Introduction
Assistive Technology (AT) is the term used to describe the large collection of services and devices that aid people to maintain or improve function and independence in daily life (World Health Organization [WHO], 2018). An integrated approach to AT, including both hard and soft AT (Cook et al., Reference Cook, Polgar and Encarnação2020; Waldron & Layton, Reference Waldron and Layton2008), results in optimal AT outcomes (de Jonge et al., Reference de Jonge, Hoyle, Layton, Verdonck, Federici and Scherer2017). Hard AT relates to the physical devices, such as wheelchairs, prosthetics, walking aids and eating utensils. Soft AT, in comparison, refers to the systems that support individuals to use these assistive technologies effectively, including collaborative assessment, trialling devices and equipment, customisation of the AT, training, as well as maintenance support, repairs and follow-up (de Jonge et al., Reference de Jonge, Hoyle, Layton, Verdonck, Federici and Scherer2017). Soft AT is particularly important as the complexity of the hard AT increases.
De Jonge et al. (Reference de Jonge, Hoyle, Layton, Verdonck, Federici and Scherer2017) outlines four levels of AT complexity based on previous literature and Australian policy (Hammel & Angelo, Reference Hammel and Angelo1996; Summers & Walker, Reference Summers and Walker2013; National Disability Insurance Agency [NDIA], n.d., as cited in de Jonge et al., Reference de Jonge, Hoyle, Layton, Verdonck, Federici and Scherer2017). Each level increases in complexity (both technology and operational requirements), level of risk to the user, accessibility and cost. Level 1 refers to mass produced consumer products (e.g., non-slip mats, modified cutlery, simple adapted computer hardware) that are simple to use, low-cost and easily accessible. Level 2 includes off-the-shelf, adjustable AT (e.g., standard wheelchair, rails, off-the-shelf orthotics) that is readily accessible but has some degree of risk. Level 3 refers to complex AT solutions (e.g., power wheelchairs, hoists, speech generation devices) which has moderate risk associated with the consideration for appropriate selection and education for use. Lastly, level 4 highlights customised solutions (e.g., power wheelchairs with specialised controls, interfaces) which requires expert advice for selection and training, therefore higher risk for the user.
Provision of appropriate AT supports the inclusion and participation of people living with disabilities in diverse aspects of society (WHO, 2018). A good fit between a person and AT can result in significant benefits for both the individual and society (Sherry et al., Reference Sherry, Ravneberg and Söderström2017). Individually, people can experience benefits related to activity participation, health and well-being. At a societal level, successful AT provision and allocation can reduce the need for formal and informal assistance and services. Globally, access to AT is often limited by high costs, lack of awareness, availability, trained personnel, policy and financing (WHO, 2018). While there are significant benefits to appropriate AT provision, AT can also be a hinderance resulting in low uptake or technology abandonment (Desmond et al., Reference Desmond, Layton, Bentley, Boot, Borg, Dhungana and Scherer2018; Sherry et al., Reference Sherry, Ravneberg and Söderström2017). The appropriate provision of AT is dependent on adequate training and knowledge by the service provider, coupled with the use of a person-centred multistep process to support receipt of appropriate AT.
A report conducted by the National People with Disabilities and Carers Council (2009) highlighted the difficulties that people with disability in Australia have in accessing appropriate AT essential for their daily activities and community participation. Access was impacted by long wait times, not just for the devices themselves, but also the services that support AT provision, for example long wait times for an occupational therapy assessment. People with disability reported having to personally fund AT, often at considerable expense, and if they could not afford the technology they would simply have to go without. When AT was available, it was not always suitable, with people reporting issues with fit, adjustment, modifications and repairs.
A paradigm shift has occurred within Australia, placing emphasis on a human rights-based approach to ensure services are matched appropriately to individual aspirations, needs and preferences (Pearson & Ridley, Reference Pearson and Ridley2017). There have been significant reforms and legislative processes implemented to improve the overall services that are provided to people with disability in Australia (Steel, Reference Steel2020), including the introduction of national schemes like the National Disability Insurance Scheme (NDIS; (NDIA, 2021) and state injury insurance schemes (such as: National Injury Insurance Scheme Queensland [NIISQ] in Queensland ([National Injury Insurance Agency Queensland, 2022]; iCare in New South Wales; [Insurance and Care NSW, 2022]). The state injury insurance schemes provide lifetime support for individuals with catastrophic injuries following motor vehicle accidents including people with traumatic brain injury and spinal cord injury. The complexity of needs following these injuries can mean that AT recipients are supported by both national (e.g., NDIS) and state-based (e.g., NIISQ) schemes. Therefore, AT advisors, suppliers and recipients are now operating within variable funding contexts, with a multitude of policies and legislation, and a fast-paced and rapidly changing AT environment. As a result, there is increased potential for pressure points in the systems that can influence AT process and outcomes.
Historically, programmes and schemes that manage disability services have been framed and evaluated in terms of value for money (Layton, Reference Layton2015; Steel, Reference Steel2019). This economic focus can detract from person-centred practices and demonstrates differing values and views between policy and research. Additionally, programmes and schemes that manage disability services have often been under-resourced, meaning that even when the policy values aligned with best practice, good AT outcomes were often never realised. People with life-long disability living in the state of Queensland in Australia may receive AT solutions managed by a range of organisations governed by either national or state-based Acts and Legislations. The inability to access suitable AT creates significant barriers to independence, participation in community, and increases the burden on the person with disability, their families and key supporters, negatively impacting quality of life. In response to the recent changes within the assistive technology sector, this project was designed to examine current practices and needs regarding assistive technology provision throughout Queensland from the perspectives of all stakeholders.
