Introduction
Starting from early ages, sedentary lifestyle and unhealthy eating habits increase metabolic and cardiovascular (CV) risks (CVR) of individuals. These issues impose medical, economic, and psychological burden on the healthcare system, which might emerge as morbidity and mortality (Clark et al., Reference Clark, Alonso, Spencer, Pencina, Williams and Everson-Rose2014). Moreover, conditions such as obesity and CV diseases might present earlier due to unhealthy lifestyle habits and environmental factors (Arora et al., Reference Arora, Stouffer, Kucharska-Newton, Qamar, Vaduganathan, Pandey, Porterfield, Blankstein, Rosamond, Bhatt and Caughey2019, Fryar et al., Reference Fryar, Carroll and Afful2020). One of the most efficient strategies to prevent or minimize these public health issues is to define the risks and intervene appropriately as soon as possible (Nissinen et al., Reference Nissinen, Berrios and Puska2001).
As for all age groups, healthy lifestyle is of key significance also in younger population. CV and metabolic risk factors presenting early are known to cause predisposition to long-term effects (Hardy et al., Reference Hardy, Lawlor and Kuh2015). In addition, results from existing literature show that effects of risk-modifying interventions might wear off in time, and younger individuals might comply poorly to intervention-induced lifestyle changes (Van De Vijver et al., Reference Van De Vijver, Oti, Addo, De Graft-Aikins and Agyemang2012, Tran and Sojobi Reference Tran and Sojobi2020). Therefore, promoting healthy lifestyle to the young as soon as possible is important due to potential of better outcomes, such as effectively raising and spreading the much needed awareness, detecting possible health risks earlier and managing any related issues properly, thus reducing the medical and economic burden (Naderi et al., Reference Naderi, Sauris, Rodriguez and Foody2012).
It could be expected that after end of a stressful period of preparation to entry exams, students recently admitted to university might comply with healthy lifestyle principles more than before. Also, a graduate who adopted a healthy lifestyle might possibly instill awareness to her/his surroundings (Vedanthan et al., Reference Vedanthan, Bansilal, Soto, Kovacic, Latina, Jaslow, Santana, Gorga, Kasarskis, Hajjar, Schadt, Björkegren, Fayad and Fuster2016). On the other hand, various issues concerning university students more closely might be threatening for their overall health. For example, students leaving their families for college might fail to properly manage the changes in their daily activities such as eating, accommodation and exercising, leading to medium to long-term health-related risks (Plotnikoff et al., Reference Plotnikoff, Costigan, Williams, Hutchesson, Kennedy, Robards, Allen, Collins, Callister and Germov2015). Apart from those, it should be noted that tobacco, recreational drugs, and various drug/non-pharmaceutical products, some claiming to promote bodybuilding and enhance performance, are frequently used by young individuals (İlhan et al., Reference İlhan, Arikan, Kotan, Tunçoğlu, Pinarci, Taşdemir, Ay and Koçak2016, Valentine et al., Reference Valentine, Schumacher, Murphy and Ma2018).
Considering all those, it is crucial to determine the extent of CVR burden in young population along with the affecting factors, in order to appropriately screen their risks and control them early. In that regard, this study aimed to determine the presence of CVR factors in university students and evaluate how these factors are affected from the knowledge, attitude, and habits of the individuals regarding healthy lifestyle.
Methods
This cross-sectional study was conducted in April–May 2018 as part of Marmara University Student Healthy Lifestyle and Cardiovascular Risk Assessment (MUSAY-CARD) Project, coordinated by Marmara University Hypertension and Atherosclerosis Research Center (HIPAM). Data were collected from the volunteers at the previously determined locations in the campuses by the involved physicians and nurses using face-to-face questionnaires, physical examination, and blood tests. Written informed consent was obtained from each participant. Ethical approval was obtained from Marmara University School of Medicine Ethical Committee for Clinical Studies (approval number: 09.2017.327).
Participants
The study population consisted of students of Marmara University, which provides education to more than 70000 students at various campuses in Istanbul. Participants of the study were determined via convenience sampling. Main campus and two other campuses, which were home to faculties of health sciences and sports sciences, were selected. All students studying at those campuses were informed about the study, and those who volunteered to participate answered the questionnaires and underwent physical examination and blood tests. A total of 1000 participants was determined as target sample group. Inclusion criteria were being an undergraduate student, being 18 years of age and older, and signing the informed consent form. Final year students, along with associate, graduate, and postgraduate students, were not included in the study.
