Cognitive–behavioural therapy (CBT) delivered in group format has attracted less research than CBT delivered on a one-to-one basis. Nevertheless, no doubt influenced by the challenge of limited resources, many centres do offer group therapy based on CBT principles as an alternative or in addition to more traditional CBT delivered to individuals. In England, the Improving Access to Psychological Therapies (IAPT) programme (Department of Health 2008) aims to greatly increase the number of people treated using evidence-based approaches (as defined by the National Institute for Health and Clinical Excellence, NICE) for depression and anxiety disorders in primary care. The potential economies of scale afforded by the use of group work will be an attractive proposition for National Health Service providers working to implement IAPT.
What is group CBT?
Group psychotherapy has its origins in psycho-dynamic models of pathology and it developed before the practice of CBT was first outlined by Aaron Beck and colleagues (Reference Beck, Rush and ShawBeck 1979). Importantly, group psychotherapy views the interactions between the group members as the vehicle of change. In CBT groups, it has traditionally been assumed that the cognitive–behavioural model taught to the group is more of an ‘active ingredient’ than the relationships between the group members (Reference Bieling, McCabe and AntonyBieling 2006). Indeed, the educational ethos is inherent in the CBT model, and this lends itself very easily to the provision of groups or classes, as does the fact that CBT is structured and directive, collaborative and time-limited (Reference Fennell, Hawton, Salkovskis and KirkFennell 1989).
However, group CBT cannot solely be about taught skills, and in common with individual (one-to-one) CBT, non-specific interpersonal factors play a part. As with individual CBT, these non-specific factors have not attracted the same research attention as the underlying cognitive–behavioural theoretical models (such as which underlying thoughts and behaviours are paramount in different disorders) (Reference Bieling, McCabe and AntonyBieling 2006; Reference Tucker and OeiTucker 2007). This is in sharp contrast to group psychotherapy, which has focused on interpersonal relationships and related mechanisms of change. The most influential of these suggested mechanisms have been Yalom's ‘curative factors’, listed in Box 1 (Reference YalomYalom 1995).
BOX 1 Therapeutic factors in group psychotherapy
-
• Installation of hope
-
• Universality
-
• Imparting information
-
• Altruism
-
• Corrective recapitulation of the primary family group
-
• Development of socialising techniques
-
• Imitative behaviours
-
• Interpersonal learning
-
• Group cohesiveness
-
• Catharsis
-
• Existential factors
How does group CBT work?
To varying degrees, Yalom's therapeutic factors are likely to be relevant to all models of group psychotherapy. Wherever you have the formation of a group you will have patterns of relating – ‘group processes’ – that will affect both the group as a whole and the extent to which group members benefit from attendance (Reference Burlingame, Fuhriman, Johnson, Lambert, Bergin and GarfieldBurlingame 2004). Some of Yalom's factors – such as the corrective recapitulation of the primary family group – might be seen as less relevant to CBT groups. However, researchers have translated aspects of the concept into CBT principles – so that the group might be seen to modify maladaptive relational patterns through observing others and trying out new styles of interacting (Reference Bieling, McCabe and AntonyBieling 2006).
White & Freeman describe the two important elements that need to be present for an effective CBT group as the group's cohesiveness and task focus. They define cohesiveness as ‘the degree of personal interest of the members for each other’ (Reference White and FreemanWhite 2000: p. xiii). All CBT groups should be task-focused, in that there should be defined goals to be achieved. Other mechanisms that probably play a part in effecting change in group CBT are listed below: as can be seen, many incorporate concepts inherent in Yalom's therapeutic factors. For a more detailed consideration of the potential mechanisms of change in CBT groups, I recommend Reference Bieling, McCabe and AntonyBieling et al (2006).
Cognitive restructuring through behavioural experiments
The group provides ready circumstances for behavioural experiments challenging automatic thoughts and their underlying core beliefs and assumptions. For example, the prediction ‘If I say something with a strong accent or use a wrong word then people will look down on me and laugh’ can be tested in the group. Beliefs can be gently challenged not only by the therapist but also by the other group members, who are to a degree acting as co-therapists (Reference Heimberg, Salzman and HoltHeimberg 1993).
