Introduction
Haiti has long been considered one of the world’s most impoverished nations, ranking 163 out of 188 countries on the United Nations (UN) Human Development Index, 1 and having one of the poorest economies in the Western hemisphere. According to the United Nations International Children’s Emergency Fund (UNICEF; New York USA) State of the World’s Children 2015 Report, Haiti’s under-five mortality was 73/1,000 live births (ranking 32 from the bottom) and its infant and neonatal mortality rates were high at 55 and 25 per 1,000 live births, respectively. 2 Many children in Haiti have difficulty accessing food, clean water, adequate housing, and medical care, and they face high rates of violence, sexual abuse, and exploitation.Reference Udy 3 Free and accessible public education for children is limited, decreasing enrolment rates for those who cannot afford private education.Reference Beau De Rochars, Alam and Telisma 4
On January 12, 2010, a 7.0 magnitude earthquake struck Haiti. The resulting destruction was massive and widespread, including an estimated 316,000 deaths, 300,000 people injured, 1.3 million people displaced, 97,294 houses destroyed, and 188,383 houses damaged in the capital and in the southern region of the country. 5 It is estimated that the earthquake affected over 1.5 million people and that children and youth represented more than one-half of those impacted by the disaster.Reference Ager, Blake, Stark and Daniel 6 The 2010 earthquake made it more challenging for children in Haiti to access the basic necessities of life and exacerbated pre-disaster concerns about child protection and violation of human rights, including trafficking, restavèks (child slaves), sexual violence, and exploitation.Reference Ager, Blake, Stark and Daniel 6 In addition, recovery from the earthquake was complicated by a widespread cholera epidemic that resulted in many additional lives lost.
Given heightened concern about child health and the welfare of children following the earthquake and the cholera epidemic, this systematic review summarizes published peer-reviewed research conducted since the earthquake that focuses on physical health, psychological health, or socioeconomic outcomes for Haitian children. The goal was to provide a comprehensive summary of the recent and post-earthquake child health research to be useful for identifying potential research gaps as well as informing programming and services for children and the allocation of resources.
Methods
Search Strategy
The purpose of this literature review was to summarize and report on research focused on health outcomes for children in post-earthquake Haiti (regardless of whether the health outcome was a direct result of the earthquake or independent of the earthquake). To identify research publications on health outcomes among children in post-earthquake Haiti, PubMed (National Center for Biotechnology Information, National Institutes of Health; Bethesda, Maryland USA); Embase (Elsevier; Amsterdam, Netherlands); PsychINFO (American Psychological Association; Washington DC, USA); LILACS (Latin American and Caribbean Center on Health Sciences Information Knowledge Management, Bioethics, and Research Area; Rua Vergueiro, São Paulo, Brazil); Web of Science (Thomson Reuters; New York, New York USA); and Sociological Abstracts (ProQuest; Ann Arbor, Michigan USA) were searched from January 10, 2010 through May 2016 using the terms “Haiti” in combination with “Child,” “Adolescent,” “Infant,” “Pediatric,” “Toddler,” “Baby,” “Boy,” “Girl,” or “Youth.” The full PubMed search strategy is provided in Table 1, and equivalent searches were conducted in the other peer-review databases. A grey literature search was also conducted using the Grey Literature Report (New York Academy of Medicine; New York, New York USA) and Open Grey (Institut de l’Information Scientifique et Technique; Vandoeuvre-lès-Nancy, Cedex, France), plus a number of pre-selected academic think tanks or centers, as well as the websites of pre-selected nongovernmental organizations, UN, and government agency websites. A complete list of grey literature sources is provided in Table 2. Because a broad definition of health and health determinants underpinned this review, any research reporting child physical health, psychological health, or socioeconomic outcomes were included. Children were defined as persons less than 18 years of age. Articles that focused on the following were excluded: (1) non-health outcomes; (2) adults 18 years of age or older; (3) Haitian refugees or migrants living outside of Haiti; (4) data collected prior to the January 2010 earthquake; or (5) humanitarian response or systems evaluation. Articles that were published in abstract format only, were written in languages other than English or French, or for which full-length articles could not be accessed were also excluded.
Table 1 PubMed Search Strategy

Table 2 Grey Literature Sources
Abbreviations: GIZ/GTZ, Deutsche Gesellschaft für Internationale Zusammenarbeit; JHPIEGO, Johns Hopkins Program for International Education in Gynecology and Obstetrics; MSF, Médecins Sans Frontières; NGO, nongovernmental organization; UN, United Nations; UNICEF, United Nations Children’s Fund.
Results
A total of 647 articles were identified, each of which was independently screened by two reviewers (AD and MM) who had been previously trained in the screening process. Articles that described peer-reviewed research with at least one physical health, psychological health, or socioeconomic outcome among individuals aged 18 years or under in Haiti since the earthquake in January 2010 were included. A total of 58 articles were retained by consensus between the two reviewers. Screening discrepancies and uncertainties were resolved through a panel discussion with a third reviewer (SB). Each of these 58 articles was then reviewed in detail by one of two investigators (AD or MM) who extracted data for inclusion in the review. Full details of the screening results, as well as the types of health outcomes described, are illustrated in Figure 1.
