1. Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a neurobehavioral developmental disorder, characterized by the symptoms of inattention and/or hyperactivity/impulsiveness. The worldwide prevalence of ADHD in children has been estimated at about 5% with a higher prevalence among boys Reference Polanczyk, de Lima, Horta, Biederman and Rohde[1]. For many children, ADHD symptoms persist into adulthood with long-term adverse outcomes such as lower educational attainment and income, and more emotional and social problems Reference Hechtman, Swanson, Sibley, Stehli, Owens and Mitchell[2]. Given that the typical features of ADHD include an inability to inhibit impulses and self-regulate, increased reward and sensation seeking behaviour, as well as poor social skills Reference Sonuga-Barke, Bitsakou and Thompson[3], it is not surprising that the disorder has been linked to a number of risk taking behaviours, such as drug and alcohol use, conduct problems [4,5] and risky sexual behaviour (RSB) Reference Nylander, Tindberg and Fernell[5]. However, although there has been an abundance of studies on the link between ADHD symptoms and other types of risk taking behaviour, research on the association with RSB has been limited. In the scientific literature, RSB commonly refers to unprotected sex, multiple sex partners, and hazardous sexual activity such as sex while intoxicated Reference Hoyle, Fejfar and Miller[6] and is regarded as a major public health problem during adolescence [7,8]. The handful of previous studies on the association between ADHD symptoms and RSB have been mostly undertaken among adults [9–12] especially males [9,13]. The research has indicated that ADHD is associated with early sexual debut, multiple sexual partners and more partner pregnancies [9,10,13,14].
Against this backdrop it has been suggested that not only is there a need for more studies on this association in adolescents, but also, for a greater focus to be placed on the dimensional aspects of ADHD, where both symptom clusters – inattention and hyperactivity/impulsivity – are investigated separately Reference Sarver, McCart, Sheidow and Letourneau[12]. In particular, impulsivity has been proposed as a likely causal pathway to RSB, with a recent review finding a small but significant association between impulsivity and RSB Reference Dir, Coskunpinar and Cyders[7]. Co-morbid conduct problems might also have a causal role in the emergence of RSB Reference Sarver, McCart, Sheidow and Letourneau[12]. However, the few studies to date that have included conduct problems as a covariate, have produced conflicting results. Some reports suggest that hyperactivity is associated with early sexual intercourse Reference Barkley, Fischer, Smallish and Fletcher[9] and that ADHD symptoms are associated with early sexual intercourse, more sexual partners, more casual sex and more partner pregnancies Reference Flory, Molina, Pelham, Gnagy and Smith[13] independently of conduct problems. Other research found an association with early sexual intercourse only when hyperactivity/inattention symptoms occurred in combination with conduct problems Reference Galera, Messiah, Melchior, Chastang, Encrenaz and Lagarde[15] or even that an early sexual debut and high-risk sexual behaviour is evident only among those young adults with a history of childhood disruptive behaviour, whereas hyperactivity symptoms are unrelated to RSB Reference Ramrakha, Bell, Paul, Dickson, Moffitt and Caspi[11]. In addition, it has been suggested that the association between ADHD and RSB is mediated by conduct problems in combination with substance use Reference Sarver, McCart, Sheidow and Letourneau[12].
When examining the association between ADHD symptoms and RSB, it might be beneficial to employ a multisystemic framework, since there are several interweaving factors besides conduct problems, associated with adolescent sexual activity, such as those that relate to:
the adolescent him/herself (e.g. behaviour and attitude);
the adolescent's family (e.g. the parent–child relationship);
or that involve extra-familial systems (e.g. peer pressure) Reference Kotchick, Shaffer, Forehand and Miller[16].
For example, previous research has shown that parenting behaviours, such as parental monitoring, parental support and parent–child communication, are associated with a lowered risk for involvement in high-risk behaviour, including RSB, during adolescence [16,17]. However, very few studies have used a multisystemic approach, when investigating the association between ADHD and RSB.
