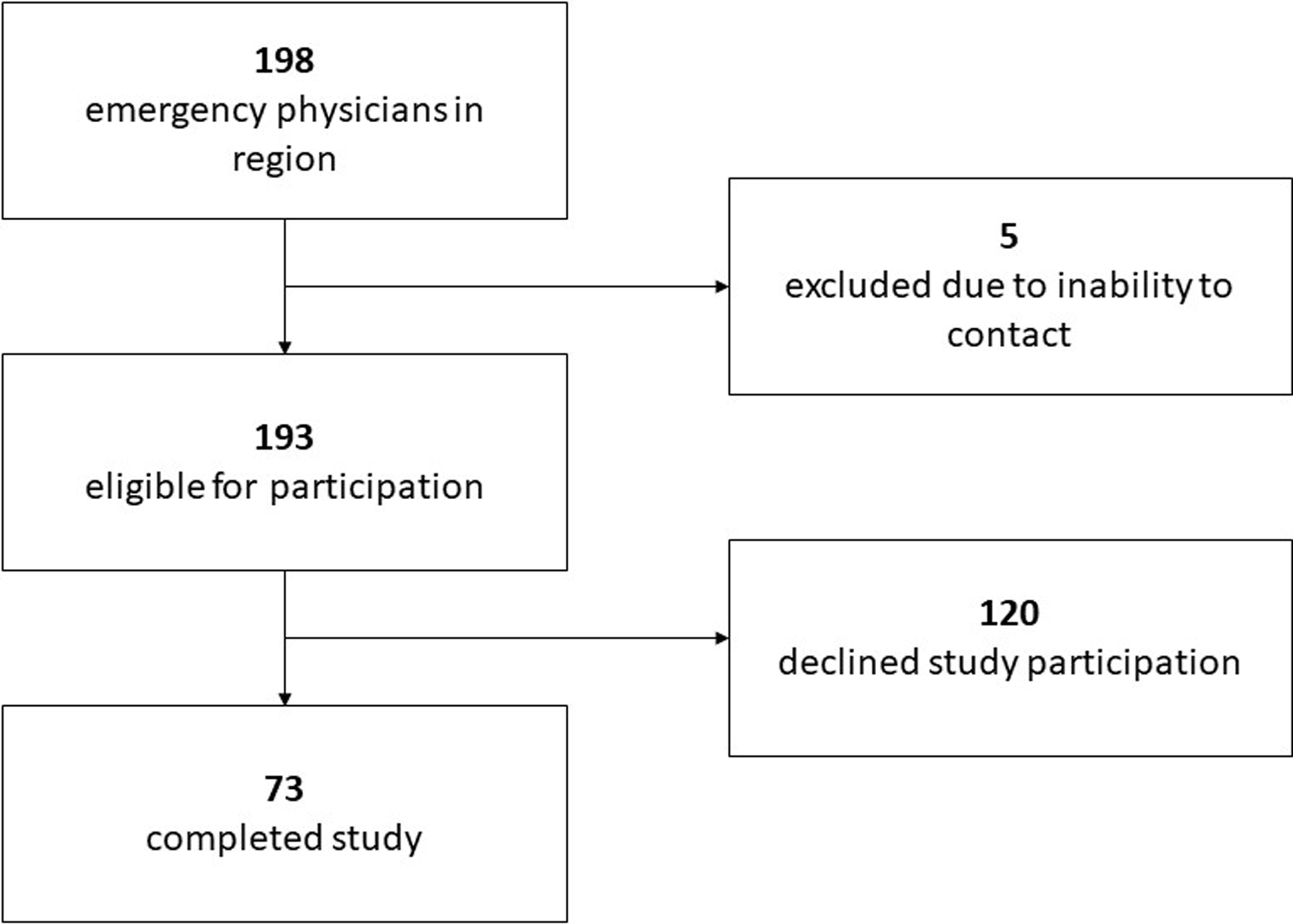
Figure 1: Study flow diagram.
Table 1: Characteristics of study participants (n = 73)
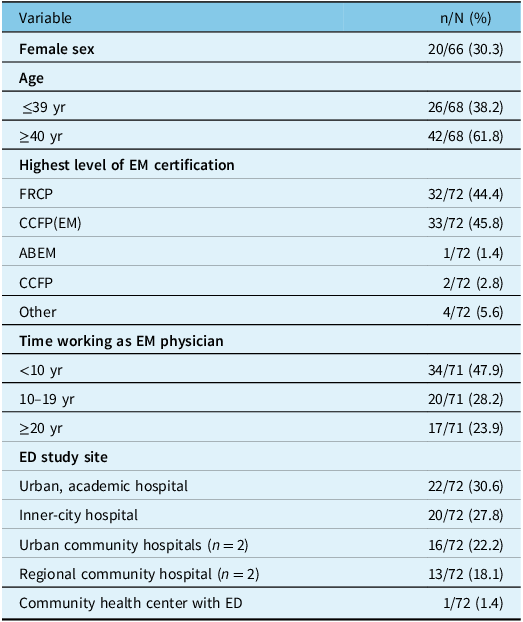
EM = emergency medicine; FRCP = Fellow of the Royal College of Physicians; CCFP(EM) = Certificant of the College of Family Physicians (Emergency Medicine); ABEM = American Board of Emergency Medicine; CCFP = Certificant of the College of Family Physicians (Family Medicine); yr = years.
