Introduction
Before November 2022, China’s “dynamic zero-COVID” policy (动态清零) played an essential role in containing the coronavirus and its variants during the pandemic. In contrast to lockdown policies in other countries, the Chinese government imposed stringent controls and regulations that had been reinforced through various technological upgrades and mobilised various layers of bureaucratic units to track, monitor and constrain people’s movement (Mei, Reference Mei2020; Li et al., Reference Li, Liu, Luo and Wang2021). The goal of the zero-COVID policy was to suppress the transmission of the virus within a designated geographical region and save more lives (Yang et al., Reference Yang, Zhang, Zhang, Cao and Zhang2022), yet its achievement is not without cost. For example, during the outbreak of the Omicron variant in the spring of 2022, in some reported cases, local authorities in Shanghai placed fences around residential buildings to prevent citizens from leaving; and several communities experienced limited access to food and medical care (Burki, Reference Burki2022). In addition to spatial and material restrictions, these heavy-handed approaches led to unintended negative consequences for mental health.
Since the outbreak of coronavirus in early 2020, an increasing number of researchers have shown that the lockdown strategy could slow the spread of COVID-19, but its downside costs could not be neglected (Zhang et al., Reference Zhang, Ji, Zheng, Ye and Li2020). Lockdowns have been linked to various mental health problems, including emotional and behavioural disorders and psychophysical disturbance (Adams-Prassl et al., Reference Adams-Prassl, Boneva, Golin and Rauh2022; Bueno-Notivol et al., Reference Bueno-Notivol, Gracia-García, Olaya, Lasheras, López-Antón and Santabárbara2021; Daria & Islam, Reference Daria and Islam2022; Ganesan et al., Reference Ganesan, Al-Jumaily, Fong, Prasad, Meena and Tong2021; Kumar & Nayar, Reference Kumar and Nayar2021; Newlove-Delgado et al., Reference Newlove-Delgado, McManus, Sadler, Thandi, Vizard, Cartwright and Ford2021). These mental health consequences were evidenced to vary according to the stringency of local lockdown measures in different countries since the degrees of compliance with lockdown measures differ (Hale et al., Reference Hale, Angrist, Goldszmidt, Kira, Petherick, Phillips and Tatlow2021).
Most of the foregoing literature focused on the overall impacts of lockdown policies, while little research has examined the direct effects of strict stay-at-home and quarantine orders by taking local neighbourhood spatial settings into account. The socio-spatial density and structure of neighbourhoods create an important venue to examine the patterns for the spread of viral diseases and provide a unique setting to understand how lockdown measures and policies affect mental health. Furthermore, there is less research investigating the mediation effects of lockdown-related factors, including restraints on material supply and medical care, neighbourhood social interaction and people’s trust in COVID policy.
Against this backdrop, this study asks two research questions. First, how did the lockdown interventions affect urban residents’ psychological distress, and how may they affect residents from adjacent non-lockdown communities? Second, how did the shortages of material supply and medical care, social interaction among neighbours and trust levels towards COVID policy explain the lockdown effects on psychological distress? To respond to the above questions, this study examines the direct impact of lockdowns on mental health under the dynamic zero-COVID policy in China. This study adopts a spatial quasi-experimental design to select locked and unlocked residential compounds as experimental and control groups within the same administrative district to examine the spillover effects of lockdowns. This research design allows us to rigorously quantify the psychological consequences of the COVID-19 lockdowns while also shedding light on the impact of neighbourhood spatial features on urban residents’ mental health, as well as accounting for the effects of social connections, political trust and the local community’s capacity in providing material supply and medical care for its restrained residents.
Theoretical background
The spillover effects of community lockdown on mental health
While lockdown policies are the most effective strategy to prevent and control the community transmission of COVID-19 (Cai et al., Reference Cai, Hu, Lin, Ren and Chen2022), they have unintended negative consequences on mental health. Many studies reported adverse effects of the lockdown on mental health, as manifested in increased levels of psychological distress and poor psychological well-being (Gao et al., Reference Gao, Zheng, Jia, Chen, Mao, Chen and Dai2020; Rossi et al., Reference Rossi, Socci, Talevi, Mensi, Niolu, Pacitti, Di Marco, Rossi, Siracusano and Di Lorenzo2020; Torales et al., Reference Torales, O’Higgins, Castaldelli-Maia and Ventriglio2020; Zhang & Ma, Reference Zhang and Ma2020). The symptoms of lockdown-induced mental problems include depression, anxiety, anger, insomnia, emotional exhaustion, acute stress symptoms, bipolar disorders and even suicidal ideation (Brooks et al., Reference Brooks, Webster, Smith, Woodland, Wessely, Greenberg and Rubin2020; Gan et al., Reference Gan, Ma, Wu, Chen, Zhu and Hall2022; Rajkumar, Reference Rajkumar2020; Rubin & Wessely, Reference Rubin and Wessel2020).
