Introduction
Vascular restenosis is the recurrent lumen narrowing phenomenon occurring in 30–50% of patients subjected to revascularization procedures, which is arbitrarily defined as a permanent narrowing of vessel diameter greater than 50% when compared with a reference artery.Reference Lesperance, Bourassa and Schwartz1 With the increased use of non-invasive detection techniques, the morbidity of in-stent restenosis (ISR) becomes increasingly frequent. However, despite the innovative devices and procedures recently developed and the novel concomitant drug therapies administered to patients, it still represents a limiting factor in the long-term success of revascularization procedures.Reference Forte, Rinaldi, Berrino, Rossi, Galderisi and Cipollaro2
Currently, for the stenosis of carotid artery, carotid endarterectomy (CEA) is still the golden standard approach for the treatment of symptomatic patients.Reference Levy, Hanel and Lau3 Recently, it has been shown in the clinical trials that carotid artery stenting (CAS) had comparable efficacy compared with CEA.Reference Ca4,Reference Massop, Dave and Metzger5 CAS may still be considered for patients with high risk for complications because of different comorbidities or anatomical variations.Reference Christiaans, Ernst and Suttorp6 However, the benefits of CAS in preventing the future stroke may be hampered by the occurrence of ISR. It has been reported that the morbidities of ISR during CAS were between 1.8% and 20%, depending on the definition of restenosis used and the duration of follow-up, which are considered to be equivalent to restenosis rates after CEA (with the morbidity of restenosis between 1.8% and 22%, Table 1).Reference de Borst, Ackerstaff and de Vries7,Reference Lal, Beach and Roubin8
Table 1: The morbidity of stroke after different interventions for asymptomatic and symptomatic patients
CEA = carotid Endarterectomy; CAS = carotid artery stenting.
Different treatment options are available when revascularization of ISR is warranted, but still no clear treatment algorithm on the optimal technique is available.Reference van Haaften, Bots, Moll and de Borst9 Previous reports have indicated that repeated stent placement, angioplasty with balloon techniques, and surgical treatments are the main treatments for ISR. Recently, drug-coated balloons (DCBs) or drug-eluting balloons (DEBs), with the features of homogenous distribution of antiproliferative drugs to the vessel wall,Reference Sangiorgi, Romagnoli and Biondi-Zoccai10 have been advocated for treatment of ISR in the coronary and femoropopliteal areas in recent years, but an overview of this application in the carotid artery restenosis is still lacking.Reference Zeller, Rastan and Macharzina11,Reference Siontis, Stefanini and Mavridis12 It has been reported that DCB angioplasty showed satisfactory efficacy in carotid artery stenosis and in-stent restenosis in several studies.Reference Morr, Lin and Siddiqui13 However, little is known about the long-term effects of DCB angioplasty compared with cutting balloon or regular balloon angioplasty or operations such as CEA. Furthermore, although a small number of reviews and several reports have summarized the intervention strategies for ISR, no comprehensive review has been conducted to investigate the efficacy and long-term prognosis of CEA, DCBs, cutting balloon angioplasty, or repeated CAS on carotid ISR patients. In this review, we searched the main databases and enrolled all the clinical studies that investigating the therapeutic efficacy of different treatment strategies on carotid ISR, while comparing the efficacy and prognosis of these different types of treatments. Our study may provide more evidence for the treatment of carotid ISR.
Methods
Data Sources and Searching Strategies
An electronic literature search was conducted to identify candidate articles published until March 2019, based on the published articles in Pubmed (MEDLINE), EMBASE, Cochrane Library, and unpublished data through clinical trials website (www.clinicaltrials.gov). MESH terms and other terms were used for literature search using different combinations. The terms used included “in-stent re-stenosis,” “in-stent restenosis,” “re-restenosis,” “in-stent stenosis,” “recurrent stent stenosis,” “carotid artery,” “treatment,” “therapy,” “PTA” or “percutaneous transluminal angioplasty,” “angioplasty,” “drug eluting balloon” or “drug coated balloon,” “drug-eluting stents” or “drug-coated stents,” “paclitaxel-coated” or “paclitaxel,” with no language restrictions. Two authors (C. He and X. Zhou) conducted that literature search independently, whereas a third investigator (S. Wang) solved any discrepancies.
