Introduction
The coronavirus disease (COVID-19) pandemic overwhelmingly affects older people residing in long-term care homes (LTCH). They are more at risk of contracting the disease and of dying from COVID-19 (Landry, van den Bergh, Hjelle, Jalovcic, & Tuntland, Reference Landry, van den Bergh, Hjelle, Jalovcic and Tuntland2020). The death toll in these facilities is high and difficult to know precisely since many countries exclude those deaths in their statistics (Comas-Herrera et al., Reference Comas-Herrera, Zalakaín, Lemmon, Henderson, Litwin and Hsu2021).
Many older people living in an LTCH are regularly visited by family members or friends. As such, they are care partners. To minimize the risk of exposure and death from COVID-19 during the first wave, having occurred between March 1 and August 31, 2020 (Canadian Institute for Health Information, 2021), many governments implemented blanket preventive measures in the spring of 2020 and suspended visits in LTCHs. Such measures often prevented care partners from supporting their older person, most of whom were cognitively impaired. Care partners were also worried regarding the lack of human and material resources in some LTCHs (Fillion, Reference Fillion2020). As such, those care partners not only carried the same burden as the rest of society because of COVID-19, but also shouldered an additional moral and psychological burden.
There have been some studies focused on this issue in the context of LTCHs. In a survey (n = 225), O’Caoimh et al. (Reference O’Caoimh, O’Donovan, Monahan, Dalton O’Connor, Buckley and Kilty2020) found that visiting restrictions in the United Kingdom (U.K.) decreased psychological and emotional well-being of care partners during the lockdown, especially if the older person they cared for lived with cognitive impairment. However, the authors mentioned the importance of better understanding the disruption in their roles and how to support them to mitigate negative consequences. Still, in the U.K., a qualitative study was conducted during the second wave of COVID-19 with care partners (n = 26) and care home staff (n = 16) to describe the impact of the lockdown on care and visits in LTCH from their perspective (Giebel et al., Reference Giebel, de Boer, Gabbay, Marlow, Stoop and Gerritsen2022). The results showed dilemma regarding care and negative impacts on care partners and staff. Another study aimed to compare the experience of care home visiting during May 2020 in the Netherlands and October and November 2020 in the U.K. (Giebel et al., Reference Giebel, de Boer, Gabbay, Marlow, Stoop and Gerritsen2022), in which 125 care partners were interviewed. The results highlighted the various types of contacts during the lockdown, the deterioration of residents’ health, the distress of visitors, and how regulations were respected or not.
However, those studies did not inquire about the actions family care partners would need to mitigate the negative impacts of the pandemic on them and the person they cared for. This limits the possibility to implement actions that would be a direct answer to care partners’ expectations in a time of crisis. Also, studies were mostly conducted in care homes or residential care facilities in European countries that have a different residents’ profile from the one in Canada.
Situation in Canada
More specifically in Canada, Dupuis-Blanchard, Maillet, Thériault, LeBlanc, and Bigonnesse (Reference Dupuis-Blanchard, Maillet, Thériault, LeBlanc and Bigonnesse2021) conducted a longitudinal ethnography (data collection May/June and December 2020) to explore the experience of family members of a person living in an LTCH (n = 17) in New Brunswick during the first and second waves of COVID-19. The province applied strict visitor restrictions in LTCHs, but there were very little outbreaks during the first wave. In that province, the first death of COVID-19 occurred in June 2020. This study describes various factors that influenced the experience of family members, for example, the nature of the workforce and problems in communication and with public health directives. It also presents the impacts on families, such as their distress and the challenges they encountered to visit. Most of the impacts occurred for them during the second wave when there were more outbreaks than during the first wave in that province.
But this province had very few cases and deaths of COVID-19 (0.3 deaths per 100,000 population during the first wave and 2 per 100,000 population during the second wave). The only provinces with a lower rate were those with no cases (Newfoundland, Prince Edward Island, Yukon, Northwest Territories, and Nunavut) (Canadian Institute for Health Information, 2021). In comparison, Québec had the most LTCH deaths in Canada, both during the first and second waves of COVID-19, with 58 deaths per 100,000 population during the first wave (ahead of Ontario that had 14 per 100,000) and 33 per 100,000 during the second wave (Canadian Institute for Health Information, 2021). Also, in New Brunswick, LTCHs are privately owned (with or without profit) (Dupuis-Blanchard et al., Reference Dupuis-Blanchard, Maillet, Thériault, LeBlanc and Bigonnesse2021), compared with Québec where they are mostly public (Commissaire à la santé et au bien-être, 2021), which could influence how a crisis is managed in those settings. As such, it is unclear what the experience of family care partners was in the context of the high cases and death rate, such as in Québec, where LTCHs were also facing important challenges before the pandemic (Commission de la santé et des services sociaux, 2016; Estabrooks et al., Reference Estabrooks, Straus, Flood, Keefe, Armstrong and Donner2020; Protecteur du citoyen, 2021).
Pre-Pandemic Challenges of LTCHs in Québec
Just before the pandemic, at the end of February 2020, there were 43,200 beds in LTCHs in Québec (Commissaire à la santé et au bien-être, 2022b), of which 85 per cent were public or private but publicly funded (Gouvernement du Québec, 2021). The average age of residents was 84 years old (Commissaire à la santé et au bien-être, 2022b), and 45 per cent of residents were 85 years or older (Gouvernement du Québec, 2021). The number of beds did not increase between 2015 and 2019, despite the growing need for this type of care. As a result, the LTCH system was at full capacity (Commissaire à la santé et au bien-être, 2022b).
From 2015 to 2019, residents with significant care needs increased by 10 per cent, and the average care hours per day increased from 3.2 to 3.7 per resident (Commissaire à la santé et au bien-être, 2022b). Between 70 and 80 per cent of residents had cognitive impairment, and most of them exhibited responsive behaviours (e.g., vocal or aggressive behaviours) (Gouvernement du Québec, 2021). Despite these changes and the aging of the population, the share of spending on LTCHs decreased slightly between 2015 and 2019 (Commissaire à la santé et au bien-être, 2022b).
Inadequate staffing ratios were observed and reported to negatively impact resident care by delaying or cancelling various care activities (e.g., hygiene care, dressing) (Gagnon & Jeannotte, Reference Gagnon and Jeannotte2019; Protecteur du citoyen, 2019). Despite provincial norms, professional inspections had highlighted the poor working conditions of registered nurses (RNs) and their insufficient number in many LTCHs (Ordre des infirmières et infirmiers du Québec, 2014). The ratio of nurses’ aides was also considered to be disregarded. These staffing issues led to overtime work, high burnout, high turnover, and the use of private placement agencies (Commission de la santé et des services sociaux, 2016). In 2019, it was considered that at least 5,000 nurses’ aides’ positions were unfilled and that 30,000 additional nurses’ aides would be needed in the coming years due to retirements (Dubois, Reference Dubois2020). As early as 2016, it was recommended that the staffing level be adapted to the needs of residents and that recruitment and retention be improved (Commission de la santé et des services sociaux, 2016). Reports also highlighted the essential role of family care partners and the need for a better partnership between staff and the family members (Commission de la santé et des services sociaux, 2016). Despite numerous reports, complaints, and recommendations, the problems persisted (Commissaire à la santé et au bien-être, 2022b; Protecteur du citoyen, 2021).