Current study
The objective of the Growing Assistive Technology Solutions in Queensland project was to conduct a needs assessment across multiple project phases with key stakeholders to establish the ‘Normative’, ‘Comparative’, ‘Expressed’ and ‘Felt’ needs for AT provision (Bradshaw, Reference Bradshaw1974; Eagar et al., Reference Eagar, Lyn and Garrett2001). In this study, normative and comparative need were established with the organisations that manage AT provision across Queensland and Australia. Additional studies explored expressed need from the perspective of the AT advisors and suppliers and felt need from the perspectives of the AT recipients. This paper reports the phase of the needs assessment that aimed to establish the normative and comparative needs of the assistive technology sector. For the purposes of this study normative need referred to services within Queensland and comparative need referred to services available in other Australian states. The aim was to examine the current practices of regulatory bodies, agencies and schemes that manage AT provision for people living with disability in Australia.
Method
Design
This sequential mixed methods study included an audit of publicly available documents and information provided on regulatory body, agency or scheme websites and semi-structured interviews with representatives from agencies and schemes.
Participants
Regulatory bodies, agencies and schemes that manage AT provision in Australia were identified by the research team (Fig. 1) for the website audit. Regulatory bodies were included in the audit because of their role in regulating schemes that manage AT provision. The agency and schemes were then contacted and asked to identify a representative who was experienced in the organisation’s policies, procedures and experiences with AT provision to participate in an interview. Interviews were completed with representatives from most of the agencies and schemes. One organisation did not respond to this request and is not represented in the qualitative data. The regulatory bodies were not contacted further for interviews.
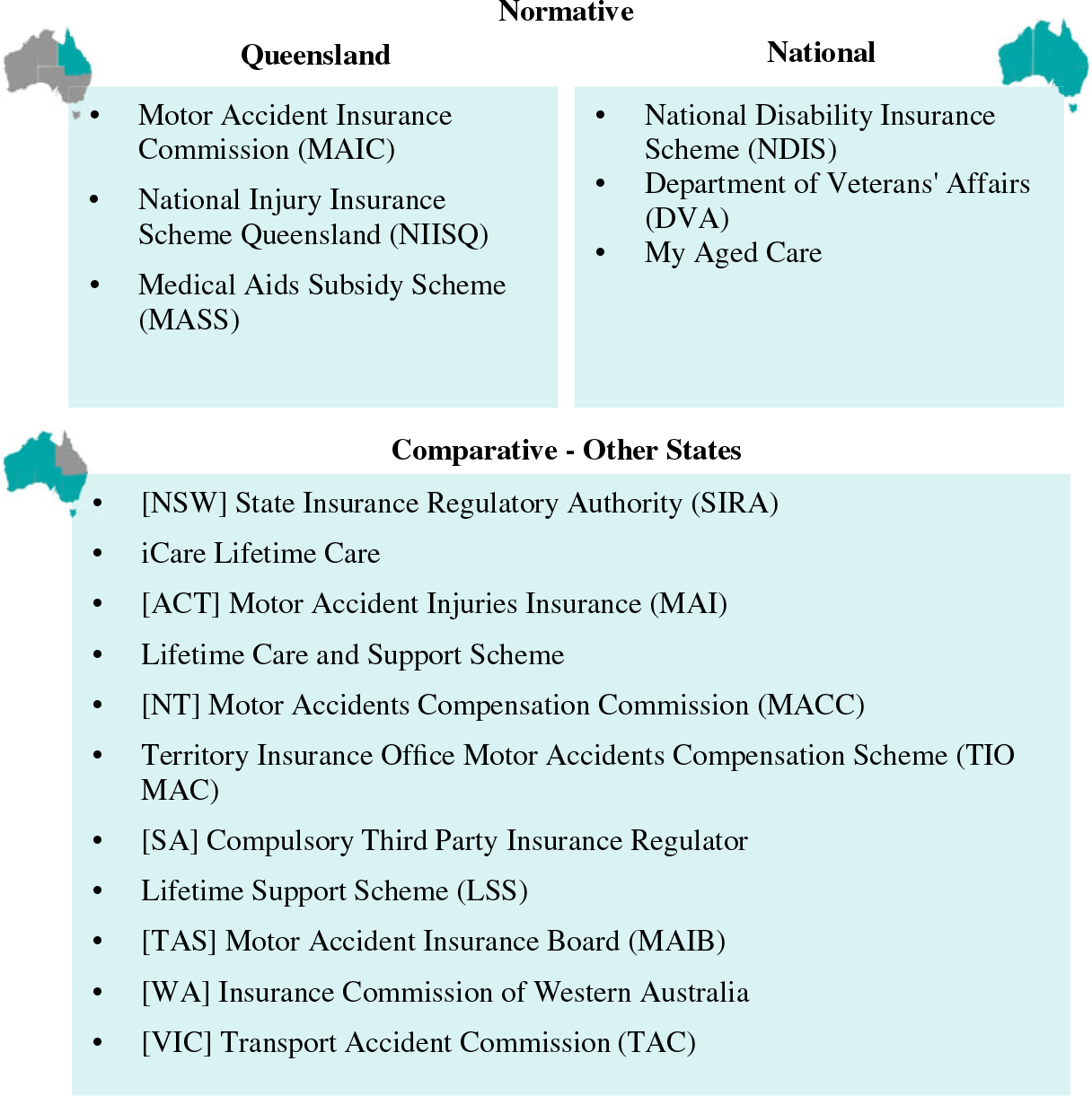
Figure 1. Regulatory bodies, funding agencies and schemes included in audit. Note. NSW = New South Wales; ACT = Australian Capital Territory; NT = Northern Territory; SA = South Australia; TAS = Tasmania; WA = Western Australia; VIC = Victoria.