Despite an increasing number of publications suggesting an association between ADHD symptoms and RSB, to the best of our knowledge, there has been limited research exploring this association outside North America. To address this deficit the current study uses data from Russia. There is reason to believe that Russia might be an especially suitable location for this research. Although there is some evidence that the prevalence of ADHD (hyperkinetic disorder) may be similar in Russian and Western children Reference Goodman, Slobodskaya and Knyazev[18], other evidence suggests that sexual risk behaviour is widespread among young people in Russia. Specifically, in an environment where sex education is not taught regularly or systematically in schools Reference Alekseeva, Krasnopolskaya and Skokova[19], a large number of adolescents are engaging in early sexual activity Reference Madkour, de Looze, Ma, Halpern, Farhat and Ter Bogt[20] with alcohol playing an important role in sexual risk behaviour Reference Stickley, Koyanagi, Koposov, Razvodovsky and Ruchkin[21]. Indeed, Russia is currently one of the countries with the highest teenage pregnancy and abortion rates in Europe Reference Panova, Kulikov, Berchtold and Suris[22]. In such circumstances, determining the role of inattention and hyperactivity/impulsivity in RSB may have important public health consequences.
The current study thus has three main aims:
to determine whether inattention and hyperactivity/impulsivity symptoms are associated with RSB in Russian adolescents;
to examine if other factors such as conduct problems, parent–child relations and risk perception are important in this association;
to investigate if there are sex differences in ADHD symptoms and RSB.
2. Methods
2.1. Participants and procedure
This study builds on and extends an earlier study that assessed ADHD symptoms and psychopathology in Russian adolescents Reference Ruchkin, Lorberg, Koposov, Schwab-Stone and Sukhodolsky[23] that was conducted in 2003 in Arkhangelsk, a large city in the Northwestern part of European Russia. In Arkhangelsk, the population's socioeconomic status (SES) is in the low to average range for the whole of Russia. The study participants, 537 adolescent school students (12–17 years of age; mean age 14.37 [SD = 0.96]), were recruited using a two-stage selection process, where school buildings and classes were randomized in order to obtain a representative sample of the adolescent school-age population. Information was collected from both the adolescents and their classroom teachers. The majority of the adolescents were of Slavic origin (Russian = 92.5%, Ukrainian = 1.1%, Byelorussian = 1.9%, other = 4.5%) and 27.1% of them came from single-parent households. In addition, the reported unemployment rates were 14.3% for mothers and 10.5% for fathers, while 15.5% of mothers and 13.6% of fathers were employed part-time. More detailed information regarding the study procedure can be found in Ruchkin et al. Reference Ruchkin, Lorberg, Koposov, Schwab-Stone and Sukhodolsky[23]. Informed consent was obtained from all participants prior to their inclusion in the study. The study was approved by the institutional review committee at the Northern State Medical University (Arkhangelsk, Russia).
2.2. Measures
2.2.1. Outcome variable
Self-rated risky sexual behaviour was assessed with four questions about students’ sexual behaviour:
“How many people have you had sexual intercourse with?”;
“The last time you had sexual intercourse, had you been drinking alcohol or using drugs?”;
“The last time you had sex did you or your partner use a condom?”;
“How many times have you been pregnant or got someone pregnant?”.
As the RSB scores were positively skewed with a large number of students not engaging in any form of RSB, in the analyses that follow the RSB variable was dichotomized so that any student that reported one instance of engaging in at least one RSB, i.e. having more than one sexual partner, using substances during last intercourse, not using a condom during last intercourse and ever being/getting someone pregnant was categorized as having engaged in RSB.
