Primary and secondary prevention are crucial to tackling the health burden of child obesity and its associated co-morbidities. The World Health Organization Report of the Commission on Ending Childhood Obesity recommends the provision of ‘family-based, multi-component, lifestyle weight management services for children and young people who are obese’ as part of universal child health care( 1 ). Family-based interventions are central to addressing childhood obesity as parents shape their child’s home environment and lifestyle behaviours, including diet and physical activity( Reference Gicevic, Aftosmes-Tobio and Manganello 2 ).
Parenting, Eating and Activity for Child Health (PEACH) is a multi-component lifestyle intervention for families with overweight and obese children of primary/elementary school age. The effectiveness of PEACH has been previously shown in a randomised-controlled trial (RCT) with a clinically and statistically significant 10 % reduction in BMIz at the end of the 6-month intervention that was maintained 18 months later with no further intervention( Reference Magarey, Perry and Baur 3 ). PEACH aims to support parents to modify their child’s lifestyle through a whole-of-family approach and is consistent with the Australian Clinical Practice Guidelines for the Management of Overweight and Obesity in Adults, Adolescents and Children( 4 ). The 6-month facilitated group-based programme targets, and is delivered to, parents as the agents of change. A key element of the PEACH programme is parenting and the provision of parental strategies to set limits around lifestyle behaviours as parenting self-efficacy has been inversely associated with parent ability to encourage healthier child behaviours( Reference Gerards, Hummel and Dagnelie 5 ).
PEACH Queensland (QLD) received government funding to scale the evidence-based PEACH programme for delivery to families in community settings across the Australian state of Queensland. The call for tender by the Queensland Department of Health to increase the capacity of Queensland families to adopt healthy lifestyles related to healthy eating and physical activity and promote healthy weight and weight management through sustainable behaviour change provided an opportunity to evaluate the implementation outcomes of PEACH when delivered at scale. The PEACH QLD funder outcomes of interest were about implementation of the programme, and health behaviours pre- and post-programme as a measure of whether benefits of the programme shown previously via RCT remained when the programme was upscaled.
Although efficacy of PEACH and other programmes has been assessed during early stages of development( Reference Oude Luttikhuis, Baur and Jansen 6 ), few child obesity management programmes with demonstrated efficacy have been scaled up for implementation in the community or as part of community health services and findings disseminated in the literature( Reference Fagg, Chadwick and Cole 7 , Reference Hardy, Mihrshahi and Gale 8 ). Implementation and evaluation of efficacious interventions delivered at scale are an important step in translating childhood obesity research into effective management services within universal child health care.
The overall aim of this study is to evaluate outcomes of a multi-component lifestyle programme for families with overweight or obese children delivered in a ‘real-world’ service/practice setting. PEACH was translated and upscaled from the PEACH intervention previously demonstrated to be efficacious in a research setting. As such, the design of the translational evaluation presented here purposefully does not include a control group.
Methods
The Parenting, Eating and Activity for Child Health programme
PEACH has been described in detail elsewhere( Reference Magarey, Perry and Baur 3 , Reference Golley, Magarey and Baur 9 , Reference Golley, Perry and Magarey 10 ), but is briefly guided by six principles: (1) work as a family for children’s health; (2) be role models; (3) be balanced and consistent when parenting; (4) base family meals and snacks on the Australian Guide to Healthy Eating (AGHE( 11 )); (5) be active often and in a variety of ways; and (6) make healthy choices easy choices. Developing parenting self-efficacy is a core component of the programme. Parents are encouraged to lead behaviour change in their families by planning ahead; setting goals; managing behaviour and consequences; and being role models.
Parenting, Eating and Activity for Child Health Queensland
The Queensland Department of Health awarded a tender to Queensland University of Technology (QUT) in 2013 to deliver PEACH to 1400 children. Stated tender aims were to (1) increase the capacity of the families to adopt healthy lifestyles related to healthy eating and physical activity, and to (2) promote healthy weight and weight management through sustainable behaviour change. The external evaluation (pre- and post-programme design) was subcontracted to researchers led by A. M. M. and J. M. at Flinders University (South Australia) and is described in detail elsewhere( Reference Moores, Miller and Perry 12 ). The evaluation was approved by Queensland Children’s Health Services Human Research Ethics Committee (HREC) (Reference HREC/13/QHC/25); QUT HREC (Reference 1300000633); Flinders University Social and Behavioural Research Ethics Committee (Reference 6231); and Central Queensland University HREC (Reference H13/09-173). Parents provided written, informed consent to participate in this research for themselves and their child. PEACH QLD was registered with the Australian and New Zealand Clinical Trials Registry (ACTRN12617000315314).