Eligibility Criteria
The clinical trials would be included in this review if they met the following criteria: (i) Participants: adults older than 18 and have been diagnosed as in-stent restenosis after PTA. Since that carotid stent induces artifactually higher peak systolic velocities, the velocity criterion was not used to evaluate carotid artery stenosis. Luminal reductions by ultrasonography on gray-scale images and color flow disturbances were evaluated.Reference Zhou, Lin and Bush14 Clinically significant stenosis was defined as luminal reduction of 80% or higher. High-grade in-stent stenosis, identified by ultrasonography, was further verified by biplanar carotid angiography, and the stenosis was measured geometrically on the basis of the North American Symptomatic Carotid Endarterectomy Trial criteria;Reference Zhou, Lin and Bush14 (ii) Intervention: the treatment strategies of the studies contained CEA, PTA (repeated CAS, regular balloon angioplasty, cutting balloon angioplasty, or drug-coated balloon angioplasty); (iii) Outcomes: treatment efficacy (e.g., angiographic stenosis ratio and peak systolic velocity changes) and treatment complications; (iv) Study design: clinical studies with the publication types such as retrospective studies and cross-sectional studies were included.
Studies were excluded if (i) they were published in the forms of case reports, reviews, editorials, conference abstracts; (ii) they were not written in English; (iii) they did not focus on carotid in-stent restenosis; and (iv) they did not report the key results concerning the treatment efficacy or complications.
Data Extractions
The data extracted from the included studies contained the following aspects: (1) Study characteristics: study design, year, publication, and study region; (2) Studies’ outcomes: diagnosis, treatment, treating results, devices used, and complications; (3) Patients characteristics: number of patients, gender ratio, mean age, symptoms, target vessels, diameter stenosis, previous treatments, time to first ISR, risk factors, and drugs used.
Results
Literature Search Results
After searching the literature, totally 545 studies were identified after removing the duplicates. Furthermore, 306 full-text eligible studies were further assessed after removing the studies that did not meet the inclusion criteria. Then 25 studies were finally included for further review, and no unpublished data were obtained. The studies finally enrolled included 5 comparative studies, 4 studies with operative treatment, and 19 studies using PTA with balloon or stent angioplasty. A flow diagram outlining the literature search strategies and results is presented (Figure 1), with the study characteristics and main results presented in Table 2. It was presented that studies conducted in USA and Italy accounted for the majority of the enrolled studies. In detail, among