Self-reported PHA Management
Emergency physicians self-reported management practices of PHA are summarized in Table 2.
Table 2: Emergency physicians self-reported management practices for patients with PHA (n = 73)
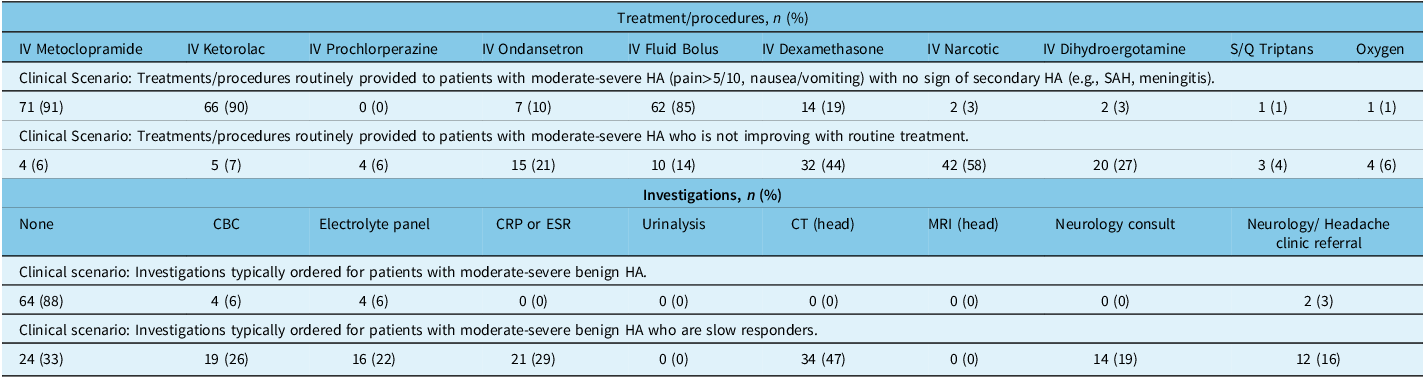
CBC = complete blood count; CRP = C-reactive protein; CT = computer tomography; ESR = erythrocyte sedimentation rate; IV = intravenous; MRI = magnetic resonance imaging; S/Q = subcutaneous.
The predominant treatment approach for patients presenting with moderate-to-severe headaches with no symptoms or signs of a secondary headache was combined therapy (e.g., IV metoclopramide [91%]; IV ketorolac [90%] and IV fluid bolus [85%]). The vast majority of EP respondents indicated that they would not order any investigations for these patients (88%). A small proportion (3%) indicated that they would consider referring these patients to a neurology or headache clinic.
For the scenario in which patients failed management or had a slow response to routine treatment, EPs reported using a variety of additional treatments, including: IV narcotic (58%), IV dexamethasone (44%), IV dihydroergotamine (27%), and IV ondansetron (21%). Some EPs (33%) reported that they would not engage in any investigations, even when patients had a slow response. Other EP respondents reported considering: head CT (47%), c-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) (29%), complete blood count (CBC) (26%), and electrolyte panel (22%). Neurology consults within the ED were identified as part of patients’ treatment plan by 19% of EP respondents and neurology/headache clinic referrals by 16%.
CT Decisions: Clinical Markers, Patient Expectations, and Physician-Patient Communication
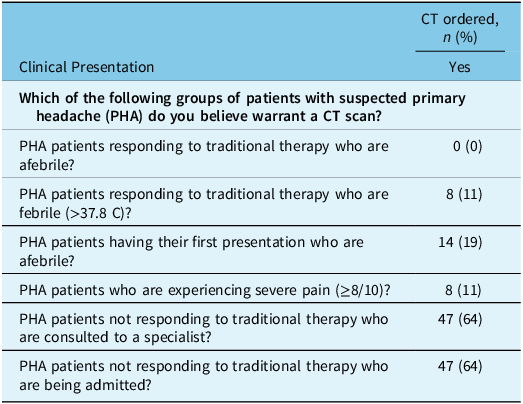
Respondents stated that they limited CT ordering for patients with PHA and ordered occasionally (25%) or rarely (56%) for patients with moderate-severe suspected PHA. The majority of EP respondents felt that CTs were rarely (58%) an appropriate component of PHA management. When analyzed by clinical presentation, a minority of EPs intended to order a CTs for their patients until they were either consulted to a specialty or admitted to hospital (Table 3).