Lockdown policies during the COVID-19 pandemic can have spillover impacts on the mental health of individuals in non-lockdown communities, both directly and indirectly. Residents in non-lockdown communities may experience stress and anxiety about the potential of community transmission from neighbouring lockdown communities to their communities due to physical proximity. However, though previous research on spatial spillover effects correctly indicated that surrounding areas would be affected by lockdowns, scholars failed to clearly identify the geographical limit of such effects. For instance, Yang et al., (Reference Yang, Zhang, Zhang, Cao and Zhang2022) revealed that public panic during the pandemic showed hierarchical and neighbourhood diffusion, with stronger influences at the outbreak sites, economically developed areas, and surrounding areas. Similarly, Davis et al., (Reference Davis, Gross and Ochsner2011) and Liberman et al., (Reference Liberman, Trope, Stephan, Kruglanski and Higgins2007) noted the positive relationship between psychological distance and spatial distance, and this relationship directly contributes to an increase in mental health concerns. Therefore, neighbourhood lockdowns lead to fear and concern about non-lockdown residents’ health and the health of their family members, which can negatively impact their mental health.
On the other hand, lockdown policies can directly lead to social isolation and disruption of routines, which can cause loneliness, depression and anxiety (Brooks et al., Reference Brooks, Webster, Smith, Woodland, Wessely, Greenberg and Rubin2020; Daria & Islam, Reference Daria and Islam2022; Rossi et al., Reference Rossi, Socci, Talevi, Mensi, Niolu, Pacitti, Di Marco, Rossi, Siracusano and Di Lorenzo2020). For instance, residents in non-lockdown communities may be unable to see their friends and family members since they are restricted from and concerned about traveling to nearby lockdown areas due to the risk of infection. This can lead to feelings of social disconnection and loneliness, which are known risk factors for poor mental health. While lockdown policies are designed to protect public health in areas with COVID-19 transmission, they can have unintended consequences on neighbouring communities, particularly geographically adjacent ones. Therefore, we test the following hypothesis:
Hypothesis 1. Lockdown is negatively associated with the mental health conditions of urban community residents, and it also has spillover effects on residents from neighbouring non-lockdown communities.
Lockdown policies, material supply and medical shortages and mental health
The fear of being infected was the leading risk factor for mental health problems when COVID-19 initially broke out in late 2019 (Ren et al., Reference Ren, Huang, Pan, Huang, Wang and Ma2020). However, people would be exposed to a broader range of lockdown-related stressors under quarantine settings, such as supply shortages, banned social gatherings, restrained activities and confined space, all of which adversely contribute to the mental health conditions of residents (Amerio et al., Reference Amerio, Brambilla, Morganti, Aguglia, Bianchi, Santi and Capolongo2020; Brooks et al., Reference Brooks, Webster, Smith, Woodland, Wessely, Greenberg and Rubin2020; Hou et al., Reference Hou, Lai, Ben-Ezra and Goodwin2020; Wang et al., Reference Wang, Kamerāde, Bessa, Burchell, Gifford, Green and Rubery2022). Safety nets to preserve livelihoods may be scarce during the epidemic, especially in developing countries (Fan et al., Reference Fan, Li, Liu, Yue and Boustras2021; Cai et al., Reference Cai, Hu, Lin, Ren and Chen2022). People under lockdowns were thrown into a survival status in which they needed to worry about food and primary medical care, as lockdowns raise the risk of income cessation and limited access to necessities with the suspension of production and outpatient care, the closure of stores and the disruption of supply chains (Hamadani et al., Reference Hamadani, Hasan, Baldi, Hossain, Shiraji, Bhuiyan and Pasricha2020). Inadequate distribution of daily necessities and supply shortages produced by the pandemic frustrate residents’ physiological needs, thereby generating risks for their psychological conditions during a lockdown (Gloster et al., Reference Gloster, Lamnisos, Lubenko, Presti, Squatrito, Constantinou and Karekla2020; Pfefferbaum & North, Reference Pfefferbaum and North2020; Rahman et al., Reference Rahman, Hasnain and Islam2021).
Moreover, access to medical services, social services and other basic infrastructure, such as sanitation, is also significant in fostering mental health (Ranscombe, Reference Ranscombe2020). Regular lockdowns might exhaust the country’s medical capabilities and put a massive strain on medical resources. The restraining regulations on medicines and the strict rules on physical movement also limited the access and delivery of non-COVID drugs and medical treatments. A lack of essential medical resources has been identified as a significant risk factor for psychological disorders under the COVID-19 pandemic and lockdown policies (Jia et al., Reference Jia, Xu, Zhang, Cheng, Han, Xu and Zhou2021; Ren et al., Reference Ren, Huang, Pan, Huang, Wang and Ma2020). In summary, we propose the following hypothesis:
Hypothesis 2. A lack of material and medical supplies caused by the lockdown is negatively associated with the mental health conditions of community residents, which are important mediators that explain the lockdown effects.
