A literature on breast-feeding in emergencies has grown up in the last decade; across the settings studied, a consistent concern is that women stop breast-feeding in times of crisis(Reference McGrath1–Reference Keeney5). Such settings, and the increased risks associated with not breast-feeding at these times, may alert the public to the need for breast-feeding in general(6) but there are also concerns specific to emergencies. Women may stop earlier or be less likely to initiate breast-feeding when it is most needed, in the face of reduced alternatives and the special need for mother–infant bonding.
The reasons why women stop breast-feeding in emergencies are not completely understood. Unsolicited formula donations might discourage breast-feeding in conflict areas where bottle-feeding was already widespread before the emergency(Reference Young7); this may have occurred in the 1999 Kosovo conflict(Reference Borrel8). According to Cogill, very few mothers have milk insufficiency, and lactating mothers are less prone to stress(Reference Cogill9). In emergencies, there may be a selection out of breast-feeding of those women who are stressed. Interrupted breast-feeding could be an actionable determinant of infant morbidity and mortality in humanitarian crises(Reference McGrath1, Reference Moss10). Yip suggested that some of the excess morbidity in the 1991 Kurdish refugee crisis may have been due to inadequate methods of infant feeding(Reference Yip11), but this is speculative as it is difficult to measure breast-feeding and mortality under such conditions.
Cultural norms and traditions affect breast-feeding and, out of context in emergencies, can be inappropriate(Reference Jelliffe12–Reference Maclaine15).
The countries of the former Yugoslavia mostly did not benefit from the international wave of support and programming for breast-feeding of the 1980s and early 1990s. The limited evidence suggests that breast-feeding practices were poor prior to the conflict. Small studies in Sarajevo showed low levels of breast-feeding and very short periods of exclusive breast-feeding(Reference Robertson, Fronczak and Jaganjac16, Reference Moro17). Studies from other parts of Bosnia reported similar findings(18–Reference Simić, Sumanović-Glamuzina and Boranić20). The studies described in the present paper provide information about breast-feeding practices in the Federation of Bosnia and Herzegovina (BiH) and the Republica Srpska (RS) during the conflict and their association with nutritional status.
Methods
The four surveys used a stratified, random, cluster sample. In 1994, UNHCR (United Nations High Commissioner for Refugees) regional teams with first-hand knowledge of each food aid programme area provided their population registers as a sample frame. This comprehensive official listing of potential beneficiaries (of the food aid programme) in nine operational areas could be divided into blocks of 1000 people. Stratifying by operational area, numbering the blocks and using a random number table, we randomly drew forty-one sites (communities) – one site for every 100 000 people on the register. Because of inflation of beneficiary population figures, this may have been closer to one site per 50 000. As far as possible, subsequent surveys revisited the same sites.
Figure 1 shows the sites included in the four surveys. The 1994 survey included households in the selected forty-one sites in BiH. The 1995 survey revisited thirty-seven of the same sites (military conditions did not permit revisiting of four sites) and an additional fifteen sites in RS; a total of fifty-two sites. In 1996, population relocation required by the Dayton Accord emptied the five Serb-held Sarajevo sites surveyed in 1994 and 1995; five new sites were selected in Eastern Bosnia. The 1996 survey covered sixty-six sites, including thirty in RS. The 1997 survey covered fifty-five communities, forty-five in BiH and ten in RS.
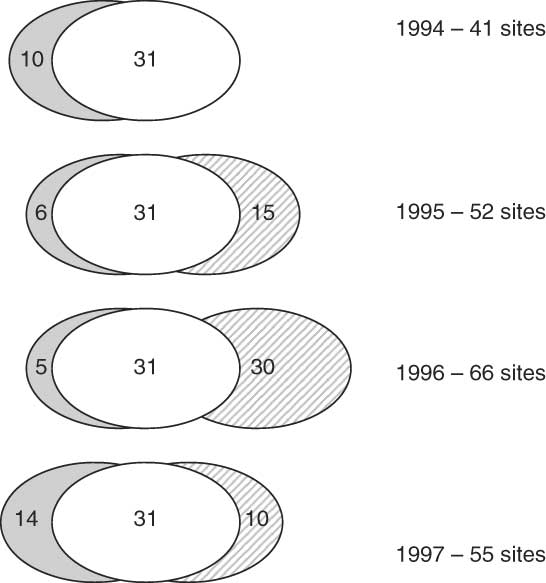
Fig. 1 Chart showing the sites covered in the four surveys: ![]() , sites in Federation of Bosnia and Herzegovina (BiH) covered in all four surveys;
, sites in Federation of Bosnia and Herzegovina (BiH) covered in all four surveys; ![]() , sites in BiH not covered in all four surveys;
, sites in BiH not covered in all four surveys; ![]() , sites in Republica Srpska (ten sites were covered in all three surveys from 1995 to 1997)
, sites in Republica Srpska (ten sites were covered in all three surveys from 1995 to 1997)
During data collection, in each community (site) the trained field teams covered approximately 100 contiguous households, radiating from a random starting point, with no sub-sampling within the site.