Context of LTCHs in Québec During the First Wave of COVID-19
In February 2020, the Québec Government began pre-emptively transferring patients from hospitals to LTCHs in anticipation of a possible pandemic. A state of emergency because of the pandemic was declared on March 13. Visits to health care facilities, including LTCHs, were not allowed as of March 14. COVID-19 cases began to multiply in LTCHs around March 20, but screening was still reserved for people who had travelled. In early April, significant outbreaks and staff absenteeism due to COVID-19 were observed in many LTCHs. Massive COVID-19 screening began in mid-April, resulting in additional staff and management being removed from work because they were contagious. Additional staff from other health care facilities and people identified through a community outreach program were brought to assist the LTCHs in late April. On April 20, the Canadian Army was deployed to some LTCHs with major staffing and infection problems. The government allowed family care partners who met certain criteria to return to LTCHs starting June 18. The army left the LTCHs at the end of June, and the Red Cross took over in early July to help some LTCHs still experiencing staffing problems (Protecteur du citoyen, 2020, 2021).
During that period of March to July 2020, almost 6,000 people died from COVID-19 in Québec and 64 per cent of them lived in an LTCH (Commissaire à la santé et au bien-être, 2022a; Institut national d’excellence en santé et en services sociaux [INESSS], 2020). After controlling for age and sex, people living in an LTCH were more than three times more likely to die from COVID-19 than people living at home (INESSS, 2020). The excess mortality was 34 per cent and disproportionally higher in the Montréal region (Commissaire à la santé et au bien-être, 2022b). As of May 3, 2020, in a population of two million in Montréal (Ministère de l’Économie et de l’Innovation, 2021), 1,365 persons had died from COVID-19 (Gouvernement du Québec, 2020). Of these, 91 per cent were over 70 years old (Gouvernement du Québec, 2020), and 70 per cent lived in an LTCH or a residence for older people (Dougherty, Reference Dougherty2020).
The unknown nature of the virus led to much confusion about post-mortem measures for people who died of COVID-19. At the beginning of the pandemic, the World Health Organization guidelines stated that both cremation and burial were possible (European Centre for Disease Prevention and Control [ECDC], 2020). In Québec, however, public health initially recommended cremation over burial. This was sometimes misunderstood to mean that burial was not allowed. At the end of April 2020, this recommendation was removed. Guidelines for personal effects were also a source of confusion for a while and were eventually clarified to state that personal effects that could not be disinfected had to be quarantined for seven days before being returned to families. This generated some confusion in funeral homes and health care facilities (Massoud, Reference Massoud2020).
Many explanations have been offered to explain the magnitude of the crisis that occurred in Québec’s LTCHs. The most frequently cited are hospital-centred decisions and a lack of understanding of the unique characteristics of LTCHs and their residents, persistent staff mobility, late initiation of infection prevention and control (IPAC) measures, delay in sending additional human resources, lack of local management, and an outdated information system (Collège des médecins du Québec – Ordre des infirmières et infirmiers du Québec – Ordre des infirmières et infirmiers auxiliaires du Québec, 2021; Commissaire à la santé et au bien-être, 2022a; Dubois, Reference Dubois2020; Protecteur du citoyen, 2020, 2021).
In contrast to other provinces, Québec left staff mobility between LTCHs to the discretion of the health care facilities, resulting in variations between facilities, despite recommendations from the Ministry of Health and Social Services to avoid it. Because of the high level of mobility before the pandemic and the severe shortage of staff, staff were often moved from hot to cold zones and between LTCHs to provide the necessary care. This initially contributed to a rapid increase of COVID-19 cases in many LTCHs (Dubois, Reference Dubois2020; Protecteur du citoyen, 2020).
Systematic screening of staff and residents did not begin until the level of infection in LTCHs was already high, training in IPAC measures was late, and personal protective equipment (PPE) was lacking (Collège des médecins du Québec – Ordre des infirmières et infirmiers du Québec – Ordre des infirmières et infirmiers auxiliaires du Québec, 2021; Dubois, Reference Dubois2020). Up to 48 per cent of workers reported having lacked PPE (Collège des médecins du Québec – Ordre des infirmières et infirmiers du Québec – Ordre des infirmières et infirmiers auxiliaires du Québec, 2021; Protecteur du citoyen, 2020, 2021). This resulted in a high number of health care workers infected with COVID-19 – up to 47 per cent of that number working in LTCHs, 11 of whom died, and a high rate of absenteeism on top of workforce problems that existed before the pandemic (Commissaire à la santé et au bien-être, 2022a; Dubois, Reference Dubois2020; Protecteur du citoyen, 2020, 2021). Because family care partners, who usually contributed to some care, were not allowed to visit, this reduced the help to maintain basic care for residents (Dubois, Reference Dubois2020).
Despite early requests for additional staff from LTCHs, efforts to deploy additional human resources were difficult and slow, largely because of the challenges of quickly adapting administrative processes that did not allow many people who wanted to help to do so. Only a fraction of the people who had volunteered were able to help (Dubois, Reference Dubois2020). At the same time, over 1,350 military personnel were deployed in many LTCHs (Commandement de la composante terrestre – Force opérationnelle interarmées [Est], 2020; Dubois, Reference Dubois2020; Protecteur du citoyen, 2020).
This crisis highlighted the absence of local managers in each LTCH since a reform in 2015, which regrouped many health care facilities under the same management. This made the infrastructure rigid and complicated the efficient implementation of sanitary and mitigation measures (Protecteur du citoyen, 2020, 2021). For example, LTCHs had to negotiate with the centralized infrastructure to acquire PPE and electronic means of communication during the crisis, which led to differences between settings.
Because of the many challenges before and during the first wave of COVID-19, the situation in Québec’s LTCHs has been described as a “perfect storm” (Protecteur du citoyen, 2021). Family care partners of relatives living in a Québec LTCH, particularly in the Montréal region, which was the most affected, were on the front line to witness the situation, and they were directly impacted by its consequences, in contrast to other provinces where they were concerned about the consequences but ultimately without many dramatic consequences in terms of cases or deaths.
Given this context, a study describing the experience of family care partners in that province and their recommendations for actions can highlight more clearly what needs to be done during a public health crisis in LTCHs and give a voice to care partners. Our study had two objectives: (a) describe the experience of being a care partner of an older person living in an LTCH during the first wave of the COVID-19 pandemic in Québec, and (b) elicit and describe the recommendations of care partners for supportive actions that should guide health professionals and public policy to ensure their health and that of older people during an epidemic.
Our research was guided by symbolic interactionism (Blumer, Reference Blumer1969). Based on this theory, being a care partner in the social context of a pandemic is understood as having meanings that influence how the care partner acts. These meanings are related to the interactions a care partner has with others and are modified by reflecting and interpreting their situation. This interpretation then guides their actions.