Table 3: CT ordering based on clinical presentation (n = 73)
While EPs relied on specific clinical markers for indicating a CT, they reported they were not alone in making the imaging decision. Twenty-seven percent of the EP respondents perceived that ordering a CT was a frequent or usual expectation of their patients with PHA. Another 42% reported that they perceived this expectation sometimes. The majority (61%) of EPs reported being completely or mostly comfortable discussing the risks of head CT. Although comfortable, less than half (44%) of respondents reported that they always or usually discuss CT risks with their patients prior to image ordering. The risks most likely to be discussed by EPs included: radiation risks associated with CT scan (90%), the lack of diagnostic and treatment utility of the CT scan for PHA (67%), and the lack of necessity of the test in light of previous normal CT (head) results (51%). However, EPs also experienced concerns that kept them from discussing CT risks with their patients when the need for imaging was assessed as immediate (42%). Additionally, they held back from discussing risks when they felt it would not influence patients’ imaging expectations (21%). When physicians discussed head CT risks with their patients, they often used “high, medium, and low” descriptors to characterize the risk (70%), and seldom characterized the imaging risks in terms of other everyday risks that the patient might be familiar with (21%).
Barriers to Limiting CT Ordering
The three major barriers that EPs encountered when limiting CT orders for patients presenting with PHA in the ED were: 1) the fear of missing a severe condition (62%), 2) patient requests or expectations (48%), and 3) fear of litigation in case a condition was missed (37%).
Factors Associated with Appropriateness of CT Ordering
Of the 73 EPs included in the study, 28 (38%) physicians were categorized as potential “intermediate CT users,” while 45 (62%) were categorized as potential “low CT users.” None of the EPs believed that CT scans were always or usually appropriate for patients with PHA, indicating a lack of potential “high CT users” among the study participants.
Table 4 shows that after adjusting for physician sex, years of practice, site of practice and other barriers to limiting CT use, EPs with CCFP (EM) certification were less likely to perceive CT ordering for patients with PHA appropriate (aOR: 0.17; 95% CI: 0.03, 0.95); those who expressed the possibility of missing a condition as the major barrier to limiting their use were more likely to perceive CT ordering for patients with PHA appropriate (aOR: 4.8; 95% CI: 1.10, 21.1).
Table 4: Association between potential intermediate CT user (reference = low CT user) and selected questionnaire variables

CCFP = Certificant of the College of Family Physicians; CI = Confidence interval; CT = Computerized tomography; EM = Emergency Medicine; FRCP = Fellowship of the Royal College of Physicians; PHA = Primary headache disorder. OR = Odds ratio; Ref = reference.
Discussion
Headache is a common presenting problem in EDs in most developed countries; however, practice variation has been widely documented and advanced imaging is a commonly overused modality. This study explored perspectives of EPs on the care they provide to patients with PHA presenting to the ED and examined how diagnostic and therapeutic decisions might be influenced by both physician preferences and patient expectations. Reference Cerbo, Villani, Bruti, Di Stani and Mostardini21 The majority of EPs reported using an evidence-based combination therapy including intravenous metoclopramide, ketorolac and rehydration for their initial management of PHA.
While responding EPs claimed they infrequently investigated patients with PHA using laboratory tests, variation was identified and explored regarding the role of ordering CT scans of the head. Overall, EPs did not report CT ordering as part of their first-line management; however, nearly half of EPs reported ordering a CT for patients who failed or incompletely responded to first-line medical treatments. Despite their infrequency, consulting a specialist and/or hospital admission were reported as strong rationales for CT ordering.
Reducing CT scan ordering in PHA has been a common recommendation of many Choosing Wisely® campaigns internationally. 22 Efforts to reduce CT overuse are often multi-dimensional (e.g., education of clinicians and patients, clinical decision rules, informatic solutions, shared decision-making, etc.) and of mixed effectiveness. When explored in more detail, both level of training and perceived barriers for limiting CT ordering seem to be influencing the perception of EPs regarding the appropriateness (and perhaps their comfort) with CT ordering for patients with PHA. A number of factors may contribute to this hypothesis generating finding: 1) changes in medical education; 2) fear of litigation; 3) improved ED access to advanced imaging; and 4) changes in physicians’ practice over time.