Inclusion criteria for children were as follows: (1) residing in Queensland, Australia; (2) above a healthy weight for their age and sex as determined by United States Centers for Disease Control and Prevention (US-CDC) BMI ≥85th percentile; (3) aged 5–11 years; (4) having a parent with sufficient English to participate in the group sessions; and (5) not concurrently participating in any other lifestyle programme. PEACH was delivered to parents via ten 90-min, face-to-face group sessions by parent facilitators. As in the RCT, sessions one to nine were initially delivered fortnightly (eighteen groups). Subsequently, in response to parent and facilitator feedback, a need to improve engagement and to provide organisational efficiencies, group sessions (for eighty-seven groups) were delivered weekly to align with school terms. This change, and other changes during PEACH QLD implementation, has been previously reported in detail elsewhere( Reference Croyden, Vidgen and Esdaile 13 ). Regardless of session frequency, session 10, a reflection and evaluation session, was held approximately 6 months after the start of the programme, with a median of 23 (interquartile range (IQR): 21·5–26·0) weeks. Facilitators aimed to provide three individual phone calls between sessions 9 and 10 to reinforce messages and provide encouragement. While parents attended group sessions, children participated in active and healthy lifestyle activities in separate, concurrent group sessions conducted by two child facilitators. Facilitators were health professionals with relevant experience and received standardised training. Parents could enrol in the programme up to session 3. Pre- and post-programme evaluation data were collected at the first session attended by the family and at session 10. Families not attending session 10 were prompted up to three times to complete surveys by email and/or telephone.
Family demographics
Demographic characteristics including family composition and parent education, country of birth and indigeneity were captured in parent-completed questionnaires. Residential postcodes were used to determine the following: (1) socio-economic index using the Socio-Economic Indexes for Areas Index of Relative Socio-economic Disadvantage (SEIFA IRSD 2011)( 14 ); and (2) geographic remoteness using the Accessibility/Remoteness Index of Australia (ARIA 2011+)( 15 ). IRSD comprises seventeen measures including low income, low education, high unemployment and level of unskilled occupations. In general, a low IRSD score indicates relatively greater disadvantage, and a high score indicates a relative lack of disadvantage. The ARIA measure of remoteness of Australian areas yields five categories ranging from highly accessible (major cities) to very remote. For the purpose of this paper, parent refers to the supervising adult of children enrolled in PEACH and includes primary caregivers (biological, adoptive and step-parents), as well as other carers (grandparents).
Parent outcomes
Parenting self-efficacy
Parenting self-efficacy has been inversely associated with parent ability to encourage healthier child behaviours( Reference Gerards, Hummel and Dagnelie 5 ). Parenting self-efficacy was measured pre- and post-programme using a four-item questionnaire from the Longitudinal Study of Australian Children( Reference Lucas, Nicholson and Maguire 16 ). Each item enquired about the child’s behaviour relative to the parent’s desires or the parent’s self-perceived ability to manage their child’s behaviour. Responses were given on a five-point Likert scale, ranging from ‘never/almost never’ to ‘sometimes’ to ‘always/almost always’ and have been collapsed for reporting. Two items were reverse-scored( Reference Hinkin 17 ) and an overall parenting self-efficacy score was calculated by averaging the scores from the four items. A higher mean score is indicative of higher parenting self-efficacy.
Child outcomes
Child anthropometrics
Child weight, height and waist circumference (WC) were measured by the trained child facilitators pre-programme (normally at the first session attended) and post-programme (session 10) using standard procedures and study-provided equipment. In the absence of facilitator-measured anthropometry data, parent-measured child height and weight were collected where possible (pre-programme 6·9 % (n 52) and post-programme 6·7 % (n 22)). Age- and sex-standardised z scores were calculated using the US-CDC2000( Reference Kuczmarski, Ogden and Guo 18 ) (heightz, weightz, BMIz) and UK1990( Reference Freeman, Cole and Chinn 19 ) (waistz) references. Biologically implausible values for z scores defined by the US-CDC( 20 ) were excluded from analyses, in addition to children who did not have an increase in height from pre- to post-programme. Children were categorised as healthy weight, overweight, obese or morbidly obese using International Obesity Taskforce extended thresholds. A waist:height ratio of ≥0·5 was considered excessive.