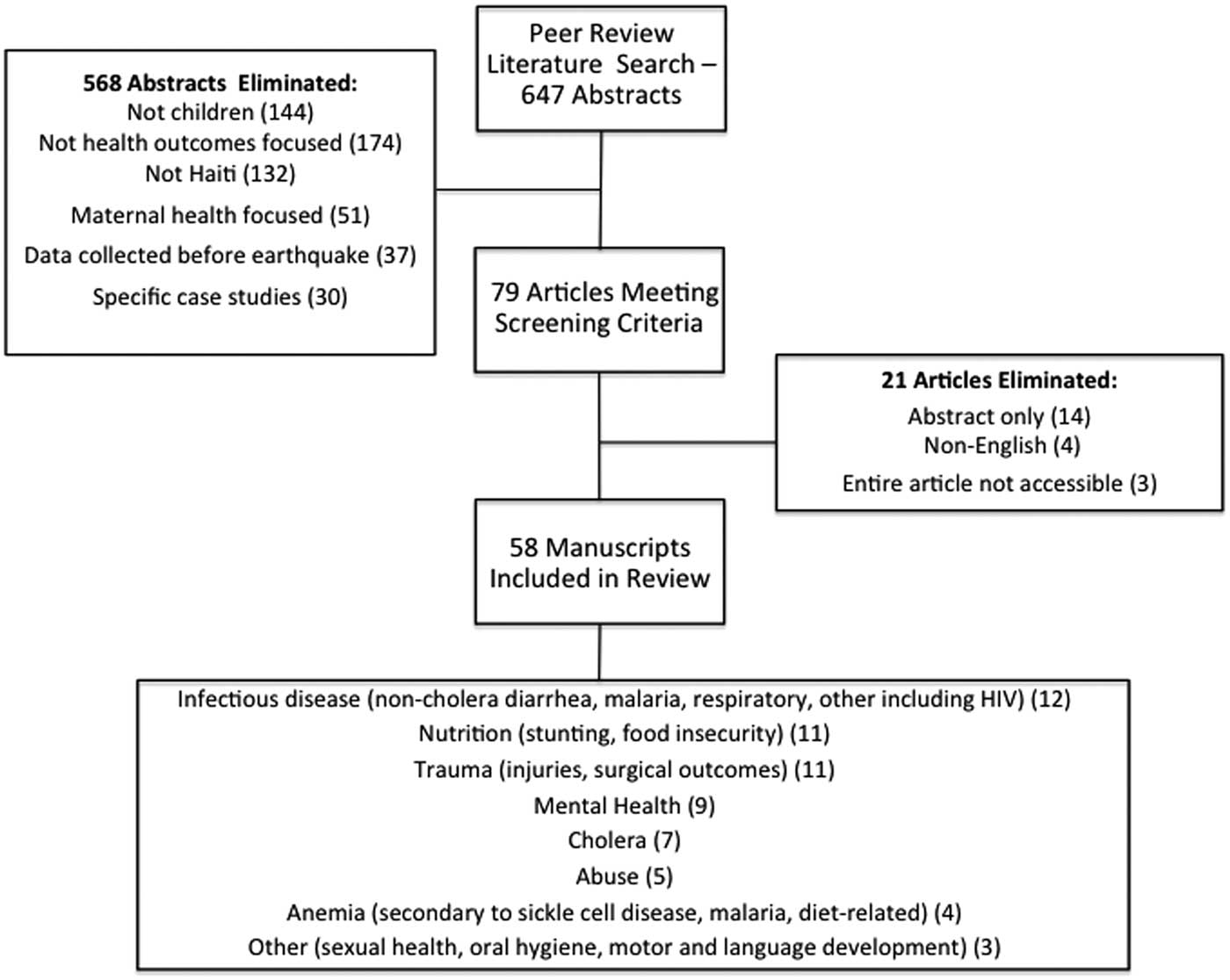
Figure 1 Screening Results and the Types of Health Outcomes Described.
Included articles were classified by topic into one of eight themes, including: infectious diseases (non-cholera [N=12] and cholera [N=7]), nutrition (N=11), traumatic injuries (N=11), mental health (N=9), anemia (N=4), abuse and violence (N=5), or other topics (N=3). Some articles focused on more than one topic, and the categories were not mutually exclusive. While some articles (N=19) focused on direct earthquake-related outcomes, other articles (N=43) were broader and reported health outcomes more generally since the January 2010 earthquake. A majority of articles were cross-sectional in design (N=39), while 12 used a cohort design following participants over time. Four studies were case-control studies, and three studies were randomized controlled trials. Overall, the age range of children included in articles was three to 17 years.