Data collection tools
Audit: The audit tool was designed to extract information from the publicly available documentation and information provided on websites of each regulatory body, agency or scheme to explore the current practices and standards of AT provision. The tool was purpose designed to reflect the type of information available and the detail of information available specific to AT. The audit tool included 12 items that facilitated collection of descriptive information such as: information available about the AT provision process; types and numbers of webpages or documents available; information on available AT; level of funding available; etc. The full audit tool is available in Appendix A.
Interview: The semi-structured interviews were designed to further explore the current practices and expected levels of service relevant to AT provision and covered the following topics: demographic questions, the AT provision process, overview of AT provision, budget, barriers/challenges and other comments not previously covered. A detailed outline of interview probes can be found in Appendix B. When indicated within the interview, additional prompts and probes were used to explore topics and information raised by the interviewee or to explore the findings of the audit.
Procedure
Ethical clearance was obtained from the Griffith University Human Research Ethics Committee [GU 2021/925].
Audit: One researcher [CH] independently collated the publicly available documentation (i.e., brochures, reports, guidelines and webpages) from each agency or scheme for later data extraction. Information was then independently extracted from the available documentation by two members [CH, AD] of the research team.
Interview: The purpose of the interview was to explore the processes, standards and expected levels of service regarding AT provision. Members of the research team phoned the agencies and schemes requesting the identification of the individual who was best placed to discuss the organisations’ practices and experiences with AT provision. The identified individuals were contacted and invited via email to participate in a semi-structured interview. If they were interested in participating, they contacted a member of the research team who then organised a time to meet via Microsoft Teams where the interview was video/audio-recorded and later transcribed verbatim. All respondents provided written consent prior to the interviews. Respondents were assured of their anonymity and that all data would be de-identified and kept confidential.
Data analysis
All data were uploaded and stored in the online secure Research Storage Space at Griffith University. The audit data were collated, and a summative content analysis (Hsieh & Shannon, Reference Hsieh and Shannon2005) identified and quantified the presence of key concepts and information in the documents. It was the intent of the study to include National data with the normative findings (as indicated in Fig. 1). However, it became apparent during the process of summarising the audit data that it was misrepresentative to incorporate the national data into the normative findings only. National data are relevant to all Australian states and therefore a decision was made to report audit data as National, normative (Queensland-based) and comparative (other Australian States). The descriptive analysis was completed by LG and checked by CH.
Three researchers (LG, AD, TH) read the interviews and completed initial coding using conventional content analysis (Hsieh & Shannon, Reference Hsieh and Shannon2005). Each researcher independently coded the interviews and met to discuss and refine the identified codes. LG completed the analysis, applying initial codes to the data, allowing new codes to develop and collating the codes into categories. The team met to discuss any emergent codes and the categories and AD cross-checked the codes and categories against the transcripts, with no changes required. Finally, the categories were summarised into the final themes, the descriptions of the themes were discussed (LG, TH, AD] and finalised with no changes required.
Results
Seventeen websites were audited, representative of national (n = 3), normative (n = 3) and comparative need (n = 11; Fig. 1). Seven were insurance commissions who regulate the provision of support for people with minor injuries from motor vehicle accidents and six were schemes that manage the provision of care and support following catastrophic injuries from motor vehicle accidents. The 17 websites ranged in quantity and depth of information, displaying between 1 and 15 webpages in total (Mdn = 4, M = 5.8), 0 and 14 consumer-specific pages or brochures (Mdn = 3, M = 3.9), and between 1 and 35 other documents (Mdn = 2, M = 5.59) such as guidelines, forms, annual reports, acts, regulations and standards. Figure 2 highlights that the normative agencies provided information predominantly from the advisor perspective while national and some comparative agencies provided more information from the participant perspective.