Clinical measurements
Body mass index (BMI) values of the participants were calculated according to height and weight measurements (Nuttall, Reference Nuttall2015). Blood pressure (BP) measurements were made in accordance with current guideline recommendations (Williams et al., Reference Williams, Mancia, Spiering, Agabiti Rosei, Azizi, Burnier, Clement, Coca, de Simone, Dominiczak, Kahan, Mahfoud, Redon, Ruilope, Zanchetti, Kerins, Kjeldsen, Kreutz, Laurent, Lip, McManus, Narkiewicz, Ruschitzka, Schmieder, Shlyakhto, Tsioufis, Aboyans and Desormais2018). Random total cholesterol (TC) and blood glucose (BG) measurements were done from capillary blood obtained by fingerstick. As test kits and strips, “Accutrend Plus/Cholesterol” (Roche Diagnostics, Basel, Switzerland) was used for TC and “Accu-Chek Performa” (Roche Diagnostics, Basel, Switzerland) was used for BG measurement.
Questionnaire data
Knowledge, attitude, and habits of the participants about their nutrition and physical activity were assessed via questionnaires. The first form included 22 items, questioning sociodemographic characteristics, nutritional and physical activity levels, along with attitudes and behaviors regarding regular use of drugs and non-pharmaceutical medicinal products. Compliance with the Mediterranean diet was examined by using Mediterranean Diet Quality Index (KIDMED). KIDMED consists of a questionnaire with 16 ‘yes/no’ questions that focus on the participants’ eating habits to assess the compliance to Mediterranean style of diet, which is suggested to be suitable for a healthy lifestyle and lower CVR (Serra-Majem et al., Reference Serra-Majem, Ribas, Ngo, Ortega, García, Pérez-Rodrigo and Aranceta2004). This index was reported to be valid and reliable in Turkish population (Şahingöz et al., Reference Şahingöz, Özgen and Yalçın2019). Students’ level of knowledge on CV diseases was measured using the Cardiovascular Disease Risk Factors Knowledge Level (CARRF-KL) Scale, which consists of 28 items questioning participants’ knowledge about characteristics of CV diseases, CVR factors, and outcome of changes in risk behaviors (Arikan et al., Reference Arikan, Metintaş, Kalyoncu and Yildiz2009). Health literacy status was evaluated via responses to Turkish Health Literacy Survey (HLS-TR). HLS-TR, which is the Turkish adoptation of HLS-EU-Q47 (European Health Literacy Survey Questionnaire), is a 32-item, 5-point Likert scale used to evaluate health literacy status by answers to questions about accessing, understanding, appraising, and applying health-related information (Abacigil et al., Reference Abacigil, Harlak, Okyay, Kiraz, Turan, Saruhan, Karakaya, Tuzun, Deniz, Tontus and Beşer2019). Collected data were compared according to the sociodemographic characteristics, and the risk factors were determined by measurements and answers. Answers to CARRF-KL scale were evaluated using 0–28 score range, whereas responses to KIDMED index and HLS-TR scale were analyzed categorically, with the first one as ‘poor’ and ‘average/good’, and the second as ‘adequate/excellent’ and ‘inadequate/problematic-limited’.
Evaluation
Based on answers to questionnaires, physical examination findings, and measurements, individuals with at least one of the following characteristics were classified in ‘high-risk group’ for CV disease risk. Accordingly, those who reported a history of smoking or diagnosis of diabetes, hypertension, and/or another cardiac diagnosis, the individuals with high BP (≥140/90 mmHg), high BG (≥200 mg/dl), and/or high TC (≥200 mg/dl), those with increased waist circumference (WC, >102 cm for males and >88 cm for females) and BMI over 30 kg/m2 were included in high CVR [CV(+)] group. Individuals without those traits were classified as low risk [CV(−)]. Data collected on physical activity levels and eating habits were compared according to CVR presence and sociodemographic characteristics.
Statistical analysis
Collected data were analyzed using IBM SPSS Statistics for Windows, Version 22.0 (IBM Corp., Armonk, NY, USA) software. Analyzed data were expressed as numbers, percentages, and/or mean ± standard deviation values, wherever appropriate. Frequency analysis was used for statistical evaluation, whereas chi-square test was used for comparison of the categorical variables. Continuous variables were evaluated for normal distribution prior to comparison using Kolmogorov–Smirnov analysis. Normally distributed data were compared using Student’s t-test, whereas Mann–Whitney U test was used in case of an absence of normality. An overall 5% type I error level was used to infer statistical significance.