Infectious Diseases
Infectious diseases (cholera in seven studies and non-cholera in 12 studies) were among the most commonly reported child health illnesses in Haiti since the 2010 earthquake (Table 3)Reference Beau De Rochars, Alam and Telisma 4 , Reference Farfel, Assa and Amir 7 – 23 and caused significant morbidity and mortality, as reflected in this review of the literature. Both cholera and non-cholera diarrheal illnesses were common, in addition to a variety of respiratory infections, malaria, and wound/skin infections. After the earthquake, cholera was thought to have been re-introduced in Haiti after the country had been cholera-free for almost a century. 23 With no pre-existing immunity to cholera, significant morbidity and mortality resulted, particularly in the Artibonite district, and children were among those most affected. Table 3 provides further details of reported infectious disease outcomes.
Table 3 Summary of Studies on Infectious Diseases Outcomes Among Children in Haiti
Abbreviations: MSF, Médecins Sans Frontières; HUP, Hôpital Universitaire La Paix located in Port-au-Prince; , Hôpital Foyer Saint Camille located in Port-au-Prince; HSN, Hôpital Saint Nicolas (HSN) de Saint Marc located in Artibonite Department; SMJ, Hôpital Saint Michel de Jacmel located in Southeast Department; HUEH, Hôpital de l’Université de l’Etat d’Haiti located in Port-au-Prince; HSD, Hôpital Saint Damien located in Port-au-Prince; GHESKIO, The Haitian Group for the Study of Kaposi’s Sarcoma and Opportunistic Infections; CTC, Cholera Treatment Center; ORP, Oral Rehydration Point; URTIs, upper respiratory tract infections; LTRIs, lower respiratory tract infections; RTIs, respiratory tract infections; MRSA, methicillin-resistant Staph. Aureus; ESBL, extended-spectrum betalactamase.
Nutrition and Food Security
Eleven studies focused on nutritional status and food security among Haitian children. A 2012 household survey studying children aged 0 to 59 months reported that 4.3% of children had wasting, 22.2% of children had stunting, and 10.5% of children were underweight.Reference Ayoya, Heidkamp, Ngnie-Teta, Pierre and Stoltzfus 24 Despite the earthquake, this represented a decline in each of the categories when compared to the 2005-2006 Haiti Demographic and Health Survey (DHS), and the rural-urban gap had also narrowed in all categories.Reference Ayoya, Heidkamp, Ngnie-Teta, Pierre and Stoltzfus 24 However, a follow-up survey in 2013 showed no significant further improvements in wasting, stunting, and underweight children.Reference Ayoya, Heidkamp and Ngnie-Teta 25 Data from the DHS and the Multiple Indicator Surveys were also used to determine the prevalence of child stunting and differential access to food between restavèk and non-restavèk children in Haiti. Among 13,907 Haitian children aged five to 14, non-restavèk children had higher rates of insufficient access to food (68.5%) in comparison to restavèk children (53.1%).Reference Haydocy, Yotebieng and Norris 26 In additional analysis of 2015 DHS data, the national stunting prevalence in children under five years of age was 31.0% among the poorest families, 21.0% among average income families, and 8.0% among the richest families.Reference Restrepo-Méndez, Barros and Requejo 27 Overall, the population prevalence of stunting was found to have decreased since 2000.Reference Restrepo-Méndez, Barros and Requejo 27
The post-earthquake literature also included nutritional data from hospitals and medical centers. A 2012 review of medical records for children aged six to 11 months at Fort Saint Michel Health Centre in the Nord Department of Haiti determined that 30.2% of the 583 children had mildly to moderately stunted growth.Reference Iannotti, Dulience, Wolff, Cox, Lesorogol and Kohl 28 Between April and June 2010, records from baby tents established in heavily earthquake-impacted areas revealed that 65.7% of infants less than 12 months of age who were unable to breastfeed were considered underweight, 14.8% were considered moderately underweight, and 19.5% were considered severely underweight.Reference Talley and Boyd 29 Among children under the age of five in the Milot Valley, 41.7% had mild or moderate stunting, 4.4% had severe stunting, 37.3% had mild or moderate wasting, 3.8% had severe wasting, 46.0% were mildly and moderately underweight, and 4.3% were severely underweight.Reference Rollet, Gray, Previl and Forrester 30 Among children between five and 14 years of age in Milot Valley, 45.9% had mild or moderate stunting, 2.9% had severe stunting, 38.2% had mild or moderate wasting, 3.5% had severe wasting, 48.7% were mildly or moderately underweight, and 1.7% were severely underweight.Reference Rollet, Gray, Previl and Forrester 30