Normalising through identification with others
When group members observe that other members have similar experiences, worries and emotional responses it illustrates for them that they are not unique in thinking and behaving as they do. This can be a powerful normalising experience which helps to reduce associated stigma and shame (akin to Yalom's universality: Box 1). The mechanism by which this occurs is the disproving of beliefs such as ‘I'm alone’ and ‘I'm defective and different from others’. The normalisation process can therefore be seen as another method of cognitive restructuring.
Collaborative therapeutic relationships
Individuals sometimes take comments made by one group member to another more seriously than those made by the therapist. This is probably because the other group members are viewed as more impartial than the therapist. The relationships within the group (therapist to group member and between the group members) must be as collaborative and as non-threatening as possible, so that questioning and suggestions are not perceived as attacking and undermining (Reference White and FreemanWhite 2000).
‘In-vivo’ exposure
Exposure to a feared stimulus is often helped by having a group of people to hand. Social phobia, for example, is a natural candidate for group CBT. Feared situations such as public speaking can be recreated within the group setting to allow individuals to habituate to their fears. Note how this links in with cognitive restructuring through the testing out of beliefs mentioned earlier.
Positive reinforcement and vicarious learning in a safe environment
Observation of others undertaking a task during a session can make it more likely that other group members will attempt it (Reference Lewinsohn and ClarkeLewinsohn 1999). They learn from others that carrying out a task or changing a viewpoint can have positive outcomes (vicarious learning). Furthermore, the general support and encouragement of the other group members, which is a product of group cohesion (Reference White and FreemanWhite 2000), further encourage participants to engage in tasks that they may otherwise have avoided. Positive outcomes are likely to be reinforced by praise from the therapist and other group members (positive reinforcement) after completing tasks both during sessions and between sessions as homework (Reference Lewinsohn and ClarkeLewinsohn 1999; Reference MorrisonMorrison 2001).
The experience of mastery
Teaching problem-solving skills will be a part of most CBT groups. Many people find applying problem-solving to other people's problems easier than applying it to their own (Reference Hollon, Shaw, Beck, Rush and ShawHollon 1979). By providing an environment in which group members can safely suggest solutions for other group members, individuals practise the skills inherent in problem-solving and gain a sense of mastery (Reference White and FreemanWhite 2000). The aim is to generalise these skills by encouraging individuals to apply them to their own problems.
How can group CBT be delivered?
From small-group therapy to psychoeducation
Practitioners of CBT have devised group protocols that deliver cognitive–behavioural principles in innovative and diverse formats. One way of classifying the range of group formats is on a continuum from ‘small groups’ through to ‘large-group psychoeducation’ (Reference MorrisonMorrison 2001). The characteristics of the ‘therapy’ delivered at these two extremes are outlined in Fig. 1. In reality, most groups will have elements from both ends of the continuum.
The psychoeducational format has been defined as ‘high volume’ and ‘low contact’: large numbers of attendees can be ‘treated’ at one sitting, although the interaction between the attendees is minimal. Sessions are delivered in a more traditional didactic teaching style (Reference Cuijpers, Smit and VoordouwCuijpers 2005). Examples include the stress control programme developed to treat large numbers of people with anxiety in primary care (Reference WhiteWhite 2004; Reference Kellett, Clarke and MatthewsKellett 2007a) and all-day workshops for stress and self-confidence (Reference Main, Elliot and BrownMain 2005; Reference Brown, Elliott and BoardmanBrown 2008). The large-scale stress workshops of Brown and colleagues contained 20–25 participants. When you consider that these workshops allowed self-referral and were offered during the weekend in a leisure centre, then the potential to offer services with reduced stigmatisation can be appreciated. Of particular interest is the fact that over 70% of attendees who referred themselves fulfilled criteria for an ICD–10 diagnosable disorder. Many of these attendees' mental health problems were not known to their general practitioners (Reference Brown, Boardman and ElliottBrown 2005). As the lowered anxiety ratings achieved in the workshops were maintained at 2-year follow-up (Reference Brown, Elliott and BoardmanBrown 2008), the potential of such interventions to deliver significant public mental health improvements can be appreciated (Reference Brown, Boardman and ElliottBrown 2005).
Advantages of having co-therapists
There are advantages to having more than one therapist in group CBT sessions. A second therapist has the flexibility to leave the room with a distressed patient or to note changes in a patient's mental state that may not be apparent to a therapist working alone. This monitoring can be more easily carried out when the group is smaller.