2.2.2. Independent variable
Teacher-rated inattention and hyperactivity/impulsivity symptoms were obtained with the modified version of the ADHD Rating Scale-IV, originally developed by DuPaul et al. Reference DuPaul, Power, Anastopoulos and Reid[24] and subsequently shortened by Power et al. Reference Power, Costigan, Leff, Eiraldi and Landau[25] by selecting six inattention and six hyperactivity/impulsivity items that best predicted a clinical diagnosis of ADHD. This scale has previously been used for assessing the prevalence of ADHD symptoms in Russian adolescents Reference Ruchkin, Lorberg, Koposov, Schwab-Stone and Sukhodolsky[23]. With regard to inattention symptoms, teacher rated how often the student “does not follow through on instructions and fails to finish work”, “has difficulty organizing tasks and activities”, “avoids tasks that require sustained mental effort”, “loses things necessary for tasks or activities”, “is easily distracted”, and “is forgetful in daily activities”. With regard to hyperactivity/impulsivity, the ratings included how often the student: “fidgets with hands or feet or squirms in seat”, “leaves seat in classroom or in other situations”, “is on the go or acts as if driven by a motor”, “blurts out answers before questions have been completed”, “has difficulty awaiting turn”, and “interrupts or intrudes on others”. The 12 items were rated on a 4-point scale ranging from never (0) to almost always (3). The scores were summed into an inattention score (with a possible range from 0–18) and hyperactivity/impulsivity score (0–18). In this sample Cronbach's alpha (α) was 0.89 for the inattention scale and 0.94 for the hyperactivity/impulsivity scale.
2.2.3. Individual-level variables
2.2.3.1. Conduct problems.
Conduct problems were measured with teacher ratings on the SNAP-IV-C Rating Scale, which is a revised version of the Swanson, Nolan and Pelham Questionnaire Reference Swanson, Kraemer, Hinshaw, Arnold, Conners and Abikoff[26], and includes five items corresponding to DSM-IV criteria for conduct disorder. The scale has previously been used with Russian adolescents for assessing the prevalence of conduct problems Reference Ruchkin, Lorberg, Koposov, Schwab-Stone and Sukhodolsky[23] while the items have been shown to load on the same factor in parental ratings, separated from inattention and hyperactivity/impulsivity Reference Cavanagh, Quinn, Duncan, Graham and Balbuena[27]. The items were rated on a 4-point scale ranging from not at all (0) to very much (3), with a possible total score ranging from 0 to 15. Cronbach's α for the scale was 0.89.
2.2.3.2. Substance use.
Substance use was investigated with two self-rating questions. The student was asked if he/she had ever used marijuana. The item was scored as yes (1) or no (0). Binge drinking was measured by asking the student on how many days (if any) did he/she have five or more drinks of alcohol in a row, that is, within a couple of hours. Answer options were 0 days, 1 day, 2 days, 3–5 days, 6 or more days. The variable was used as a discrete variable, ranging from 0 to 4 with higher scores indicating more problematic alcohol use.
2.2.3.3. Perception of risk.
Perception of risk was assessed with nine questions inquiring about respondents’ perception of the risk of harming themselves when engaging in such potentially dangerous activities as substance use, gun carrying, fighting, dropping out of school, sexual intercourse without a condom, etc. These items have previously been used in the Social and Health Assessment (SAHA) study Reference Ruchkin, Schwab-Stone and Vermeiren[28]. Students responded using a 4-point scale where the answer options ranged from no risk (scored 1) to great risk (scored 4). The possible total score ranged from 9 to 36, with higher scores indicating a greater perception of risk. Cronbach's α for the scale was 0.84.
2.2.4. Family-related variables
2.2.4.1. Socio-economic status (SES)
Socio-economic status (SES) was measured using student reports on parents’ (mother and father's) occupation: “not employed” scored as 0, “employed part-time” = 1, and “employed full-time” = 2, with a possible score for each family household of between 0–4.
2.2.4.2. Parenting behaviour.
Parenting behaviour was assessed by youth perceptions of the degree to which their parents and/or primary guardians were involved, supportive or controlled aspects of their lives Reference Ruchkin, Schwab-Stone and Vermeiren[28]. Parental involvement was assessed by six items, e.g. my parents or guardians “Ask me about my life”, “Encourage my interest in different things”. Parental warmth included five items, e.g. my parents or guardians “Are kind to me”, “Show their love for me”. Parental control was assessed by eight items, e.g. my parents or guardians “Tell me what time to be home when I go out”, “Want to know who I am meeting with”. Responses for all three parenting scales were reported on a 4-point scale (1 = never, 2 = rarely, 3 = sometimes, 4 = often). An acceptable level of internal consistency was obtained for all three scales (α = 0.75, α = 0.80, and 0.71, respectively).