Methods
Design
We conducted a critical ethnography that considers the sociocultural context in studying human activities. This design aims to reveal hidden agendas, power relationships, and assumptions to influence political agendas (Madison, Reference Madison2005; Thomas, Reference Thomas1993), which seemed especially relevant in regard to the context of the first wave of COVID-19 in Québec. According to Thomas (Reference Thomas1993), critical ethnography relies on the same methods and on symbolic interactionism theory as conventional ethnography but goes further by also requiring a description of what could happen, to stimulate reflection, empowerment, and changes in the social culture (Madison, Reference Madison2005; Thomas, Reference Thomas1993).
Participants
In the Québec context described above, we recruited 24 care partners of an older person living in an LTCH from Montréal using purposive and snowball sampling. Most of the care partners had participated in previous studies by the first author and had given consent to be recontacted to participate in future studies. To ensure a maximum variation sampling, we recruited two types of care partners based on the status of the older person (alive or deceased). In ethnography (Leininger, Reference Leininger2001), it is recommended to recruit at least seven to nine participants per type or until there is redundancy in the meanings of data (Hennink, Kaiser, & Marconi, Reference Hennink, Kaiser and Marconi2017). The inclusion criteria were: (a) being a person who had an emotional and social relation with a person 65 years or older living in an LTCH during the COVID-19 pandemic, and (b) fluency in English or French.
Data Collection
Participants were eager to voice their experience and recommendations by taking part in our project, and we were able to collect all data between July 10 and July 27, 2020. Sociodemographic data were collected using a questionnaire. A research assistant (GL) conducted semi-structured interviews with each care partner, using a guide based on the objectives and framework. An example question is: “Imagine that there are no resource constraints and that you could decide what actions to take to help care partners during the pandemic, what actions would you take?” In respect of public health guidelines at that time, she conducted these interviews by phone (n = 22), by Zoom (n = 1), or in person outside (n = 1) depending on the participant’s preference. Despite some beliefs, studies have shown that phone or videoconferencing interviews do not necessarily have a negative impact on the quality of data collected (Holt, Reference Holt2010; Johnson, Scheitle, & Ecklund, Reference Johnson, Scheitle and Ecklund2019). As recommended, to ensure quality non-face-to-face interviews, the interviewer carefully listened to the interviewees and was particularity attentive to non-verbal cues (e.g., silences, crying) (Farooq, Reference Farooq2015). The interviews were recorded (M = 60 minutes ± 29) and transcribed, including non-verbal cues such as silences and crying. To ensure reflexivity, the research team wrote field notes to document reflections, observations, and relations with partners (Emerson, Fretz, & Shaw, Reference Emerson, Fretz, Shaw, Atkinson, Coffey, Delamont, Lofland and Lofland2001).
Data Analysis
Two of the authors (GL and AB) listened to the audio files of the interviews and read the verbatim many times to ensure deep familiarity with verbal and non-verbal data. Then, they assigned codes to all data. Two suffixes were added to each code: one to identify the period to which the code referred (i.e., during strict lockdown or after), and another one to identify whether the older person was alive or had died. Where relevant and to help with interpretation, the codes also included the non-verbal cues, for example, crying in parentheses in the corresponding code. The codes were then sifted for similarities and differences following Spradley’s method (Reference Spradley1979), which entailed carrying out domain, taxonomic, componential, and theme analyses. The process was iterative and done by one author (GL or AB) and revised by another (AB or GL). Discussions resolved differences in interpretation. Following several iterations, the research team met to finalize the themes.
Domain analysis consisted of grouping codes with at least one common characteristic. Ten domains were identified. Taxonomic analysis involved organizing all the codes associated with a domain by assigning them to a semantic relation (e.g., X related to Y) then cross-referencing them with each other to determine whether there was a relationship. The codes with a relationship were organized hierarchically, representing the similarities and differences between the data. Componential analysis involved examining differences based on the status of the older person (living or deceased) and those related to the time frame (during strict lockdown or after). Theme analysis raised the level of abstraction through various strategies, including discussing with the research teams, a thorough rereading of verbatim to integrate results and drawing schemas of relations between potential themes (Spradley, Reference Spradley1979). We used Excel for the analysis (Meyer & Avery, Reference Meyer and Avery2009).
Ethics standards
Our study protocol was approved by an institutional ethics review board (no. CER VN 20-21-13). Informed consent was obtained from participants. The research assistant who conducted the interview was a master’s trained nurse who is highly competent in establishing a trust relationship and in assessing distress signs; she offered support to participants showing distress.
Results
Socio-Demographic Characteristics
Care partners were mostly women in their sixties (Table 1). Most participants had a post-secondary education and were the child of the older person. More than 65 per cent (16 of 24) of the care partners spent time with the older person living in an LTCH more than once a week before the pandemic. During those visits, most spent one hour or more with the older person.
Table 1. Socio-demographic characteristics of care partners
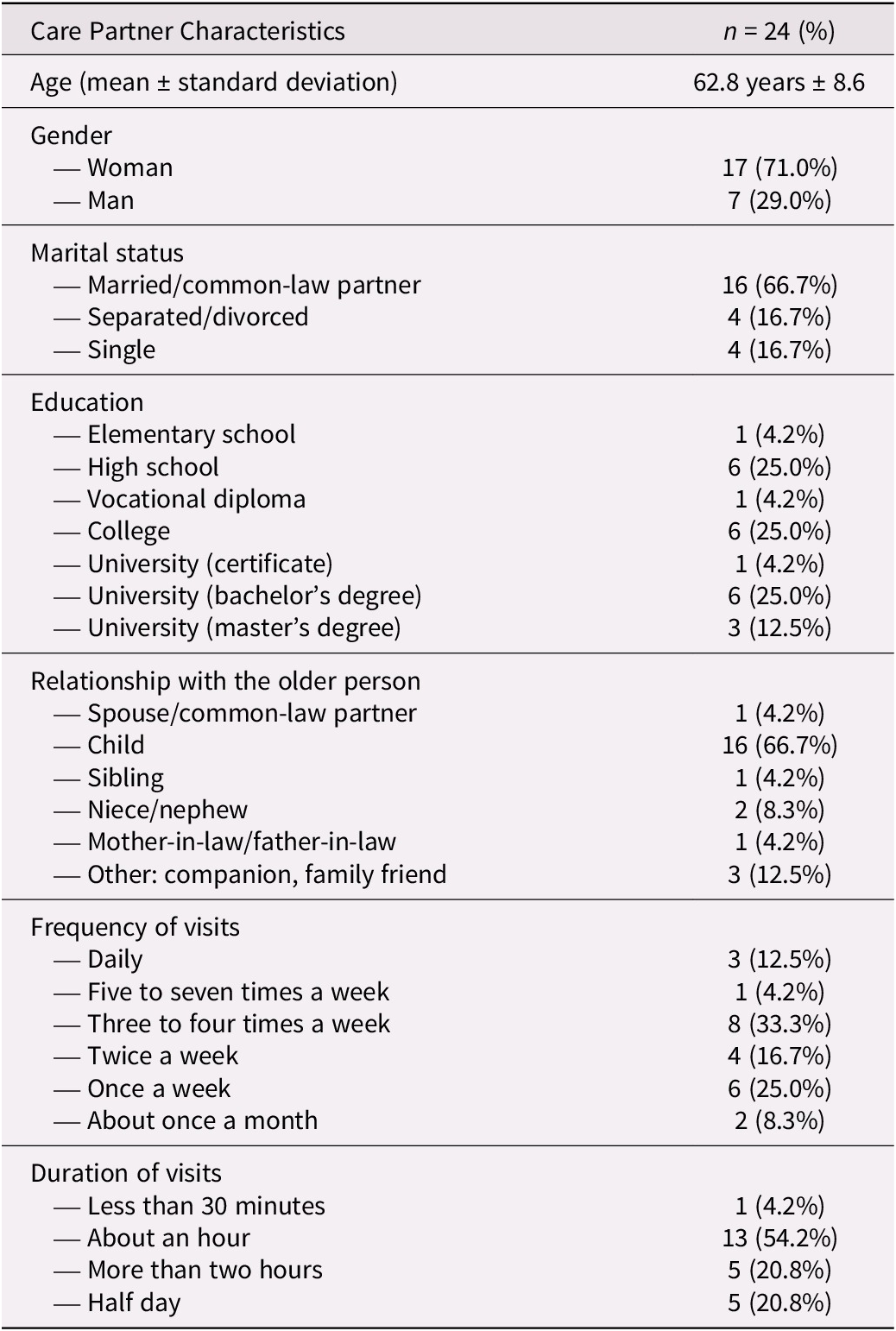
Note: Percentages have been rounded, so some totals may not be exactly 100%.