Social capital, political trust and mental health
Neighbourhoods comprise one of the most critical social ecosystems for individuals, especially in China, where collectivism is valued (Huang, Reference Huang2006; Steele & Lynch, Reference Steele and Lynch2013). Previous literature has proposed the mechanisms through which neighbourhood-level processes promote individual mental health, one of which is community social capital (McElroy et al., Reference McElroy, McIntyre, Bentall, Wilson, Holt, Kullu, Nathan, Kerr, Panagaki, McKeown, Saini, Gabbay and Corcoran2019; Qiu et al., Reference Qiu, Liu, Liu and Li2019). Social capital refers to the resources embedded in one’s social networks, including both cognitive and structural components, with the former focusing on norms, beliefs and attitudes that promote cooperation and the latter highlighting the social relations and connections within a community (Coleman, Reference Coleman1988; Kawachi et al., Reference Kawachi, Subramanian and Kim2008; Putnam, Reference Putnam1993; Wu, Reference Wu2021).
Various indicators of community social capital, such as community-based collaboration and social support from neighbourhoods, positively predict individual mental health (Henderson & Whiteford, Reference Henderson and Whiteford2003; Wind et al., Reference Wind and Komproe2012). Social connection and social support, as representative forms of social capital, help individuals cope with stress, stay resilient, and sustain mental health (Pancani et al., Reference Pancani, Marinucci, Aureli and Riva2021). Combating the COVID-19 epidemic collectively may promote individuals’ mental health by generating solidarity and fostering social integration. However, the spread of the COVID-19 pandemic and lockdowns have disrupted face-to-face interactions, decreased social connectedness and imposed social isolation (Banerjee & Rai, Reference Banerjee and Rai2020). To be specific, lockdowns decrease social capital by disrupting social contacts and limiting access to social support, which frustrate the psychological need for relatedness and induce an increased risk of internalising and externalising disorders among people in COVID-19-affected communities (Bartscher et al., Reference Bartscher, Seitz, Siegloch, Slotwinski and Wehrhöfer2021; Luo et al., Reference Luo, Zhang, Shen, Yin, Yang and Jia2022).
In addition to social capital, people’s trust, confidence and consensus in the government’s capacity to quickly suppress community transmission also influence their mental health during the pandemic. Political trust can be broadly categorised to include five levels along the lines of ‘political community, regime principles, regime performance, regime institutions, and political actors’ (Norris, Reference Norris1999). Considering the foregoing fivefold categorisation, this definition helps find some kernels of truth concerning the relationship between political trust and mental health. First and foremost, in the broader study on the role of political trust on mental health during the global pandemic, scholars agree that such trust shields people from threats; during COVID-19, those who trust their governments do not worry as much as those who do not exhibit political trust (Dryhurst el al., Reference Dryhurst, Schneider, Kerr, Freeman, Recchia and Van Der Bles2020; Lindstrom & Mohseni, Reference Lindstrom and Mohseni2009). Second, concerning depression, Choi et al. (Reference Choi, Jung and Kim2023) argue that political trust can play a protective role for ‘those who worry more and feel more anxious about COVID-19’. Based on these studies, political trust is negatively associated with depression. Moreover, when individuals have high levels of political trust, they are more likely to have faith in the ability of their government to manage crises and address social problems effectively. This can lead to feelings of safety and security, therefore reducing stress and anxiety levels. By way of contrast, low levels of political trust can lead to feelings of uncertainty, fear and distrust, which can increase stress and anxiety levels. Therefore, the foregoing observation leads to our third hypothesis:
Hypothesis 3. Neighbourhood social interaction and people’s trust in the government’s ability to suppress community transmission and consensus towards zero-COVID policy are related to lower levels of psychological distress and significantly explain the lockdown effects on mental health.
Data and methods
Research site and data collection
Since November 2021, the Omicron variant of SARS-CoV-2 has swiftly supplanted the Delta variant as the dominant circulating strain, posing severe challenges for the world’s epidemic control efforts. Since the Omicron variant has quickly spread across the country, the Chinese central government has reinforced the nationwide mobilisation for the ‘dynamic zero-COVID policy’. To some extent, local citizens from all other major cities in which COVID cases have been identified have to go through the inconveniences of community lockdown. In February 2022, a new wave of Omicron infection rapidly emerged in Shanghai, causing the city to become the epicentre of this new variant. By May 4, 2022, the Shanghai Municipal Health Commission announced that 593,336 cases had been diagnosed, including 538,450 asymptomatic patients. As a result, Shanghai was poised to enter a 3-month-long strict lockdown for the entire city.
Our research team conducted a community-based online survey in April 2022 in Hangzhou, a major city known for its proximity to the epicentre of Shanghai. We retrospectively collected information on the lockdown interventions that had been implemented by local officials in the selected neighbourhood (shequ, 社区) that included three residential compounds (xiaoqu, 小区). The selected neighbourhood in this study was established in 2016, which includes four residential compounds, and has approximately 3,200 households in 2022. Since one residential compound was built in 2020 and had a limited number of households, it was excluded from the study. As Hangzhou has undergone rapid urbanisation, it is a rising middle-class neighbourhood outside the downtown area of Hangzhou. In April 2022, the average housing price of the examined neighbourhood was approximately 40,000 RMB per square metre, which is above the average housing price for the city of Hangzhou, 34,000 RMB per square metre.