2.3. Statistical analyses
All statistical analyses were performed using the Statistical Package for the Social Sciences (IBM SPSS version 24). Associations between the inattention and hyperactivity/impulsivity symptoms, covariates and RSB were calculated with Spearman's rho correlation coefficients. Mann-Whitney U-tests were used to calculate sex differences in symptoms-ratings, while chi-square tests were used to examine if there were any sex differences in RSB. The association between teacher-rated ADHD symptoms (inattention and hyperactivity/impulsivity, as well as the combined measure in a separate model) and RSB was calculated using a hierarchical multiple binary logistic regression model in three blocks; Block 1 adjusted for SES, age and sex; Block 2 additionally adjusted for conduct problems, binge drinking, marijuana use and perceived risk; lastly, in Block 3 we also adjusted for parenting behaviour. The results are presented as odds ratios (OR) with 95% confidence intervals (CI). Finally, we investigated if there were any correlations between ADHD symptoms and different forms of RSB separately using Spearman's rho correlation coefficients, as well as if there was any effect of engaging in more than one RSB on ADHD symptoms using an ANOVA analysis. Two-tailed tests with P-values < .05 were considered significant.
3. Results
The frequency and mean values of all the study variables and male and female differences in these values are presented in Table 1. Teacher ratings were higher for boys than girls for inattention, hyperactivity/impulsivity symptoms and conduct problems. According to the self-reports more boys than girls had used marijuana and had engaged in RSB. In total, 95 (17.7%) students reported RSB, with 8% having had 2 or more sexual partners, 8% had not used a condom during last sex (intercourse), while 3% had been drinking alcohol or using drugs when they last had sex. Very few adolescents reported a pregnancy (2.1%), although there was a much higher prevalence of binge drinking (5 or more drinks in a row) during the previous month (32.7%), and 5.7% had more than one reported RSB.
In the correlation analysis, teacher-rated inattention (ρ = 0.23; P < 0.001), hyperactivity/impulsivity (ρ = 0.10; P = 0.023) and combined (ρ = 0.19; P < 0.001) symptoms were all positively associated with increased RSB. In addition, male sex (ρ = 0.16; P < 0.001), more conduct problems (ρ = 0.16; P < 0.001), marijuana use (ρ = 0.14; P = 0.002), binge drinking (ρ = 0.33; P < 0.001) and perception of risk (ρ = −0.26; P < 0.001) were all significantly associated with RSB (Table 2).
In the hierarchical binary logistic regression analysis (Table 3), inattention symptoms were positively associated with RSB in all blocks, adjusting for possible confounders. Thus, in the final model, RSB was predicted by inattention symptoms (OR = 1.14, 95%CI = 1.01–1.28; P = 0.032), as well as male sex (OR = 2.90, 95%CI = 1.44–5.83; P = 0.003), binge drinking (OR = 1.83, 95%CI = 1.42–2.36; P < 0.001), and low perceived risk (OR = 0.93, 95%CI = 0.87–0.99; P = 0.019). Neither hyperactivity/impulsivity symptoms, nor the combined ADHD symptom score (data not shown), were associated with RSB in any of the models. In addition, age, SES, conduct problems, marijuana use, parental involvement, warmth and control were also not associated with RSB in the final model.
Table 1 Frequency (%) and mean values for all study variables, also split by sex.