the five comparative studies, two studies compared the efficacy between regular with cutting balloon angioplasty and the other three studies compared CEA with PTA, balloon angioplasty with balloon plus stent implantation, stenting with cutting balloon angioplasty, respectively. Four studies reported the treatment of ISR with CEA. Meanwhile, among the 16 studies with PTA treatment, 7 studies reported re-PTA with stent placement,Reference Chakhtoura, Hobson and Goldstein15–Reference Koebbe, Liebman, Veznedaroglu and Rosenwasser21 5 studies reported DCB angioplasty,Reference Gandini, Del Giudice and Da Ros22–Reference Tekieli, Pieniazek and Musialek26 the other 4 studies reported the efficacy of ISR treatment with regular or cutting balloon angioplasty.Reference Donas, Eisenack and Torsello27–Reference Setacci, Sirignano and de Donato30
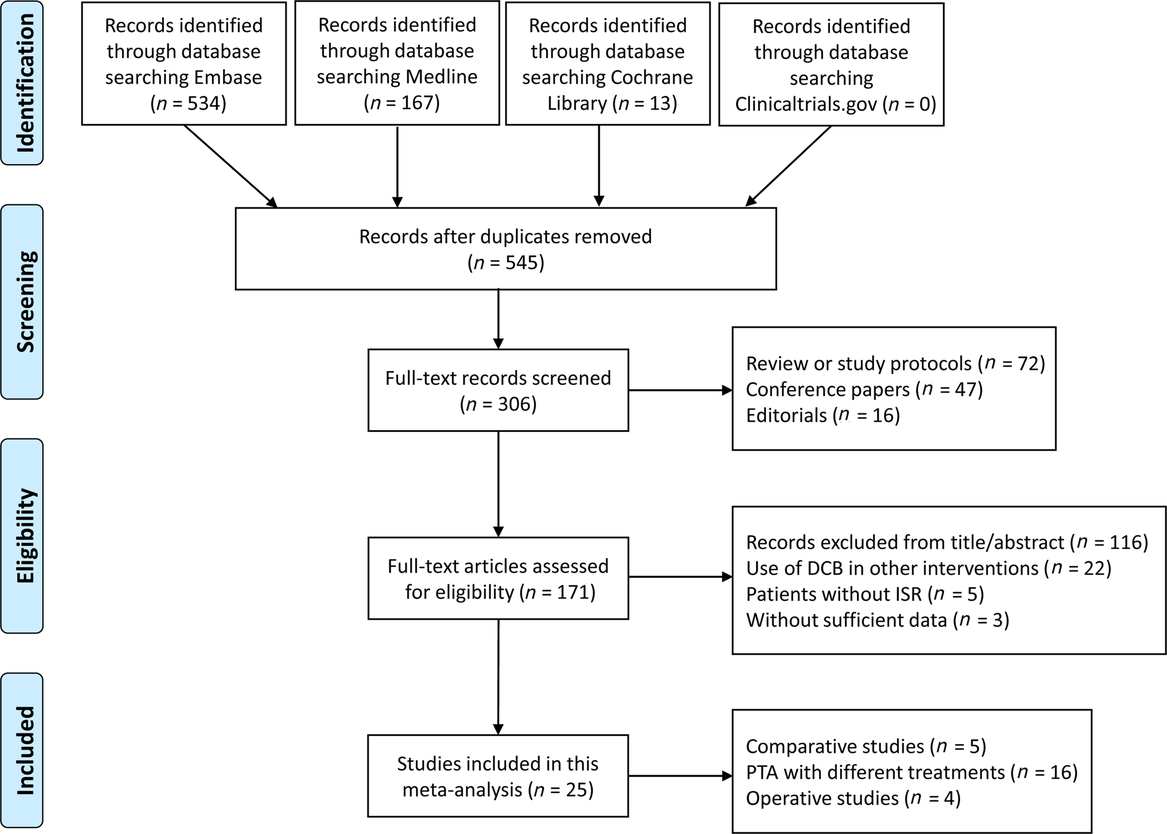
Figure 1: The flow diagram of literature search and selection of studies.
Table 2: Basic information and main results of included studies
CAS = carotid artery stenting; DCB = drug-coated balloon; DEB = drug-eluting balloon; PTA = percutaneous transluminal angioplasty; CEA = carotid Endarterectomy; PSV = peak systolic velocity; ICA = internal carotid artery; EFS = event-free survival; MI = myocardial infarction; TIA = transient ischemic attack; CB = cutting balloon.
Outcomes of Treatment Efficacy
Comparative Studies
Among the five comparative studies, Aburahma et al. compared the efficacy of operative treatment with PTA/stenting for the treatment of carotid restenosis, demonstrating that PTA/stenting has a higher incidence of restenosis than reoperation, but with less perioperative and neurological complications.Reference Aburahma, Bates, Stone and Wulu31 Meanwhile, Chung et al. indicated that treatment using balloon angioplasty did not improve the long-term outcomes of patients with carotid ISR.Reference Chung, Valentine and Sharath32 However, Levy et al. reported angioplasty with balloon technique decreased carotid restenosis more efficiently.Reference Levy, Hanel and Lau3 Furthermore, Setacci et al.Reference Setacci, de Donato and Setacci33 reported that cutting balloon angioplasty had better long-term outcomes [14 ± 5% restenosis, peak systolic velocity (PSV) of internal carotid artery (ICA) 95 ± 11 cm/s] compared with repeated balloon angioplasty (17 ± 8% restenosis, ICA PSV 105 ± 15 cm/s) or repeated CAS (22 ± 7% restenosis, ICA PSV 122 ± 13 cm/s). Also, Zhou et al. reported that cutting balloon angioplasty improved the ISR by decreasing the ISR rate from 88.6% to 15%, whereas PTA decreased the ISR rate from 82.5% to 20%.Reference Zhou, Lin and Bush14 These results indicated that CEA might provide better effects in improving the ISR compared with PTA, while among the balloon angioplasty techniques, cutting balloon angioplasty could exert better long-term prognosis.