In the selected neighbourhood, one residential compound, as the treatment group, experienced a 2-week strict lockdown intervention from March 13 to 27, 2022. All residents were not allowed to enter or leave the compound since there was one identified case of COVID-19. The other two residential compounds that did not receive lockdown intervention were considered as control groups. Residents who joined their neighbourhood social media WeChat groups were invited to participate in the online survey. Survey respondents answered questions regarding their life experiences over the 2 weeks of lockdown. The survey asked respondents to evaluate their mental health conditions, trust level about the zero-COVID policy and social connections with their neighbours. Furthermore, they were asked to report sociodemographic information about themselves and their families. A total of 522 participants in three residential compounds completed the questionnaires. The treatment group consisted of 178 participants, and 344 participants were from the two control groups.
The initial research design attempted to randomly select residents from all households in three residential compounds for on-site questionnaire interviews. On-site interviews can help to increase the response rate. However, due to strict epidemic control, local community officials could not provide specific individual information on the sampling frames due to their protection of residents’ privacy in sealed-off residential compounds. In addition, because of the zero-COVID policy, we could not conduct on-site interviews and only collect data through online questionnaires. As suggested by local community officials, we distributed the online questionnaires to the WeChat group in the community. During the epidemic control period, all households were asked to join and be included in a WeChat group created by local officials. These WeChat groups were used daily for communication purposes – informing residents of relevant information with regard to pandemic control and other important notices and messages from the local community. Through these WeChat groups, we could reach out to as many households as possible, thus improving the sample’s representativeness. However, we cannot rule out the possibility of a low representation of the elderly population in the sample. They may have limited access to digital devices and the internet, resulting in sample selection bias.
Ethical concerns
When collecting COVID-related data in China, it is necessary to comply with the research ethics and to obtain permission and support from the local government. We submitted the questionnaire for review by the local government and community officials and sought their approval. This is a prerequisite for the data collection process for our research project. According to the previous research, the initial questionnaire included a series of standardised scales measuring psychological distress, social capital and political attitudes. Because local officials deemed many questions on the standardised scales to be sensitive, we revised the questionnaire and the standardised scales. For example, they believed that the question of suicide could have a negative guiding effect on the residents, especially during the epidemic lockdown. They, therefore, deemed the initial design unsuitable for distribution. Therefore, we made corresponding adjustments to the original scales and questions, and the revised questionnaire passed the review by the local government and community officials. We acknowledge that this solution may affect the reliability and validity of the measurement, resulting in some measurement errors.
Overall, we have attempted to collect data from all possible sources; however, due to the pandemic and the restrictions placed on in-person research, the data we have collected is not perfect. We have attempted to use online sources to access more households, but the data is still limited due to censorship. However, as a valuable historical record, our data reflects the real reactions of urban community residents to the lockdown interventions during China’s zero-COVID period.
Quasi-experimental design
Figure 1 shows the map of the studied neighbourhood and the spatial locations of treatment and control groups. Our research design yields two essential features. First, although we do not have control over the treatment and it is not randomly assigned, the confirmation of the first identified COVID case in the selected neighbourhood can be considered a random event, and the assignment of treatment resembles a natural quasi-experimental design. In addition, according to local community officials, residents of the studied neighbourhood are from similar sociodemographic backgrounds and receive the same community services, which yields a substantial homogeneity of background factors. Thus, the current design can account for systemic differences among treatment and control groups and avoid selection bias. Second, we purposefully select two control groups to directly examine the spillover effects of lockdown intervention on the mental health of residents in non-lockdown residential compounds. As shown in Figure 1, control group A is separated from the treatment group by a river and is close to a subway station, while control group B and the treatment group are adjacent to each other. We expect that the lockdown intervention will have a more substantial spillover effect on mental health when comparing the treatment group and the control group B. Consequently, our design reveals that the influences of lockdown depend on the neighbourhood’s spatial settings.