There were several studies on nutritional supplementation among Haitian children. In a randomized controlled trial among three to 13-year-olds in Cap Haitien, a fortified ready-to-use supplement increased the body mass index z score and percentage fat mass compared with control at each time point (P<.001).Reference Iannotti, Henretty and Delnatus 31 In 2013, 1,167 children aged three to 13 years in northern Haiti were randomized to receive either an unfortified cereal bar (Tablet Yo), a fortified ready-to-use supplement (Mamba), or a control group without supplementation.Reference Iannotti, Henretty and Delnatus 31 In longitudinal modeling, Mamba supplementation increased body mass index z score, while both Mamba and Tablet Yo increased mean fat mass.Reference Iannotti, Henretty and Delnatus 31 The authors concluded that fortified, ready-to-use supplementary food decreased the odds of wasting by 55.0% when compared to supplementation with an unfortified cereal bar or a control group.Reference Iannotti, Henretty and Delnatus 31 And finally, a study conducted in an urban slum area followed mother-child pairs with singleton births less than one year old dividing them into three groups: 191 control pairs, 196 pairs with a three-month old child, and 202 pairs with a six-month old child.Reference Iannotti, Jean-Louis, Lesorogol, Green and Nickerson 32 The latter two groups received a daily sachet of a lipid-based nutrient supplement (LNS) and attended a clinic at the start of each month; LNS supplementation for six months significantly increased the length-for-age z score and the effects were sustained at six months. However, morbidity and developmental outcomes did not differ by trial arm.Reference Iannotti, Jean-Louis, Lesorogol, Green and Nickerson 32
Two additional studies reported on food security among Haitian children. In the months after the earthquake, 17.2% of Port-au-Prince households reported that their child had gone hungry in the previous month, 22.5% stated that their child had skipped a meal in the past month, and 22.6% reported that they had reduced the size of their children’s meals in the previous month.Reference Hutson, Trzcinski and Kolbe 33 School attendance and household amenities prior to the earthquake were found to have a negative correlation to going hungry while age, gender, and health had no association with going hungry.Reference Hutson, Trzcinski and Kolbe 33 Household damage, sense of security, levels of posttraumatic stress disorder (PTSD), and size of household were found to be positively correlated with skipped meals and meal size reductions after the earthquake.Reference Hutson, Trzcinski and Kolbe 33 Rural-to-urban migration among seventh grade students after the earthquake was associated with increased food security due to a wider diversity of available foods and increased peer social interactions.Reference Heckert, Boatemaa and Altman 34
Trauma, Injuries, and Care
In the immediate relief effort following the 2010 earthquake, many aid organizations and medical groups treated children with earthquake-related injuries, and these were subsequently reported in the literature (11 studies). A Swiss Confederation medical team working at a field hospital, for example, managed 471 pediatric patients with traumatic injuries, including 42.0% with crush injuries to their extremities, 22.0% with axial injuries, 6.8% with other musculoskeletal injuries, 3.4% with open head injuries, and 2.7% with each of compartment syndrome and a non-musculoskeletal surgical injury.Reference Gamulin, Armenter-Duran, Assal, Hagon and Dayer 35 In a hospital run by Project Medishare in Port-au-Prince from January through June 2010, seven children died (41.2% of all earthquake-related deaths at that hospital) and 159 survived (29.8% of all surviving patients).Reference Dulski, Basavaraju and Hotz 36 The US Naval Ship Comfort also contributed to the management of pediatric earthquake injuries by providing surgical treatment to 237 children, with many of those (167 out of 237) having extremity injuries (134 fractures, 29 soft tissue injuries, and four vascular injuries).Reference Walk, Donahue, Sharpe and Safford 37 Furthermore, 4.2% of patients had burns, 8.8% had head and neck injuries, 0.8% had pelvic injuries, 1.7% had spinal injuries, and 10 children required an amputation.Reference Walk, Donahue, Sharpe and Safford 37 Aboard the US Naval Ship Comfort, 409 pediatric patients were treated in January 2010 with 47.0% of those patients requiring admission for their traumatic injuries, including 29 open fractures, 64 lower limb fractures, 17 upper limb fractures, and eight axial skeleton fractures.Reference Bar-On, Lebel, Blumberg, Sagi and Kreiss 38 At the Fort de France University Hospital in Martinique, 23 of 53 pediatric patients evacuated from Haiti after the earthquake were admitted for surgical care of earthquake-related injuries in January and February 2010, eight with open fractures, 10 with tissue damage, three with open depressed skull fractures, one with peritonitis, and one with gaseous gangrene.Reference Arquès, Vincent, Olive, Cabié, Canivet and Hochedez 39 At the Israeli field hospital in Port-au-Prince, 57.0% of the 272 pediatric patients treated in the 10 days immediately following the earthquake had injuries directly resulting from the earthquake.Reference Farfel, Assa and Amir 7 These injuries included 48 (15.0%) open fractures, 52 (16.4%) open wounds, 29 (9.2%) crush injuries, 29 (9.2%) superficial injuries, eight (2.6%) contusions, five (1.6%) dislocations, five (1.6%) head injuries, and six (1.8%) other or unspecified injuries.Reference Farfel, Assa and Amir 7
Pediatric injuries treated at six hospitals in the Central and Artibonite districts of Haiti in the six months prior to the earthquake included 14 traumas/burns, nine fractures and dislocations, two amputations, and two burns among the 423 overall pediatric surgeries conducted. This injury pattern was compared by Hughes et al to that in the six months following the earthquake with an increased volume of 670 operative pediatric patients as well as a much higher injury incidence: 259 traumas/burns, 195 fractures and dislocations, 23 amputations, and nine burns.Reference Hughes, Nash and Alkire 40