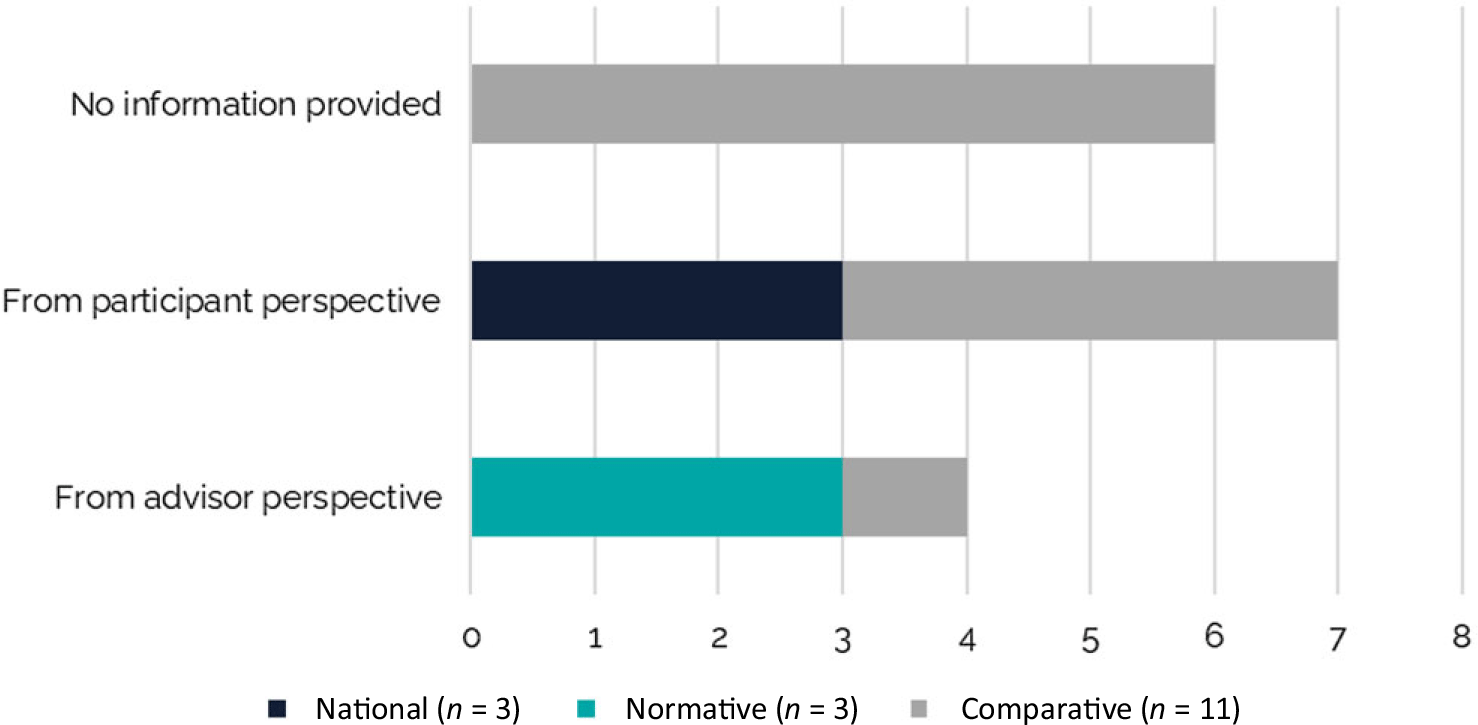
Figure 2. Number of websites with information about Assistive Technology process.
The range and level of detail provided about the funding available for AT was variable (Fig. 3) and key areas reported were the availability of AT for driving and transport, design and building for access and safety, and mobility (Fig. 4).
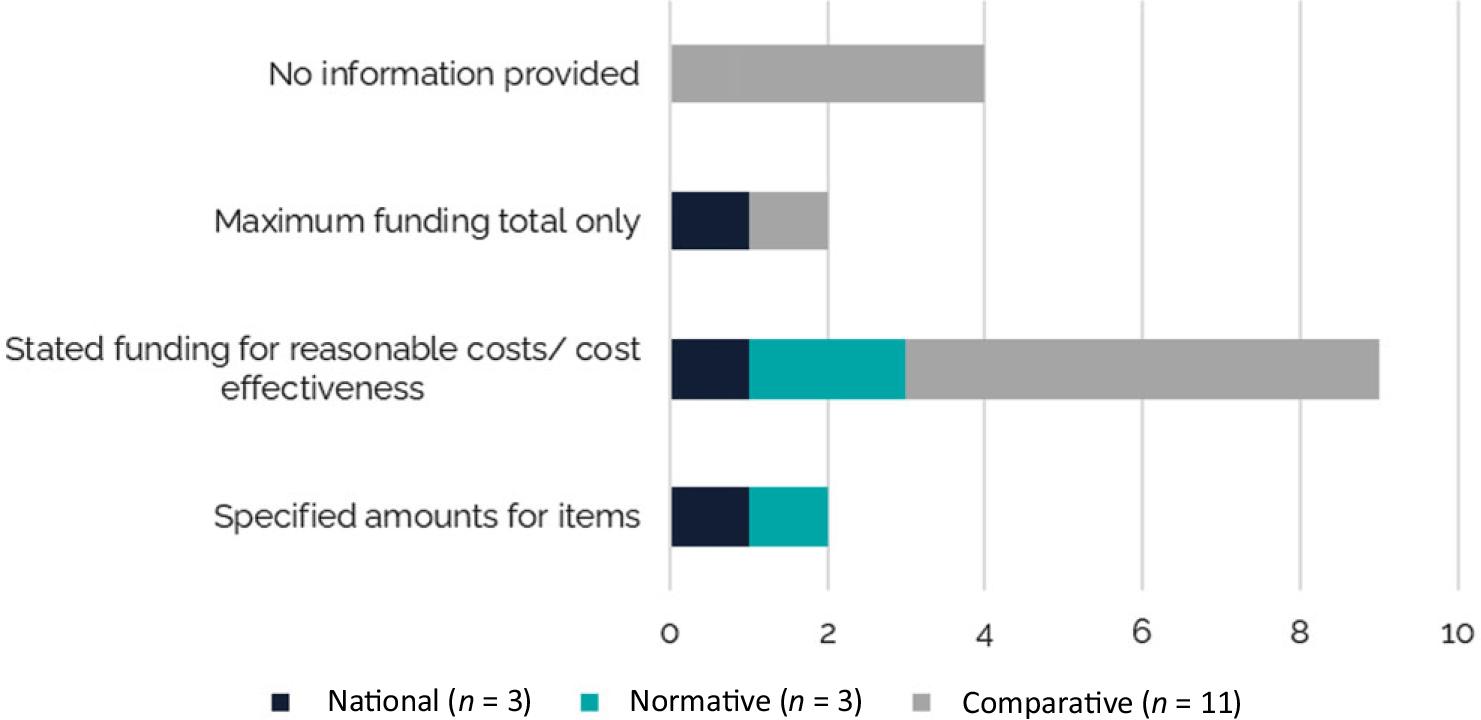
Figure 3. Number of websites with information about funding available.