Results
A total of 770 students were included in the study (response rate: 77.0%). The mean age was 22.3 ± 2.6 (range: 19–41 years) and 59.6% (n = 459) were female. Details of sociodemographic characteristics and health-related habits were presented in Table 1. More than half (53.4%) of the students fell into ‘average/good’ KIDMED category, whereas in terms of health literacy, 51.8% were ‘inadequate/problematic-limited’ (Table 1). The mean CARRF-KL score was 22.8 ± 2.9 (Table 2).
Table 1. Sociodemographic and other characteristics of the participants

a Cardiovascular risk.
b Mediterranean Diet Quality Index.
c Turkish Health Literacy Scale.
Table 2. Distribution of general characteristics by presence of cardiovascular risk
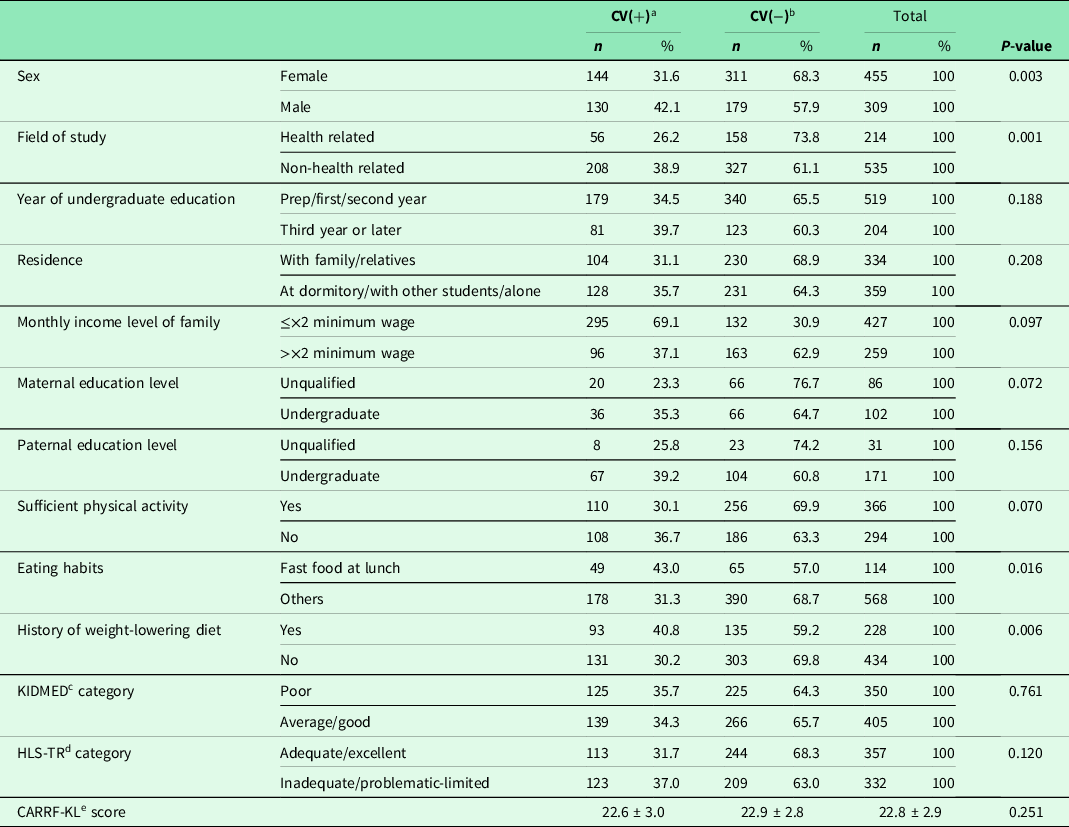
a Cardiovascular high-risk group.
b Cardiovascular low-risk group.
c Mediterranean Diet Quality Index.
d Turkish Health Literacy Scale.
e Cardiovascular Risk Factors Knowledge Level Scale.