Child diet
Parents completed the forty-item semi-quantitative Children’s Dietary Questionnaire (CDQ)( Reference Magarey, Golley and Spurrier 21 ), and ten-item Core Food Group Intake Tool( Reference Golley, Magarey and Daniels 22 ). The previously validated CDQ assesses frequency and variety of intake of foods and food behaviours of particular relevance to children in the context of overweight( Reference Golley, Magarey and Daniels 22 ). Four diet quality scores – (1) fruit and vegetables, (2) non-milk sweetened beverages, (3) fat from dairy products and (4) discretionary foods (high fat/high sugar) – are determined from twenty-eight items estimating the variety of fruit and vegetables consumed, frequency of intake of non-milk sweetened beverages (fruit juice/fruit drink and non-diet soft drink/cordial), reduced-fat dairy products and non-core foods high in energy, salt, fat or sugar, respectively. Target scores are based on the Australian Dietary Guidelines( 11 ). The reliability and validity of these scores at the group level has been previously reported( Reference Magarey, Golley and Spurrier 21 ). A fifth score, food behaviours, uses the remaining twelve items to assess the frequency of behaviours associated with obesity (e.g. eating in front of television, eating meals as a family, size of meals). The Core Food Group Intake Tool was used to determine the number of daily serves of foods from each of the five core food groups in the AGHE( 11 ): (1) fruit; (2) vegetables and legumes/beans; (3) grain (cereal) foods, mostly whole grain and/or high cereal fibre varieties; (4) lean meats and poultry, fish, eggs, tofu, nuts and seeds and legumes/beans; and (5) milk, yogurt, cheese and/or alternatives, mostly reduced fat. Examples of common foods in each of the five core food groups, including serve size descriptions, were provided to assist parents completing these questions. Average daily intake was estimated as ((serves on weekdays×5)+(serves on weekend days×2))÷7. The proportion of children meeting age and sex recommendations( 11 ) for each of these core food groups was determined.
Child physical activity and screen-based sedentary behaviour
Parents reported the length of time their child usually spends in physical activity and screen-based sedentary behaviours in a typical week using the Children’s Leisure Activities Study Survey( Reference Telford, Salmon and Jolley 23 ). Screen-based sedentary behaviours included watching television/videos, playing Playstation/Nintendo/computer games and using the computer/Internet. These data were used to categorise children in one of two groups – those meeting recommendations and those not meeting recommendations – separately for physical activity and sedentary behaviour, based on Australia’s Physical Activity and Sedentary Behaviour Guidelines 5–12 Years( 24 ) recommending ≥60 min/d of moderate-to-vigorous physical activity, and ≤2 h/d sedentary time, respectively. These physical activity data are available for a subsample as the measurement tool was subsequently modified to reduce participant burden with the aim of improving questionnaire completion.
Data collection, completion and statistical analysis
Data were collected via survey hardcopy or online completion (SurveyMonkey Inc.). All data were entered, cleaned and analysed in IBM® SPSS® version 23 (IBM Corp.). Continuous data were reported as bootstrapped means and 95 % CI and categorical data were reported as numbers and percentages. Repeated-measures t tests with bootstrapping were used to analyse changes over time for continuous data. Wilcoxon’s signed-rank test and related samples McNemar χ 2 test was used to assess shifts in categorical variables over time. In keeping with a comparable upscaled programme( Reference Hardy, Mihrshahi and Gale 8 ), missing values were not imputed in this study as the objective is to similarly report real-world changes in pre–post evaluation of a service delivery project. The threshold for statistical significance was set at P<0·05 and exact two-sided P values are reported.
Sample size
The PEACH Programme has previously demonstrated efficacy in a RCT of 169 children, of whom 80 % provided data at 6 months( Reference Magarey, Perry and Baur 3 ). There was a 10 % reduction in BMIz for participants in the parenting and healthy lifestyle group( Reference Magarey, Perry and Baur 3 ), which is comparable with the intervention used in the PEACH QLD Project. As PEACH QLD was funded by a service delivery tender from the Queensland Government (Australia), there were no a priori power calculation or sample size analyses. Instead, PEACH QLD had enrolment targets and initially aimed to enrol 1400 children, which was later revised to 1100 children. A total of 1184 children were enrolled in PEACH QLD, of whom 926 were above a healthy weight at baseline. This outcome paper reports the outcomes for this subsample of children. A reduction in the effect size of the PEACH intervention was anticipated with the delivery of the intervention at scale in the PEACH QLD Project; however, the magnitude of the difference in effect size between the RCT and large-scale community programme was not able to be estimated a priori owing to a lack of comparable studies in the published literature.
Results
PEACH QLD enrolled 926 overweight/obese children from families in 105 groups across Queensland, Australia, from October 2013 to September 2016. The level of engagement in providing evaluation data for families and children is shown in Fig. 1. Paired evaluation data (i.e. data provided pre-programme and post-programme) for parenting, diet, activity and anthropometric measures were available for 51 %, 51, 33 and 44 % of children with pre-programme data, respectively. Owing to variability in questionnaire completion in a real-world service delivery setting, there are varying levels of missing data resulting in differing n values for each evaluation measure.