For each survey, we trained four to six field teams, each comprising eight to ten members, with the majority female. The same trainer conducted classroom and practical training sessions over one week in each of the four surveys and more than half the team members undertook all four surveys. Special sessions covered measurement of mid upper-arm circumference (MUAC).
The directly administered questionnaire in ‘Serbo-Croat’ (Bosnian) documented the household structure (age and sex of each member), the sex of the head of the household, and how she or he earned a living in the last month. Because of the security implications of questions about ethnicity in the context of ethnic cleansing and conscription, interviewers coded ethnicity of households by observation, without direct questioning.
For each child under 5 years of age, the interviewers asked the mother about aspects of child health, including asking ‘At how many months of age was additional food, besides breast-feeding, introduced?’ and ‘At how many months of age was breast-feeding stopped?’ We did not ask about the nature of the added foods. The interviewers measured MUAC of these same children.
Analysis
Data entry relied on Epi-Info version 6·1, the public domain data entry and analysis package (Centers for Disease Control and Prevention, Atlanta, GA, USA). Double data entry and verification minimised key-stroke errors. Analysis relied on CIETmap open source software(Reference Andersson and Mitchell21).
We analysed patterns of breast-feeding among children aged 1–12 months at the time of the survey (infants). We categorised children as ‘ever breast-fed’ if their mothers gave an age for stopping breast-feeding. Among those children who were ever breast-fed, we took the age in months their mothers reported stopping breast-feeding as the overall duration of breast-feeding (exclusive or not). We counted children who were still breast-feeding at the time of the survey as having breast-fed for the number of months of their age. We considered children who had ever breast-fed to be exclusively breast-fed up until the age when the mother reported they first received complementary foods.
We categorised children with a MUAC of less than 125 mm as malnourished.
Bivariate analysis examined the strength and statistical significance of associations between individual variables and outcomes of interest, with calculation of the Mantel–Haenszel odds ratio and the 95 % confidence interval. Multivariate analysis of the simultaneous effects of different variables relied on simultaneous stratification using the Mantel–Haenszel(Reference Mantel and Haenszel22) and the Mantel Extension(Reference Mantel23) test (for trend). The multivariate analysis began with a saturated model (including all variables potentially related to the outcome of interest) and stepped down to the point where all the remaining variables in the model were significantly related to the outcome. We initially developed three models to examine the effects of individual, household and community characteristics separately. The household/individual variables and the community characteristics included in the initial models are shown in Table 1. We combined the three final models from the step-down process in a single model and repeated the step-down process to produce a single final model.
Table 1 Variables in initial models of multivariate analyses
BiH, Federation of Bosnia and Herzegovina; RS, Republica Srpska; BF, breast-fed; EBF, exclusive breast-feeding.
We adjusted for clustering using the method devised by Lamothe (G Lamothe, unpublished results); this applies a published variance estimator to weight the Mantel–Haenszel odds ratio for cluster-correlated data(Reference Bieler and Williams24, Reference Williams25). The magnitude and statistical significance of associations are expressed as the unadjusted odds ratio from bivariate analysis (OR) and the adjusted odds ratio (ORa) from multivariate analysis. The 95 % confidence intervals around the odds ratio are those of Cornfield, adjusted for clustering by the Lamothe method (CIca).