Cardiovascular risk factors
Participants with single CVR factor was 27.5% (n = 210) of all, whereas 8.4% (n = 64) had multiple-risk factors. Mean risk count of the 274 CV(+) individuals (35.9%) was 1.3 ± 0.5 (range: 1–3). The most common risk factor was smoking (20.6%), followed by high TC (7.5%), hypertension/high BP (6.0%), increased WC (5.6%), obesity (3.4%), diabetes/high BG (1.8%), and cardiac disease (0.5%), respectively. The prevalence of smoking and hypertension/high BP was higher in males (27.7% versus 15.8% and 10.3% versus 3.1%, respectively; P < 0.001 for each), whereas increased WC was more common in females (7.2% versus 3.2%, respectively; P = 0.018) (Figure 1). Parametric values of the examined data by gender were presented in Supplementary Table 1.
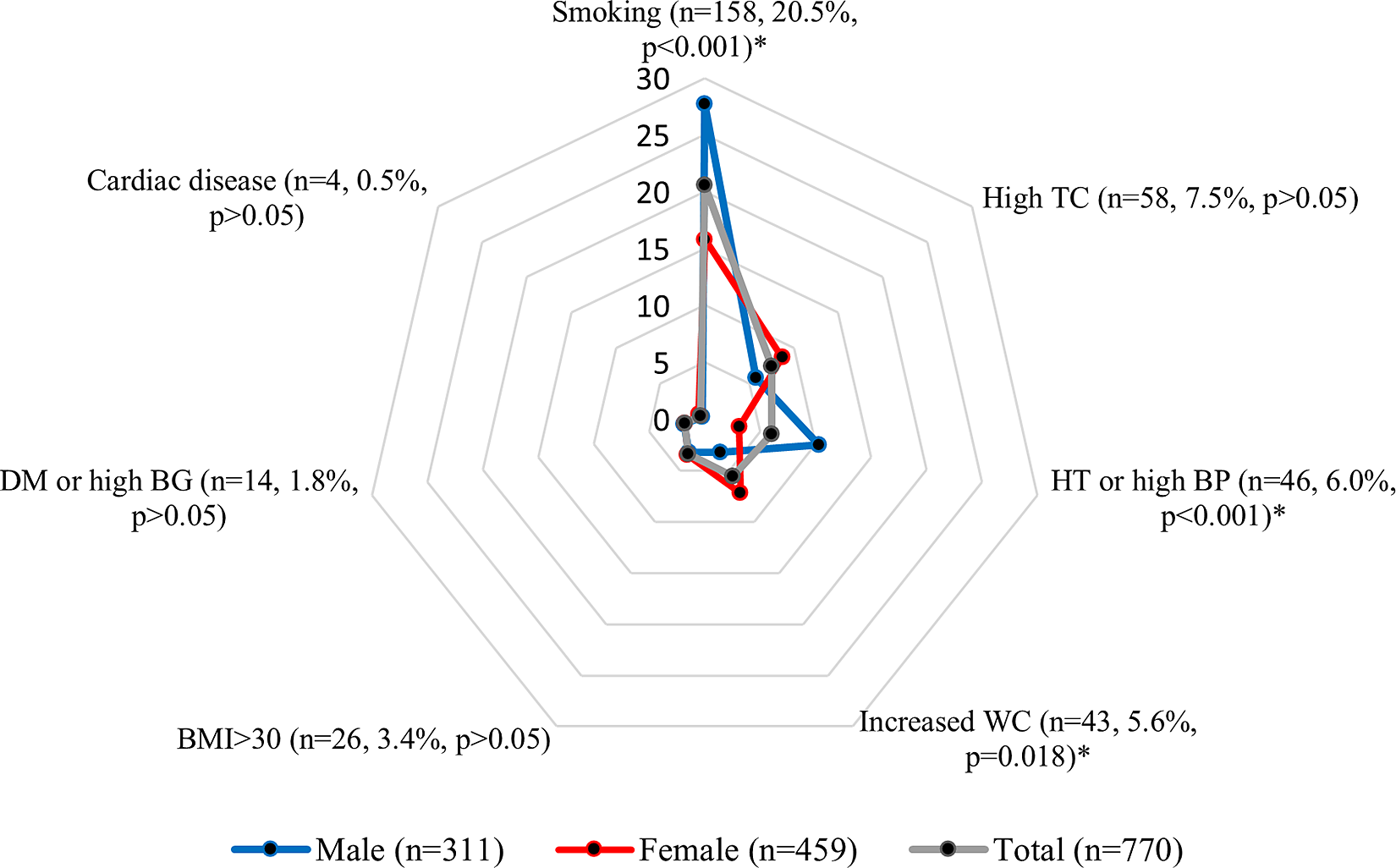
Figure 1. Percentage distribution of risk factors by gender. *: P < 0.05. TC: Total cholesterol, HT: Hypertension, BP: Blood pressure, BMI: Body mass index, DM: Diabetes mellitus, BG: Blood glucose.