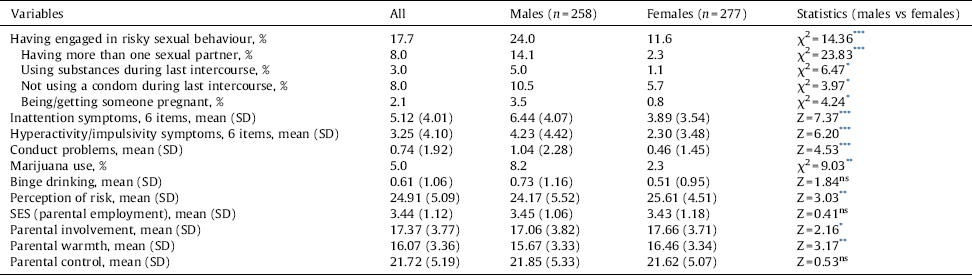
* Mann-Whitney or Chi-square test: P < 0.05.
** Mann-Whitney or Chi-square test: P < 0.01.
*** Mann-Whitney or Chi-square test: P < 0.001.
In an additional analysis that examined the association between inattention/hyperactivity and different forms of RSB separately, the inattention, hyperactivity/impulsivity and combined ADHD symptoms score variables were all associated with having 2 or more sexual partners (ρ = 0.21; P < 0.001; ρ = 0.17; P < 0.001; ρ = 0.21; P < 0.001, respectively), inattention was also associated with not using a condom during last intercourse (ρ = 0.12; P = 0.008). Also, in an ANOVA analysis, an increasing number of RSBs did not result in any differences in the teacher-rated inattention, hyperactivity/impulsivity or combined symptoms measures compared to having one RSB (data not shown).
4. Discussion
In this study, which used data from a community cohort of Russian adolescents, teacher-rated inattention symptoms were associated with significantly increased odds for RSB, such as having unprotected sex, multiple sex partners, sex while intoxicated and unintended pregnancy. To the best of our knowledge, this is the first study to focus exclusively on the association between inattention and hyperactivity/impulsivity symptoms and RSB among adolescents in Russia while also using a multisystemic framework that included possible confounding factors at both the individual- and family-level. The association between inattention and RSB was independent of hyperactivity/impulsivity, conduct problems, substance use, risk perception, and parenting behaviours. In addition, male sex, binge drinking and a lower assessment of perceived risk all predicted RSB in the adjusted model.
Adolescence is characterized by a desire for autonomy and by increasing conflicts with parents, and in this context risk-taking behaviours should not simply be dismissed as maladaptive, as they may serve important developmental functions, such as an attempt to crystallize identity and find self-worth Reference King and Lewis[29]. Unfortunately, RSB is also associated with serious social, health, and school problems, such as increased substance use, illicit substance use, antisocial behaviours, lower school grades, lower self-esteem and an increased risk of sexual victimization [30–33]. Furthermore, the potential consequences of unstable sexual relationships include a heightened risk for medical outcomes such as sexually transmitted diseases [34,35]. Among this sample of Russian adolescents, 17.7% reported engaging in RSB, which was more common in boys than girls. A higher risk for RSB in males is frequently described in the academic literature, with males starting to have sex at an earlier age than females and reporting more sexual partners Reference Dir, Coskunpinar and Cyders[7].
The main finding of this study, that symptoms within the ADHD spectrum were associated with RSB, is in line with the findings from previous research, with reports of an association between ADHD symptoms and early sexual debut, more partners and more partner pregnancies [9,10,13,14]. These findings may reflect more general deficits in executive function that have been linked to ADHD symptoms, such as an inability to inhibit impulses and self-regulate behaviours; a greater propensity to engage in reward and sensation seeking behaviour, and poor social skills Reference Sonuga-Barke, Bitsakou and Thompson[3]. Previous research has highlighted impulsivity as a possible underlying causal factor in the pathway to RSB among individuals with ADHD [7,9]. In this study, hyperactivity/impulsivity was indeed associated with RSB in the correlation analysis. However, the association disappeared in the regression analysis which indicates that this behavioural trait is not uniquely predictive of RSB, a result which is in line with a previous study Reference Sarver, McCart, Sheidow and Letourneau[12]. The finding that inattention rather than hyperactivity/impulsivity is linked to RSB accords with the result from an earlier study which showed that childhood inattention alone predicted subsequent substance use in adolescence Reference Molina and Pelham[36], and with the finding from a recent study where inattention was uniquely associated with a higher prevalence of alcohol use before sex in young adult women Reference Hosain, Berenson, Tennen, Bauer and Wu[10].
