Hypertension is a key feature of the metabolic syndrome(1). Weight loss, exercise, smoking cessation, and restriction of alcohol and sodium are lifestyle changes that are well known to lower blood pressure (BP)(Reference Dickinson, Mason and Nicolson2, Reference Chobanian, Bakris and Black3). Although such modifications often promote minor alterations in BP, even small reductions may be beneficial on a population basis as hypertension is a major public health challenge. Dietary fat modification may influence BP as shown previously(Reference Shah, Adams-Huet and Garg4–Reference Geleijnse, Giltay and Grobbee6), but the knowledge of the effects in subjects with the metabolic syndrome is limited. Targeted interventions in these subjects are important as they have increased risk of hypertensive organ damage(Reference Cuspidi, Meani and Fusi7) and elevated pulse pressure (PP) that predicts cardiovascular events(Reference Franklin, Khan and Wong8, Reference Mansia, De Backer and Dominiczak9). The objective of the present analysis was to investigate the effect of an isoenergetic change in dietary fat quality and quantity on BP in subjects with the metabolic syndrome.
Experimental methods
The LIPGENE study was a 12-week parallel, randomised controlled trial that was performed in eight European centres as part of an European Union Sixth Framework Project (http://www.ucd.ie/lipgene/). The study was conducted according to the Declaration of Helsinki, and all procedures involving human subjects were approved by the local ethics committees at all centres. Written informed consent was obtained from all subjects. US National Library of Medicine Clinical Trials registry number: NCT00429195.
Subjects
Study participants were of Caucasian ethnicity, aged 35–70 years (BMI 20–40 kg/m2), and had the metabolic syndrome defined by three or more of the following slightly modified National Cholesterol Education Program Adult Treatment Panel III criteria(1): levels of fasting plasma glucose >5·5mmol/l, TAG ≥ 1·5 mmol/l, HDL-cholesterol < 1·0 mmol/l (males) or < 1·3 mmol/l (females), systolic BP (SBP) ≥ 130 mmHg or diastolic BP (DBP) ≥ 85 mmHg or on BP-lowering medication, and waist circumference >102 cm (males) or >88 cm (females). Antihypertensive medication, hormone replacement therapy, multivitamin supplements and non-fatty acid-based nutritional supplements were allowed if the subjects adhered to the same diet regimen throughout the study. Exclusion criteria included pre-diagnosed diabetes, inflammatory diseases, use of statins and anti-inflammatory drugs, fatty acid supplements, alcohol abuse and a recent weight change ≥ 3 kg.
Diets
Subjects were randomly assigned to one of the four isoenergetic diets differing in fat quantity and quality as described extensively(Reference Shaw, Tierney and McCarthy10). In short, two diets provided 38 % energy from fat: one with high content (16 % energy) of SFA (HSFA diet) and another with high content (20 % energy) of MUFA (HMUFA diet). Two low-fat, high-complex carbohydrate (LFHCC) diets contained 28 % energy from fat, with diet LFHCC n-3 including 1·2 g/d supplement of very long-chain marine n-3 PUFA and diet LFHCC control including a control high-oleic acid sunflower-seed oil capsule (Lipid Nutrition, Loders Croklaan, Wormerveer, The Netherlands). A food exchange model was developed, and fat-modified food products (margarines, cooking and baking fats, oils, dressings and biscuits) were supplied by Unilever (Vlaardingen, The Netherlands). All participants completed a 3 d weighed food record and a FFQ to estimate dietary intake. Food records were also completed mid- and post-intervention to assess compliance. Nutrient composition was calculated using centre-specific dietary analysis programmes, including the nutrient composition of the LIPGENE intervention foods. Dietary targets were achieved with aimed differences in fat quantity and quality(Reference Shaw, Tierney and McCarthy10).