The residents were, on average, 85 years or older and were mostly women (Table 2). To be admitted in an LTCH, those residents needed at least three hours of care per day. More than 96 per cent of our sample lived in a public or private but publicly funded LTCH. The public LTCHs were regrouped in two large integrated public health centres (n = 13 on 24; 3 in one integrated health centre, and 10 in another). An integrated health centre shares the same management for many LTCHs. Residents from private but publicly funded LTCHs were from three centres (n = 10; 3 in two different ones, and 4 in the other one), and one resident lived in a private LTCH. The residents had been residing in the LTCH for more than seven months, and most had a major neurocognitive disorder. Ten of the 24 older people died during the first wave of the pandemic. Of those, seven (70%) did not see their care partner before they died.
Table 2. Socio-demographic characteristics of older people
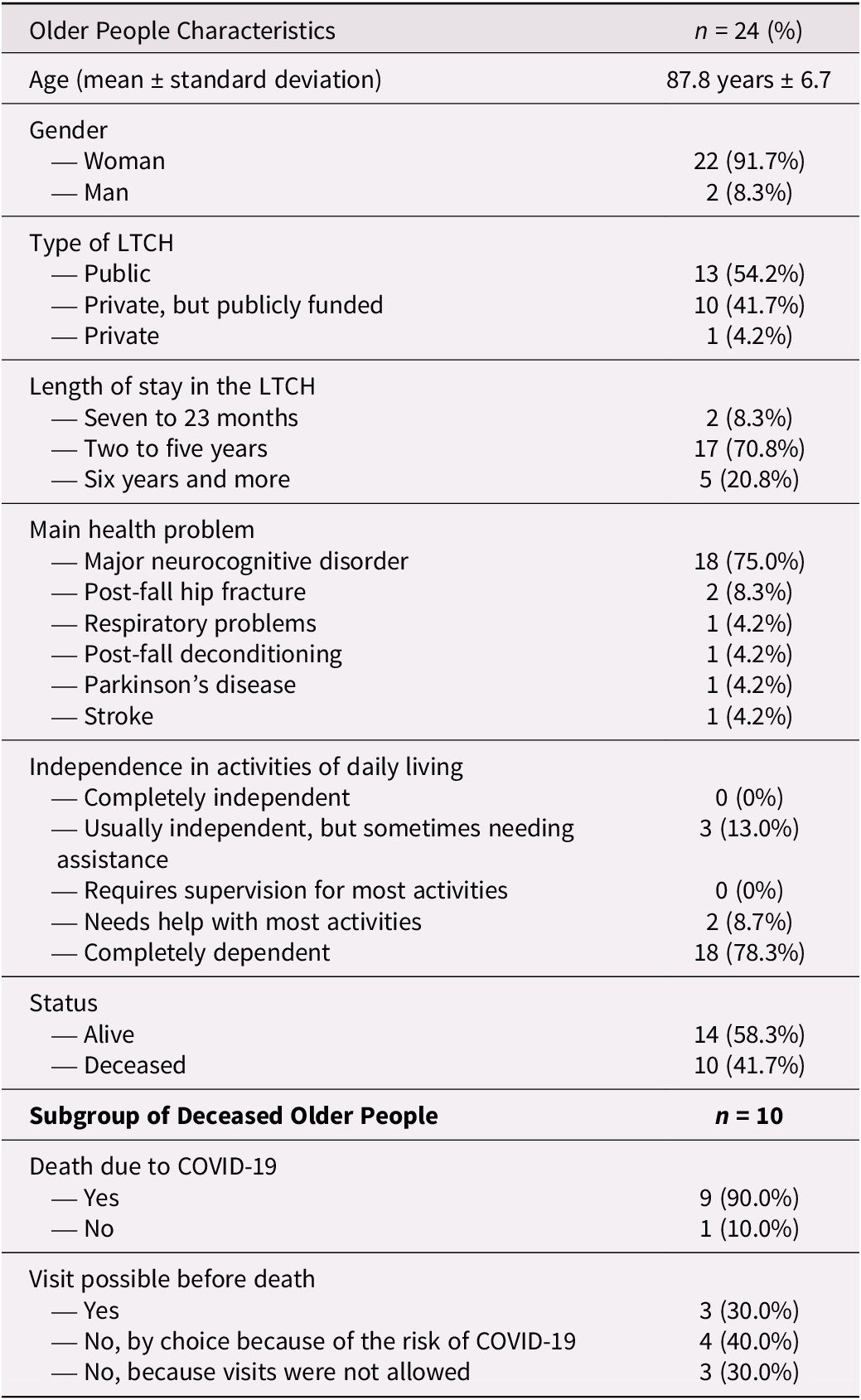
Note: Percentages have been rounded, so some totals may not be exactly 100%.
Description of Their Experiences and Recommended Supportive Actions
We identified five themes describing the experiences of care partners and their recommendations for supportive actions. All names are pseudonyms. Some quotes were originally in French and were translated for this paper.
Theme 1. Forced separation
A data analysis revealed that the older person–care partner dyad had a hard time with its forced separation due to the ban on visits in LTCHs and the high cases of COVID-19 reported. This situation generated a lot of distress for them.
Irremediably bonded: Hell for the older person, hell for us. Care partners expressed significant concerns for the well-being of the older person without being able to assume their roles with them. According to the participants, older people did not understand why their care partners had seemingly vanished, and experienced a significant decrease in their quality of life as a result. The distress of both resulted in them being irremediably bonded in this situation. They qualified it as hell for older people and for care partners. Care partners felt that older people were being held hostage or that their rights were not being respected:
They are hostages here [in the LTCH], they do not belong to you those people, they have rights, do you understand (angry tone)? They do not belong to you. (Ms. Ornella, her aunt’s care partner, line 71)
Many older people who died did so alone. This generated immense distress and anger for care partners. The lockdown resulted in an abrupt loss of their role, which was a sacrifice. However, they understood the need for protective measures for the sake of the older people’s well-being.