It is uncertain what underlies the association between inattention and RSB, although different mechanisms might be involved. Previous studies have indicated that impairments in executive functioning, i.e. the cognitive processes by which we organize and plan behaviour in order to facilitate the attainment of goals, are primarily associated with symptoms of inattention rather than hyperactivity/impulsivity [37,38]. In line with this, four of the ADHD symptoms included within the predominately inattentive subtype relate to problems with organization and planning (i.e., loses things, is forgetful, has difficulties organizing tasks, and fails to finish tasks). Hypothetically, deficits in planning and organizing behaviours, as well as being easily distracted and forgetful might result in greater difficulty when it comes to predicting the consequences of one's own sexual (and other) activities and thus an increased likelihood of engaging in RSB, although in this study, inattention remained associated with RSB even after adjusting for risk perception. An earlier study which found that inattention was the sole predictor of later substance use among children diagnosed with ADHD suggested that academic difficulties might be the mechanism that linked inattention and substance use Reference Molina and Pelham[36]. Academic problems might also be important in the current study as previous research has indicated that inattention symptoms are strongly associated with school failure (lower grades) Reference Serra-Pinheiro, Mattos, Regalla, de Souza and Paixao[39], while low school attachment, getting into trouble at school, a low reading score and plans to leave school early have all been linked to the initiation of earlier sexual activity Reference Paul, Fitzjohn, Herbison and Dickson[33]. There is also some evidence that inattention is more strongly linked to low self-esteem than hyperactivity in adolescents with ADHD Reference Klassen, Miller and Fine[40], while lower self-esteem has also been related to risky sexual behaviour in adolescents Reference Ethier, Kershaw, Lewis, Milan, Niccolai and Ickovics[41].
Some previous studies have reported a higher risk for RSB only when ADHD symptoms were co-morbid with conduct problems Reference Galera, Messiah, Melchior, Chastang, Encrenaz and Lagarde[15] or when a history of childhood disruptive behaviour was reported Reference Ramrakha, Bell, Paul, Dickson, Moffitt and Caspi[11]. However, in the current study, the association between inattention symptoms and RSB was independent of conduct problems. This finding is nevertheless in line with several previous reports where ADHD symptoms predicted earlier sexual intercourse, more sexual partners, more casual sex and more partner pregnancies independent of conduct problems [9,13]. Given these contradictory results across studies, more research on the interrelations between ADHD symptoms, conduct problems and RSB is now required in different settings and among different age groups to better elucidate these associations. Among the covariates, the finding that binge drinking was the most important predictor for RSB is also in line with the results from a review study which showed that alcohol use by adolescents was highly correlated with a range of other risky behaviours, including illicit substance use, lower school performance, delinquency, and adolescent mortality Reference Windle[42].
Table 2 Correlations between inattention and hyperactivity symptoms, other study variables and risky sexual behaviour (RSB).
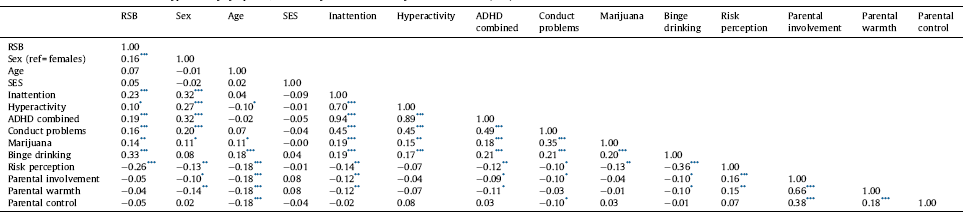
* Spearman's rho: P < 0.05.