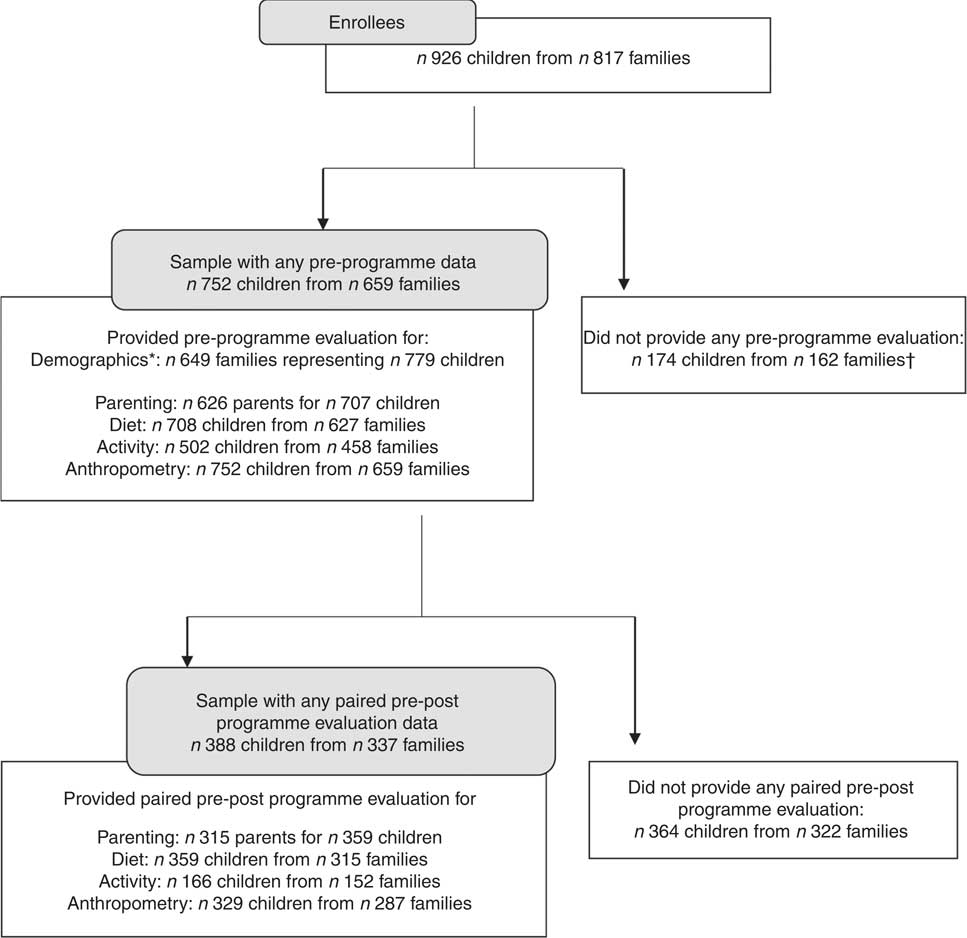
Fig. 1 Flow chart of data collected in Parenting, Eating and Activity for Child Health Queensland. * Parent and family demographic data are collected at the family level, and not for each child. Hence, some children may have parent- and family level demographics but no child-level data (e.g. diet, anthropometry). † Families with more than one enrolled child may have had children with and without child-level baseline data.
Table 1 shows characteristics of families in the whole sample who provided any demographic data pre-programme (n 659). For the purpose of evaluating completion bias, the sample was dichotomised to give two groups: those families who provided pre-programme data only (n 322) and those who provided paired pre–post-programme data (n 337). Families with paired pre–post-programme data were more likely be dual-parent households (P<0·001), be Australian-born (P=0·011) and have higher levels of education (P=0·002) compared with those with pre-programme data only. A comparison of children with paired pre–post v. pre-programme data only indicates that those with paired data were younger (−0·29 years; 95 % CI −0·54, −0·03) (P=0·029), and appeared to be proportionately more female (57 to 52 %), with a lower BMI z score (−0·039; 95 % CI −0·1, 0·026); however, neither of the latter differences reached statistical significance. At baseline, children with pre–post-programme data were 8·8 (95 % CI 8·6, 9·0) years old, and at follow-up were 9·3 (95 % CI 9·1, 9·4) years old, with the mean time between pre- and post-programme measures being 0·46 (95 % CI 0·45, 0·47) years (approximately 5·5 months). In all, 22 % (n 206) of enrolled families did not attend any sessions. Overall, for families who attended at least one session (n 618; 720 children), median attendance was 7 (IQR 3–9) of a maximum ten sessions, whereas families providing paired data (n 337 families; n 388 children) attended 8 (IQR 7–9) of ten sessions.