We calculated the gain in preventable cases of malnutrition by multiplying the risk difference (RD) by the proportion requiring intervention for each variable associated with the outcome in a multivariate analysis. The number that would need to change an aspect of breast-feeding in order to save one case of malnutrition was estimated as 1/RD (number needed to treat). Testing the difference between means relied on a t test or the Kruskal–Wallis test for two groups.
The 4-year time trends analysis included only the thirty-one sites in BiH that could be visited in all four surveys and excluded sites in RS, since no sites in RS were included in the 1994 survey.
Results
We collected and analysed data about 1123 infants over the four surveys: 120 in 1994, 225 in 1995, 301 in 1996, and 477 in 1997. Among the 1123 infants, 538 were aged 1–6 months and 585 were aged 7–12 months.
Initiation of breast-feeding
Of the infants in the four surveys, usable information about breast-feeding was available on 96·8 % (1087/1123). Table 2 shows the proportions of children who were ever breast-fed. One in every five children (220/1087) was never breast-fed at all.
Table 2 Breast-feeding among children aged 1–12 months in four linked representative cross-sectional household surveys in Federation of Bosnia and Herzegovina and Republica Srpska, 1994 to 1997
In a bivariate analysis, infants in BiH were significantly less likely to start breast-feeding compared with their counterparts in RS (OR = 0·63, 95 % CIca 0·42, 0·96; 178/810 in BiH and 42/278 in RS had never breast-fed). On multivariate analysis, ethnicity explained this pattern: ethnic cleansing meant there were no Muslims in RS, and in BiH a typical Muslim infant was much less likely to start breast-feeding than a non-Muslim counterpart (OR = 0·58, 95 % CIca 0·37, 0·91; 420/557 Muslim and 212/252 non-Muslim infants started breast-feeding). Only two factors remained associated with ever breast-feeding in the final multivariate model: Muslim infants were less likely to breast-feed (ORa = 0·57, 95 % CIca 0·35, 0·91) and children from displaced households were less likely to breast-feed (ORa = 0·14, 95 % CIca 0·08, 0·26).
The combination of these two risk factors (Muslim and displaced) increased the disadvantage considerably (Fig. 2). Most Muslim displaced children never breast-fed at all (58·9 % never breast-fed, based on 43/73), compared with 50·4 % (65/129) displaced children, 24·6 % (137/557) Muslim children, 15·5 % (82/528) non-Muslim children and 12·8 % (60/468) non-Muslim non-displaced.
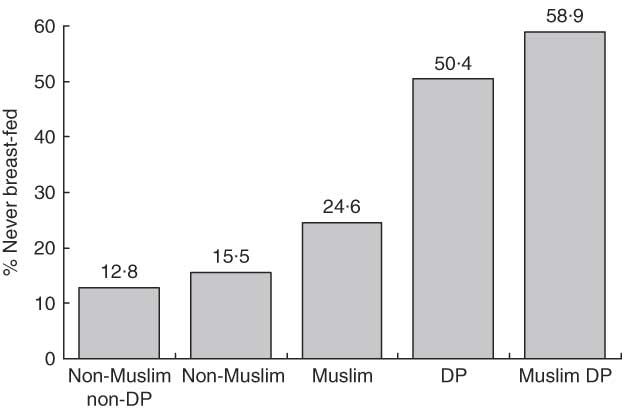
Fig. 2 The combined effect of being Muslim and displaced (DP): percentage of children aged 1–12 months who never breast-fed in four linked representative cross-sectional household surveys in Federation of Bosnia and Herzegovina and Republica Srpska, 1994 to 1997
In the thirty-one sites that participated in all four surveys, there was no consistent change in the proportion of children who were ever breast-fed over the four years.
Duration of breast-feeding
Table 2 shows the average total duration of breast-feeding (exclusive or non-exclusive) among infants who were ever breast-fed (excluding those who were still breast-feeding at the time of the interview). In all infants the average duration was a little over 4 months. The difference in duration of breast-feeding between male and female infants was not statistically significant (P = 0·85), nor was the difference between Muslim (mean 4·64 months) and non-Muslim infants (mean 4·12 months, Kruskal–Wallis H = 2·19, 1 df, P = 0·139).