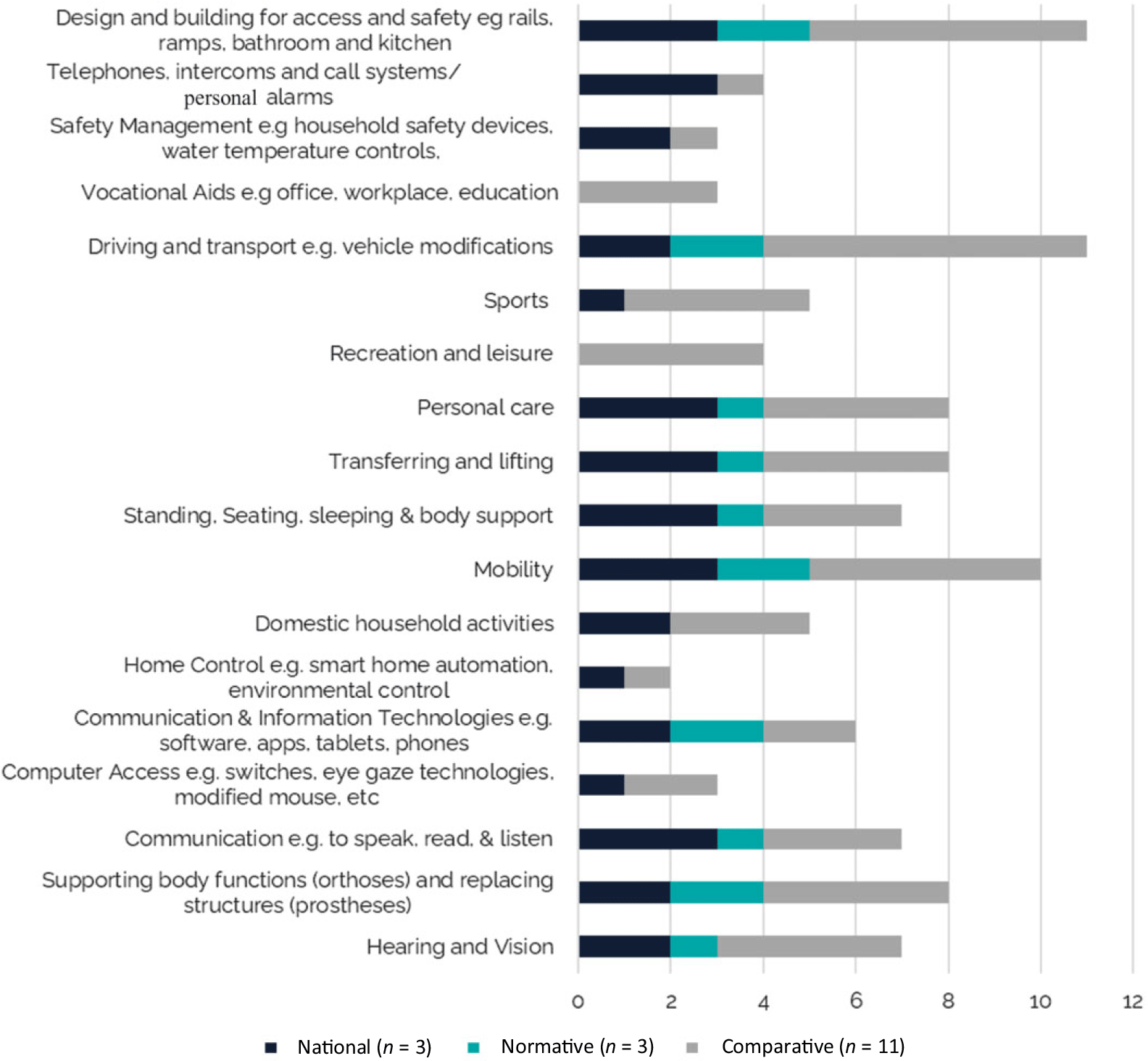
Figure 4. Number of websites with information about specific Assistive Technology solutions/purposes.
Interview findings
Operationalising the legislation
Respondents spoke about the ‘the Act’ as ‘[something] that governs… underpins everything that we do’ (P09). There were additional layers for the agencies and schemes supported by the relevant motor accident injury or insurance acts which led to ‘quite a lot of policies that we work along with … we actually run under [a motor accident insurance body], so we’ve also got to be running under their Acts and regulations in unison’. (P01). Each scheme developed guidelines, operating procedures and decision-making frameworks to operationalise the legislative requirements into decisions about funding. The audit identified limited information on websites regarding these guidelines and the respondents confirmed that many of these were internal-facing and not visible to the AT advisors or recipients. One respondent described that ‘there’s some information on the website…But it’s pretty vague…if needed, we’ll engage an allied health professional to look at your AT needs and work with you to work out what the best option is’. (P02)
The challenges to this approach were articulated clearly when one respondent stated
‘…people are not necessarily privy to our legislative requirements which are applied to every decision around funding. So, from a therapist’s point of view, in terms of what a client needs, they may not view it in terms of our legislative requirements, so then that’s when it becomes really tricky. And it’s very hard for them to understand why we’ll fund some items and not others’. (P09)
In response, another scheme was ‘in the process of writing guidelines that will be externally- and internally-facing because it’s probably the part that we haven’t had before; something that’s externally facing’. (P05)
Eligibility and entry requirements were linked to the purpose of each scheme such as: lifetime care available for people ‘[following a] catastrophic injury, due to a workplace injury or motor vehicle accident injury’ (P02), or support for ‘people over 65 or over 50 if they are Aboriginal or Torres Strait Islander…living at home’ (P04). Some had additional administrative eligibility criteria such as holding a concession, seniors, or defence-related card. The phrase ‘permanent and stabilised’ (P01) was common and a scheme for people with a newly acquired, serious injury explained that the first 2 years within the scheme was an interim period: ‘they come in for two years and we work with them to meet their goals and fund all that treatment care and support. And at the end of that 2 years, they get reassessed with exactly the same assessments. And if they still qualify to … they stay in for life’. (P05)
Internal AT processes
The level of risk associated with the AT often influenced the number of approvals required within an application process. Some considered that if the AT was low-risk to the participant such as ‘…a shower chair. A reacher. A four-wheel walker’ (P02), they could be ordered by the health professional. In comparison, AT considered medium- to high-risk required pre-approval and additional layers of approval within organisations.