Care partners whose older person died were sometimes faced with a dilemma when they were allowed to visit the person at the end of life. They were torn between the possibility of visiting in the LTCH and the risk of contracting COVID-19 and contaminating relatives.
Each on our own: Impacts on our health. This situation had an undeniable effect on the health of older people and their care partners. The participants described several new or worsened health problems in the older person. The most frequent ones were that older people became bedridden and lost their independence. Malnutrition and dehydration were also reported. Several older people had greater cognitive deficits and no longer recognized their care partners. Some older people told their care partner that they had experienced anxiety or even “depression”:
She [older person] told me, ‘I have been very sick and almost died.’ I said, ‘It is true that you were very sick, you caught a virus.’ She said: ‘No, no, I had a deep depression and inside I do not know if I am still well.’ That is what she told me. (Ms. Diane, her aunt’s care partner, line 119)
This situation had an impact on the health of care partners. They reported experiencing sadness, uncontrollable crying, and fear, as well as symptoms of depression and anxiety. They also experienced loss of motivation, anger, helplessness, and guilt, which were sometimes compounded by fatigue and insomnia.
Take actions to help us: Facilitate our involvement and help us take care of ourselves. In response to the devastating effect of this forced separation, care partners recommended that their essential role be officially recognized particularly in an epidemic. They believed that visiting should never be prohibited, but rather supervised. They also wanted help to get involved with the older person appropriately during a crisis.
Our participants recommended direct support to be offered to care partners by the LTCH during a crisis. They emphasized their need to share their experience with other care partners, for example, in virtual support groups.
Theme 2. Care and support
Most participants felt the care of their older person was inadequate and, in some cases, inhumane while older people were alive and, sometimes, even after they had died. They often questioned the quality of care. A minority felt the care and support offered were good.
When there were problems, it was because of management. Our participants perceived the problems experienced in LTCHs existed for years before the pandemic and stemmed primarily from poor management:
Sincerely, [there were problems before] COVID-19… I’ve been saying it for ten years regarding long-term care homes. That’s what a long-term care home is, I’ve seen it in intermediate resources, in private homes, I’ve done them all. It’s always the same thing. When we arrived at this long-term care home, they had problems. I know that the nurses’ aides, there are good ones, there are not good ones. The problem is so much the management, it’s so, so much the management. (Ms. Xéa, whose mother-in-law died, line 53)
The participants also believed a lack of staff and instability in care teams causes inhumane situations for vulnerable people. Some participants said that staff sometimes either did not do their work or did it poorly because of a lack of supervision. They also believed that COVID-19 outbreaks were related to management problems and that LTCHs were unprepared. Participants noted that they knew the situation could have been well managed because in some LTCHs it was. In those settings, there were no COVID-19 cases, and an approach that favoured the involvement of care partners had been used before the pandemic.
Exceptionally, we trust the staff, but often we have tensions with them. The few participants who came from LTCHs and felt they were well-managed expressed confidence in the care teams:
I’ll tell you, from the start, that I was confident, [I had] a good opinion of the long-term care home, so I didn’t feel overly worried, I know that there, she is well treated, I know that the nurses’ aides are good, I have confidence in the staff there. (Mr. François, his mother’s care partner, line 102)
This trust was the exception. Most participants expressed that there was poor quality of care even before the COVID-19 crisis. Their fear about the quality of care was exacerbated when visits were prohibited. Once visits were again allowed, care partners observed staff not doing their job (e.g., not spending time on feeding or hygiene). Some participants explicitly alluded to abuse because of the lack of appropriate care:
So we were under no illusion, we knew our mother was being abused. Not in the sense that she was being beaten, but I think she was not getting the [care for the] basic needs of a 90-year-old who is ultra vulnerable, who had her eyes closed, who had no physical strength. (Mr. Quintin, whose mother died, line 165)
This situation created tension between staff and care partners when the latter requested that care be improved. Care partners reported feeling unwelcome in the LTCH and being treated unprofessionally by staff when they asked for news about the older person.
After death, it is more difficult for us than it should be. Participants whose older person died said the post-mortem interactions they had with staff or managers made an already difficult time inhumane. Their grief was particularly painful, more so than it would have been under normal circumstances, sometimes because of the way public health rules were interpreted. The older people of some care partners were cremated, against the wishes of the deceased older person because of misunderstanding of initial public health rules during the first wave. Planned end-of-life rituals were prohibited and post-mortem procedures were particularly dehumanizing. Those situations that prevented respecting the wishes of the deceased person caused a lot of suffering for care partners.
In some cases, post-mortem practices in LTCH were especially dehumanizing. Some care partners were contacted at end-of-life regarding the rapid disposal of their person’s remains following death. Some care partners were given the deceased’s personal belongings in garbage bags, others were told their belongings would be burned:
Like recently, they emailed me, well three months later [after death], to say … (he cries) all your mother’s belongings are going to be burned because of COVID, it is going to be thrown away and burned. (Mr. Henri, whose mother died, line 106)
Although care partners understood the need for special post-mortem measures, the ways in which they were communicated and the lack of empathy and support during the process accentuated the distress of care partners in an already difficult context.
Take actions for quality care: Provide sufficient, qualified, empathetic caregivers. Care partners recommended that there be sufficient and stable staff comprising a diversity of professionals who are empathetic and well trained. They said a better ratio of nurses to residents is needed to increase the quality of care and to supervise nurses’ aides. Participants also stressed the importance of having regular managers in LTCHs. Their leadership should be humanistic rather than complacent; they should also have a crisis management plan.
The bereaved participants indicated that more empathy and understanding are needed toward them, especially considering the difficult circumstances in which their relative died and the restrictions surrounding post-mortem care and procedures. They mentioned that there should at least be a call from a health professional to support them and bring closure to this stage of their lives. They recommended that funeral procedures be explained appropriately and that respectful rules concerning the deceased’s personal belongings be implemented to attenuate the negative impacts of modified post-mortem care during an epidemic. They also expressed the wish for acknowledgement, monetary compensation, and apologies from LTCHs about the difficult conditions in which many deaths occurred, as well as commemorations to remember those who died during this crisis.
Theme 3. Communication practices
Many inequalities were reported regarding communication practices. Some LTCHs displayed inertia to adapt communication with care partners during the first wave of the pandemic, whereas others communicated creatively, despite restrictions.
Is the older person able or not able to communicate in this context? Participants described that some older people could communicate by phone, which was reassuring. Some care partners were pleasantly surprised by the capacity of the older person to communicate by videoconferencing (e.g., Zoom, Skype), despite cognitive impairment:
I was surprised how attentive my mother was to the screen, I was very very surprised. I thought that she would not be attentive, that it would be too difficult for her. On the contrary, she was very attentive. It is sure that after 15, 20 minutes her attention decreased, but the first minutes, the attention is there, she listened to us, then she expressed herself, I found that really good and everyone in the family who experienced it found it very very good, she was able to see her friends again with that. (Mr. François, his mother’s care partner, line 167)
Others found the older person’s abilities and/or medical condition (e.g., inability to speak or cognitive impairment) made communication via videoconferencing or phone difficult.