In a stratified, cluster sample survey one year after the earthquake, Doocy et al reported injury ratios of 40/1,000 and 39/1,000 for children less than nine years of age and children 10 to 19 years old, respectively.Reference Doocy, Jacquet, Cherewick and Kirsch 41 The mortality ratios for children less than nine years of age and children 10 to 19 years old were 20/1,000 exposed and 19.5/1,000 exposed, respectively.Reference Doocy, Cherewick and Kirsch 42
The post-earthquake literature also included a report on critical care provided to pediatric patients in Haiti since 2010. Following the earthquake, Project Medishare admitted nine infants and 20 children to neonatal and pediatric intensive care units, respectively, at a Port-au-Prince field hospital.Reference Doocy, Cherewick and Kirsch 42 Among these patients, there was one burn injury, one traumatic superior mesenteric artery tear, and two traumatic brain injuries.Reference von Saint André-von Arnim, Brogan and Hertzig 43 The only study examining the prevalence of disabilities and access to services among Haitian children was conducted in 2012. In this report, 2.9% of 656 children under five years of age had an identified disability, and these children were less likely to be in school and had more limitations and restrictions on activity than control group children.Reference Danquah, Polack and Brus 44
Anemia
Four peer-reviewed publications reported findings associated with studies of sickle cell and diet-related anemia in Haitian children. The prevalence of the sickle cell genotypes HbSS and HbSC was one in 173 newborns, which was twice that for African Americans living in the US, and thus representing a significant burden of disease.Reference Burke, Burns and Linden 45 In a 2012 study, the prevalence of diet-related anemia was 30.0% overall (1,405 of 4,721 children) but was as high as 51.5% among children six to 11 months of age.Reference Ayoya, Heidkamp and Ngnie-Teta 25 A variety of nutritional supplementation and deworming programs had been implemented to address this high prevalence of anemia.Reference Ayoya, Heidkamp and Ngnie-Teta 25 For instance, a research trial in Cap Haitien randomized three to 13 year old school children to receive fortified snacks versus regular snacks in Cap Haitien and measured hemoglobin concentrations at three points in time using World Health Organization (WHO; Geneva, Switzerland) anemia and severe anemia thresholds.Reference Iannotti, Delnatus and Odom 46 Seventy-one percent of children were anemic and 2.6% were severely anemic. Parent-reported vitamin A supplementation and deworming were positively associated with higher hemoglobin concentrations.Reference Iannotti, Delnatus and Odom 46 Diet supplementation with a fortified ready-to-use supplementary food reduced the odds of developing anemia by 28.0% compared to controls.Reference Iannotti, Delnatus and Odom 46
Mental Health
Nine published studies examined mental health among children in Haiti, including research on the psychological impact of the disaster. A 2011 study in Port-au-Prince examined the levels of traumatic exposure, PTSD symptoms, and social support of 540 children aged two to 18 years who had experienced the earthquake but not received psychological care.Reference Derivois, Mérisier, Cénat and Castelot 47 The investigators reported high rates of PTSD symptoms, particularly among females, and noted higher rates of social support for children attending school in comparison to children who were not in school. Social support was significantly correlated with school attendance, level of traumatic exposure, and PTSD symptoms.Reference Derivois, Mérisier, Cénat and Castelot 47 However, there was no significant correlation between level of traumatic exposure and PTSD symptoms.Reference Derivois, Mérisier, Cénat and Castelot 47 Using a questionnaire self-administered to 658 children aged 10 to 17 years of age, Derivois et al reported that among children 10 to 13 years of age, 9.9% had low PTSD symptoms, 55.3% had average PTSD symptoms, and 34.9% had high PTSD symptoms.Reference Derivois, Cenat and Merisier 48 For children between the ages of 14 and 17 years, 5.3% had low PTSD symptoms, 55.5% had average PTSD symptoms, and 39.1% had high PTSD symptoms.Reference Derivois, Cenat and Merisier 48 Other investigators used the PSYCa 3-6 questionnaire to measure psychological disturbance among children and found that all but one of the of 166 participants had directly witnessed and/or were victims of the earthquake.Reference Mouchenik, Marty-Chevreuil and Marquer 49 Using nine as a threshold of disturbance, the average disturbance score for participants was 9.8, with 51.8% of children scoring over nine and 25.0% of children scoring over 12.0.Reference Mouchenik, Marty-Chevreuil and Marquer 49 Males were observed to have higher scores in comparison to females.Reference Mouchenik, Marty-Chevreuil and Marquer 49 The PSYCa 3-6 questionnaire was also used to analyze the relationship between environment and psychological health for children three to six years of age. In this study, males had greater psychological disturbances than females, and the number of siblings, neighborhood violence, and the perception of environmental harm were positively correlated with psychological disturbances.Reference Mouchenik, Dauriac-Le Masson and Marquer 50