‘They send through an aids and equipment request, which is about a three or four-page document, that’s got all of the outcomes of trials and all the other things they’ve had to think of, like the pros and cons against the AT…. Certainly, we’ve got certain policies and procedures in turning around, I suppose, review and approvals. We have not just the technical specialists and myself [who]will review all of these … At certain times where there is quite a significant cost we might have the legal tech as well, as the actual manager of the claims, review the actual request’. (P10)
This process could be delayed if the agency did not receive ‘information that we actually need to be able to make a decision on some of the items that they’ve requested. In which case we’ll go back to the provider and go can you please provide more information. So that can be a barrier, cause delays for some things’. (P09) For many schemes, decisions were made on a case-by-case basis and, although it was stressed that the health professionals were the people that agencies were ‘looking to provide us with the recommendations and the justification’ (P06), there was still a sense that the scheme was the final decision-maker.
‘They’re not the decision makers, so we can override those if we think there are other things at play…and we need to think of, well, in the longer term, would this provide better value for money for [the scheme], and would this have that durability for that longer term’. (P07)
Reasonable and necessary
Decisions were reportedly made based on a ‘clinical’ need and how reasonable the request was. As indicated in the previous theme, this would often be reviewed within the agency.
‘…it’s going to be something that helps to improve the independence of that person, the social connectedness of that person, the safety and the clinical needs. When we do get things that come in, and it’s probably more around your one-off items…that are maybe of higher cost, or that needs prior approval, those will all go through our adviser services, I suppose, to determine the clinical appropriateness of the request’. (P07)
The agencies differed with respect to which aspects of life were covered, with some agencies only considering AT for life within the home and some agencies not including AT for leisure activities, indicating that the person would need to access this from another agency. Questions were raised about equity, querying how many leisure activities were reasonable and if they should be existing or new pursuits. One agency articulated reasonable in terms of the individual and their interests.
‘…what would your life have looked like pre-accident. Without those injuries what would that potentially look like. So I think that’s where it comes back to where we have those discussions, we get right into the nuts and bolts of what that space looks like, and what’s important for a person, and still got to buy what’s reasonable’. (P06)
AT was commonly supplied for items related to personal care, mobility and continence. Other everyday technologies were often discussed as a ‘case-by-case basis’ with less clear decision-making processes. Insurance schemes identified that it was essential to identify that the need for the device was linked to injury and this was not always simple. I case of continuous positive airway pressure (CPAP) machines for sleep apnoea were provided as one example. AT was provided to support activities in the kitchen but kitchen appliances such as Thermomix™ or KitchenAid™ would raise considerations about how reasonable and necessary they were. Smart phones and watches were highlighted as ‘an interesting field to try and nut [work] out’ (P09) such as deciding if the need to use the device as an alarm was a reasonable request.
‘And the other element is, when does something become a mainstream item? Because generally, at the [scheme], household, mainstream items are something we wouldn’t fund. So that’s where it can get a bit tricky’. (P08)
There were differences in how schemes supported activities related to work or education, with some stating that they would not provide equipment that would be considered a general requirement but would supply specialist equipment required due to person’s individual need. Alternatively, another scheme would ‘fund to support a [person] to go to work, but not at work’ (P03) and that it was the responsibility of the employer to provide the required equipment.
Risks in the AT pathway
The knowledge, skill and availability of health professionals was often referred to as a risk. Clinical expertise takes time to develop and there was recognition of the risk of the influx of recent graduates into the sector for the graduates, the recipients and the schemes.
‘I think there is some openness … from the professions, but obviously some – always had this wonderful belief that their people graduated and could do anything, they’re starting to give that the big flick with the concept of consumer law responsibilities and professional responsibilities’. (P03)
There was an identified need for upskilling AT assessors and advisors to ensure that they were ‘clinicians with specialist skills for prescription who have experience with … the emerging technology, and the higher spec stuff’. (P02) A lack of specialists who could confidently and competently offer high-end technology led to lower than anticipated provision of this AT to recipients:
‘But I think a lot of the time it can be limited by the clinician’s knowledge of what’s available and how tech-savvy they are…. I guess their knowledge and how they keep that up-to-date can vary, geographically as well as in terms of their experience as well’. (P02)
There were also challenges identified where demand for service was greater than the available health professionals, and although this was often related to rural or regional areas, there was mention of one Australian capital city where waitlists were up to 6 months long.