Although it is harder to tailor the content of group therapy sessions to meet the needs of individual members' formulations it is not impossible, particularly in smaller groups. However, group therapy may not be able to follow an individual's formulation completely (as each patient's formulation is different) as would be the case in individualised therapy (Reference MorrisonMorrison 2001).
The influence of group size on therapy
Most group CBT will attempt to incorporate the key characteristics of individually delivered CBT. The therapist aims to promote a group culture that encourages gentle challenging and questioning of preconceptions. In smaller groups this style allows group members to interact in such a way that they serve as de facto therapists to each other (Reference Heimberg, Salzman and HoltHeimberg 1993). Homework tasks are an integral and essential component of CBT, so that the principles addressed during sessions can be generalised outside them. The therapist should review the outcomes of the homework, although the extent to which this can happen for all group members is questionable in very large psychoeducational groups.
It is clear that the experience of attending an ‘intimate’ small CBT group of five will be very different from that of attending a large psychoeducational didactic group with little interaction between group members. This has implications in terms of the active ingredients of the particular form of CBT delivered. It can be hypothesised that some of the factors outlined in the previous section will be particularly important in small groups – such as the ability to use other group members as co-therapists. Other factors, such as the normalising effect of having the same problem as so many other people who make up the group, may be more active in larger psychoeducational groups (Reference Kellett, Clarke and MatthewsKellett 2007b). However, this remains to be proven.
Who can benefit from group CBT?
In addition to whether there is an evidence base supporting the use of group CBT for a particular condition or problem, other patient factors need to be considered. Box 2 summarises factors that are believed to influence therapeutic success in individual CBT (Reference MooreyMoorey 1996). The presence of any of these variables need not preclude CBT: a patient may have multiple Axis I diagnoses or significant Axis II problems and still gain great benefit from CBT. It is simply that these factors need to be taken into account when a clinical decision is made about whether to progress with therapy.
BOX 2 Variables that may impair outcome in individual CBT
-
• Coexisting DSM–IV Axis I diagnoses
-
• Coexisting substance misuse
-
• Coexisting DSM–IV Axis II diagnoses
-
• More severe presentation
-
• More chronic presentation
-
• Psychosocial factors such as ongoing severe stress or relationship problems
-
• Strong, fixed negative core beliefs (schemas) about self
-
• Little motivation to change
-
• Difficulty in identifying a clear goal for therapy
-
• Difficulty in understanding and working with the CBT model (linked to ‘psychological mindedness’)
-
• Patient cannot or will not complete homework tasks outside of the sessions
These factors also undoubtedly apply to the consideration of a person's suitability for group CBT. Box 3 outlines additional factors that may indicate whether someone will be able to use or to benefit from group-based therapy. These should be considered alongside the general CBT suitability factors (Box 2). Measured consideration of these factors is needed before a decision is taken to include a person in a particular CBT group. For example, the presence of a more severe or chronic problem, or coexisting personality problems, may make someone suitable for a small group in which close monitoring of risk and mental state is feasible. They may not be suitable for a large psychoeducational group that does not offer this potential. Similarly, patients with severe self-harm may still be treated within CBT groups provided that provisions can be made to manage their behaviour. This can be made easier when other group members have the same or similar presenting problems. Indeed, CBT groups are usually populated by people who have the same type of problem or diagnosis. The major reason for this is that the model of CBT used (and associated treatment approaches) varies greatly between disorders, far more than is usually the case for many other psychotherapies (e.g. psychodynamic psychotherapy). Placing people with very disparate diagnoses in a single CBT group is likely to result in treatment that is confusing and at any given point will not be directly relevant to some of the group members.
BOX 3 Additional factors that may indicate that someone is less suitable for CBT in group format
-
• Communication problems sufficient to severely interfere with group interactions
-
• Potentially disruptive factors such as aggression or a severe tendency to dissociate or self-harm, causing distress to self and others
-
• Active suicidal ideation – better treated individually so that close monitoring of mental state is easier
-
• Presence of multiple conditions, making identification with the problems of others in a group less likely
-
• Known interpersonal factors such as extreme competitiveness or a tendency to dominate group environments, which are likely to interfere with group function
-
• A fear of group environments sufficient to impair concentration or cause a high risk of disengagement
-
• Patient choice: the individual prefers another model or format to address their problem(s)
Other factors may suggest that a candidate for CBT may be able to tolerate group therapy more easily than individual therapy. For example, the patient may feel that individual therapy is ‘too intrusive’, with group therapy allowing for greater anonymity. This will probably make larger psychoeducational groups particularly attractive. Some patients have a history of forming very strong and sometimes destructive (often dependent or regressive) relationships in one-to-one therapy – no matter what the model. Although there is no guarantee that this will not happen in group CBT (towards therapist or other participants), these patients may tolerate a group environment better and make behavioural change without seemingly being derailed.