Several institution-based studies had also examined mental health among children in Haiti since the earthquake. Cénat et al investigated PTSD symptoms and depression among 872 children at 12 schools and two homeless shelters in zones of Port-au-Prince that were heavily affected by the earthquake.Reference Cenat and Derivois 51 In this 2012 study, 63.7% of children met criteria for significant distress on the peri-traumatic distress inventory, 36.9% of children had PTSD, and 46.2% of children had depression.Reference Cenat and Derivois 51 Another school-based study investigated psychological consequences of the earthquake among nine to 12-year-olds, based on distance from the epicenter (urban versus rural) and studied whether children separated from their biological parents/families displayed more severe symptoms.Reference Dass-brailsford, Thomley and Talisman 52 Children from Port-au-Prince (16 miles from the epicenter) and Mirebalais (50 miles from the epicenter) were enrolled. The study found that all children displayed significant symptoms of depression, anxiety, and trauma, regardless of their location.Reference Dass-brailsford, Thomley and Talisman 52 Children who lived in orphanages scored lower for anxiety and PTSD symptoms than did children living with their biological families, and thus orphanages appeared to have played a protective role in Haitian children’s lives.Reference Dass-brailsford, Thomley and Talisman 52 Other groups of children had also been the focus of research on mental health in Haiti. For instance, using the Child Psychosocial Distress Screener, 104 Pan American and Olympic games athletes aged 12 to 18 years were compared to 104 gender and age matched children from several schools and orphanages.Reference Yim, Macy and Ciottone 53 The authors reported no significant differences in psychosocial scores between the athletes (19.0%) and the control group (21.0%).Reference Yim, Macy and Ciottone 53
Two identified studies evaluated the impact of psychological health interventions on children in Haiti. The first determined the efficacy of an eight-week yoga intervention on reducing trauma-related symptoms as well as emotional and behavioral difficulties (EBD) in children aged seven to 17 years living in orphanages.Reference Culver, Whetten, Boyd and O’Donnell 54 Children in both the yoga group and the aerobic dance group had lower trauma-related symptoms and EBD, although the results were not statistically significant.Reference Culver, Whetten, Boyd and O’Donnell 54 Participants in the yoga program reported that they enjoyed the sessions and that their overall well-being was improved as a result.Reference Culver, Whetten, Boyd and O’Donnell 54 The second study assessed the effect of a psychosocial support program offered to children relocated in Port-au-Prince compared with a control group. Using the Ute Sodeman’s Psychosocial Assessment Questionnaire for Children, 68.0% of children in the psychosocial support program had severe levels of PTSD and 40.9% had severe depression versus 50.0% and 20.5% in control group, respectively.Reference Blanc, Bui, Mouchenik, Derivois and Birmes 55 The authors concluded that these surprising results could be explained by the absence of equivalence between the two groups in terms of demographics and because the subjects were not randomly selected.Reference Blanc, Bui, Mouchenik, Derivois and Birmes 55
Abuse and Violence
Of the 58 studies reviewed, five focused on issues of abuse or violence among Haitian children. In 2012, Flynn-O’Brien et al used the Violence Against Children Survey to document the incidence of physical violence against children in Haiti. In this report, 69.9% of children aged 13 to 17 years reported lifetime experiences of physical violence with most of the violence perpetrated by parents or teachers as a form of punishment or discipline.Reference Flynn-O’Brien, Rivara and Weiss 56 Almost all of the children in this study were punched, kicked, whipped, or beaten, and 11.0% had experienced abuse with a knife or other weapon.Reference Flynn-O’Brien, Rivara and Weiss 56 Restavèk children, children kept as household domestic servants in Haiti, were also surveyed to identify their experiences of physical abuse. Restavèk children aged five to 14 years reported less physical abuse (8.6%) than non-restavèk children (16.6%).Reference Haydocy, Yotebieng and Norris 26 However, restavèk children had significantly lower school attendance and more labor experiences.Reference Haydocy, Yotebieng and Norris 26
Following the earthquake, there was considerable media attention around rising incidents of sexual violence in Haiti. A household study in Port-au-Prince estimated that 5,209 girls and 324 boys from 1,732 households had been sexually assaulted after the earthquake in 2010.Reference Kolbe, Hutson and Shannon 57 Nation-wide surveys in Haiti estimated the lifetime prevalence of sexual violence to be 21.2% in males and 25.7% in females before 18 years of age, but only 6.6% of boys and 10.0% of girls had received formal support services following experiences of sexual violence.Reference Sumner, Mercy and Saul 58 The lifetime prevalence of experiencing unwanted, completed sex before age 18 in Haiti was estimated to be 7.6% for males and 9.0% for females.Reference Sumner, Mercy and Saul 58 Sumner et al also reported specifically on sexual violence among boys in Haiti and found that 23.1% had experienced some form of sexual violence before the age of 18 and 18.0% of 327 participants were 10 years of age or less at the time of the first sexual assault.Reference Sumner, Mercy, Buluma, Mwangi and Marcelin 59 This work generated an estimated prevalence of unwanted sex of 8.8%, which was higher than estimates for Kenya and Cambodia.Reference Sumner, Mercy, Buluma, Mwangi and Marcelin 59