Among infants who ever breast-fed, two out of every three completed at least 4 months of breast-feeding (549/867). In a multivariate analysis, four variables remained in the final model of breast-feeding duration (Table 3). Infants were significantly less likely to breast-feed for more than 4 months if they were from male absent households, if they were living in a frontline community, if they were living in RS (rather than BiH), and if their household did not receive remittances from abroad. The average duration of breast-feeding was significantly shorter in infants with any of these risk factors (Table 3).
Table 3 Risk factors for not completing 4 months of breast-feeding (exclusive or non-exclusive) from final multivariate model, Federation of Bosnia and Herzegovina and Republica Srpska, 1994 to 1997
BF, breast-feeding (exclusive or non-exclusive); ORa, odds ratio adjusted for effects of other variables in multivariate analysis; CIca, cluster-adjusted confidence interval around odds ratio; RS, Republica Srpska; BiH, Federation of Bosnia and Herzegovina.
*From Kruskal–Wallis test for two groups.
There was no statistical interaction between the four variables. Coming from a frontline community and a female-headed household produced an effect (ORa = 0·39, 95 % CIca 0·24, 0·64) similar to that of just coming from a female-headed household, after taking account of living in RS and not receiving remittances from abroad. Table 4 shows the proportions of children breast-feeding for more than 4 months with different combinations of the four risk factors.
Table 4 Proportion of children breast-feeding longer than 4 months, with different combinations of risk factors, from stratified multivariate analysis, four surveys combined, Federation of Bosnia and Herzegovina and Republica Srpska, 1994 to 1997
FHH, female-headed household; MHH, male-headed household.
Among Muslim children, there was no evidence that boy children were more likely than girl children to complete 4 months of breast-feeding (bivariate analysis, OR = 0·94, 95 % CIca 0·60, 1·48; 134/208 boys and 139/211 girls completed 4 months). There was no significant difference in the average duration of breast-feeding between Muslim boys and girls (P = 0·107).
In the thirty-one sites visited by all four surveys, the mean duration of exclusive breast-feeding was 4·77 months (n 246, sd 3·644) in the conflict years 1994 and 1995, and increased to 5·77 months (n 217, sd 3·409) in the post-conflict years 1996 and 1997 (Welch t test, P=0·0026).
Duration of exclusive breast-feeding
Among infants ever breast-fed, the average duration of exclusive breast-feeding was 3·31 months (sd 2·058, n 754). Exclusive breast-feeding was significantly longer among Muslim infants than among their non-Muslim counterparts (0·37 months longer, P = 0·013). There was no detectable difference between the average duration of exclusive breast-feeding between male and female children but, among Muslim children, the duration of exclusive breast-feeding was significantly longer in girls than in boys (on average 0·5 months longer, P = 0·027).
Among infants ever breast-fed, just 8·2 % (62/754) received complementary foods for the first time during their sixth month of life; others were exclusively breast-fed for less than 5 months or more than 6 months. The proportion with exclusive breast-feeding into their sixth month was the same in male and female children, for Muslim and non-Muslim children and, among Muslim children, for male and female infants.
During the period of the conflict, there was a consistent increase in duration of exclusive breast-feeding. In the thirty-one sites visited by all four surveys, the mean duration of exclusive breast-feeding in months was 3·04, 3·42, 3·76 and 4·19 respectively for 1994, 1995, 1996 and 1997.
Breast-feeding and malnutrition
Infants who never breast-fed were much more likely (in a bivariate analysis) to be malnourished (MUAC < 125 mm; OR = 1·78, 95 % CIca 1·26, 2·52; 70/177 malnourished among those who never breast-fed and 201/749 malnourished among those ever breast-fed). In a multivariate analysis, no other variable was significantly related to malnutrition in infants.
Considering only infants ever breast-fed, the average duration of breast-feeding (exclusive or non-exclusive) among children with MUAC < 125 mm was 4·58 months compared with 5·25 months among those with normal MUAC (P = 0·027). And, in a multivariate analysis, an average infant who did not complete 4 months of breast-feeding was significantly more likely to be malnourished (ORa = 1·45, 95 % CIca 1·02, 2·07; 134/431 who stopped breast-feeding before 4 months were malnourished, compared with 84/354 who stopped later).