Removing a patient from the group
In all groups some people will progress better than others. Occasionally, for reasons such as a deteriorating clinical state or disruptiveness, it will be necessary to remove a group member from the group. They may transfer to one-to-one treatment or, in extreme cases, exit treatment altogether. Some therapists ask group members at the beginning of therapy to sign a therapy contract which includes provisions for ending treatment. Even if that level of formality is not used, all group CBT should begin with a discussion and agreement of group rules which the therapists and group members verbally agree to abide by. These will include items such as not interrupting another group member, respecting others and punctuality.
Is group CBT effective?
There is a substantially larger body of evidence supporting the use of individually delivered CBT compared with the evidence supporting CBT in groups. However, some clinicians have erroneously taken the evidence supporting the former as implicitly supporting the latter. This ignores the likelihood that the format of the therapy, in addition to the underlying model, affects its effectiveness. From the summary of the current evidence base relating to depression and anxiety disorders outlined below, it can be seen that we cannot unequivocally conclude that group and individual CBT interventions have equivalent outcomes. Tucker & Oei have analysed the evidence base for group and individual CBT to calculate which is the most cost-effective (Reference Tucker and OeiTucker 2007). They tentatively deduce that group CBT is more cost-effective for depression, but less cost-effective for anxiety and social phobia. They point out that the available evidence has significant methodological shortcomings (including whether the efficacy trials can be generalised into naturalistic settings) and conclude that ‘It cannot be summarily or definitively stated that group CBT is a cost-effective treatment’.
Depression
The recently updated NICE guidelines on depression (National Collaborating Centre for Mental Health 2009a) state that there is a place within the stepped care model of treatment for group CBT based on the ‘Coping with Depression’ approach (Reference Lewinsohn, Clarke and HobermanLewinsohn 1989; Reference KuehnerKuehner 2005). This approach, which uses the concepts of traditional CBT, has a strong psycho-educational element and consists of twelve 2-hour sessions over 8 weeks (sessions are twice weekly for the first 4 weeks). The guidelines comment that this traditional CBT group approach has a medium effect size for mild depression. However, because they find that group CBT is less cost-effective than low-intensity approaches (such as bibliotherapy and computerised CBT) they recommend that the latter be the first-line treatment in the majority of cases. Interestingly, because of this evidence supporting the use of low-intensity interventions and traditional group CBT for milder depression, the guidelines have now removed the previous recommendation for counselling as a first-line treatment for mild to moderate depression. Specifically, the guidelines recommend that group CBT should be considered: ‘for people with persistent subthreshold depressive symptoms or mild to moderate depression who decline low-intensity psychosocial interventions’ (p. 250).
In addition to traditional CBT groups, the updated NICE depression guidelines also continue to recommend mindfulness-based cognitive therapy, which is generally provided in group format (Reference Segal, Williams and TeasdaleSegal 2002). Groups meet for eight weekly 2-hour sessions with four follow-up sessions in the following year. Mindfulness has developed from Buddhist principles of meditation and has a specific remit in this context of reducing the relapse rate rather than treatment of depression during an episode (Reference Teasdale, Segal and WilliamsTeasdale 2000). Consequently, it is a treatment for recurrent depressive disorder and the guidelines recommend it for people who have had at least three episodes of depression.
The NICE guidelines for depression in adults with a chronic physical health problem (National Collaborating Centre for Mental Health 2009b) appear to recommend group CBT for a greater range of presentations than is the case for the generic depression guidelines (National Collaborating Centre for Mental Health 2009a). Also, in contrast to the OCD guidelines (National Collaborating Centre for Mental Health 2006) they define group CBT as a ‘high-intensity’ psychological intervention. They recommend group-based CBT as an initial option for moderate depression associated with a chronic physical health problem and for people with milder presentations who have not responded adequately to ‘low-intensity’ interventions such as peer support groups or computerised CBT.