Does the LTCH facilitate communication with us or not? Communications between participants with the older person and staff varied. This inequality was related to the setting itself and to the passage of time. During the strict lockdown, some participants had no possibility of communicating with the older person whatsoever. For some, this lasted several weeks. Even when there was communication between staff and care partners about the situation in the LTCH or about the older person, the frequency was often inadequate. In some settings, a phone number was set up to allow partners to get news. However, some participants reported that no one answered when they called. Others were admonished by staff for trying to get updates:
As soon as we were forbidden [to visit], we didn’t know what was going on, we called, and they didn’t answer us. Once or twice, ah yes, it’s fine, it’s fine [they said], but not more than that [silence], I didn’t even know who had called. I would call, my sister would call, my brother would call, everyone would call, but we didn’t have [news of my mother]. (Mr. Salvador, whose mother died, line 78)
Participants wanted information about the older person’s health status. Some did not have the opportunity to discuss the older person’s level of care, and medical decisions were made without their input. Videoconferencing was not offered at all or offered late to some care partners. Sometimes, the timing or duration of the meetings was inadequate and prevented optimal communication with the older person.
In some LTCHs, communication was satisfactory because care partners received news about the older person from the beginning of the pandemic and videoconferencing was offered. Videoconferencing was considered very helpful, especially when it was frequent. Some also received emails and photos of the older person sent by staff; this was reassuring to them. Finally, one LTCH was creative. It involved able residents in the communication process by answering calls from care partners. They got personalized information about the older person from nurses then reported it to care partners. This was appreciated:
Then, on two occasions, it was their job [the cognitively competent residents]. They had the mandate to receive and answer the phone. I thought that was so cute! And they did it well. At that time, it was easier to reach them, the nurses, like that (laughs). Because the one who was ‘on call’ that day taking calls, she was efficient. So there, they let them look for the nurse of Mrs. so-and-so, she [tells the nurse]: ‘She’s calling to know what’s happening with Mrs. so-and-so.’ So that’s how it was, it was pleasant, easier for the nurses. (Ms. Clemence, whose mother died, line 29)
Take actions to communicate with us proactively. Care partners wanted to be informed and reassured proactively. They believed this kind of support is a right. They recommended that designated staff who know the older person well should be the ones to provide information to care partners. Some suggested giving care partners access to a virtual file on the older person so they could track their health and activities.
They recommended the use of videoconferencing at least weekly during a crisis, but also in normal times for partners who wish to communicate in that way. They suggested hiring people responsible for this type of communication and encouraging staff to share videos/photos of the older person at the request of care partners. They also wished to be regularly informed (e.g., weekly e-mail, newsletters) about the status of outbreaks and visiting conditions during the pandemic and afterward.
Theme 4. Visitation practices
The application of the visitation rules laid out by the government varied from one LTCH to the next and sometimes even within the same one, especially after the rules were relaxed. Some care partners had little constraints to visit, and others had a lot even when visits were officially allowed.
A long ban on visits in an anxiety-inducing context generated great distress in us. The long ban on visits was particularly anxiety-provoking for care partners. They worried that their absence would result in their older person not receiving the care they required. Although compassionate visits were officially allowed for people at the end-of-life, some partners were denied this right which increased their sense of helplessness.
After the strict lockdown, public health directives allowed care partners to visit if they provided significant support (physical and/or emotional) to their older person. However, some LTCHs interpreted this directive narrowly and only allowed access to care partners who supported their older person with physical care before the pandemic (e.g., feeding, hygiene care). This instrumentalization of their role frustrated care partners since it did not necessarily match their conception of their role.
Our visits to LTCH: So important to maintain our connection with the older person but managed in an unequal way. Participants emphasized how important visiting was to maintain their connection with and ensure the quality care of the older person. Visiting practices evolved over time but differed between, and sometimes within the same LTCHs. In some LTCHs, visits were poorly organized and inflexible. Sometimes, infection prevention and control (IPAC) measures were not explained. For others, the organization of visiting schedules and IPAC explanations were helpful, demonstrating that it was possible to adopt better practices:
Yeah, I’ve been visiting regularly for the last two weeks, three times a week, with the mask, the goggles, the gown. Everything is well, everything is A-1 as a precaution. […] We had an information course, for an hour and a half [on preventive measures]. (Ms. Julienne, the care partner of her friend, lines 33-35)
With adjustments to public health directives, visits were gradually organized according to a predetermined schedule. These schedules were often restrictive and ignored the availability of care partners. Some were allowed to visit, but only outside. Some were allowed to visit only when there was no case of COVID-19, even if the official directives allowed visits, despite an outbreak. Some were only permitted to visit under the supervision of a staff member; this restricted intimacy with the older person. Some care partners reported that they had not been given the same opportunities to visit as others, without knowing why:
It’s because we got an email saying that people have been going in [the long-term care home] for two weeks now. I called [the receptionist] and I asked her if I could be part of those people. She told me flat out no. I said why? She told me because you accepted the visits [with your mother] outside [previously]. I said OK and now I can’t go see my mom inside? She says, it’s until August 16. From August 16, we’ll see where we are, it will depend on the pandemic, what happens and all that. (Ms. Lucille, her mother’s care partner, lines 147-148)
This unequal management of visits generated feelings of injustice.
Most residents in LTCHs were happy to see their care partner when visitations were allowed. A few reacted negatively, either because they had felt abandoned or because of the personal protective equipment:
We came in, but she would not see us, she kicked us out. She did not want to see us, she did not understand the shield and the mask, and she said, ‘Look if you want to end the communication, you win. There is no way I am talking to you in this getup.’ (Ms. Diane, her aunt’s partner, line 113)
Take actions to give us access to the older person. Without exception, care partners said they must have access to the older person living in an LTCH even during a health crisis since they contribute to ensuring the well-being of these vulnerable people. They recommended being allowed to visit with appropriate IPAC measures. They added that these measures must be respected by anyone who enters the LTCH. They also recommended that LTCHs maintain access to private companions as they contribute greatly to the quality of life of older people, especially when there is a shortage of human resources.
Theme 5. Community
Care partners considered LTCHs as neglected communities within the society. This neglect, they felt, led to the crisis during the pandemic.
Older people deserve better, and this is shocking. Participants emphasized how appalling they found the situation in LTCHs, including the lack of crisis preparedness and the high rates of infection and death that resulted from it. Some called the situation a catastrophe, arguing that older people deserved better given their contribution to society. The discrepancies between the government’s directives and their experience led to contradictions that undermined the credibility of public health messages:
The government would say a thing and here [in the long-term care home] they would ignore it, it wasn’t true, it wasn’t implemented. (Ms. Eugenie, her mother’s care partner, line 185)
This situation led partners to believe the government did not understand the reality in LTCHs.