As shown in Fig. 3, infants with exclusive breast-feeding into their sixth month of age had the lowest proportion malnourished, with higher rates of malnutrition among those with exclusive breast-feeding for less than 5 months or more than 6 months. The highest rate of malnutrition was among infants with exclusive breast-feeding for 2 months or less. An infant with exclusive breast-feeding for less than 5 months or more than 6 months was significantly more likely to be malnourished than one with exclusive breast-feeding into their sixth month of life (ORa = 1·98, 95 % CIca 1·01, 7·35; 156/609 with exclusive breast-feeding less than 5 months or more than 6 months and 8/54 with exclusive breast-feeding into their sixth month had MUAC < 125 mm).
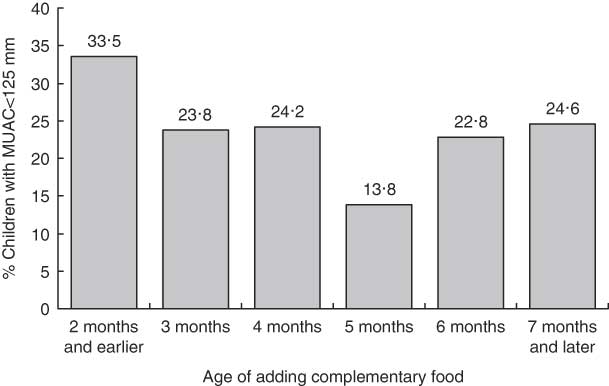
Fig. 3 Proportion of infants with mid upper-arm circumference (MUAC) <125 mm with different durations of exclusive breast-feeding, among infants ever breast-fed, in four linked representative cross-sectional household surveys in Federation of Bosnia and Herzegovina and Republica Srpska, 1994 to 1997
Table 5 summarises the potential population gain for infant malnutrition that could have been achieved by improving breast-feeding, assuming no change in other factors related to infant malnutrition.
Table 5 Summary implications of changing breast-feeding patterns for malnutrition in children aged 1–12 months, Federation of Bosnia and Herzegovina and Republica Srpska, 1994 to 1997
MUAC; mid upper-arm circumference; RD, risk difference; NNT, number needed to treat; PRI, proportion requiring intervention (malnourished who do not benefit); gain = RD × PRI, reflected here per 1000 of the analysis base (e.g. never starting, in the first row); population gain, applying this to the entire childhood population aged 1–12 months, per 1000.
• If all children had breast-fed, this could potentially have reduced malnutrition by ten per 1000 infants; every eight additional infants who breast-fed could potentially have saved one case of malnutrition among non-breast-fed infants.
• If all breast-fed children had continued breast-feeding for longer than 4 months this could potentially have saved another five cases per 1000 infants; every nineteen additional infants who continued breast-feeding beyond 4 months could potentially have saved one case of malnutrition among those who did not go beyond 4 months.
• Among those infants ever breast-fed, if all had continued exclusive breast-feeding into the sixth month of life this could potentially have saved twenty-five cases of malnutrition per 1000 infants; every nine additional infants with exclusive breast-feeding into their sixth month could potentially have saved one case of malnutrition.
Overall, improving breast-feeding could have reduced infant malnutrition by some 2–3 %, if other factors related to malnutrition did not change.
Discussion
Two factors reduced the chances of starting breast-feeding during the conflict: being Muslim and being displaced. The combined effect of these two factors on starting breast-feeding was bigger than either factor on its own; close to 60 % of Muslim displaced children never started breast-feeding. It is not clear why there was less breast-feeding among Muslim children; the Koran supports a full two years of breast-feeding for all children(Reference Hutchinson26–Reference Shaikh and Ahmed29). Among displaced people, one likely explanation is the interruption of support networks. It is not surprising that mothers should be less enthusiastic to breast-feed when they are threatened with genocide, when every family has lost members and homes to ethnic cleansing, and they live in a state of siege depending on the UN for food rations. It would take a special sort of resilience to continue mothering as normal in the face of this. The surprise is that many did manage to breast-feed, and in fact the duration of breast-feeding and exclusive breast-feeding increased among children who breast-fed at all. The factors that increased the risk of not completing 4 months of breast-feeding – living in RS, being in a female-headed household, not receiving remittances from abroad and living in a frontline community – show how the effects of vulnerability accrue to different population segments.