Generalised anxiety disorder
When considering anxiety it is worth noting again that individual studies have shown evidence of efficacy for group CBT, including that offered in the larger psychoeducational groups (e.g. Reference White, Keenan and BrooksWhite 1992, Reference White1998; Reference Main, Elliot and BrownMain 2005). A meta-analysis focusing on the psychological treatment of generalised anxiety disorder described group CBT as delivering ‘moderate outcomes’ with recovery rates of about one-third – less efficacious than individually delivered CBT, which had recovery rates of just over half (Reference Fisher and DurhamFisher 1999). The NICE guidelines on anxiety (National Collaborating Centre for Mental Health 2007) recommend that large-group CBT should be considered as a treatment for generalised anxiety disorder. However, it labels this group CBT a ‘self-help’ intervention, with less evidence of longer duration of effect than either selective serotonin reuptake inhibitors or individually delivered CBT. They also advocate the potential use of support groups (including by teleconference) that may be based on CBT principles.
Panic disorder
Individual studies have looked at specific CBT groups for panic disorder – with positive results (Reference Cromarty, Robinson and CallcottCromarty 2004; Reference Sharp, Power and SwansonSharp 2004; Reference Heldt, Manfro and KipperHeldt 2006; Reference Galassi, Quercioli and CharismasGalassi 2007). A comparison of individual and group CBT for panic and agoraphobia in primary care reported a benefit with group CBT, but it did not appear to be as efficacious as individual CBT (Reference Sharp, Power and SwansonSharp 2004). Of more concern was that, given a choice, 95% of patients chose individual CBT over group work. The NICE guidelines on anxiety disorders do advocate the use of support groups, which may be based on CBT principles, for panic disorder (National Collaborating Centre for Mental Health 2007). However, the guidelines do not mention large-group CBT for panic as they do for generalised anxiety disorder.
Obsessive–compulsive disorder
The NICE full guidelines on obsessive–compulsive disorder (OCD) describe group CBT as ‘a lower intensity treatment if the number of therapist hours per patient is below that of an equivalent course of individual CBT’ (National Collaborating Centre for Mental Health 2006: p. 98). They define the therapy in terms of the group time divided by the number of attendees, which suggests that NICE believes there to be no added advantage from interaction between group members. The guidelines include the trial of Reference Cordioli, Heldt and BochiCordioli and colleagues (2003), which showed benefit for group CBT over waiting-list controls in the treatment of OCD, in addition to observed improvements in quality of life.
Since the guidelines define group CBT as a ‘low-intensity CBT treatment’ they recommend it within a stepped care model for OCD with milder impairment. This is in contrast to individually delivered CBT (a ‘high-intensity’ treatment), which they recommend should be used for more severe OCD presentations.
Papers published since the NICE guidelines have also shown conflicting results. Reference Anderson and ReesAnderson & Rees (2007) compared group and individual CBT for OCD. They had identical treatment protocols for each therapy format. At the end of treatment the group that had received individual CBT showed most improvement although the disparity between the two treatment formats had disappeared at follow-up. Reference Fineberg, Hughes and GaleFineberg and colleagues (2005) found no difference in outcome between group CBT and relaxation therapy for OCD. A recent systematic review and meta-analysis concluded that, although there is now more robust evidence supporting the use of CBT in group format as an effective treatment for OCD, more studies are still needed to compare the relative effectiveness of CBT delivered in groups and on an individual basis (Reference Jónsson and HougaardJónsson 2009).
Social phobia
Social phobia is a natural candidate for group CBT. Not only is there the opportunity to learn from each other but the group format allows the delivery of social exposure and behavioural experiments (such as having to deliver a talk in front of the group). Although some trials have shown good outcomes (e.g. Reference Heimberg, Salzman and HoltHeimberg 1993; Reference Chen, Yumi and TetsujiChen 2007), sometimes equivalent to individually delivered CBT, this has not always been the case (e.g. Reference Stangier, Heidenreich and PeitzStangier 2003). The latter study found that both group and individual CBT effectively treated social phobia, but that the individual format was superior.