Table 1 Pre-programme demographics of families, parents and children in Parenting, Eating and Activity for Child Health Queensland(Numbers and percentages; mean values and 95 % confidence intervals)

SEIFA IRSD, socio-economic index for areas index of relative socio-economic disadvantage; ARIA, Accessibility/Remoteness Index for Areas.
*P reports statistical difference between sample with pre-programme data only and sample with both pre- and post-programme paired data.
† Parent demographics are reported at the family level.
‡ United States Centers for Disease Control and Prevention reference for BMIz ( Reference Kuczmarski, Ogden and Guo 18 ); extended International Obesity Task Force weight status cut-off points( Reference Cole and Lobstein 25 ).
Anthropometry
Distribution of children across weight status categories and z scores pre-programme, and for the sample with paired pre–post-programme data, are shown in Table 2. After intervention there were significant decreases in BMIz (−0·11, P<0·001) and waistz (−0·05, P=0·012). The prevalence of children classified as morbidly obese declined by 8 percentage points, corresponding to percentage point increases in prevalence of children classified as healthy weight, overweight and obese: 2, 5 and 1 %, respectively (P<0·001).
Table 2 Anthropometry for children in Parenting, Eating and Activity for Child Health Queensland(Numbers and percentages; mean values and 95 % confidence intervals)
WHtR, waist:height ratio.
*Paired-samples t test, McNemar χ 2 test or Wilcoxon’s signed-rank test used; P indicates difference between pre- and post-programme paired data.
† United States Centers for Disease Control and Prevention references( Reference Kuczmarski, Ogden and Guo 18 ) for heightz, weightz and BMIz; UK1990( Reference Freeman, Cole and Chinn 19 ) reference for waistz; extended International Obesity Task Force weight status cut-off points( Reference Cole and Lobstein 25 ); WHtR ≥0·5 considered excessive( Reference McCarthy and Ashwell 26 ).
‡ One child only BMI was available from hospital records (no separate height and weight).
Diet
Pre-programme and paired pre–post-programme changes in diet for both core foods and CDQ scores are shown in Table 3. There was a significant improvement in the proportion of children meeting age and sex recommendations( 11 ) for serves of foods from the vegetables and legumes/beans core food group (4 v. 9 %, P=0·001). There was a reduction in the proportion of children meeting the daily serve recommendation for cereal (grain) foods from 27 to 21 % (P=0·024), corresponding to a mean decrease of a third of a serve. There were significant improvements in all CDQ scores post-programme, indicating changes in consumption and behaviours in line with nutrition objectives for the programme, which are based on child diet recommendations.
Table 3 Diet intake and food behaviour for children in Parenting, Eating and Activity for Child Health Queensland*(Numbers and percentages; mean values and 95 % confidence intervals)
*708 children had any diet data pre-programme (from 676 to 683 for individual outcomes) and 359 children had any paired pre–post-programme diet data (from 320 to 351 for individual outcomes). Paired-samples t test used for continuous data; related samples McNemar χ 2 test used for categorical data.
† A higher score indicates a healthier intake/behaviour.
‡ A lower score indicates a healthier intake.
Physical activity and screen-based sedentary behaviour
Time spent engaged in physical activity and screen-based sedentary behaviour and the proportion meeting recommendations are described in Table 4, for the subsample for whom pre–post data were available (n 166). There was a mean increase of 19 min of physical activity per d (from 86 to 105 min/d, P=0·001), corresponding to a 9 % increase in children meeting this recommendation at the end of the programme (64 v. 73 %, P=0·017). The proportion of children meeting sedentary activity guidelines also increased (34 v. 50 %, P=0·001) consistent with the significant decrease of 42 min of sedentary screen time per d (190 v. 148, P=0·001).
Table 4 Time spent by the child in screen-based sedentary behaviours and moderate-to-vigorous physical activity*(Numbers and percentages; mean values and 95 % confidence intervals)

*502 children had any activity data pre-programme (from 492 to 501 for individual outcomes) and 166 children had any paired pre–post-programme activity data (from 160 to 166 for individual outcomes); values are rounded to nearest whole minute. Paired-samples t test used for continuous data; related samples McNemar χ 2 test used for categorical data.
†Recommendations are as follows: physical activity, ≥60 min/d moderate-to-vigorous physical activity( 24 ); sedentary screen time, ≤2 h/d( 24 ).
