Introduction
Cholesteatoma is considered a benign, progressive and destructive epithelial lesion, consisting of keratinising squamous epithelium in the middle ear and/or mastoid.Reference Castle1,Reference Maniu, Harabagiu, Perde Schrepler, Cătană, Fănuţă and Mogoantă2 It is a common health problem, with an incidence of 9.2 per 100 000 in adults and 3 per 100 000 in children.Reference Volgger, Lindeskog, Krause and Schrötzlmair3 If undetected and untreated, cholesteatoma may lead to significant complications associated with the destruction of temporal bone structures.Reference Volgger, Lindeskog, Krause and Schrötzlmair3 This can result in conductive and sensorineural hearing loss, cranial invasion (leading to brain abscess or meningitis), and, in some cases, facial nerve paralysis.Reference Maniu, Harabagiu, Perde Schrepler, Cătană, Fănuţă and Mogoantă2 The only therapy is surgery. However, the main challenges in cholesteatoma surgery are the prevention of cholesteatoma recurrence, and the preservation and improvement of hearing.
Previous research showed recurrence rates ranging from 0 to 70 per cent. Recurrence risk depends on multiple factors, such as the chosen surgical technique and the size and localisation of the cholesteatoma. Although there is broad literature about recurrence rates and risk factors, predominantly in university medical centres, it is hard to translate this to daily clinical practice in a secondary hospital, because of great variations in study design, patient population and surgical technique.Reference Britze, Møller and Ovesen4
This study aimed to determine predictors of cholesteatoma recurrence and binaural hearing loss in patients who underwent combined approach tympanoplasty. In addition, this study functions as a baseline for a future investigation evaluating recurrence after combined approach tympanoplasty with mastoid obliteration.
Materials and methods
Participants
This retrospective cohort study includes 67 patients who underwent cholesteatoma removal between 2015 and 2018 in a leading secondary clinical medical centre in The Netherlands (Jeroen Bosch Hospital). The patient and cholesteatoma characteristics are shown in Table 1.
Table 1. Patient and clinical characteristics*

* n = 67. †As observed during first-look surgery. Pre-op = pre-operative; AC = air conduction; SEM = standard error of the mean; BC = bone conduction; ABG = air–bone gap
The selection of patients was performed using the treatment code for cholesteatoma surgery, for procedures conducted within the time frame stated. Patients were included if a cholesteatoma was observed during surgery and if the first cholesteatoma removal procedure took place in the Jeroen Bosch Hospital. In order to prevent bias associated with surgical technique, only the patients who had undergone combined approach tympanoplasty were included; this was the preferential treatment during the stated time frame.
The average follow-up time was 35 months after the first operation. Most patients underwent a pre-operative computed tomography (CT) scan, which was used to assess the ossicular anatomy and to obtain an idea of the extension of the cholesteatoma. The indication for an eventual ‘second look’ was based on diffusion-weighted magnetic resonance imaging (MRI) or findings during the first surgery (extensive cholesteatoma or postponed chain reconstruction).
Outcomes
The primary aim of this study was to evaluate predictors of recurrence. Recurrence was evaluated by diffusion-weighted MRI or second-look surgery. We did not distinguish between residual and recurrent cholesteatoma in this retrospective study, so the collective term ‘recurrence’ was used.
Secondarily, we aimed to evaluate predictors of binaural hearing loss. Binaural hearing loss was defined as a mean conductive hearing loss of less than 20 dB over the frequencies 0.5, 1, 2 and 4 kHz. Monaural hearing loss was defined as a mean conductive hearing loss of 20–35 dB (monaural hearing loss without a need for hearing aids) and hearing loss over 35 dB (monaural hearing loss with a need for hearing aids).
Data were obtained from the medical records and surgical reports. The information collected included: the location of recurrence, complications, air and bone conduction thresholds at 0.5, 1, 2 and 4 kHz, age, gender, affected side, and localisation and size of the cholesteatoma. In order to assess cholesteatoma size, the middle ear was divided into eight compartments: hypotympanum, protympanum, mesotympanum, epitympanum, sinus tympani, facial recess, antrum and mastoid.Reference Volgger, Lindeskog, Krause and Schrötzlmair3 The cholesteatoma could be present at multiple locations, depending on its size.