Methods
BP was measured at screening, baseline and at the end of the study using an automatic BP measuring device. According to the European Society of Hypertension Guidelines(Reference Geleijnse, Giltay and Grobbee6), BP measurement was obtained with an appropriate sized cuff positioned at the heart level, after the subjects had rested for at least 5 min. The same arm was used for each measurement and at least two measurements were performed at each visit, and the average was used for data processing. PP was calculated as the difference between SBP and DBP.
Statistical methods
Baseline data are presented as group means and standard deviations, and BP changes are given as mean per group and 95 % CI. General linear models (two-way analysis of covariance (ANCOVA)) were used to assess differences in BP between groups, adjusted for baseline BP, centre, age and body weight. The ANCOVA model in which weight change was included yielded the same point estimates and P values of the dietary effects on BP that were the same as those yielded by the model in which weight change was not included. Moreover, weight change was not a significant factor in the adjusted model. A two-sided P value < 0·05 was regarded significant. Analyses were performed using SPSS for Windows 16.0 (SPSS, Inc., Chicago, IL, USA) and R 2.8.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Pre-investigation was completed in a total of 486 subjects across the eight centres, and 428 subjects had baseline BP measurements available (196 males and 232 females, HSFA n 102, HMUFA n 115, LFHCC control n 109 and LFHCC n-3 n 115). Clinical characteristics are described in Table 1; there were no differences between dietary groups at baseline. Baseline BP did not differ between completers and non-completers, and the non-completers were evenly distributed between dietary groups.
Table 1 Baseline clinical characteristics
(Mean values and standard deviations)

SBP, systolic blood pressure; DBP, diastolic blood pressure; PP, pulse pressure; AU, arbitrary units.
In the overall ANCOVA, there were no differences in the changes observed in SBP, DBP or PP between the four dietary groups (P = 0·52, 0·24 and 0·78, respectively). We investigated whether hypertensive and normotensive individuals responded differently to the intervention, but no differences were observed. Body weight remained unchanged in the two high-fat dietary groups, but it was slightly reduced in the two low-fat dietary groups (LFHCC control: − 0·9 (95 % CI − 1·3, − 0·6) kg and LFHCC n-3: − 0·7 (95 % CI − 1·0, − 0·3) kg).
In a secondary analysis, we compared the HSFA and the HMUFA diets, and a significant diet × sex interaction for PP (P = 0·01) was seen. In a sex-specific subanalysis, the effect in males differed between the two diets. The PP increased in the HSFA group by 2·8 (95 % CI 0·0, 5·7) mmHg, and it did not change in the HMUFA group. There was also a significant diet × sex interaction for SBP (P = 0·03) and PP (P = 0·01) between the HSFA diet and the low-fat diets. In a sex-specific subanalysis, SBP and PP differed between these diets only in males. The HSFA diet was associated with an increase in PP and no change in SBP, whereas the low-fat diets were followed by a decrease in SBP ( − 3·7 (95 % CI − 6·0, − 1·4) mmHg) and a NS change in PP ( − 1·8 (95 % CI − 3·9, 0·3) mmHg) (Table 2).
Table 2 Blood pressure (BP) and pulse pressure (PP) at baseline and change during intervention
(Mean values, standard deviations and 95 % confidence intervals)
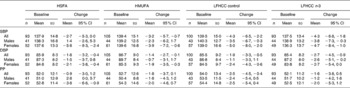
HSFA, high-fat diet rich in saturated fat; HMUFA, high-fat diet rich in monounsaturated fat; LFHCC control, low-fat, high-complex carbohydrate diet with control supplement; LFHCC n-3, LFHCC with very long-chain n-3 PUFA supplement; SBP, systolic BP; DBP, diastolic BP.