At the time of the surveys, 4 months was the minimum recommended duration of exclusive breast-feeding(30–Reference Robertson32) although a subsequent Cochrane review concluded that exclusive breast-feeding for 6 months has additional advantages over exclusive breast-feeding for 3 or 4 months(Reference Kramer and Kakuma33) and this led WHO to recommend exclusive breast-feeding for 6 months(Reference Kramer and Kakuma34). Social norms for weaning (adding complementary foods) vary enormously from place to place. There are some useful biological pointers. The infant digestive system is able to accept other foods after the sixth month(35). Because Fe stores are used up by the age of 6 months, delaying introduction of complementary foods beyond this age could put the infant at risk for Fe-deficiency anaemia and other micronutrient deficiencies(Reference Dewey36). Our analysis considered the sixth month as the appropriate point for adding complementary foods.
Only 8 % of ever breast-fed children in our study benefited from exclusive breast-feeding into their sixth month of life. Exclusive breast-feeding for either less than 5 months or more than 6 months was associated with more malnutrition than exclusive breast-feeding into the sixth month. While a number of authors have indicated the advantages of exclusive breast-feeding for 6 months over shorter durations of exclusive breast-feeding, there is a need for more information about potential disadvantages for nutritional status of continuing exclusive breast-feeding for longer than 6 months(Reference Kramer and Kakuma33). Small shifts in breast-feeding could matter in emergencies. Child health might ‘decompensate’ differently to produce more malnutrition than in non-emergency settings. The finding of a narrow window for adding complementary foods may be important, if other studies in emergency settings reproduce the finding.
The surveys produced evidence that poor breast-feeding patterns contributed to infant malnutrition. Malnutrition increased over the course of the conflict(Reference Andersson, Legoretta-Soberanis and Paredes-Solis37), despite no change in the proportion ever breast-fed and an actual increase in duration of breast-feeding and exclusive breast-feeding among those who started. The increased malnutrition may have been related to a reduced quality of breast-feeding, such as less frequent or shorter feeds, not reflected in the measured breast-feeding indicators of initiation, duration of exclusive breast-feeding and overall duration. The adequacy of complementary foods in the diet may also have decreased, but we have no direct evidence on this point.
Our evidence suggests some of the increased childhood malnutrition that occurred during the conflict could have been avoided if breast-feeding had improved. Several authors have stressed the importance of supporting breast-feeding in emergencies, providing practical guides for doing so(Reference Al Gasseer, Dresden and Keeney2, 4, Reference Keeney5, Reference Kelly38). The steps it takes to support initiation and adequate duration of breast-feeding(Reference Latham39) are well within the reach of the UN relief organisations.
Conclusions
The low proportion of children ever breast-fed and the short duration of breast-feeding and exclusive breast-feeding in the conflict reflected pre-conflict levels. Never breast-feeding and short duration of breast-feeding and of exclusive breast-feeding were related to infant malnutrition. If relief agencies had promoted and supported breast-feeding, this might have avoided some of the increased malnutrition that occurred during the Bosnian conflict.
Acknowledgements
Sources of funding: This work was supported by the World Food Programme and the United Nations High Commissioner for Refugees (surveys in 1994, 1995 and 1996), and the World Bank (1997 survey). Conflict of interest declaration: The authors have no conflicts of interest. Authors’ contributions: N.A. designed the studies and instruments, trained the managers and field coordinators, conducted the analysis and drafted the paper. S.P.-S. assisted with the fieldwork management and with data management and analysis, and critically reviewed the paper. J.L.-S. assisted with the analysis and critically reviewed the paper. A.C. assisted with the analysis and helped to draft the paper. L.S. reviewed the analysis, supporting the drafting of the paper, and critically reviewed the paper. Acknowledgements: Kate Galt, Indira Kulenovic, Nicole Massoud, Sharmila Mhatre, Lorenzo Monasta, Manuel Pascual Salcedo, Aparna Swaminathan and Charles Whitaker of CIET supported the data collection in one or more of the four surveys. Thanks go to Mary Cameron and Jeff Jarabek for their help with retrieval of the literature. Gilles Lamothe developed a variance estimator that weights the odds ratio for cluster-correlated data using the Mantel–Haenszel procedure, and Mario Beauchamp developed an open source application that made this available for the analysis.