Additional data gathered from the surgical reports included: surgeon, surgical approach, ossicular chain status and reconstruction, scutum reconstruction, Silastic sheet use, and presence of an overhanging or low tegmen (hereafter referred to as a low tegmen). Peri-operatively, a tegmen was defined as low if the view of the attic was restricted.
Furthermore, complications with a direct effect on patient wellbeing were reported. A complication was considered serious when: it caused permanent damage, surgical reintervention was indicated, prolonged hospitalisation was necessary or it led to a potentially life-threatening situation.
Statistical analysis
All the data, pseudonymised and recorded in a database, were exported to SPSS® software (version 26) for statistical analysis. Variables that are potentially related to recurrence were entered in the logistic regression model using backward selection. Because of the limited sample size, the level of significance for the logistic regression was set at 0.3 or lower.Reference Bekkers, van Hulst, Erasmus, Delsing, Scheffer and van den Hoogen5 We present the predictive values for recurrence. Goodness of fit was evaluated using a Hosmer–Lemeshow test for quartiles; significance was set at 0.05 or less, which indicates a poor fit of the model.
The pre- and post-operative audiometric data were analysed using a logistic regression with backward selection, and a Mann–Whitney U test. The difference in cholesteatoma localisation between the first and the second surgery was analysed using McNemar's test. The significance level was p ≤ 0.05.
Ethical considerations
Our study retrospectively examined the outcomes of a cohort of patients. Patients were diagnosed and treated according to the department and national guidelines. This research had negligible risks and involved the use of existing patient data. Furthermore, there was no harm or discomfort for the participants. All the data were collected as part of an internal evaluation to improve the quality of care. The main risk in this retrospective cohort was the breach of trust or confidentiality. We minimised this risk by making the data accessible only to the researchers; the data were also anonymised as soon as feasible. We believed that the expected benefits of this project exceeded this minimal chance of inconvenience.
Results and analysis
Patient characteristics
The characteristics data of the 67 patients were included for analysis (Table 1). Of the participants, 65.7 per cent were male, and the average age at the time of surgery was 40 years. The patients were divided into adults (n = 56) and children (age of less than 16 years, n = 11). Fifty-five per cent of the patients were treated for a cholesteatoma on the left side.
In 7.5 per cent (n = 5) of the patients, the combined approach tympanoplasty was converted to a canal wall down procedure because of radicalisation by the cholesteatoma itself or a restricted view of the attic. None of these five patients eventually had a recurrence (p = 0.147). Nineteen out of the 67 patients developed a recurrence (28.4 per cent). The recurrence rate was 23.3 per cent in adults and 45.5 per cent in children.
After the first surgery, revision surgery (second-look surgery) was indicated in 25 patients (37 per cent). In 19 of the 25 patients, recurrence was the indication for the second-look surgery. Out of these 25 patients, 3 are scheduled for revision surgery, and 2 patients were referred to another hospital for treatment.
Twenty patients underwent a second look in the Jeroen Bosch Hospital. In 10 patients, the decision for the second-look surgery was based on MRI findings; in the other cases, it was based on the first surgery or clinical findings. The median time to the second look was 16.5 months. In 14 of these 20 patients (70 per cent), a recurrence was found. The canal wall was maintained in 19 patients. The median time to recurrence was 25 months. Four patients (6 per cent) required a third look because of recurrence or ossicular chain reconstruction.
Prediction model for recurrence
Nineteen out of 67 patients had recurrences. Based on previous literature and surgeons’ experience, the variables childhood, size, surgeon and low tegmen were entered in the univariate analysis. There was no multicollinearity between the variables. After backward selection, two variables were identified as predictors of recurrence: low tegmen and childhood (Table 2). Statistical analysis showed a good fit of the model. As a result, cholesteatoma recurrence ranged from 18 per cent, in adults without a low tegmen, to 82.8 per cent, in children with a low tegmen.