Angioplasty Efficacy
To evaluate the efficacy of those types of therapeutics, three parameters were used, the angiographic stenosis rate, the PSV changes, and the long-term prognosis. For the angiographic stenosis rate, the studies adopting the PTA interventions, few studies reported about the angiographic stenosis rate, but most of the studies reported that through endovascular PTA treatment, angiographic stenosis decreased significantly and ISR was successfully treated. On the other hand, most of the studies adopting DCB angioplasty reported the angiographic stenosis changes. In detail, it showed that the study of Gandini et al. showed that DCB treatment decreased the angiographic stenosis from 87% to 6%,Reference Gandini, Del Giudice and Da Ros22 while the study of Montorsi et al. showed that the final angiography stenosis reduced from 84.5% to 19% after intervention.Reference Montorsi, Galli and Ravagnani23 Also, the study of Pohlmann et al. showed the restenosis area decreased from 85% to 16%Reference Pohlmann, Holtje, Zeile, Bonk, Urban and Bruning25 and the study of Tekieli et al. exhibited the stenosis reduced from 84.6% to 10.7% upon DCB treatments.Reference Tekieli, Pieniazek and Musialek26 For the treatment of regular balloon angioplasty, the stenosis rates decreased to 16% in Zhou et al.’s study after intervention.Reference Zhou, Lin and Bush14 For the treatment of common or cutting balloon angioplasty, the study of Donas et al. showed that the primary and assisted primary patency rates were 68.8%,Reference Donas, Eisenack and Torsello27 while the angiography stenosis rates also decreased to 20% after treatment (Heck’s studyReference Heck28). At last, the therapeutic of CEA could also significantly solve the problem of carotid ISR.
The second parameter is the PSV changes before and after the angioplasty intervention. It showed that the PSV values decreased from 4.7 to 0.6 m/s in Gandini et al.’s study,Reference Gandini, Del Giudice and Da Ros22 from 4.0 to 0.9 m/s in Montorsi et al.’s study after DCB treatment.Reference Montorsi, Galli and Ravagnani23 The studies covering other types of therapeutics did not report the changes of PSV values.
The third parameter is the long-term follow-up results, which is the most important outcome in choosing the appropriated treatment modalities. As to the PTA with stenting treatment, Koebbe et al. showed that among the 19 carotid ISR patients, 1 patient exhibited restenosis after re-PTA for 14 months of follow-up.Reference Koebbe, Liebman, Veznedaroglu and Rosenwasser21 Lal et al. reported the long-term results of PTA relieved carotid ISR in three out of five patients after 1-year follow-up.Reference Lal, Hobson and Goldstein16 In the study of Lanzino et al., it showed that PTA combined with stent placement effectively treated the carotid ISR for at least 6 months.Reference Lanzino, Mericle, Lopes, Wakhloo, Guterman and Hopkins17 Meanwhile, in the study of Willfort-Ehringer et al., it was demonstrated that the six patients with carotid ISR were all treated with PTA with stenting, with only four patients remained patent for >1 year. As to the treatment with DCB, it was shown that the revascularization rate was 33.3% after DCB treatment in Gandini et al.’s study.Reference Gandini, Del Giudice and Da Ros22 In the study of Piccoli et al., 14 of 18 patients were without restenosis, and the other 4 patients with mild (<30%) restenosis during follow-up.Reference Piccoli, Biondi-Zoccai and Gavrilovic24 In Pohlmann et al.’s study, the 1-year event-free survival (EFS) was 100%, with the rates of 2-year/3-year/5-year EFS were 83%.Reference Pohlmann, Holtje, Zeile, Bonk, Urban and Bruning25 Furthermore, for the treatment of other balloon angioplasty, all patients remained asymptomatic and without recurrent restenosis greater than 30% during 18 months of follow-up using regular balloon angioplasty. Also, the 1-month patency without restenosis after cutting balloon angioplasty was 5/6 (83%), and the patency without restenosis was 4/5 (80%) after 20 months follow-up adopting the cutting balloon angioplasty.Reference Heck28 For the patients using CEA for carotid ISR, Borst et al. reported that all four surgically treated patients remained asymptomatic and without recurrent restenosis over a mean follow-up time of 13 months.Reference de Borst, Ackerstaff, Mauser and Moll34 Marcucci et al. and Reichmann et al. all described that patients with a normal patency of the surgical correction were without recurrent restenosis during the follow-up period,Reference Marcucci, Accrocca, Giordano, Antonelli, Gabrielli and Siani35,Reference Reichmann, van Laanen and de Vries36 while Yu et al. reported that one patient occurred recurrent symptomatic restenosis (90%) 1 year later and all other patients remained asymptomatic and without recurrent restenosis.Reference Yu, Yan and Zhang37
Complications
As to complications, most of the studies reported the 30-day peri-operative or peri-procedure complications. Aburahma et al. compared the 30-day perioperative complications between CEA and PTA/stenting, indicating that patients with CEA had less ipsilateral strokes but more cranial nerve injuries.Reference Aburahma, Bates, Stone and Wulu31 The study of Chung et al. showed that one stroke and subsequent death occurred at 30 days,Reference Chung, Valentine and Sharath32 other comparative studies all reported that no procedure-related complications occurred within 30 days.