Many factors contribute to an individual clinician’s decision to order a test. The International Classification of Headache Disorders classification of PHA requires a normal physical examination and no alternative explanation for the headache presentation. 23 In the busy emergency environment, where a formal, complete, and thorough neurological examination may be difficult to obtain, some physicians may request advanced imaging, such as CT or MRI, during the diagnostic assessment. In this study, we focused on physician attitudes towards head CT ordering. Future studies could explore the specific roles the setting and neurological skills have on influencing ED MD advanced imaging decisions in PHA presentations.
Importantly, some responding EPs reported that they did not rely on clinical judgement and/or evidence alone when making the imaging decision; patient requests or expectations were important contributors for nearly one-quarter of respondents while patient expectations was perceived as a barrier to limiting CT ordering for nearly half of respondents. These results are mirrored in other studies reporting patient expectations or requests as barriers to reduce unnecessary ordering of tests, treatments and procedures. 22 These studies typically report clinician’s perspectives only and more research is needed to explore patients’ perspectives regarding these perceived expectations or whether these result from known communication challenges in the ED. Reference Roh and Park24,Reference Kuehn25 Regardless of how EPs arrive at this understanding of their patients’ imaging expectations, less than half of EPs reported always or usually discussing the risks of undergoing CT. This low proportion may be partially attributed to the nearly one-quarter of respondents who felt that discussing risks would not have any impact on their patients’ expectations. For these EPs, discussion was perceived as futile. Additional barriers such as insufficient time, and limited access to helpful resources to discuss risk have also been documented in the ED. Reference Robey, Edwards and Murphy26
Overall, introducing shared decision-making tools may help to effectively make these conversations commonplace in care, while providing efficient care. Reference Hess, Grudzen, Thomson, Raja and Carpenter27 Future studies should also explore linking patient and EP characteristics and perceptions of imaging requests in order to identify the following: 1) frequency of patient expectation for imaging and 2) clinical and non-clinical factors associated with imaging expectations that may influence practice.
Limitations
This study was conducted in a single urban ED center as part of a larger study regarding PHA decision-making; reproducing these results elsewhere would be important. Given the nature of the study, selection bias is a relevant concern given the number of EPs who declined to participate in the study (∼60%). The study was based upon self-reported practices. Albeit perception of practice is a vital aspect of readiness to change, self-reporting often differs from practice data collected from a third-party source (e.g., medical records). Reference Roter and Russell28 Additionally, given campaigns such as Choosing Wisely® which recommend limiting advanced imaging ordering, social desirability bias may have influenced physicians’ responses to the imaging questions and further influence self-report. Reference Van de Mortel29 Future studies exploring differences between self-reported practice and the actions documented on medical records may assist in identifying which areas of practice most need to be addressed, and targeted for behavioral change. Finally, we opted for a conservative analytic approach to explore drivers of physicians’ perceptions regarding the appropriateness of CT ordering for patients with primary headache. While this was a post-hoc and exploratory analysis including variables derived from the study questionnaire, they were chosen as representatives for individual physician practice patterns (potential “intermediate vs. low CT users”).
Conclusion
While physicians reported consistency and evidence-based medical management of patients with PHA in this study, they also highlighted the complexities of limiting CT ordering. Specifically, this study revealed the high frequency with which physicians’ level of training and perceived barriers to reduce CT ordering for patients with PHA impact advanced imaging decisions. These factors can be used as a foundation for further study and interventions aimed at engaging them in shared decision-making.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/cjn.2024.6.
Acknowledgements
The authors wish to thank the Emergency Medicine Research Group (EMeRG) at the University of Alberta for their assistance with this study. Additionally, we thank the members of the PRIHS-2 Choosing Wisely Team for their input in the development and review of this study.
Statement of authorship
LDK: Acquisition and interpretation of data. Drafting of the manuscript.
CVR: Study concept and design, obtained funding and critical revision of the manuscript.
EHY: Analysis/interpretation of data and critical revision of the manuscript.
SC: Literature search, data collection and critical revision of the manuscript.
MBO: Study concept and design, obtained funding and critical revision of the manuscript.
BRH: Study concept, obtained funding and critical revision of the manuscript.
BHR: Study concept and design, obtained funding and critical revision of the manuscript.
Funding
Funding support for this study was provided by the Partnership for Research and Innovation in the Health System (PRIHS) grant from Alberta Innovates. At the time of this study, Dr Rowe was supported as a Tier I Canada Research Chair in Evidence-based Emergency Medicine from the Canadian Institutes for Health Research (CIHR) through the Government of Canada (Ottawa, ON). Dr Rowe’s research is now supported by the CIHR through the Scientific Director’s Operating Grant (CIHR SOP#: 154602 and 168483). At the time of this study, Dr Villa-Roel was also funded by CIHR. The funding partners take no responsibility for the conclusions reported.
Competing interests
None of the authors have any known conflicts of interest to declare.