Table 2. Prediction model for cholesteatoma recurrence risk*
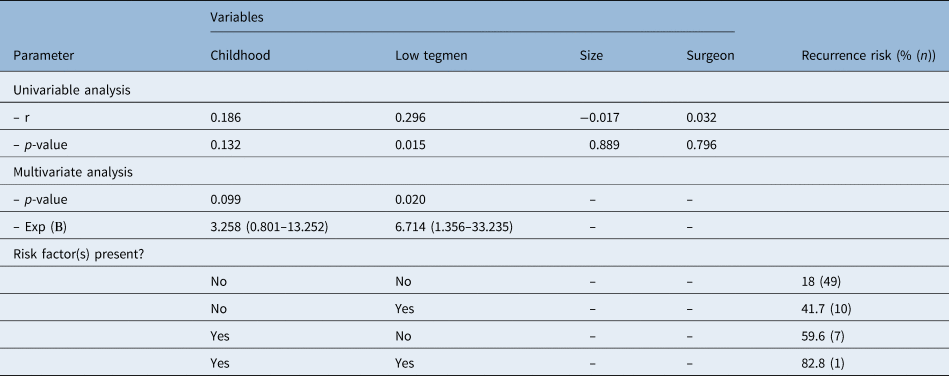
* n = 67. R = correlation for recurrence. Nagelkerke R2 = 0.160. Hosmer–Lemeshow test value = 0.539. Exp (B) = exponentiation of beta coefficient
Secondary outcomes
Binaural hearing loss predictors
Binaural hearing loss, defined as a mean air conduction threshold of less than 20 dB over the frequencies 0.5, 1, 2 and 4 kHz, was reached in 13 patients (21.3 per cent) after the first surgery or, if performed, the second-look surgery. Based on previous literature and surgeons’ experience, the variables childhood, protympanic localisation, surgeon, stapes erosion and incus erosion were entered in the univariate analysis. Ossicular chain reconstruction during the first and second look was excluded because of the multicollinearity with surgeon. After backward selection, two variables were identified as predictors of binaural hearing loss: stapes erosion and childhood (Table 3). Statistical analysis indicated a good fit of the model. The model showed that children without stapes erosion have a 49.2 per cent chance of binaural hearing loss. However, adults with stapes erosion have only a 5.5 per cent chance of binaural hearing loss.
Table 3. Prediction model for a post-operative air conduction of less than 20 dB*
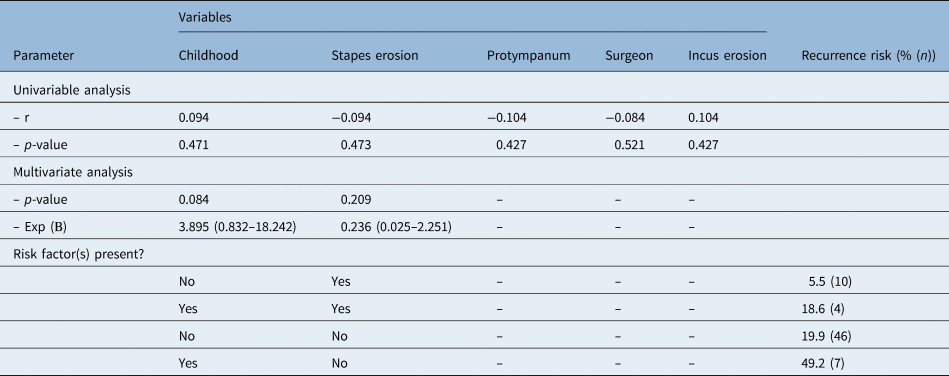
* n = 61. R = correlation for air conduction of less than 20 dB. Nagelkerke R2 = 0.105. Hosmer–Lemeshow test value = 0.594. Exp (B) = exponentiation of beta coefficient
Audiometry
The patients underwent pure tone audiometry before and after surgery (Figure 1). The mean pre-operative conductive hearing level was 39.03 dB. After surgery (first and second), this improved to 34.30 dB. Twenty-one patients (35.0 per cent) needed hearing aids because of a post-operative air conduction of over 35 dB. Post-operatively, 26 patients (43.3 per cent) had monaural hearing loss without the need for hearing aids (20–35 dB). Thirteen patients (21.6 per cent) had a conductive hearing loss of less than 20 dB after cholesteatoma removal (Table 4).