We also support other older people. The participants also reported that their role as a care partner went beyond supporting their specific older person in the LTCH. Some were involved in the care of other older people who lived in the LTCH, contributing to a community life that was beneficial to all. They also had relationships with other care partners and caregivers:
I remember that there were residents who would tell me, ha when you come [to visit your mother], you are my visit. I also supported them; I gave them little gifts because I knew that they did not have visits. I would take them [for a stroll], I would have two wheelchairs in the elevator to take them down [at the same time as my mother]. (Ms. Clemence, whose mother died, line 75)
The pandemic interrupted this mutual support and generated concerns for other older people, especially for those who had no visitors before the pandemic. For care partners whose older person had died, the permanent loss of those relationships added to their grief.
Take actions to understand the reality of LTCHs. Care partners said they must have a voice, perhaps via spokespersons, to inform the government of what is happening in LTCHs. They also recommended regular unannounced inspections. They suggested various means to support care partners who want to temporarily bring the older person home during a crisis: with home support and financial assistance, for example. Some also wanted to care for other residents besides their older person. Some care partners whose older person died during the pandemic expressed a desire to return to the LTCH to help them mourn.
Care partners wanted the role of volunteers and companions to be better recognized. They believed there should be more of such people to provide a richer environment and reduce the isolation of older people. They suggested various strategies to recruit them (e.g., open houses, intergenerational activities). All supportive actions recommended directly by partners are summarized in Table 3.
Table 3. Summary of supportive actions recommended by care partners
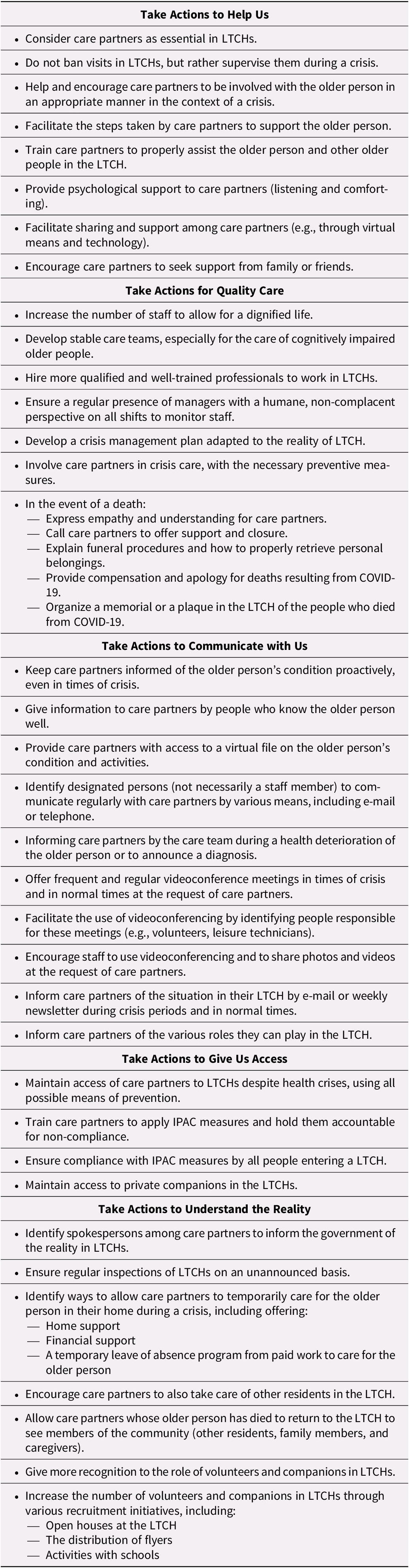
IPAC, infection prevention and control; LTCH, long-term care home.
Discussion and Implications
Our results revealed the importance of care partners in LTCHs, even when there is a major public health crisis and many cases of infections and deaths as this was the case in Québec. They contribute to the well-being of their own older person. They also support the community of the LTCH, that is, other older people, their care partners, and staff. Our results also revealed the significant distress that resulted from the ban on visits and from the high rate of COVID-19 cases and deaths in the context of LTCHs in Québec which were already facing many challenges before the pandemic and created a “perfect storm” (Protecteur du citoyen, 2021). This distress was exacerbated by poor communication, misguided visitation practices, and by the questionable quality of care offered in many LTCHs during as well as before the pandemic (Protecteur du citoyen, 2021). This also includes the impact of older adults dying sometimes alone and of dehumanizing post-mortem care that deeply affected care partners whose relatives died in an LTCH during the first wave of COVID-19. This situation was influenced by the public health department’s initially unclear guidelines about post-mortem measures that generated confusion (Massoud, Reference Massoud2020). These various aspects led care partners to believe that society has neglected the people who live, support, and work in LTCHs. Besides the description of their experience, which is complementary to other studies (Dupuis-Blanchard et al., Reference Dupuis-Blanchard, Maillet, Thériault, LeBlanc and Bigonnesse2021; Giebel, de Boer, et al., Reference Giebel, de Boer, Gabbay, Marlow, Stoop and Gerritsen2022; Giebel, Hanna, et al., Reference Giebel, Hanna, Cannon, Shenton, Mason and Tetlow2022; O’Caoimh et al., Reference O’Caoimh, O’Donovan, Monahan, Dalton O’Connor, Buckley and Kilty2020), we offer a better understanding of the experience of care partners who suffered the death of an older adult living in LTCH or feared, with reasons, for their relatives considering the high rate of cases and death in Québec. Our study also adds to the scientific literature by describing recommendations of care partners for supportive actions (see Table 3). Some are global; others are specific. They reflect what family care partners wanted to voice to policy makers, health care managers, and clinicians. Although those actions apply to the pandemic context, several suggestions of care partners are relevant regardless of the context. Our results also provide some nuances by showing that it is possible to offer quality care, despite a severe crisis like the COVID-19 pandemic was in Québec, as some family care partners trusted the staff in LTCH, which led to less distress. In the same difficult context, some LTCHs were capable of innovation to support care partners and older people.
Because of the nature of our results and the urgency to act, in addition to this scientific publication, we conducted various knowledge transfer activities in 2020–2021. Some were carried out as early as during data collection to alert the government of the significant negative impact of their measures on the well-being of both care partners and older people. Short briefs were also produced for various local health care advocacy and health system evaluation organizations to ensure a large diffusion toward health managers and the government.
The essential role of care partners highlighted in our findings has been discussed in some studies, where they are known as a “second invisible patient” given the consequences their role can have on their own health (Jeste, Mausbach, & Lee, Reference Jeste, Mausbach and Lee2021). Our results show these aspects were not recognized during the first wave of the COVID-19 pandemic in Québec (Canada), as it is also the case in many other provinces or countries where visits were also broadly restricted (Chu et al., Reference Chu, Wang, Fukui, Staudacher, Wachholz and Wu2021; Dupuis-Blanchard et al., Reference Dupuis-Blanchard, Maillet, Thériault, LeBlanc and Bigonnesse2021; Verbeek et al., Reference Verbeek, Gerritsen, Backhaus, de Boer, Koopmans and Hamers2020). By labelling them as “visitors,” the restrictive measures failed to recognize the critical role care partners play in the well-being of LTCH residents. It also resulted in many care partners experiencing great distress, often for weeks or months. Those whose older person died were particularly impacted.