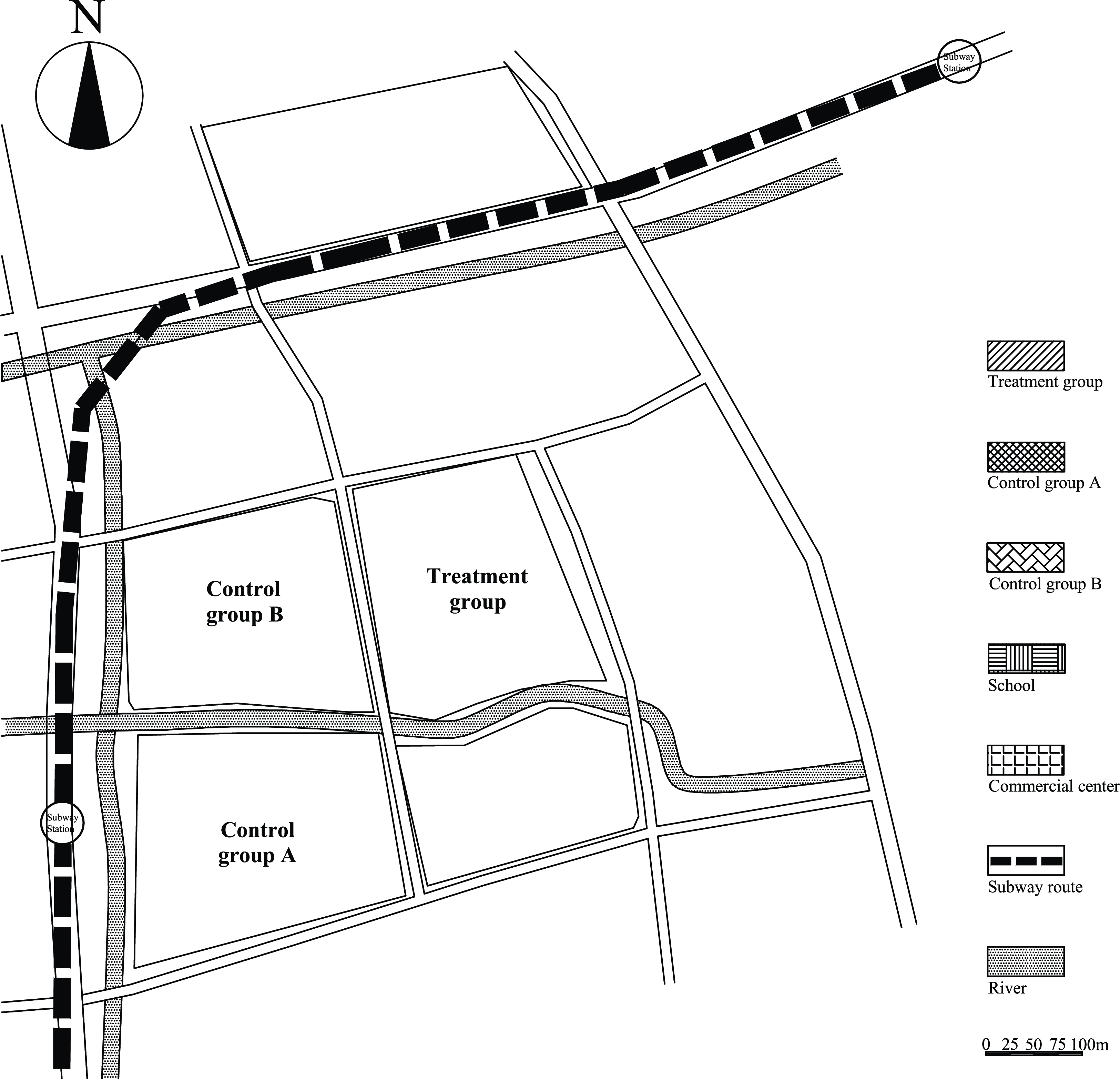
Figure 1. Illustration of spatial quasi-experimental design examining the lockdown effects on mental health.
Measurements
Outcome variable
A nine-item composite variable is constructed to measure respondents’ psychological distress. Participants were asked to rate on a four-point Likert scale how tired, nervous, helpless, unrested, anxious, fearful and worrisome they felt during the past week (1 = not at all to; 4 = most of the time). The nine-item measurement yields a high internal consistency. The Cronbach’s alpha coefficient is 0.94. The factor analysis shows that the first extracted factor based on nine scale items through principal component analysis accounts for 68% of the total variance.
Key independent variables
We include a series of dummy variables to capture the treatment and control group status and examine the lockdown effects. The treatment group, the residential compound that experienced lockdown interventions, is the reference group.
Other covariates
As discussed above, we first control whether participants experienced material or medical supply problems during the 2-week lockdown period (1 = yes; 0 = no). Second, we control how often the respondent communicates with their neighbours within the residential compound during the past month (1 = never; 5 = talk with neighbour daily). Third, a four-item composite variable is constructed to measure the levels of trust and consensus that residents have toward the dynamic zero-COVID policy. The Cronbach’s alpha coefficient is 0.80. Respondents were asked to answer whether they agree with the following statements (1 = strongly disagree; 5 = strongly agree): (1) epidemic prevention and control are more important than economic development; (2) epidemic prevention and control are more important than personal freedom; (3) strict measures should be taken to prevent overseas import, even if it has a certain impact on daily life; (4) epidemic prevention and control are the most important task of the government at present. Finally, models include controls for sociodemographic factors. Control variables include gender (female = 1; male = 0), age, participants’ household registration status (local Hukou = 1; non-local Hukou = 0), family annual income (1,000 RMB), educational attainment (junior high school or below as reference group; senior high school; junior college; university degree and above), household size, marital status (married = 1; unmarried = 0), and self-reported health status (poor = 1; excellent = 5).
Analytical strategies
The analyses proceed in three steps. First, descriptive statistics demonstrate the observed differences between treatment and control groups in the studied neighbourhood. Second, a series of Ordinary Least Squares (OLS) regression models are used to examine the association between lockdown interventions and psychological distress, with medical care and material support problems, communication with neighbours, and trust with COVID policy as important mediators of such relationships. More importantly, we examine the different effects of lockdown interventions on psychological distress by comparing different control groups accounting for the neighbourhood spatial setting to demonstrate the spillover effects. Third, we acknowledge that unobserved confounders may cause bias; that is, some unmeasured factors related to the lockdown interventions and psychological distress may explain their association, with no true causal effect. As a result, we conduct a sensitivity analysis to check the robustness of our findings. Sensitivity analysis considers how strongly the unmeasured confounder would have to be associated with the treatment and outcome variables for the treatment–outcome association not to be causal. As suggested by VanderWeele and Ding (Reference VanderWeele and Ding2017), we calculate the E-value to perform the sensitivity analysis. The E-value is the minimum strength of correlation on the risk ratio scale that an unobserved confounder would need to have with both the lockdown interventions and psychological distress to fully explain away the estimated effect, net of observed confounders (VanderWeele & Ding, Reference VanderWeele and Ding2017).