Parenting self-efficacy
Although children were the enrollees in PEACH, the intervention was delivered to parents. Table 5 reports the changes in parenting self-efficacy. Parents reported improvements in the following three domains of parenting self-efficacy. Does your child behave in a manner different from the way you want him/her to? Do you feel that you are good at getting this child to do what you want him/her to do? Do you feel that you are in control and on top of things when you are caring for your child? No significant changes were found in the domain ‘Do you think that your child’s behaviour is more than you can handle?’ This corresponded to a significant increase in overall parenting self-efficacy score (3·6 to 3·7, of a maximum 5·0, P=0·001).
Table 5 Parenting self-efficacy( Reference Lucas, Nicholson and Maguire 16 ) for parents in Parenting, Eating and Activity for Child Health Queensland†(Numbers and percentages; mean values and 95 % confidence intervals)

*Paired-samples t test used for continuous data; related samples McNemar χ 2 test used for categorical data.
†707 children had any parenting self-efficacy data pre-programme (from 705 to 707 for individual outcomes) and 359 children had any pre–post-programme paired parenting self-efficacy data (from 358 to 359 for individual outcomes).
‡ Combined score reports mean of all four items (Cronbach’s α 0·754) with items 1 and 2 (marked #) reverse scored( Reference Lucas, Nicholson and Maguire 16 ).
Summary of outcomes
Table 6 reports all outcomes from PEACH QLD and whether there was a positive change (improved), no statistically significant change or a negative change (worsened) in parenting, health behaviours and anthropometry.
Table 6 Summary table of outcomes in Parenting, Eating and Activity for Child Health Queensland

WHtR, waist:height ratio.
* P<0·05, ** P<0·01.
† (c), Child; (f), family; (p), parent.
‡ No statistically significant change.
Discussion
A growing body of literature suggests that parent-led interventions for child obesity management, or those that target family rather than individual child behaviours, are effective( Reference Berge and Everts 27 , Reference Loveman, Al-Khudairy and Johnson 28 ). Here we demonstrate that PEACH delivered to parents of obese primary school-aged children improved parent self-efficacy that in turn was consistent with favourable changes in child diet, with increases in daily serves of vegetables, variety and frequency of fruit and vegetable intake and decreases in the consumption of discretionary foods and non-milk sweetened beverages. In additionally, there were desirable changes in activity patterns with increased time spent in physical activity and decreased levels of screen-based sedentary behaviour. Overall, the stated tender aims related to enhancing capacity of families to adopt healthy lifestyles were met.
These lifestyle changes are consistent with reductions in both BMI z scores and the prevalence of obesity and overweight, indicating that PEACH remains effective when delivered at scale. Despite the fact that there was an 8 % reduction in the prevalence of morbid obesity and reduction in BMIz, at the end of the programme most children remained above a healthy weight. Hence, ongoing maintenance of lifestyle changes is required for long-term improvements in child weight status. PEACH provides parents with skills and knowledge to make sustainable lifestyle changes, and at the end of the programme parents are encouraged to continue to apply the programme principles, and these messages are reinforced at the final session, and in personalised feedback letters to families upon programme completion.
We have previously shown in an RCT that PEACH is efficacious with approximately 10 % relative weight reduction at 6 months( Reference Magarey, Perry and Baur 3 ). In the present study, we observed an approximate 5 % reduction in BMIz representing a halving of effect when delivered at scale. This effect size is similar to that shown in a recent study of children (n 1776) who participated in the 10-week Go4Fun programme (approximately 5 %, NSW, Australia), which was also approximately half the effect reported in the original efficacy trial that reported outcomes at 6 months( Reference Hardy, Mihrshahi and Gale 8 , Reference Sacher, Kolotourou and Chadwick 29 ). The Go4Fun was adapted from Mind, Exercise, Nutrition..Do it!, which had been previously delivered at scale in the UK and reported to yield a relative weight loss of 6·7 %( Reference Fagg, Chadwick and Cole 7 ). Not surprisingly, it appears that the relative weight loss that can be achieved when a parent-led child obesity programme is scaled for health service delivery will be less than that observed in more rigorous, tightly controlled RCT. Notwithstanding this reduction in effect size, we have here demonstrated effectiveness of PEACH when delivered on a larger scale as a community health programme. Although it is unlikely that any single programme can solve the complex issue of childhood obesity in isolation, the evidence-based PEACH intervention should be included within a multi-strategic approach to its prevention, which includes supporting children who are already overweight or obese( Reference Okely 30 ).