Discussion
We found no major BP effects of isoenergetic dietary fat modification in subjects with the metabolic syndrome. However, the HSFA diet had a minor unfavourable effect on BP in males. The potential of dietary changes to lower BP was clearly demonstrated in the Dietary Approaches to Stop Hypertension (DASH) study(Reference Appel, Moore and Obarzanek5). A low-fat diet with increased consumption of fruit and vegetables, low-fat diary and whole-grain products substantially decreased SBP and DBP compared with a control diet. The fat content and composition of the DASH diet and control diet in this trial were similar to those of the LIPGENE LFHCC and HSFA diets. We observed a similar tendency in SBP in males only, and no effect in the total LIPGENE cohort. However, the LIPGENE cohort was more overweight, and the whole diet approach taken in the DASH study was different from the LIPGENE modification of macronutrient composition. In line with the present findings, no difference in BP was observed between a high saturated fat diet and a low-fat diet in a small crossover study in normotensive subjects with type 2 diabetes(Reference Storm, Thomsen and Pedersen11).
DBP was reduced on a high monounsaturated fat diet compared with an isoenergetic high saturated fat diet in healthy subjects in the KANWU study(Reference Rasmussen, Vessby and Uusitupa12). Dietary targets and study design were comparable to the HSFA and HMUFA diets in the LIPGENE study. We did not confirm these findings in our cohort; however, we found a disadvantageous effect of saturated fat in males. This has also been reported by others; in a crossover dietary intervention study in normotensive subjects, both SBP and DBP were significantly higher during the high saturated fat period compared with isoenergetic high monounsaturated, n-6 or n-3 fatty acid periods(Reference Lahoz, Alonso and Ordovas13).
We observed no statistical differences between the LFHCC n-3 and the LFHCC control diets.
The lack of BP-lowering effects of the very long-chain marine n-3 PUFA supplementation may be due to the relatively low dose (1·2 g/d) used in the present study, as only supplements of high doses (>3 g/d) of very long-chain marine n-3 PUFA are found to lower BP in hypertensive patients(Reference Mansia, De Backer and Dominiczak9).
The LIPGENE study is one of the largest dietary intervention studies carried out in subjects with the metabolic syndrome. With subjects from all over Europe, the dietary interventions were implemented on a heterogeneous dietary background. The dietary intakes, as assessed by weighed food records, were achieved with significant differences in fat quantity and quality between diets(Reference Shaw, Tierney and McCarthy10). The study was designed to be isoenergetic, and the subjects were not to lose weight. Body weight did not change in the high-fat groups, but there was a minimal, although statistically significant, weight loss < 1 kg in the low-fat groups. The change in body weight, however, was not significantly correlated with changes in BP, and it did not influence the results in the ANCOVA modelling. The primary endpoint of the LIPGENE study was insulin sensitivity; therefore, the original power calculations did not include BP estimates, which limit the impact of the present analysis. However, post hoc analysis indicated a power of 80 % to detect a 4 mmHg difference in DBP between groups. All our BP measurements were performed according to guidelines, yet both the regression to the mean effect and the habituation effect, the phenomenon that BP decreases with repetitive measurements, are well-known problems in BP research. These effects might partly explain the reduction in BP in all the four dietary groups, and could be responsible for masking differences between the diets.
In conclusion, altered quantity and quality of dietary fat had no major effects on BP in subjects with the metabolic syndrome participating in the LIPGENE dietary intervention study. The HSFA diet had minor adverse effects on SBP and PP in males.
Acknowledgements
The study was supported by LIPGENE – an European Union Sixth Framework Program Integrated Project (FOOD-CT-2003-505944), the Norwegian Foundation for Health and Rehabilitation, South-Eastern Norway Regional Health Authority and Johan Throne Holst Foundation for Nutrition Research. J. L., C. D., E. E. B., J. L.-M., A. D.-K., B. K., H. M. R. and C. A. D. contributed to conception and design of the LIPGENE dietary intervention study. H. L. G., I. M. F. G., A. C. T., D. I. S., O. H., A. M. J. v. H., J. D.-L., I. L.-G. and U. R. contributed to acquisition of data. H. L. G. and I. M. F. G. performed the statistical analyses, interpreted the data and drafted the article. C. A. D. and K. I. B. provided significant academic advice and consultation through interpretation of data and writing of the article. All authors contributed to the revision of the manuscript and approved the final version. There is no conflict of interest for any of the authors.