** Spearman's rho: P < 0.01.
*** Spearman's rho: P < 0.001.
This study has several limitations that should be noted when considering the findings. The assessment of ADHD symptoms and conduct problems was based solely on teacher reports, which may have been subject to reporting bias especially as some conduct problems may not be evident in the school-setting. Indeed, although parental or teacher ratings have been shown to be generally valid with regard to externalizing symptoms Reference Collett, Ohan and Myers[43], using data on ADHD symptoms from other information sources, such as those obtained through parental ratings or a structured diagnostic interview would have improved confidence in our findings. In addition, information on RSB, substance use, risk perception and parenting behaviours was obtained from adolescents’ self-reports, which may also be vulnerable to several types of potential bias, although research has suggested that adolescent self-reports of some forms of health risk behaviour (e.g. regarding drinking behaviour) can be regarded as being generally valid Reference Lintonen, Ahlstrom and Metso[44]. In addition, as this study was cross-sectional, causality could not be established for the observed associations. Finally, as this study was undertaken in just one region of Russia, future research will be needed in other locations to establish generalizability.
5. Conclusions
In conclusion, this study has shown that inattentive but not hyperactive/impulsive symptoms are associated with RSB in Russian adolescents. This is an important finding, especially as during childhood the more ‘overt’ symptoms within the ADHD spectrum, such as hyperactivity/impulsivity, are regarded as being more impairing than symptoms of inattention Reference Coles, Slavec, Bernstein and Baroni[45]. As a consequence, children with hyperactive symptoms are often evaluated as being more in need of additional services Reference Coles, Slavec, Bernstein and Baroni[45]. However, symptoms of inattention persist, to a higher degree than hyperactivity/impulsivity, into adulthood Reference Thapar and Cooper[46], and are more closely linked with school failure Reference Serra-Pinheiro, Mattos, Regalla, de Souza and Paixao[39]. Thus, our finding highlights the importance of both detecting and treating inattention problems in childhood and adolescence.
Table 3 Results of a hierarchical binary logistic regression analysis predicting risky sexual behaviour (RSB).
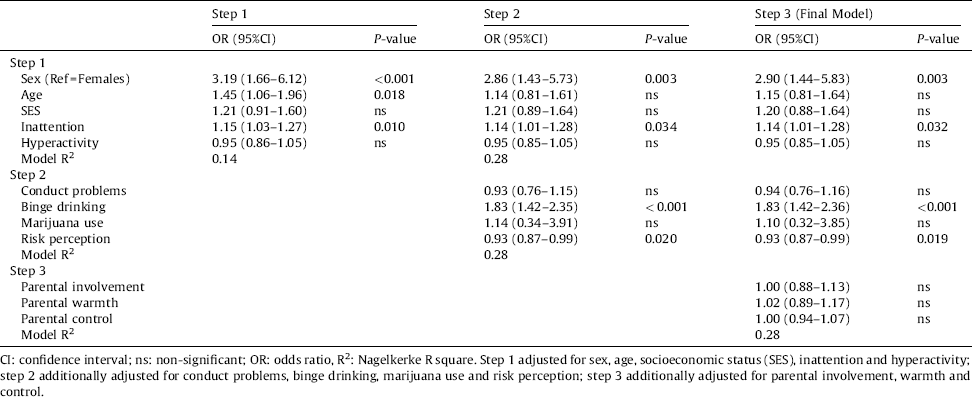
CI: confidence interval; ns: non-significant; OR: odds ratio, R2: Nagelkerke R square. Step 1 adjusted for sex, age, socioeconomic status (SES), inattention and hyperactivity; step 2 additionally adjusted for conduct problems, binge drinking, marijuana use and risk perception; step 3 additionally adjusted for parental involvement, warmth and control.
Disclosure of interest
The authors declare that they have no competing interest.
Acknowledgements
This research was supported by funds from the Uppsala University Hospital Research Fund (ALF) to JI. We are grateful to all the adolescents and teachers who participated in the study.






Comments
No Comments have been published for this article.