Post-traumatic stress disorder
A Cochrane systematic review of psychological approaches used to treat post-traumatic stress disorder (PTSD) concluded that there is now a reasonable evidence base supporting the efficacy of individually delivered trauma-focused CBT (Reference Bisson and AndrewBisson 2007). In comparison, the weight of research investigating trauma-focused CBT delivered in group format is very small. Nevertheless, group trauma-focused CBT was more efficacious in the evidence available (one study of a small sample) than the equivalent waiting list/usual care interventions in reducing symptoms of PTSD.
Many PTSD groups comprise patients who have had similar trauma experiences. People who perceive themselves to be survivors, whether of a natural disaster or war, may find it easier to relate to and empathise with others who have endured similar circumstances. They are also likely to need to cover similar topic areas during therapy. I have found this to be the case in a CBT group that I led for survivors of the Bali bombings.
The NICE guidelines on the treatment of PTSD do not include group CBT in their clinical practice recommendations (National Collaborating Centre for Mental Health 2005).
Conclusions
There appear to be clinical advantages and disadvantages to delivering CBT in group format (Boxes 4 and 5). Some patients appear to benefit most from individualised approaches, whereas others appear to do very well in group CBT. The potential of attracting individuals who do not want the stigma of using formal psychiatric services but who are willing to attend a psychoeducational large group in a community setting such as a leisure centre has real public mental health implications (Reference Brown, Boardman and ElliottBrown 2005). Thus, there is a case for offering a choice of CBT delivery where this can be practically accommodated. There may also be a particular role for group CBT for people who have a very specific problem in common – such as postnatal depression (Reference Milgrom, Negri and GemmillMilgrom 2005) – or for the treatment of depression associated with chronic physical ill health (National Collaborating Centre for Mental Health 2009b). It is worth noting, however, that it is not clear which conditions, and equally which personal characteristics, indicate whether a group or individual approach is likely to be most helpful for a given individual. Questions remain, not only about the relative effectiveness of group CBT compared with individual therapy (Reference Tucker and OeiTucker 2007), but also about their relative acceptability for patients and drop-out rates (Reference Heimberg, Salzman and HoltHeimberg 1993; Reference Sharp, Power and SwansonSharp 2004; Reference Semple, Dunwoody and SullivanSemple 2006).
BOX 4 Advantages of delivering CBT in groups
-
• Groups can treat more people at a time
-
• There is the opportunity to learn from the experiences and homework tasks of the other group members – so-called vicarious learning (Reference Lewinsohn and ClarkeLewinsohn 1999)
-
• Groups can be less stigmatising for some – and the stigma that there is can be reduced by the ‘normalisation effect’ of meeting others with the same problem(s) (Reference YalomYalom, 1995)
-
• CBT groups incorporate a ready ‘audience’ which can be utilised for exposure and behavioural experiments
-
• The views of other group members often carry more weight or are viewed as more ‘neutral’ than the views of the therapist(s) – useful for cognitive challenging (Reference Hollon, Shaw, Beck, Rush and ShawHollon 1979)
-
• Can be useful for people who struggle with a one-to-one professional relationship (such as those likely to form a regressive and very dependent relationship)
-
• Some people feel uncomfortable with a one-to-one professional relationship in therapy and so may prefer group work
BOX 5 Disadvantages of delivering CBT in groups
-
• Less time per patient with disadvantages inherent in this – such as a reduced ability to monitor mental state and changes in affect during the therapy session
-
• Less opportunity to tailor therapy to the individual circumstances and formulation of the patient – exacerbated by increasing the group size (Reference MorrisonMorrison 2001)
-
• Groups are less acceptable to some people and some may be too anxious in groups to concentrate fully on the content
-
• Groups may have higher drop-out rates (Reference Heimberg, Salzman and HoltHeimberg 1993)
-
• Group members may not get on and it can be difficult to prevent individuals from monopolising or forming subgroups (Reference MorrisonMorrison 2001)
-
• Groups usually require a regular time slot so that it is less likely that different patients' appointment preferences can be accommodated
-
• It can be difficult to remove a patient when it becomes clear that their problem or personality is not suitable for group CBT
-
• Group therapy may not be suitable for more severely ill individuals because of risk or concentration problems
-
• Group CBT does not have as strong a supporting evidence base as individual CBT
It has been noted that there is no clear evidence yet for the use of group CBT with people from different cultures (Reference Oei and DingleOei 2008). One critical issue pointed out by Oei & Dingle is that there is currently no coherent theory for group CBT that encapsulates both the content of the CBT model and the interpersonal processes that are occurring in the group. This may go far in explaining why the outcome research is at times conflicting – perhaps it is measuring different processes in different populations. When the theory is clearer we may be able to firmly determine the role of group CBT.