The mean ages of CV(+) and CV(−) groups were similar (22.6 ± 3.0 and 22.2 ± 2.4, respectively; P > 0.05). CV(+) individuals were more common in males (42.1% versus 31.6% in females; P = 0.003). The percentage of non-health-related field students were higher in CV(+) group (78.8% versus 67.4% in CV(−); P = 0.001). CV(+) and CV(−) were similar in terms of other sociodemographic characteristics, CARRF-KL scores, KIDMED index, and HLS-TR categories (P > 0.05), (Table 2).
Physical activity status
Almost half of the students (44.6%) declared their physical activity as below the CV-protective level. Inadequate physical activity was more widespread in females (53.4% versus 30.5% in males; P < 0.001). Physical activity level was not significantly different by CVR presence, category of residence, monthly income of the family, and maternal education level (P > 0.05). Distribution of participants stating an increase or decrease in activity after starting university were similar in CV(+) and CV(−) (P > 0.05), (Supplementary Table 2).
Eating habits
Approximately one-sixth (16.5%) of the participants reported consuming fast foods at the university cafeteria for lunch. That was more common in CV(+) than CV(−) (21.9% versus 14.3%, respectively; P = 0.017). Distribution by gender was similar (P > 0.05). 33.8% of the students stated going on a diet at least once to lose weight, and the percentage of those were higher in CV(+) (41.5% versus 30.8% in CV(−), P = 0.006) and females (38.2% versus 29.2% in males, P = 0.03). Students who reported having a better diet since the start of university were more common in CV(−) group compared to CV(+) (27.2% versus 17.0%; P = 0.003). Conversely, percentage of participants stating that their diet had worsened were higher in CV(+) (49.4% versus 38.3%, respectively; P = 0.005), (Supplementary Table 3).
Multiple cardiovascular risk factors
Of 64 students with multiple-risk factors, 53 (7.0% of all participants) had 2 and 11 (1.4%) had 3. Most commonly accompanying CVR factors were increased WC with obesity in 19 students (29.7%), high TC with smoking in 15 (23.4%), and increased WC with smoking in 10 (15.6%) (Table 3). Comparison of single versus multiple-risk factor individuals showed that history of weight-lowering diet was more commonly observed in single-risk group (P < 0.001), whereas “average/good” KIDMED category was more abundant in multiple-risk group (P = 0.019), (Supplementary Table 4).
Table 3. Distribution of cardiovascular risk factors among patients with multiple risks
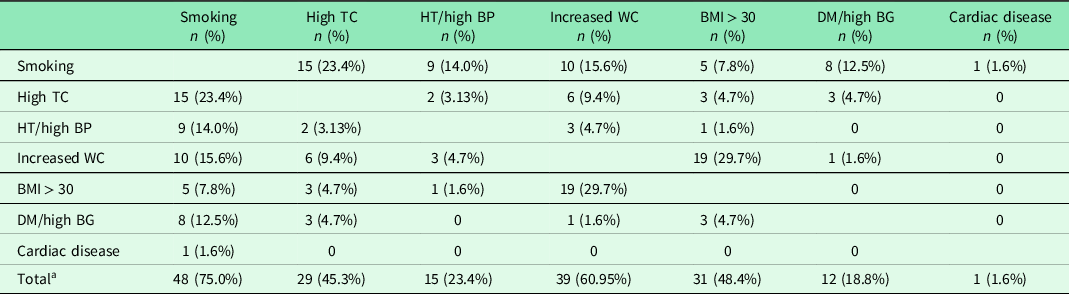
a Percentages were calculated over the total number of patients with multiple risks (n = 64).
Regular use of drugs
Of all participants, 15.5% (n = 109) reported use of at least one drug/non-pharmaceutical product regularly. 9.1% of the students (n = 64) were regular drug users due to underlying chronic conditions. This was more common in CV(+) group (12.9% vs 7.1% in CV(−), P = 0.012) and females (11.9% versus 4.7% in males, P = 0.001). Those who declared regular use of non-pharmaceutical products (8.5%) were more common in females (10.0%) compared to males (4.7%), (P = 0.011); whereas the distribution by CV(+) and CV(−) groups was similar (10.3% versus 6.9%, respectively; P > 0.05). A total of 50 drugs containing 30 different active ingredients were reported. Most commonly used three drugs were levothyroxine (n = 9, 18% of all drugs), sertraline (n = 4, 8%), and acetylsalicylic acid (n = 3, 6%), whereas in non-pharmaceutical products, the first three consisted of vitamins (51.8%), dietary supplements (19.6%), and protein powder (12.5%).