The relationship-centred care approach for older people in which the well-being of older people, care partners, and formal caregivers are recognized as interconnected and interdependent would have averted much suffering (Kemp, Reference Kemp2021; Nolan, Brown, Davies, Nolan, & Keady, Reference Nolan, Brown, Davies, Nolan and Keady2006). Adopting this approach would imply that care partners are not considered visitors and are understood as essential to the well-being of older people and of formal caregivers, and vice versa. In a context of scarce resources and increased stressed and uncertainty, this partnership can make a positive difference in the life of all involved. As there were well-documented problems even before the pandemic, including regarding family care partners (Commission de la santé et des services sociaux, 2016), this approach would be beneficial to follow many recommendations that have been and are made to improve quality of care.
Also, an asymmetry always exists in the power relations in LTCHs between the staff and the care partner–older person dyad; the pandemic accentuated this asymmetry and increased the dyad vulnerability, especially considering the gravity of the situation in Québec where the high rate of infection and death in LTCHs were described daily in the media. Based on symbolic interactionism and critical ethnography (Blumer, Reference Blumer1969), this situation is understood as influencing the meanings given by care partners to their experience and their recommendations. Our results underline that it is important to avoid measures that throw the power dynamic further out of balance (Hartigan, Kellher, McCarthy, & Cornally, Reference Hartigan, Kellher, McCarthy and Cornally2021). During the pandemic, care partners of an older person who died were individually, doubly penalized by restrictions; they experienced the adverse effects of the lockdown measures, but without benefiting from their expected preventive impacts, as it did not protect their older adult from the infection or from dying from it or a related cause (Hartigan et al., Reference Hartigan, Kellher, McCarthy and Cornally2021).
In a rapid review of the literature published in 2020 on long-term care policy and measures during the pandemic, Byrd, Salcher-Konrad, Smith, and Comas-Herrera (Reference Byrd, Salcher-Konrad, Smith and Comas-Herrera2021) found that most studies involved preventing or controlling COVID-19, and they reported that LTCHs with higher quality of care and adequate human resources had fewer COVID-19 cases and fewer deaths. Given that Québec had significant staffing and quality of care issues prior to the pandemic, this corroborates many reports that have been produced to explain the magnitude of the crisis during the COVID-19 pandemic (Collège des médecins du Québec – Ordre des infirmières et infirmiers du Québec – Ordre des infirmières et infirmiers auxiliaires du Québec, 2021; Commissaire à la santé et au bien-être, 2022a; Dubois, Reference Dubois2020; Protecteur du citoyen, 2020, 2021). Although this review (Byrd et al., Reference Byrd, Salcher-Konrad, Smith and Comas-Herrera2021) did not identify publications addressing the perspective of care partners, it does validate the fears of our participants about the effect of understaffing and suboptimal quality of care before the pandemic.
Our findings also highlight a novel and troubling aspect rarely mentioned in the literature, that is, the importance of caring post-mortem procedures, especially in a time of crisis. Our participants received little support after the death of their relatives and, in addition, some interpretation of public health measures contributed to increasing their distress. Post-mortem procedures should be planned based on a scientific basis and clear guidelines, which was not the case during the first wave, despite progressive knowledge about the transmission mechanisms of the virus (Massoud, Reference Massoud2020). Considering the complicated grief many care partners experienced because of the context of death, an empathetic approach is especially important in applying those procedures to increase the quality of care, decrease distress, and prevent prolonged grief disorder in care partners as well as disenfranchisement of their mourning (Kokou-Kpolou, Fernandez-Alcantara, & Cenat, Reference Kokou-Kpolou, Fernandez-Alcantara and Cenat2020).
Some of our participants noted that videoconferencing had been an effective means of communication. This ability to provide good support to the person, even at the end of life, using technology, was corroborated by another study (Feder et al., Reference Feder, Smith, Griffin, Shreve, Kinder and Kutney-Lee2021) and guidelines (Canadian Academy of Geriatric Psychiatry, 2021). Videoconferencing should be used at a frequency and for a duration that correspond to the wishes of care partners and older people while respecting their privacy.
Participants said care partners need to be allowed to visit the older person even during a public health crisis, if adequate means to protect older people and themselves are in place. Some authors (Bergman et al., Reference Bergman, Stall, Haimowitz, Aronson, Lynn and Steinberg2020) recommend identifying a primary partner and ensuring that these visits aim at promoting the well-being of the residents. However, this suggestion raises issues about who is responsible for judging whether visits promote well-being. If this judgment falls solely to the staff, it could exacerbate the asymmetry in power relations with care partners. The perspective of the care partners and of the older person must be considered. Our participants reported inconsistencies in duration and arrangements, even when visits were allowed. Considering this finding, studies should explore the factors contributing to this inequity based on frameworks that consider public policy, but also implementation science.
Our participants considered the LTCH as a community and the pandemic had additional impacts on care partners actively involved in this community. According to a systematic review (Backhaus et al., Reference Backhaus, Hoek, de Vries, van Haastregt, Hamers and Verbeek2020), little has been written about this communal characteristic even in normal times. One study (Baumbusch & Phinney, Reference Baumbusch and Phinney2014) describes that some care partners complement and improve the quality of care offered by staff. This contribution was lost during the first wave of the pandemic. LTCHs would benefit from supporting the active involvement of care partners in this community life for the well-being of all concerned.
Our study has some limitations. As with any qualitative studies, the results cannot be generalized to the experience of all care partners or all LTCHs. Our sample was recruited from LTCHs in an urban region with a high rate of death by COVID-19 that might not reflect the experience in rural regions or in countries with a different health care system. Also, the data obtained from partners could not be triangulated with those of managers, staff, or older people because of feasibility and ethical issues in the context of the first wave of the pandemic.
Conclusion
In many countries, as in Québec, the problems in LTCHs have been known for many years and the exacerbation of these problems during the pandemic is troubling. Most underestimated the impact of the ban on visitations on care partners and older people. Compassionate and supportive care for vulnerable people and their care partners should not be the exception but the rule in all LTCHs. The recommendations outlined directly by our participants are intended to serve as a catalyst for change toward better care for older people and their care partners, as well as for the community that is each LTCH. The catastrophe such as the one that occurred during the first wave of the COVID-19 in LTCHs must never happen again. The voice of family care partners must be heard and lead to radical changes in the design of care in long-term care homes.
Acknowledgements
We wish to thank the care partners who generously shared their experiences during a most difficult time. We also thank the president of the institutional ethics review board who approved this work and wholeheartedly supported our effort to let the voice of care partners be heard. Our thoughts are with older people, care partners, and health professionals who lived and died during the COVID-19 pandemic.
Funding
This work was supported by funding from the Research Centre of the Institut de gériatrie de Montréal, the Canada Research Chairs Program (to AB), and the Research Chair in Nursing Care for Older People and their Families (to AB). The funding agencies did not play any role in the design, execution, analysis, and interpretation of data, or writing of the study.