Currently, the NICE guidelines for depression, anxiety disorders (panic disorder and generalised anxiety disorder) and OCD all advocate the use of CBT delivered in groups but only under certain circumstances and within a stepped care framework. For example, they recommend group-delivered traditional CBT only for milder presentations of depression in those who decline low-intensity psychosocial interventions (National Collaborating Centre for Mental Health 2009a). All of these guidelines state or infer that group CBT is either less efficacious than individually delivered CBT or that the evidence base supporting its use is less well developed. Yet the potential of CBT delivered in group format remains – that it may afford the opportunity for patients to learn from each other and for more patients to be treated together with greater efficiency.
Innovative ways of delivering CBT in groups have been developed, as outlined in this article (e.g. the large-group format), but other potential methods are only just being explored. One such is the novel use of intensive CBT groups in the CBT department of Leicestershire Partnership NHS Trust. Patients can elect to be treated over a shorter time frame – perhaps over 4 weeks, but more intensively, with three or four sessions a week rather than the traditional one session weekly. These groups are based on similar intensive CBT developments in individual therapy (Reference Abramowitz, Foa and FranklinAbramowitz 2003; Reference Storch, Merlo and LehmkuhlStorch 2008). Initial results from our department show that this approach provides reasonable outcomes. The intensive format is very popular with many patients for a variety of reasons – most commonly because leave from work and arrangement of childcare is often easier to organise as a block over a short period of time rather than for a few hours a week over a longer period. This is an example of how creative service development can produce potential benefits and choice.
In England, the interventions provided by IAPT services (Department of Health 2008) will be dependent on the relevant NICE recommendations. It is clear that group CBT has a role within these services and despite the often tight stipulations provided by NICE, such a large development of psychological therapy services affords us with the opportunity to further innovate and measure the effectiveness and acceptability of differing approaches, including CBT in group format.
MCQs
Select the single best option for each question stem
-
1 In group CBT, a cohesive group
-
a is not believed to predict a better outcome
-
b refers to how much the CBT model is relevant to the patients' problems
-
c is likely to be most cohesive at the beginning of therapy
-
d helps the group focus on the work to be achieved
-
e is not (by definition) influenced by the therapist.
-
-
2 CBT in group format:
-
a is particularly useful in the treatment of psychotic depression
-
b has been shown to be a more effective treatment of OCD than has individual CBT
-
c is recommended within a stepped care model by the updated (2009) NICE guidelines on depression
-
d is known to be better used by men than by women
-
e almost certainly leads to better outcomes compared with individual CBT in the treatment of social phobia.
-
-
3 Patients who are likely to be potential candidates for group CBT rather than one-to-one CBT include:
-
a those who have not responded to group CBT in the past
-
b those with very severe OCD
-
c those noted to be extremely competitive with their peers
-
d those with mild depression
-
e those who express a preference for individual therapy.
-
-
4 Large-group CBT approaches:
-
a usually do not have a psychoeducational emphasis
-
b characteristically use individualised formulations to dictate all of the content of the intervention
-
c are used as a treatment for anxiety problems
-
d cannot be used by patients concurrently receiving other treatments or therapies
-
e are particularly useful for treating large numbers of people with PTSD in leisure centres.
-
-
5 In England, the Improving Access to Psychological Therapies programme:
-
a aims to increase access to both talking therapies and antidepressant medication
-
b involves the development mainly of secondary care services
-
c involves both ‘low’ and ‘high’ intensity treatments
-
d will focus on bipolar disorder and schizophrenia
-
e is unlikely to lead to the provision of group CBT.
-
MCQ answers
| 1 | d | 2 | c | 3 | d | 4 | c | 5 | c |
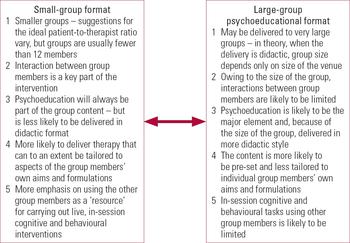
FIG 1 Continuum of CBT group delivery.




eLetters
No eLetters have been published for this article.