Fig. 1. Mean pre-operative (pre-op) and post-operative (post-op) air conduction (AC) and bone conduction (BC) thresholds in children (a) and adults (b).
Table 4. Changes in air conduction threshold due to surgery
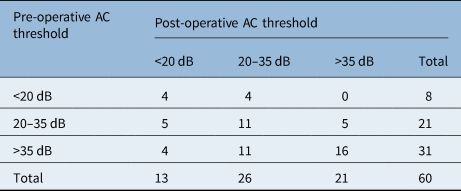
AC = air conduction
The patients in the group with more than 35 dB hearing loss pre-operatively had a significantly larger cholesteatoma than the patients in the group with less than 20 dB hearing loss (4.3 vs 2.9 compartments involved; p < 0.05). The cholesteatoma size in the 20–35 dB group (3.81 compartments) did not significantly differ from that in the more than 35 dB hearing loss group and the less than 20 dB hearing loss group.
In nine patients (13.4 per cent), the ossicular chain was intact and not removed; in the other patients (n = 58, 86.6 per cent) the chain was disconnected by the cholesteatoma or removed during surgery (disconnected chain). Forty-eight of the patients with a disconnected chain underwent ossicular chain reconstruction, resulting in 57 patients with a post-operative intact chain. The mean air conduction in patients with an intact ossicular chain was 37.87 dB pre-operatively; post-operatively, it improved to 33.31 dB. In patients with a disconnected ossicular chain pre-operatively, the air conduction was 46.39 dB, and post-operatively it improved to 40.00 dB. The improvement is comparable in both groups (p = 0.427).
Furthermore, patients with a pre-operative conductive hearing loss of over 35 dB had a 12.9 per cent chance of binaural hearing loss and a 35.5 per cent chance of monaural hearing loss without the need for hearing aids, and 51.6 per cent still needed hearing aids post-operatively. Patients with a pre-operative hearing loss of 20–35 dB had a 23.8 per cent chance of binaural hearing loss. However, 23.8 per cent of patients experienced hearing loss. There is a 50 per cent chance that patients with a less than 20 dB conductive hearing loss before surgery will remain below that threshold (Table 4).
Second-look surgery
The patients with a recurrence who underwent a second look were analysed (n = 14). The location of the cholesteatomas during the first look was compared with the location during the second look. Most recurrences were discovered in the epitympanum and antrum. There was a low chance of recurrence in the facial recess when initial cholesteatoma was located in the facial recess (p = 0.008).
Complications
There were no serious complications reported. Post-operative otorrhoea was not described in the patients’ clinical notes. Post-operatively, one patient experienced vertigo without nystagmus, one had facial pain without a focus, one had a wound infection, one had a seroma and one had a post-auricular fistula. There was no indication for reintervention.
Discussion
This study revealed that a low tegmen and young age are predictors of cholesteatoma recurrence in primary surgery conducted in a secondary hospital. A low tegmen led to a recurrence in 59.6 per cent of the patients. In children with a low tegmen, the risk of recurrence is as high as 82.8 per cent. Moreover, young age and the absence of stapes erosion are predictors of binaural hearing loss.
The recurrence rates of this study, which were 23.3 per cent in adults and 45.5 per cent in children, are in line with previous literature.Reference Volgger, Lindeskog, Krause and Schrötzlmair3,Reference Britze, Møller and Ovesen4,Reference Iino, Imamura, Kojima, Takegoshi and Suzuki6,Reference Morita, Takahashi, Izumi, Kubota, Ohshima and Yamamoto7 Despite the acknowledged importance of an experienced surgeon, the operating surgeon was not identified as a risk factor for recurrence in our study.Reference Volgger, Lindeskog, Krause and Schrötzlmair3 We were able to identify childhood and a low tegmen as risk factors for recurrence, especially when both these risk factors are present. Previous research showed that cholesteatomas are more aggressive in children than in adults; this is in line with our results.Reference Jackson, Addison and Prinsley8
A large cholesteatoma is also considered a predictor of recurrence in children younger than eight years.Reference Stangerup, Drozdziewicz and Tos9 In our study, cholesteatoma size was not a predictor of recurrence. Moreover, cholesteatoma size was equal in children and adults, and was equal between patients with and without a low tegmen, which indicates that size is not the most important determinant. Ossicular chain erosion and an inexperienced surgeon are other known risk factors for recurrence.