As to the PTA/stenting treatment, most studies reported that no periprocedural complication occurred, indicating that PTA/stenting is a safe treatment that could be widely used for carotid ISR. For DCB treatment, three studies described that no interventional complications leading to new or aggravated neurological deficits in the patients,Reference Gandini, Del Giudice and Da Ros22,Reference Pohlmann, Holtje, Zeile, Bonk, Urban and Bruning25,Reference Tekieli, Pieniazek and Musialek26 whereas Montorsi et al. reported that one patient had a left hemispheric stroke 2 months after procedure and Piccoli et al. reported that one patient had a transient ischemic attack (TIA) during prolonged DCB inflation.Reference Montorsi, Galli and Ravagnani23,Reference Piccoli, Biondi-Zoccai and Gavrilovic24 For the studies that intervened with the cutting balloon angioplasty, Heck reported no procedural complications or ischemic events during the follow-up period,Reference Heck28 while the study of Satecci et al. showed no major intraprocedural complications.Reference Setacci, Sirignano and de Donato30 As to the operation treatment, two out of four studies reported that no major complications occurred. Reichmann et al. reported that 1 patient sustained an intraoperative minor ischemic stroke, while no neurologic complications occurred in the other 14 patients.Reference Reichmann, van Laanen and de Vries36 Also, Yu et al. reported that a total of three complications happened in three patients (30%).Reference Yu, Yan and Zhang37
As to the long-term complications, it was shown that patients with PTA remained asymptomatic and without recurrent restenosis over a mean follow-up time of 10 ± 6 months.Reference Chakhtoura, Hobson and Goldstein15 Also, Radak et al. reported that no TIAs or strokes were verified during the follow-up, and non-neurologic mortality was 3.13%.Reference Radak, Tanaskovic and Sagic18 No ischemic events were observed during the follow-up period in any of the six patients reported by Heck.Reference Heck28 Other studies did not provide long-term risk of treatments. Therefore, we might conclude that PTA/stenting and balloon angioplasty treatment had less complications compared with CEA.
Factors Affecting the Prognosis
In order to further analyze the factors that might affect the efficacy and long-term prognosis of patients with carotid in-stent restenosis, we summarized the main commodities and other risk factors in Table 3.
Table 3: Basic characteristic of patients in the included studies
CAS = carotid artery stenting; RICA = right internal carotid artery; LICA = left internal carotid artery; DCB = drug-coated balloon; DEB = drug-eluting balloon; HTN = hypertension; DM = diabetes mellitus; CAD = coronary artery disease; SMK = smoking; CEA = carotid Endarterectomy; ISR = in-stent restenosis.
As to the baseline characteristics, it showed that mean age of patients in the enrolled studies ranged from 61.3 to 78.1 years. For the features of the diseases, most of the patients in these studies were asymptomatic. As to the target vessels, most of the studies did not provide the detailed information, while it was reported that patients in the DCB group had both the left and the right carotid lesions. Furthermore, as to the diameter stenosis of the lesion vessels, most of the studies reported that a larger than 80% restenosis existed. However, Chung et al. reported a >50% restenosis,Reference Chung, Valentine and Sharath32 Radak et al. reported that the stenosis was >50% for symptomatic patients and >80% for asymptomatic patients.Reference Radak, Tanaskovic and Sagic18 In the balloon angioplasty and CEA groups, the diameter stenosis was larger than 70%.