Results
Table 1 shows descriptive statistics for the observed covariates from the total, treatment and two control samples. The results show that there is a statistically significant difference in psychological distress between the treatment and control group A, where the standardised score is .142 for respondents in the lockdown compound, and the score is −.160 for those in the control group A, with a .302 difference in the scale of standardised scores. However, although respondents in control group B who did not experience lockdown have lower scores for psychological distress than their counterparts who suffered from the lockdown, this gap between the treatment group and control group B is insignificant. Furthermore, we do not find statistically significant differences in all other background factors among different residential compounds. This is consistent with our interviews with local community officials that residents in all studied residential compounds have similar sociodemographic backgrounds.
Table 1. Descriptive Statistics by Community Lockdown Status
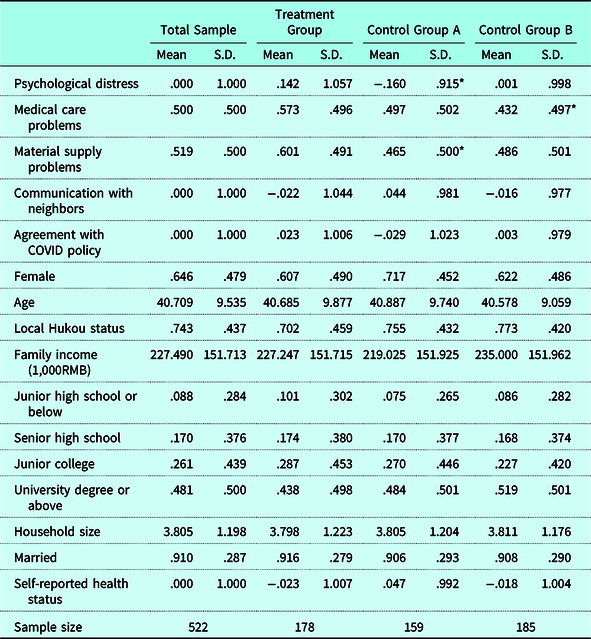
Note. Asterisks indicate a statistically significant difference of means between the treatment and designated control group.
*p < .05; **p < .01; ***p < .001 (two-tailed).
Table 2 presents results from OLS regression models examining the effects of lockdown on psychological distress. In Model 1, the results show that without adding background controls, there is a statistically significant difference in the psychological distress scale between the treatment group and control group A, but not for the control group B. Compared to the residential compound that experienced lockdown interventions, the standardised psychological distress scale is .301 scores lower in the control group A, and .141 scores lower in the control group B. These results suggest that local community lockdown interventions have direct and negative impacts on mental health and may have a spillover effect on adjacent residential compounds.
Table 2. OLS Regression Models Estimating the Effects of Lockdown on Psychological Distress
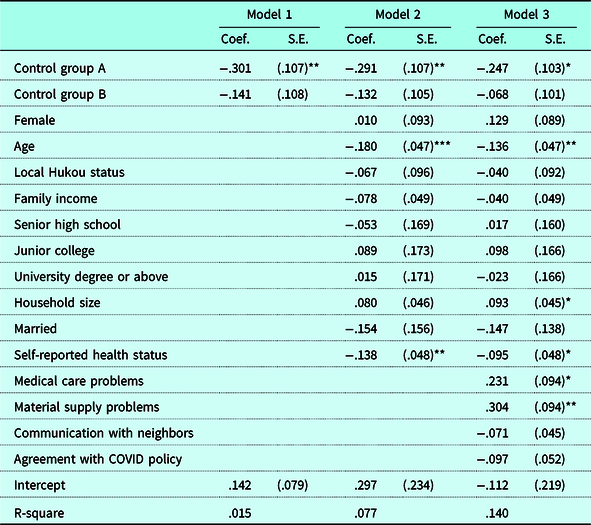
Note. N = 522. Robust standard errors are in parentheses. The treatment group and junior high school or below are the reference groups.
*p < .05; **p < .01; ***p < .001 (two-tailed).
Model 2 adds sociodemographic factors to the model. We see that younger respondents tend to have significantly higher levels of psychological distress compared to their older counterparts. Respondents who self-report better health status have lower levels of psychological distress. Model 3 further examines the influences of mediating variables. The results show that medical care and material supply problems significantly increase psychological distress. Communication with neighbours and respondents’ trust levels of COVID policies are negatively associated with psychological distress, but their effects are not statistically significant. These results indicate that the lockdown interventions strongly and negatively impact mental health after controlling for background factors. Compared to social capital and political trust, medical care and material supply shortages significantly explain the variation in psychological distress.