Other
There were three remaining studies included in the review that were single articles on sexual health,Reference Carver, Devieux, Gaston, Altice and Niccolai 60 oral hygiene,Reference Hosokawa, Taura, Ito and Koseki 61 and motor and language development.Reference Iannotti, Dulience, Wolff, Cox, Lesorogol and Kohl 28 Among 200 adolescents, 60.0% were found to have engaged in sexual intercourse. Males were 3.52 times more likely to have had sex, 5.42 times more likely to report sexual debut before the age of 14, 9.75 times more likely to have more than one sexual partner, and 3.33 times more likely to not have used a condom during their last sexual encounter than females.Reference Carver, Devieux, Gaston, Altice and Niccolai 60 Adolescents living with parents or family were less likely to report having engaged in unprotected sex.Reference Carver, Devieux, Gaston, Altice and Niccolai 60
The oral hygiene of 56 children from an urban orphanage and 64 children from a suburban orphanage was evaluated in October 2010.Reference Hosokawa, Taura, Ito and Koseki 61 Children in the suburban orphanage had significantly fewer caries than those in the urban orphanage and there had been an overall increase in the prevalence of dental caries after the earthquake. It was speculated that the observed trends may be related to sweets distributed by medical teams after the disaster.Reference Hosokawa, Taura, Ito and Koseki 61
The final article was from a study investigating the relationship between stunting and the motor/phonetic language acquisition among 583 children aged six to 11 months. In this longitudinal study, stunting was significantly associated with slower motor and phonetic language acquisition, and dietary diversity, consumption of eggs and oil, length-for-age, and stunting were predictive of motor and language acquisition.Reference Iannotti, Dulience, Wolff, Cox, Lesorogol and Kohl 28
Discussion
The objective of this review was to provide a comprehensive summary of recent child health literature in Haiti (using the January 2010 earthquake as a cutoff for the literature search) with the goal of informing health programming and services as well as identifying potential research gaps. In total, 58 unique articles were identified, spanning topics such as infectious disease, nutrition and food security, trauma and injury, mental health, anemia, abuse, and violence. Most of the research was cross-sectional in design (47 of 58 studies) and many of the studies were conducted in the greater Port-au-Prince area. It is also noteworthy that because the literature search was completed prior to Hurricane Matthew in October 2016, it did not capture research concerning the health impact of that disaster, which was a Category 4 storm that affected more than 350,000 people in Haiti and exacerbated the cholera epidemic. 62
Although the authors of this review did not look at the prevalence of studies prior to the earthquake and are not able to comment on a specific change in volume, it is obvious that the earthquake did affect the research landscape with one-third of the included studies (19/58) having focused on direct earthquake-related outcomes. These direct earthquake-related studies highlight the important impact of this large-scale disaster on children, particularly in terms of traumatic injuries and the potential for long-term disabilities. It is noteworthy, however, that only a single identified study examined disabilities among Haitian children. Given the amount of destruction caused by the 2010 earthquake and the anticipated resultant disabilities, this may be an area that warrants further study.
As is common across humanitarian crises, this review highlights that infectious diseases were an important cause of morbidity and mortality in Haiti after the earthquake. As illustrated in Table 3, the most commonly reported infections were diarrheal illnesses, which typically result from lack of access to safe water, poor hygiene, and over-crowded living conditions due to displacement and crowded sheltering. Given its highly infectious nature and the lack of pre-existing immunity, the cholera outbreak that followed the 2010 earthquake had a significant impact on the health of Haitian children with the Center for Disease Control (CDC; Atlanta, Georgia USA) reporting over 82,000 cases of cholera in children under the age of five, representing 90.0% of all cholera cases reported in that study. 23 Cholera was not endemic to Haiti and this represented the first cholera cases in the country in almost 100 years. 23 The disruptions in public health and health care infrastructure, as well the already stretched resources resulting from the earthquake, made it all the more challenging to mount an effective response to the cholera epidemic. While other reported infectious diseases such as malaria may have resulted from earthquake-related loss of housing or loss of preventative measures like mosquito nets, it is not possible to make any such conclusions from this review.