As to the previous treatments before the restenosis, three out of seven studies adopting re-PTA/stenting had previous CEA treatment while the other four studies had CAS history. For balloon angioplasty group, only one study had previous CEA treatment, with other studies had CAS interventions. For the CEA subgroup, all the studies had previous CAS interventions. The time to first ISR after treatments was also reported in the included studies. For patients with previous CEA treatment, the time to first ISR after treatments was 16–57 months, whereas for CAS interventions, this time interval ranged from 6 to 21 months.
For the comorbidities of patients in these studies, most of the studies reported that patients were complicated with hypertension, diabetes, dyslipidemia, and smoking. However, the percentage of these commodities were similar in different subgroups, which did not affect the long-term effects of the treatment modalities. Meanwhile, among the drugs used before and after the interventions, double antiplatelet therapy was commonly used in most of the studies.
Discussion
Despite various CAS procedures reported in the literature, the long-term incidence of ISR remains undefined, especially for carotid arteries. Choosing the best treatment strategy for stenosis and in-stent restenosis has been studied widely. Previous reports indicated that CEA and CAS had their own advantage and disadvantages for the treatment of carotid stenosis. However, for carotid ISR, little is known about the best treatment strategy. According to previous review, the most commonly used treatment option for ISR is re-PTA combined with the regular balloon angioplasty.Reference Pourier and de Borst38 In this review of the literature, we showed that the treatment of CEA might be the best in achieving the best angioplasty efficiency, but with increased possibility of periprocedural complications, while for those patients with high-risk factors, re-PTA with balloon angioplasty might provide better protections.
Different reports have been published about the incidence for ISR.Reference Pourier and de Borst38 For ISR after CAS, infrequent complication was reported by several authors, with an incidence of 3.5–4.9%,Reference Wholey, Wholey and Mathias39 which is still common for patients with CAS. Previously, the heterogeneity in the minimally required degree of ISR of studies limited the availability to compare the results. Some studies used the degree of lumen reduction, detected by ultrasound, whereas other studies adopted the PSV values. It has been reported that duplex velocities would increase with the presence of a stent and in absence of a stenotic lesion, while the type of stent used for previous CAS could also influence the ISR patent and the PSV values.Reference de Borst, Meijer, Lo, Vosmeer, Ackerstaff and Moll40–Reference Pierce, Rosero and Modrall42 Therefore, the difference in these parameters in the treatment of ISR limited the summary of previous studies. Meanwhile, the diagnosis of ISR in the studies enrolled in this review was based mainly on the lumen stenosis by ultrasonography. However, due to the differences of patient selection, types of stents, and follow-up durations, a quantitative meta-analysis cannot be conducted. Furthermore, the degree of stenosis at which revascularization for symptomatic lesions is favored is also unclear. Because carotid ISR lesions appear less embologenic,Reference Zahn, Ischinger and Zeymer43 it is plausible that intervention may be reserved for only high-grade stenoses rather than for all lesions >50%.Reference Chung, Valentine and Sharath32
As to the treatment options of carotid ISR, still limited evidence was presented and the ideal therapeutics have not been identified, with the choice of re-PTA/stenting, repeated balloon angioplasty (regular, cutting or DCB), and surgical treatment (CEA with stent removal, carotid artery bypass, or interposition graft).Reference Jost, Unmuth, Meissner, Henn-Beilharz, Henkes and Hupp44 In our study, we showed that all the therapeutic measures for carotid ISR could effectively relieve the problem, whereas CEA might bring better long-term prognosis. Still, other studies indicated that the placement of a stent for carotid stenosis was associated with a 5.8% composite rate of stroke, death, and myocardial infarction compared with a rate of 12.6% for CEA at 30 days according to the SAPPHIRE trial. Nevertheless, an increased number of patients with recurrent stenosis in the subgroup of stenting compared with operation arm according to the CARESS trial.Reference Levy, Hanel and Lau3 Also, in the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS), severe (70–90%) recurrent stenosis was found in 14% of patients who had undergone angioplasty with or without stent placement compared with 4% of those who had undergone surgery.Reference Ederle, Bonati and Dobson45 Conducting CEA might provide better results with less occurrence of carotid ISR with the longest follow-up of 7 years for 0.1%.Reference Ecker, Pichelmann, Meissner and Meyer46