Table 3 reports results from the Karlson-Holm-Breen (KHB) decomposition to examine how the shortage of material and medical supplies, communication with neighbours and trust levels of COVID policies help to explain the lockdown effects on psychological distress. The KHB method is used to estimate the relative contributions of the shortage of material and medical supplies, communication with neighbours and trust levels of COVID policies to mediate the association between the community lockdown and psychological distress (Breen et al., Reference Breen, Karlson and Holm2018). The KHB method accounts for rescaling between non-linear models and can be applied to linear models. The results show that the shortage of material and medical supplies, communication with neighbours and trust levels of COVID policies explain 15.18% of the association between the lockdown and psychological distress when comparing the treatment group and control group A, and 48.70% of the association between the lockdown and mental health when comparing the treatment group and control group B. Across individual measures, shortage of material and medical supplies are the most influential mediators of the relationship between the lockdown and psychological distress, while communication with neighbours and trust levels of COVID policies play limited roles in explaining the lockdown effects.
Table 3. Mediation Analysis of Lockdown Effects on Psychological Distress
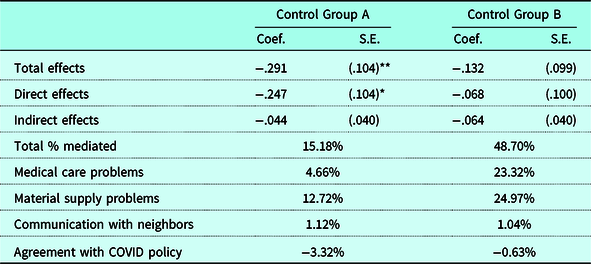
Note. N = 522. Standard errors are in parentheses. Reference group is the treatment group. Models include controls for gender, age, local Hukou status, family income, educational attainment, household size, marital status, and self-reported health status.
*p < .05; **p < .01; ***p < .001 (two-tailed).
To check the robustness of the effect of lockdown interventions, we conduct a sensitivity analysis and calculate the E-value (VanderWeele & Ding, Reference VanderWeele and Ding2017). As shown in Figure 2, the observed effect of .247 standard deviations could be explained away by an unmeasured confounder that was associated with both the treatment and the outcome by a risk ratio of 1.81-fold each, above and beyond the measured confounders, but a weaker confounding factor may not do so. The confidence interval could be moved to include the null by an unobserved confounder related to both the treatment and the outcome by a risk ratio of 1.25-fold each, net of the observed confounders. As suggested by VanderWeele and Ding (Reference VanderWeele and Ding2017), in the context of social sciences research, effect sizes greater than two- or three-fold occasionally occur but are not particularly common, and a variable that affects both treatment and outcome each by two- or three-fold would likely be even less common. Overall, these analyses provide some evidence to confirm the effect of lockdown interventions on mental health but cannot completely rule out the possibility of endogeneity.

Figure 2. Sensitivity analysis on the OLS estimator of lockdown effects. Note: The E-value is the minimum strength of association, on the risk ratio scale, that an unmeasured confounder would need to have with both the treatment and outcome, conditional on the measured covariates, to explain away a treatment–outcome association.
Discussion and conclusion
Using a spatial quasi-experimental design, this study assesses the psychological consequences of COVID-19 pandemic lockdowns in the context of China. We found that lockdowns lead to more mental health problems among young urban dwellers and that strict lockdown measures tend to have spillover effects on adjacent communities. With all other variables controlled, the negative impact of the lockdown was strong and significant, and its effect size was nearly .25 in standardised units. This finding is consistent with previous studies, which demonstrated that many psychological disorders emerged due to the lockdown (Brooks et al., Reference Brooks, Webster, Smith, Woodland, Wessely, Greenberg and Rubin2020; Gan et al., Reference Gan, Ma, Wu, Chen, Zhu and Hall2022; Rajkumar, Reference Rajkumar2020). In addition, the results reveal the spatial spillover effect of lockdown on the dwellers’ mental health of the adjacent community, which sheds light on the strong impact of urban planning on people’s mental health. These results suggest that neighbourhood spatial arrangements and housing environments influence mental health and can further alter the impacts of lockdown interventions. This study not only confirms the existence of spatial spillover effects but also outlines how far, the physical distance, those effects can travel. Indeed, our research shows that the psychological distance of control group B was farther than control group A, because the former was separated from the outbreak site by a river, despite being in the same community. Overall, Hypothesis 1 was supported, suggesting the strong negative influence of lockdown on people’s mental health.
Among the lockdown-related stressors, namely a lack of material supplies and medical care, social interaction and trust levels of COVID-19 policy, only the lack of material and medical support is a significant predictor of residents’ mental health, which also are more important mediators for explaining the lockdown effects. Thus, Hypothesis 2 was supported by our empirical findings, while Hypothesis 3 was not. This finding also corresponds to a large cross-national study covering seventy-eight countries, which revealed that an insecure financial situation and limited access to basic supplies were the strongest predictors of unfavourable psychological outcomes (Gloster et al., Reference Gloster, Lamnisos, Lubenko, Presti, Squatrito, Constantinou and Karekla2020).