Discussion
This study involved high number (n = 770) of university students, focusing on their lifestyle habits regarding health and conducted with direct and voluntary participation of student clubs. In the study, which represented both genders in a balanced manner, remarkable findings related to the lifestyle and CVRs of the young population were revealed. Accordingly, the frequency of CVR factors among university students being similar to the general population might be regarded as concerning. Despite the partial relationship between CVRs of participants with physical activity levels and eating habits, health literacy levels and monthly income levels of families do not appear to be directly related with those risks.
Although the EuroSCORE risk model is more widely used in clinical practice nowadays, due to its validity being limited to individuals at age 40 or older, mainly Framingham Risk Analysis parameters were used in the study to assess CVR of our sample of younger age (Cooney et al., Reference Cooney, Dudina and Graham2009, Pencina et al., Reference Pencina, D’Agostino, Larson, Massaro and Vasan2009). It is noteworthy that more than one-fourth of participants have at least one CVR factor, and smoking was the leading one. According to Global Adult Tobacco Survey data, smoking prevalence in Turkey was 27.1% (Turkish Public Health Institution, 2014). In a study done among university students in seven European countries, smoking prevalence in Turkey was reported as 49.8% in males and 37.7% in females, whereas the rates in other countries vary between 19%–44% in males and 17%–39% in females (Pischke et al., Reference Pischke, Helmer, McAlaney, Bewick, Vriesacker, Van Hal, Mikolajczyk, Akvardar, Guillen-Grima, Salonna, Orosova, Dohrmann, Dempsey and Zeeb2015). Percentage of regular smokers in our study is lower both in males (27.7%) and females (15.8%) than the aforementioned studies, hence, our results could suggest a downward trend. On the other hand, it should be noted that around three-fourth of the participants were first or second-year students. Previously, it was reported that prevalence of smoking doubled in senior undergraduate students compared to freshmen (Sarioglu et al., Reference Sarioglu, Cuce, Erel, Kose, Arslan and Bodur2016). Furthermore, any delay in age of onset of smoking due to early interventions is known to help in reducing nicotine addiction (Everett et al., Reference Everett, Warren, Sharp, Kann, Husten and Crossett1999). All these information suggest that despite the effective campaigns and the measures taken against tobacco products in Turkey in recent years, high prevalence of smoking among university students retains its place as a health issue. Thus, for further interventions planned against smoking among university population, focusing to the students those newly started to education might be more beneficial.
The second most common risk factor was high TC, which was similar in both genders. Turkish Chronic Diseases and Risk Factors Prevalence Study, which determined the frequency of various CV and metabolic risk factors nationally, reported mean TC values as 148.8 ± 0.9 mg/dl in 15–24-year-old males and 153.7 ± 0.8 mg/dl in females of the same age. That study also reported high cholesterol levels showed female predominance in all age groups, except 25–44-year-old age group (Turkish Public Health Institution, 2013). In our study, TC levels under 150 mg/dl could not be measured, hence, that prevents a direct comparison of our results with the existing literature. Nevertheless, mean TC values of both female (175.1 ± 21.7) and male (171.1 ± 22.4) subjects over 150 mg/dl seems to be consistent with the findings of previous studies. The prevalence of increased WC (7.2% in females versus 3.2% in males) observed in our study was lower than the national prevalence (10.6% in females versus 5.9% in males); however, these two results were in accordance in terms of female predominance (Turkish Public Health Institution, 2013). The similarity of university students and the general population in frequencies of modifiable risk factors such as smoking, TC, and WC needs attention. On the other hand, the rapid rise in CVR seen in females both in Turkey and worldwide in recent years made raising awareness necessary and stimulated the initiation of campaigns as a result (Maas et al., Reference Maas, Van Der Schouw, Regitz-Zagrosek, Swahn, Appelman, Pasterkamp, Ten Cate, Nilsson, Huisman, Stam, Eizema and Stramba-Badiale2011). Similar interventions might also be necessary and effective for young people, including university students.