Eleven of the 58 articles focused on malnutrition among Haitian children with high reported prevalence of stunting and wasting.Reference Ayoya, Heidkamp, Ngnie-Teta, Pierre and Stoltzfus 24 – Reference Heckert, Boatemaa and Altman 34 A 2012 study suggested declines in rates of malnutrition after the 2010 earthquake.Reference Ayoya, Heidkamp, Ngnie-Teta, Pierre and Stoltzfus 24 This may be a reflection of food aid and medical care distributed by humanitarian organizations after the disaster, and it is unclear if these positive trends will continue now that the disaster is well into the rebuilding phase and financial resources are being diverted to other emergencies. Another study highlighted food insecurity, but is it difficult to know how the earthquake may have affected this since the focus was exclusively post-earthquake.
The current review included nine published studies focused on mental health in Haiti. Many of these articles reported a very high prevalence of PTSD, peri-traumatic stress, anxiety, and depression among children since the earthquake. Distance from the epicenter of the earthquake did not appear to mediate these symptoms.Reference Cenat and Derivois 51 Li et al reported similarly surprising results after the Wenchuan 2008 earthquake, where individuals who lived in highly disaster-affected areas were less concerned about safety and health in comparison to those who lived further from the epicenter.Reference Li, Rao and Bai 63 Following the Haiti earthquake, higher rates of social support were noted for children attending school, and children who lived in orphanages had lower scores for anxiety and PTSD symptoms than did children living with their biological families. These findings are consistent with a 2011 meta-analysis which showed that school-based support was useful for reducing mental health symptoms among children in humanitarian settings.Reference Tol, Barbui and Galappatti 64 Although higher rates of suicidal ideation were reported after the 1999 Turkey earthquake,Reference Ertem Vehid, Alyanak and Eksi 65 the current review did not identify any studies that examined suicidal ideation among children and adolescents after the 2010 earthquake. It is noteworthy that because of the on-going stressors that many youth in Haiti face on a regular basis (poverty, violence, and food insecurity), it is difficult to definitively link mental health outcomes to the earthquake.Reference Dass-brailsford, Thomley and Talisman 52
Abuse and violence were also identified as areas of concern with over two-thirds of children reporting physical violence, primarily at the hands of teachers and parents. Interestingly, restavèk children reported less physical abuse, although they were more likely to be deprived of an education and were often engaged in child labor. Studies conducted after the earthquake report a high prevalence of sexual violence, including one in five boys and one in four girls with a lifetime experience of sexual abuse. These prevalence estimates for sexual violence are similar to those for the United States as estimated by the National Sexual Violence Resource Center (Harrisburg, Pennsylvania USA; one in four for girls and one in six for boys). 66
Although the search strategy was designed to capture studies in post-earthquake Haiti related to all aspects of child health, studies have largely focused on clinical presentations and outcomes. However, large natural disasters such as the 2010 earthquake often weaken many aspects of society, including public health infrastructure, educational services, employment opportunities, housing, and basic services such as water, sanitation, and electricity. Knowledge gaps associated with these broader determinants of health, such as earthquake-related changes in poverty, occupational opportunities that affect child and family life, or disruptions in schooling, were under-represented in this review and are a recommended area of priority for future research. In future research, including research on the health impact of Hurricane Matthew, it will be important to consider the impact of these social determinants of health on children.
Limitations
This study is limited by its inherently retrospective nature and its reliance on a large number of case studies. Although six peer-review databases were searched in addition to the grey literature, it is possible that relevant articles were missed and a total of five non-English/non-French articles were excluded. Because the review only included literature published after the 2010 earthquake, it was not possible to juxtapose health outcomes for children before and after the disaster. Without reviewing baseline health conditions, other than the direct earthquake-related traumatic injuries, it is impossible to draw definitive conclusions regarding the role of the earthquake in determining health outcomes.
Future Research
Several areas for future research were identified. First, it is recommended that long-term disability among children and youth in Haiti be studied. Given the large numbers of reported injuries among children after the 2010 earthquake, there may be a significant unmet need for rehabilitation, physiotherapy, and occupational therapy services. Second, future studies should more closely examine the social determinants of health, such as adequate housing, access to safe water, attendance in school, and social support structures.
Conclusions
The post-earthquake research landscape for child health in Haiti is characterized by relatively few published studies and a heavy representation of cross-sectional designs. Many children were injured in the 2010 earthquake, and since then, children have been significantly impacted by infectious diseases, particularly diarrhea and including cholera. Access to clean water and proper sanitation will be important for reducing these preventable causes of morbidity and mortality in the future. Malnutrition and food insecurity are other important health concerns for children in Haiti, despite on-going efforts to address hunger. Large numbers of Haitian children have significant symptoms of PTSD, peri-traumatic stress, depression, and anxiety, and future health programs for children and youth in Haiti should consider mental health as a priority.
Authors’ Contributions
AD and MM screened and extracted data. AD and MM summarized findings from the articles and provided a rough draft of the results section. CD analyzed the results and provided the discussion. SB conceived the idea and was a major contributor in writing the methods, results, and discussion. All authors edited and approved the final manuscript.
Acknowledgements
The authors are grateful to Dr. Shada Rouhani for her review and helpful comments on this manuscript.