PEACH has a specific focus on parenting skills, encouraging an authoritative parenting style and supporting parents to be agents of change and role models for their child’s health behaviours. Although there was a statistically significant improvement in parenting self-efficacy score from pre- to post-programme, the magnitude of the change in the score derived from four items is notably small. However, our results show that post programme fewer parents reported their child behaving in a manner different from that they want them to, and more parents reported feeling good at getting their child to do what they want them to, and feeling in control and on top of things when caring for their child. Other studies identified in a recent Cochrane review of parent-only interventions for childhood overweight or obesity in children aged 5–11 years( Reference Loveman, Al-Khudairy and Johnson 28 ) reported inconsistent measures of parenting, which cannot be compared with each other or the present study (Parenting Scale( Reference West, Sanders and Cleghorn 31 ), Alabama Parenting Questionnaire( Reference Magarey, Perry and Baur 3 ) and Ghent Parental Behaviour Scale( Reference Moens and Braet 32 )). In addition, unlike PEACH, not all family-based child obesity programmes have a strong emphasis on parenting. Future research is needed to further understand how parenting skills training and practices can affect child and family healthy lifestyle behaviours including whether there is any interactive effect with more than one parent/caregiver, domain-specific parenting behaviours( Reference Costanzo and Woody 33 ) and the sustainability of parenting changes in the long term, including its association with child lifestyle behaviours.
Family engagement was challenging with approximately one in five enrolled families not providing any data and not attending any sessions. The characteristics of this group cannot be described owing to the lack of available data. Demographics associated with PEACH QLD attendance have been reported elsewhere: briefly, advantaged families, parents who were partnered, with higher education levels and those who self-referred to PEACH had higher programme attendance( Reference Williams, Van Lippevelde and Magarey 34 ). Of the families who provided pre-programme data, approximately half also provided post-programme data allowing pre–post-programme evaluation of effectiveness. Children with paired pre–post-programme data tended to come from families of slightly higher SES and generally had more favourable diet and activity behaviours initially than children with pre-programme data only. Overall, as expected, engagement and retention bias were evident and potentially limit the generalisability of the programme outcomes for all families with children above a healthy weight range. The relationship between disadvantage and health is complex( Reference Marmot 35 ), and although disadvantaged and minority groups have a higher burden of child obesity, engagement of these populations in PEACH was limited. This suggests that PEACH may be better suited to more highly educated, double-parent families, or as a result of their relative advantage such families may have greater resources to improve their capacity to participate and attend programme sessions.
Although attrition from the programme was not directly reported here, evaluation data provision is a reasonable proxy for attrition as anthropometric measurements were taken in the final session. Attrition rates reported in the literature vary widely, and depend on the definition( Reference Dhaliwal, Nosworthy and Holt 36 , Reference Skelton and Beech 37 ). A recent review of twenty-three studies reported a median attrition rate of 37 % (ranging from 4 to 83 %) from paediatric obesity management services( Reference Dhaliwal, Nosworthy and Holt 36 ). This review also found that older children were more likely to discontinue care; however, sex and pre-programme weight status did not predict treatment attrition. Our findings were similar with respect to age, as children with paired data were younger, but we also found evidence of differences in sex (higher proportion of females) and weight status (lower mean BMIz) for those children with paired data. The overall higher proportion of girls is in line with the PEACH RCT( Reference Magarey, Perry and Baur 3 ) and unsurprising, as previous studies have found parents of overweight girls more frequently recognised as being overweight, compared with boys( Reference Fisher, Fraser and Alexander 38 , Reference Maynard, Galuska and Blanck 39 ). The proportion of girls was then greater in the sample providing pre–post-programme data, which may indicate that parents of girls rate their need to participate in the programme, and/or its benefits to their child’s health, higher than parents of boys or that girls are more weight conscious and willing to seek/continue treatment. In addition, the over-representation of obese and morbidly obese children, compared with overweight children, indicates limited early identification of child weight issues or the possibility that child weight management programmes such as PEACH may have been considered a last resort, rather than first step, for families who have attempted to manage their child’s weight. A previous qualitative study, which explored reasons why a sample of twenty-one parents enrolled their children in PEACH QLD, reported that parents were aware of their child’s weight issue for a long time and their enrolment came after previous unsuccessful attempts at weight management and was triggered by their child’s own concern with their weight( Reference Davidson and Vidgen 40 ).