Another remarkable finding of the study was the CV(+) and CV(−) groups being alike in terms of family income and parent education. Also, the distribution of CARRF-KL scores and HLS-TR categories of the two groups were similar. These findings point out that the family income and parent education levels, along with the health literacy of the participants, might not be directly reflected onto their health-related attitudes and behaviors. Although that approach of these young adults could change at their later ages, it was reported that undesirable effects of CVR factors occurring at an early age might present in adulthood, even if they were treated as soon as possible (Murthy et al., Reference Murthy, Abbasi, Siddique, Colangelo, Reis, Venkatesh, Carr, Terry, Camhi, Jerosch-Herold, De Ferranti, Das, Freedman, Carnethon, Lewis, Lima and Shah2016, Tran and Sojobi, Reference Tran and Sojobi2020). For that reason, that holds a significant importance to develop effective and participatory ways to transform health-related knowledge into internalized attitudes and behaviors (Schwalm et al., Reference Schwalm, McCready, Lopez-Jaramillo, Yusoff, Attaran, Lamelas, Camacho, Majid, Bangdiwala, Thabane, Islam, McKee and Yusuf2019, Tran and Sojobi, Reference Tran and Sojobi2020).
Almost half of the subjects reported insufficient physical activity levels. More than half of females and approximately one-third of males had insufficient physical activity levels. These findings are consistent with the results of current literature, which emphasized low levels of physical activity in whole population including university students (Dinc et al., Reference Dinc, Sozmen, Ergor, Sakarya, Yardim and Unal2015, Tek et al., Reference Tek, Mortas, Arslan, Tatar and Kose2020). Higher percentage of individuals with increased physical activity (55.2%) than those who were more sedentary than before (27.5%) might be related to well-developed facilities in their campuses, as well as their previous exercising habits. In addition, significant reduction in physical activity after starting university education were reported in a recent study (Alkhateeb et al., Reference Alkhateeb, Alkhameesi, Lamfon, Khawandanh, Kurdi, Faran, Khoja, Bukhari, Aljahdali, Ashour, Bagasi, Delli, Khoja and Safdar2019). Relatively high numbers in individuals with increased physical activity could be regarded as favorable. On the other hand, students in the last years of high school education might have been away from exercising during long periods of exam preparation. Therefore, a significant proportion of students being physically more active could be attributed to them being excessively sedentary before university. Overall, despite slight improvements in some students, physical activity levels in university students could be regarded as below expectations. In accordance with the relevant medical guidelines, interventions facilitating and encouraging exercising should be chosen over instead of solely settling with preferences of the individuals (Piepoli et al., Reference Piepoli, Hoes, Agewall, Albus, Brotons, Catapano, Cooney, Corrà, Cosyns, Deaton, Graham, Hall, Hobbs, Løchen, Löllgen, Marques-Vidal, Perk, Prescott, Redon, Richter, Sattar, Smulders, Tiberi, Van Der Worp, Van Dis, Verschuren and Binno2016).
Another notable finding of the study was the higher rate of fast food consumption, which could be interpreted as an unfavorable eating behavior, in CV(+) group. Moreover, among those who declared such behavior, there were more subjects who stated a decrease in their physical activity levels. These findings are important in pointing out that attitudes and behaviors unfavorable for CV system might coexist, and holistic approaches are needed to provide effective solutions. Consistent with the student statements above, it was revealed that only 11% of the participants comply well with the Mediterranean diet according to KIDMED index. A study conducted among high school students in Istanbul reported that the rate of healthy eating behavior, which was described as consuming at least three of the food groups in the food pyramid at the right amounts, was found to be 23% (Akman et al., Reference Akman, Tuzun and Unalan2012). This could suggest that dietary habits might become less heart friendly when transitioning from high school to university. Another study conducted among university students in UK reported that similar to our results, healthy eating behavior was found to be 19% and 31% of the participants were found to have risky or mixed eating habits (Tanton et al., Reference Tanton, Dodd, Woodfield and Mabhala2015). In a qualitative study conducted with university students, the most critical finding was put forth as the importance of consulting students while planning any interventions to develop healthy eating behaviors on campus (Sogari et al., Reference Sogari, Velez-Argumedo, Gómez and Mora2018). This result suggests that attempts to be made with the participation of university student groups, as in our study, might be more successful.