DCB angioplasty is a newly development technique that has the following advantages: immediate drug release without the use of a polymer that could trigger late thrombosis; no prolonged, direct drug contact with the arterial wall, allowing better reendothelization of the vessel; no foreign object left in the body, which is especially important in peripheral applications where stents may be used for suboptimal results; maintenance of original vessel anatomy and flexibility; and finally, lower restenosis rates in most indications.Reference Marzullo, Aprile, Clementi, Stella, Modena and Sangiorgi47 However, it is worth keeping in mind that the concept of DCBs is still in development. This technology was hampered by a lack of solid preclinical data and long-term animal studies, non-standardized coating methods, and variances in the reproducibility of results. Currently, several kinds of DCBs are developed in market.Reference Sangiorgi, Romagnoli and Biondi-Zoccai10 The mechanical action as the balloon crushes the plaque creates microchannels through which the paclitaxel can be absorbed by the vessel. Preliminary preparation of lesions using pre-dilation, atherectomy, or cutting balloon can optimize drug transfer during DCB inflation. Compared to long inflation durations, short inflations and nominal pressure cause less arterial injury, preserving the inhibitory effect. In our study, several studies reported that several patients might have TIA during prolonged DCB inflation. Therefore, in the setting of carotid ISR, utilization of distal or proximal protection devices is highly recommended. Furthermore, an enormous need for robust preclinical data is related to drug transfer capability, drug transfer amount in the vessel, residual drug concentration after inflation, and vessel tolerance to large drug amounts delivered in a short interval. Subsequently, this information must be translated to the clinical arena by randomized controlled clinical trials to confirm DCB efficacy in patients affected by atherosclerotic disease. Through the data from our review, we recommend using the paclitaxel-eluting technologies for carotid in-stent restenosis, which may provide better long-term results, but still more clinical trials are needed.
The major events occurring during or immediately after a revascularization procedure and triggering post-intervention vascular restenosis in patients include endothelial denudation, damage or rupture of elastic laminae in the vascular wall, oxidative stress, an imbalance in MMPs (matrix metalloproteinases) and their inhibitors, inflammation, apoptosis, cytokine and chemokine release, homing of circulating progenitor cells, and a phenotype switch of resident cells.Reference Weintraub48 Restenosis is considered as an excessive wound healing reaction or as a maladaptive response of the artery to trauma induced during revascularization, resulting in neointimal hyperplasia and vascular remodeling. Currently, the available DCBs could release the drugs (paclitaxel, by inhibiting cell proliferation; trimetazidine, by protecting the endothelia) to the different targets in this pathological process. However, several other kinds of drugs, such as anti-inflammatory drugs, antioxidant drugs, drugs inhibiting cell proliferation and migration, have also been developed and tested in the restenosis models of animals. Therefore, considering these promising results, further efforts are warranted to develop DCB conjugated with novel drugs that are able to selectively affect smooth muscle cells, not just endothelial cells, both proliferation and migration.
The limitations of this review are as follows. First, most of the included studies are cross-sectional studies and with heterogeneity in patients’ characteristics, which cannot be quantitatively analyzed and synthesized. Meanwhile, the number of studies concentrating on the different interventions in treating carotid ISR is still very few, and more comparative studies are needed to further prove the long-term prognosis.
Conclusions
The therapeutic measures for carotid ISR had their own features, with CEA had the highest efficacy while re-PTA/stenting and balloon angioplasty were with less complications. More large-scale comparative clinical studies are needed to further ascertain the best strategies.
Statement of authorship
Study conception and design was contributed by SW and CH; literature search and data acquisition was conducted by CH and XZ; interpretation of the data was performed by XZ and ZY; CH drafted the manuscript; SW critically revised the manuscript; final approval was done by CH, SW, XZ, and ZY.
Disclosures
The authors have no conflicts of interest to declare.