‘And like [capital city], for example, there was a real lack of providers in that area…and I mean naturally because where the volume is so high we have some, like I say, delays, and we had people that we’re not able to provide – like we’re not able to meet everyone’s needs’. (P04)
Getting the right specialists and professions around a person to identify what they might need was particularly problematic for the larger states and led to disadvantage. ‘…availability of the right skilled assessor and availability of trial equipment would probably be the biggest barriers’. (P05) Limited capacity to trial equipment was problematic with shipping costs high when a person could not easily access a supplier to trial the item. State-based schemes flew clinicians with specialist skills into remote or rural communities to address the inequity of services for people who did not live near major areas. However, the challenges of access to trial equipment remained.
‘…needs more specialist therapists in regional and remote areas…how [do] we upskill those people and how do we get trial equipment out to those people? Because it’s a real – it’s such a big state that you’re at an advantage if you have an accident and a disability and you live near … [state capital city and surrounds]. Anywhere else you’re disadvantaged… especially [with] the complex AT’. (P05)
There were benefits recognised of working with clinicians who were familiar with the scheme and with whom there were strong working relationships.
‘…we can pick up the phone and we can say, hey, we’ve got this situation going on with this person. We’re a bit concerned about them and whether they’re okay at home. Can you duck out and do an assessment? And I tell you what, like I said, they tend to make it a priority. Which we’re very fortunate’. (P06)
Conversely, this led to concerns, for it was recognised that ‘we’ve got a few key clinicians that we use on a regular basis, in those [regional] areas. But for some areas, like [regional area], if she retires, we’re stuffed’. (P02)
Finally, the relationship between clinicians and suppliers was an identified determinant for the effectiveness of the process with agencies indicating that when clinicians worked with just the one supplier, this could limit the suitability and range of AT offered to individual recipients.
Discussion
This project reports the findings of the normative and comparative needs analysis of agencies and schemes that support AT provision for people around Australia. This was the first study to comprehensively explore AT practices with the diverse agencies and schemes around Australia and the findings indicate the commonalities in need between agencies and schemes in Queensland, and the comparative agencies and schemes around Australia. There are four points that will be discussed further: the information publicly available about the AT process and decision-making; the phrase ‘reasonable and necessary’; the availability, knowledge and skills of health professionals; and the access to trial equipment.
AT recipients must receive devices and supports that are appropriate for their individual circumstances and help them to achieve their goals for independence, community participation and benefit overall quality of life (Scherer, Reference Scherer2002). Inadequate or incorrect AT solutions can negatively impact these domains or lead to abandonment of the AT (Ranada & Lindström, Reference Ranada and Lidström2019). Abandonment of AT or negative outcomes are significant risks for the agencies, particularly when additional AT assessments are required and additional AT devices funded, increasing the overall economic cost. The development and implementation of policies, and procedures that adhere to the legislation can support best practice AT provision. However, the audit of the websites indicated that there was very little publicly available information regarding how legislation, policies and procedures informed their decision-making. Equally, it cannot be ignored that there is a ‘value for money’ element to the decision-making (Layton, Reference Layton2015). As recognised by some of the respondents, the process can be difficult or delayed when the identified clinical need and request was not consistent with the guidelines or policies of the agency or scheme. Opportunities exist to enhance publicly available information to prevent this outcome.
The information obtained on the websites about AT ranged from comprehensive, with individual items named, through to general statements. AT solutions that were frequently mentioned on websites included AT for mobility, transferring and personal care; design and building for access and safety; driving and transport; and orthoses and prostheses. In contrast, the following AT solutions were named by three or less websites: AT solutions such as home control, computer access, vocational aids and safety management. Home control is one example of an area of AT where new technologies are easier and more accessible (e.g., control from applications on smart phones). The internet has changed the health and disability landscape enabling people to become active consumers of information (McMullan, Reference McMullan2006). Accordingly, the information on websites could influence (positively or negatively) recipient and advisor knowledge and expectations regarding the AT solutions available to them. Overall, an exploration with key stakeholders from agencies, advisors and recipients could explore ‘what’ and ‘how’ information about policies, guidelines and supported AT solutions could be available publicly.
Although not universally applied by all schemes, the terms reasonable and necessary were often used by the respondents. ‘Reasonable and necessary’ was introduced in 1965 by Medicare in the USA and has presented an enduring challenge to define (Neumann & Chambers, Reference Neumann and Chambers2012). Indeed, recent attempts by the Medicare in the USA to redefine ‘reasonable and necessary’ based on commercial insurers has raised concerns about the integrity of the decision-making process when there is limited information to the public about how decisions are made (Padmanabhan, Reference Padmanabhan2021). The findings of the present study suggest similar challenges within the Australian disability context, which is further complicated with the varied uptake, application and operationalisation of the terms across agencies. It appears that low-risk AT (levels 1 and 2), which is often supplied without additional review or approval, is considered reasonable and necessary. This process, coupled with the messaging on websites and the lack of clarity regarding decision-making when additional approval is required, may lead both advisor and recipient to consider it prudent to prioritise and apply for AT solutions that are mass produced (level 1) or off-the-shelf (level 2).