To the best of our knowledge, a low tegmen has not been identified as a risk factor for recurrence until now.Reference Volgger, Lindeskog, Krause and Schrötzlmair3,Reference Stangerup, Drozdziewicz and Tos9 It is known that exposure of the protympanum and anterior epitympanum may be challenging in a canal wall up procedure.Reference Park, Amoodi, Kuthubutheen, Chen, Nedzelski and Lin10 It is possible that inadequate visualisation, resulting from a low tegmen, can lead to a residual cholesteatoma.
This study also shows that ossicle erosion predicts worse post-operative hearing, especially in adults. Recent studies have revealed a relation between ossicle erosion and conductive hearing loss; the more the ossicles were eroded, the worse the conductive hearing loss.Reference Martins, Victor and Selesnick11,Reference Olsen, Ribeiro Fde, Yasui and dos Santos12
Additionally, previous research found a mean air conduction improvement of 8.15 dB; in this study, the improvement was 4.73 dB.Reference Prasad, La Melia, Medina, Vincenti, Bacciu and Bacciu13 This contrast may be explained by a difference in age, as the former study evaluated only children and the latter study evaluated both children and adults. Another important determinant of post-operative hearing is pre-operative hearing.Reference Blakley, Kim and VanCamp14 This study provides an indication of hearing outcome post-operatively based on the pre-operative audiometry.
Strengths and weaknesses
The current study provides insight into, and predictors of, cholesteatoma recurrence and binaural hearing loss in a secondary hospital. Nevertheless, this study has some flaws. First, patient numbers were limited, and there was a large difference in the numbers of operations performed by each surgeon. All patients, however, received equal treatment, and exclusions were limited, which increases the extent to which the results are generalisable. Second, there was only a limited follow-up time. Future research would increase the inclusion period, the follow-up time and the number of participants. Third, we were unable to distinguish between residual and recurrent cholesteatoma, because this was not reported. Fourth, some audiological data were missing, and those patients could not be included in the prediction model for hearing outcome. This was, however, only a secondary aim of the study.
Implications for clinical practice
Clinicians should be aware of a high recurrence risk in children, especially in combination with a low tegmen. Bowdler and Walsh stated that microscopy fails to give adequate visualisation of the protympanum in a canal wall up procedure, and that a solution for this is to use 0 and 70 degree otoendoscopes.Reference Bowdler and Walsh15 The value of this technique can be studied further to rule out epithelial debris in cases of a low tegmen. Additionally, future research could investigate the value of pre-operative CT scanning in predicting the need for an adjusted surgical technique based on tegmen height.
The treatment analysed here consisted of combined approach tympanoplasty without mastoid obliteration. The current literature describes obliteration techniques with lower recurrence rates. Mastoid obliteration has been introduced in clinical practice in our hospital. Future research aims to compare the outcomes of cholesteatoma surgery with and without mastoid obliteration.
• The cholesteatoma recurrence rate was 23.3 per cent in adults and 45.5 per cent in children
• A low tegmen and young age are predictors of cholesteatoma recurrence
• In cases of a low tegmen, additional techniques could be used to rule out any epithelial debris
• Young age and the absence of stapes erosion are predictors of binaural hearing loss
• Patients and parents could be counselled based on the predictors of recurrence and hearing loss
Furthermore, this study confirms that hearing outcome is often disappointing. Patients and parents can be counselled based on the reported determinants concerning recurrence risks and hearing outcome.
Conclusion
This study demonstrated that patients – especially children – with a low tegmen have an increased risk of recurrence. Age and a low tegmen are easily determined pre-operatively. We recommend that ENT surgeons be aware of recurrence in children, particularly in cases of a low tegmen, and adjust surgical techniques appropriately. Furthermore, this study indicates that childhood and the absence of stapes erosion are predictors of binaural hearing loss.
Competing interests
None declared