Approximately one out of every seven students reported regular drug/non-pharmaceutical product use, and one-eleventh of all participants declared regular drug use due to chronic disease. Levothyroxine being the most reported drug seems in accordance with the high prevalence of hypothyroidism in Turkey (Erdoǧan et al., Reference Erdoǧan, Demir, Emral, Kamel and Erdoǧan2009). The second most used drug was the antidepressant drug, sertraline. The prominence of sertraline among antidepressants may be related to being among most frequently prescribed drugs by both adult and child and adolescent psychiatrists (Aydin et al., Reference Aydin, Kirmizi, Isli, Aksoy and Akici2020). That finding might imply the significance of depression and anxiety disorders in young adult group, which our subjects belong to. Also, one-twelfth of the students using at least one non-pharmaceutical product regularly is noteworthy. Vitamin, mineral, and protein supplements being the most used ones is consistent with the results of existing studies (Lieberman et al., Reference Lieberman, Marriott, Williams, Judelson, Glickman, Geiselman, Dotson and Mahoney2015). As a result of regular use of these products without supervision of a healthcare professional, undesirable effects such as overdose, medication errors, adverse effects, and interactions with other drugs were reported (Ruiz, Reference Ruiz2010). For example, some studies stated excessive intake of protein powder, which was among the most commonly used non-pharmaceutical products in our study (Sánchez Oliver et al., Reference Sánchez Oliver, Miranda León and Guerra-Hernández2011). Uncontrolled use of these products was reported to lead unwanted outcomes such as deteriorated kidney and liver functions, musculoskeletal diseases, and rapid progression of coronary heart disease (Delimaris, Reference Delimaris2013). It could be assumed that limiting the use of these products to the situations under the supervision of healthcare professionals might reduce the aforementioned risks.
Our findings should be interpreted with its limitations. Firstly, convenience sampling, which was used in the study, is not without flaws. As a non-probability sampling method, this could affect the generalizability of the results negatively, and might lead to biases emerging from the subjects’ tendencies that might differ from the population, for example, those opted to participate might have been more inclined to be aware of the principles of healthy lifestyle compared to a random individual. It should be taken into account that the answers of the participants, regarding their physical activity and eating habits etc., might not reflect their behavior in real life. Hunger/satiety state of the individuals, as well as recent changes in habits that may affect BG and TC values, were not questioned prior to clinical measurements. Also, TC values lower than 150 mg/dl were below the threshold of detection for the device. Thus, absolute numerical values of these individuals could not be obtained, and those results had to be excluded from parametric analyses. In addition, health-related field students participating in the study might have increased overall health literacy and CV knowledge scores, so that might have led to a bias. Finally, no detailed inquiries have been made regarding the use of illegal products such as illicit drugs. None of the participants reported such use as an answer to the question related to drug/non-pharmaceutical products. Thus, a lack of more detailed questioning of any illicit drug use might also be regarded as a limitation of the study.
In conclusion, this study revealed that whilst being more common in males, one out of every three university students had at least one CVR that might negatively affect their overall health. Despite the presence of CVR appearing not to be directly related to health literacy of participants, family income, and parent education levels, the prevalence of CV problems and risks being that of the general population seems concerning. Furthermore, the participants seem to perform below expected levels in terms of nutrition and physical activity, and unhealthy eating habits were more common among CV(+) subjects. These findings point out that in terms of preventive medicine, extensive additional measures are needed to encourage young individuals, especially the ones in at-risk groups, for healthy nutritional and physical activity habits. The outputs of the study could be regarded as examples to similar interventions that might be initiated in other campuses and universities to increase awareness of the students regarding healthy life, which has an emerging importance.
Acknowledgements
We thank to Prof. Sibel Sakarya, Prof. Oguzhan Deyneli, Prof. Hakki Arikan, Songul Cecen, and Ismail Sahin for their contributions to the study design and data collection and to Marmara University Rectorate, Marmara University Health, Sports and Social Affairs Office and student clubs, Cyclists Association, Turkish Heart Foundation, Kadikoy and Uskudar Municipalities for their valuable contributions during and after the project phase.
Parts of this study were presented internationally at the 24th WONCA Europe Conference (26–29 June 2019, Bratislava, Slovakia) as a poster, and nationally at 13th Family Medicine Autumn School (16–20 October 2019, Antalya, Turkey), 18th National Family Medicine Congress (31 October–2 November 2019, Ankara, Turkey), and 25th National Pharmacology Congress (4–7 November 2019, Izmir, Turkey) as oral presentations.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1463423621000578
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflict(s) of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the Helsinki Declaration, as revised in 2013. Written informed consent was obtained from all subjects.