Terminology such as aids or equipment within policy documents can imply a heavy focus on AT that are designed specifically for people with disability (Steel, Reference Steel2020). Consequently, mainstream devices that could be economically effective and less socially stigmatising may not be supported as an AT solution (Steel, Reference Steel2020). Our findings suggest that there is ambiguity regarding the provision of AT solutions considered mainstream technology. In particular, the use of smart devices and kitchen appliances were highlighted as challenging areas for the agencies and schemes. Steel et al. (Reference Steel, Buchanan, Layron and Wilson2017) advocated that AT solutions should include both specialist and mainstream products and services. Mainstream products are acceptable and easily accessible to people living with a disability. When there is good fit to the individual and their environment, mainstream products can offer solutions that support the individual to achieve their goals for engagement in a range of everyday activities. The findings draw attention to the need for further investigation and clarity regarding the guidelines for these mainstream AT solutions.
Finally, health professionals’ knowledge and skills, and access to trial equipment were identified risks in the AT process. There was an identified need to upskill and increase the number of advisors with the requisite skills to ensure that there adequate geographical coverage. Approaches mooted to address this need include the development of training programmes, ‘train the trainer’ schemes to support existing AT advisors to train and upskill others, or the development of ‘independent centres of expertise’ (de Witte et al., Reference de Witte, Steel, Gupta, Delgado Ramos and Roentgen2018, p 469). The high-risk, level 3 and 4, AT requiring customisation and specialist training was identified as a particular area of unmet need for all geographical areas. However, the provision of services to people living outside of major metropolitan areas in Australia was highlighted. Reduced accessibility to healthcare professionals in regional and rural areas is well documented (Australian Institute of Health & Welfare, 2022), and thus these findings are not unique. The complex nature of AT provision which requires a specialist team of advisors, access to the AT to trial and access to a specialist who can customise the AT can have significant implications for costs when a ‘fly in, fly out’ service is required. Opportunities to explore alternate models such as telehealth or using other technology to connect all required specialists with the individual could be explored. However, the issue of access to the AT solution for trial may remain problematic.
Limitations
This study has explored the area of AT from one perspective only, that is the regulatory bodies, agencies and schemes. To ensure that a comprehensive review of the sector is completed, future studies by this team explore the perspective from AT advisors and recipients, and suppliers. WorkCover is a key stakeholder for the support of the worker who is injured temporarily or permanently and was not included in the study. It was considered that the unique focus on the injured worker, governed by a specific set of Acts and Legislation, was not consistent with the focus of this study. It is unclear if their inclusion would have altered the findings.
Conclusions
The regulatory bodies, agencies and schemes that support the provision of AT maintain an important role in the health and well-being of people living in Australia with disability. AT development, from low-tech aides through to complex systems, is a fast-paced and rapidly changing market. This leads to a strong need to ensure access to high-quality services to build capability, not only for advisors and AT recipients, but also agencies to ensure that the pathways to acquisition of AT is appropriate, and that the uptake and integration of AT is successful for people living with disability. This study has identified opportunities for review of information available on websites, highlighted ambiguity in the operationalisation of the terms ‘reasonable and necessary’ and identified the risks for the AT sector based on variable health professional availability, knowledge and skills, and limited accessibility to trial AT. These factors can impact best practice and should be explored further from the perspective of AT advisors, participants and suppliers.
Acknowledgements
This project could not have occurred without the generous contributions of the advisory group: Bridget Manning, Lloyd Walker, Soo Oh, Frances Porter, Genevieve Lee, Adam Schickerling, Alejandro Melendez-Calderon, Natasha Layton (OT Australia), Gaenor Walker, Michelle Owens, Hayden Boyd, Dee Hoffman, and the Statewide Rehabilitation Clinical Network.
Funding support
This work was supported by funding from the National Injury Insurance Scheme Queensland.
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Authorship statement
All authors contributed to conceptualisation and design of the study. Data were collected by CH, AD, TH, MB and analysed by CH, LG, CS, AD, TH. The manuscript preparation was conducted by CH & LG. Editing and revision of the manuscript was completed by all members of the research team.
Appendices
Appendix A. Audit Tool
-
1. Funding Agency/Scheme Name
-
2. State/Territory
-
3. Document Type/Title (i.e., webpage, consumer brochure, guidelines, etc.)
-
4. Uniform Resource Locator (URL)
-
5. What is the AT provision process?
-
6. What are the eligibility criteria?
-
7. What AT is available?
-
8. Maximum funding level
-
9. Most common types of AT
-
10. Is there training available for the providers?
-
11. Is there an information sheet for consumers?
-
12. Are there links to other sites (i.e., funder linking to insurance scheme)?
Appendix B: Service Provider Interview Probes
Demographic Questions
-
1. Please state your employer
-
2. What is your professional background/experience?
-
3. How long have you been in your role?
AT Provision Process
-
1. What is the process for obtaining/providing AT?
-
2. What does the patient journey look like?
-
3. Does the organisation have any relevant policies/procedure for AT provision?
-
4. What guides decisions about high level tech provision?
AT Overview
-
1. Who is generally accessing your service (i.e., TBI, SCI, Stroke, etc.)?
-
2. What AT is available?
-
3. What types of AT are commonly prescribed?
-
4. Low- versus high-tech AT
-
5. What are the over prescribed/under prescribed areas of AT?
-
6. Is the core business providing AT for inside or outside of the home?
Budget
-
1. What is your organisation’s rough AT budget?
-
2. How much of this AT budget is used?
-
3. What portion of this budget is used on low- versus high-tech AT?
-
4. Is funding provided for discretionary/non-discretionary activities?
Barriers/Challenges
-
1. What are the barriers to AT provision (i.e., knowledge, need, want, etc.)?
-
2. From your perspective, where are the challenges?
-
3. Where is the process working/not working?
Other
-
1. Is there anything else you would like to share with us regarding your organisation’s AT procedure, policies, or challenges?