The aim of this study was to evaluate the effectiveness in the ‘real-world’ practice setting of an evidence-based service targeting families with obese children. The study purposefully did not intend to repeat the evaluation of the efficacy of the PEACH intervention. Inclusion of a control group was not required to achieve this aim, and furthermore, in the practice context, would not have been acceptable to programme recipients, the service providers who delivered the PEACH Program nor the funder as core business for both the funder and service providers is service delivery for the community rather than scholarly research. This means that we cannot extrapolate our results to those families who were not ready or otherwise unable to engage in the programme. Hence, it is difficult to say whether those families who did not provide data did/did not experience any success in the programme. At the first session, parents received a 105-colour-page PEACH workbook, which outlined the programme principles, content for each session and reputable sources for further information and support. Thus, parents had access to programme content, which they may have engaged with on an ad hoc, self-paced basis. Although the programme is designed to be facilitated by a trained professional and be group-based to enable peer support and shared learning, this may not have been enjoyable or acceptable for all parents and may have impacted engagement. Ultimately, we have no way of ascertaining the applicability or effect of PEACH on the group that did not report paired data. However, these are the very families who are unlikely to seek support from and engage with the kind of service that this study evaluates. It highly likely that a range of evidence-based practice/service responses will be required to meet the diverse needs of families with overweight and obese children. This study evaluates one such response and demonstrates that it was acceptable and effective in a select group of families. Clearly, studies are required that are specifically designed to identify other engagement strategies and features of intervention design and delivery to extend reach and range of effective service/practice level responses to childhood obesity. Ultimately, it is clear that for the sample who did engage in sessions and provide pre–post-programme data, PEACH was effective in achieving child and family lifestyle behaviour change and consequently a relative reduction in children’s level of overweight.
Strengths and limitations
A strength of the current study is the collection of comprehensive measures for lifestyle behaviours up to 4 months after completion of the intervention, rather than immediately after the end of group sessions. As such, these evaluation data provide for a follow-up period. When delivered at a larger scale, programmes may have limited evaluation depending on needs, budget and health service. When a programme is fully translated, it becomes embedded in existing practice and health services where evaluation is likely to be curtailed and restricted to limited service monitoring data such as attendance and/or rudimentary assessment of participant satisfaction.
With the exclusion of child anthropometric measurements, which were largely collected at sessions by trained facilitators, all other evaluation data (parent self-efficacy, diet, activity) were parent-reported and may be subject to acquiescence bias. Although it was not feasible for the primary school children enrolled to provide information on their dietary intake and activity behaviours, we acknowledge that there are objective measures that could have been used in place of, or to validate, parent-reported data (e.g. doubly labelled water, accelerometry). Our selection of data collection tools to assess outcomes was determined by the large sample size, evaluation budget and the needs of the funder to ascertain public health benefit – that is, data were collected with an emphasis on service provision rather than research. Therefore, our methods reflected the need to reduce participant burden and select economical methods that are feasible for use in evaluation of programmes or health services delivered at scale within the community setting.
Conclusion
When delivered on a large scale, PEACH is an effective family-based, multi-component, lifestyle weight management programme for overweight and obese children. Investment in the delivery of childhood obesity management services at scale should be informed by evidence, and the results of this study make a substantive contribution to the limited body of existing evidence. PEACH has demonstrated its effectiveness across the translation continuum. This research contributes to the limited data available on the magnitude of dietary, activity and anthropometric change, which can be expected from a programme when delivered at scale. Further research is needed to determine whether these lifestyle changes are sustainable and can be maintained in the long term following delivery at scale and the system and service factors that support such a programme being routinely available as part of universal child health as recommended by the World Health Organization( 1 ). Key challenges for efficient provision of childhood obesity management programmes include the identification of excess weight early in its evolution and the engagement of families in these services.
Acknowledgements
The authors acknowledge Ms D. Croyden for their leadership role across the project, and all staff from the Queensland University of Technology Implementation team and Flinders University Evaluation team who contributed to implementation and evaluation of the PEACH programme in Queensland from 2013 to 2016. The authors are grateful to all facilitators, parents and children for their participation in PEACH QLD.
PEACH Queensland was funded by the Queensland Government of Australia (2014–2016). The views expressed in this publication do not necessarily reflect those held by the Queensland Health Department or the Queensland Government of Australia. The PEACH Queensland Project was originally funded as a joint Australian, State and Territory Government initiative under the National Partnership Agreement on Preventive Health (2013–2014).
A. M. M. and L. A. D. conceived and designed the PEACH QLD study and its evaluation framework, and selected data collection tools. L. A. D. directed the PEACH QLD Project, H. A. V. oversaw the implementation in Queensland and A. M. M. and J. M. managed the evaluation. C. J. M. managed data collection, entry and integrity, performed the statistical analysis and wrote the first draft of the manuscript. A. M. M., H. A. V., J. M. and L. A. D. assisted with data interpretation and writing the manuscript. All authors contributed to all reviews and revisions of the manuscript and have read and approved the final version.
A. M. M. and L. A. D. are inventors of the original PEACH programme and have received licence money for the use of PEACH materials in the PEACH QLD Project. All other authors declare no conflicts of interest.