We found that social interaction was not significantly related to residents’ mental health. This finding does not align with most previous literature indicating that social capital functioned as a protective factor against psychological distress during the COVID-19 pandemic (Rung et al., Reference Rung, Gaston, Robinson, Trapido and Peters2017; Wu, Reference Wu2021). It may be due to our measure of social capital, which yields several limitations. While the frequency of social interaction can provide insights into the magnitude of interactions, it may not capture the quality of those interactions. Further, social capital is a multifaceted construct that encompasses various dimensions, including structural, cognitive and relational aspects (Cohen-Cline et al., Reference Cohen-Cline, Beresford, Barrington, Matsueda, Wakefield and Duncan2018). While the frequency of social interaction may capture the structural dimension, it may not fully capture the cognitive and relational dimensions of social capital, such as shared norms, values and social support networks. Previous research has found that cognitive social capital, compared with structural one, had stronger associations with mental health (Cohen-Cline et al., Reference Cohen-Cline, Beresford, Barrington, Matsueda, Wakefield and Duncan2018). In the present study, the items used to evaluate social capital mainly reflect structural rather than cognitive aspects of social capital. The measurement bias might be a possible reason for the non-significant results.
Moreover, in the early stage of the COVID-19 pandemic, dwellers in communities with high social capital tend to engage in socially desirable activities, whether willingly or as a result of the compulsory lockdown policy (Borgonovi et al., Reference Borgonovi, Andrieu and Subramanian2021), which may protect them from anxiety and panic when the information on the virus was less known. Nevertheless, when knowledge about the virus becomes available, the function of social capital might reduce as fear of infection is no longer a prominent predictor of individual mental health beyond the initial period of the pandemic (Borgonovi et al., Reference Borgonovi, Andrieu and Subramanian2021). Furthermore, the neighbourhood was relatively loose in urban communities where interactions between neighbours were not as frequent as in rural areas (Jia et al., Reference Jia, Xu, Zhang, Cheng, Han, Xu and Zhou2021). The lockdown policy was implemented administratively in a top-down approach that each family was in the same situation. There was little space for residents’ community participation and mutual support.
This study contributes to the body of knowledge on the consequences of COVID-19 lockdown policies. Several prior studies on COVID-19-related topics had endogeneity problems due to data restrictions. To ensure the internal validity of this study, we adopted a spatial quasi-experimental design involving experimental and control groups in a selected administrative district to examine the psychological consequences of lockdowns. This research design controls the disruptive and unexpected external shocks, therefore providing a more rigorous investigation of the effect of the lockdown on the mental health of community dwellers in China. Accordingly, this study provides strong empirical evidence for relevant policies and practices, based on which we proposed the following implications for policymakers, civil servants and social workers.
The results imply that the dynamic zero-COVID-19 policy affects residents’ mental health in the quarantined communities. It may have lasting impacts on different layers of social lives. Addressing mental health problems during the pandemic period needs to rely on multi-level measures through the collaboration of multiple sectors. First, governments may initiate to explore and design a new model of epidemic prevention and control that could contain the virus’s spread without resorting to disruptive lockdowns. Considering the significant effect of supply shortages on mental health, welfare provision should be targeted at residents with low socioeconomic status who suffer from deficiencies in primary material and medical resources to maintain their psychological well-being. Second, social services or intervention programmes must be designed to improve community integration by promoting mutual communication and maintaining social contacts in lockdowns. Because quarantine prevents face-to-face contact, digital-based interventions could be implemented to encourage sociability, provide online social support and sustain social connectedness among quarantined residents, all of which have been proven to be essential for mental health protection (Pancani et al., Reference Pancani, Marinucci, Aureli and Riva2021). Third, the physical environment influences urban residents’ mental health near the quarantined communities. Based on our empirical findings, lockdown arrangements, such as setting physical barriers and fences between quarantined and open communities, could be adopted to reduce the spread of the virus but could lead to more psychological distress for residents in adjacent communities. Finally, in contrast to lockdown interventions, vaccination is a long-term and effective strategy to build immunity against COVID-19 in the population, which helps to reduce the transmission of the virus by reducing the number of infected individuals who can transmit the virus to others. Thus, a holistic plan for promoting mental health is needed for the quarantined communities and the designated areas.
Several limitations need to be noted. Regarding the variable measurement, the current study used a self-design scale that may have measurement bias. Future research may adopt well-validated measurement tools incorporating multiple indicators to assess cognitive and structural components of social capital and political trust. Also, this study used items covering a series of negative emotional symptoms to measure the concept of psychological distress. Following the current trend of the dual-factor model of mental health with positive and negative indicators (Antaramian et al., Reference Antaramian, Huebner, Hills and Valois2010), future research could examine the effect of lockdown on psychological well-being and distress simultaneously. Furthermore, concerning the research design, despite the spatial quasi-experiment ensuring high internal validity when assessing the impact of lockdowns on mental health, longitudinal studies could be conducted to collect pre- and post-test data and examine within-person changes before and after lockdowns to provide more rigorous evidence on the psychological impact of lockdowns. Finally, future research may explore the potential pathways underlying the relationship between lockdowns and mental health to enrich the influencing mechanisms. The heterogeneous effect of lockdowns for subgroups by gender, age, marital status and socioeconomic status could also be tested, which could be beneficial for providing specific evidence to deliver targeted services for each group.
Competing interests
The authors declare none.







