DOI: 10.1017/S2040174417000526, published by Cambridge University Press, 19 July 2017.
Unfortunately the above mentioned article was published without the author’s full corrections implemented. The fully corrected version is contained in this erratum.
The Publishers apologise for the error.
The use of assisted reproductive technologies (ART) for the treatment of infertility has grown exponentially over the last 20 years, and now accounts for 4% of all births in Australia, and over 1 m births annually around the globe. There is consistent reporting of increased risk of adverse perinatal outcomes and birth defects following infertility treatment. However, change in practice has been stymied by critical knowledge gaps with regards to (a) the relative contribution of patient and treatment factors to adverse outcomes, (b) the independent contribution of specific contemporary treatments and treatment combinations to outcomes, (c) the impact of innovations in laboratory and clinical practice on treatment success and observed risk and (d) changes over time in patient characteristics. Here we summarize key findings from the South Australian Birth Cohort, which is a whole-of-population cohort of over 300,000 births from 1986 to 2002. Relative to spontaneous conceptions, singletons from assisted conception were more likely to be stillborn [odds ratio (OR)=1.82; 95% confidence interval (CI) 1.34–2.48], while survivors as a group were comprehensively disadvantaged at birth, including lower birth weight (OR=2109 g; 95% CI 2129–289), very low birth weight (OR=2.74; 95% CI 2.19–3.43), very preterm birth (OR=2.30; 95% CI 1.82–2.90) and neonatal death (OR=2.04; 95% CI 1.27–3.26). Major birth defects, including cardiac, urogenital and musculoskeletal defects are doubled after fresh intra-cytoplasmic sperm injection (ICSI) cycles, which is a particular concern as ICSI now accounts for 70% of all treatment cycles globally. Future study is needed to provide contemporary, precise evidence to inform patient and clinic decision making, and generate knowledge for future innovation in ART laboratory methods and clinical practice, thereby optimizing treatment and health outcomes while reducing adverse events.
Key words
developmental stage
fetus/fetus
human
pregnancy
Introduction
The use of assisted reproductive technologies (ART) for the treatment of infertility is increasing dramatically. Globally more than five million babies have been born from assisted conception and this population is now increasing by over one million per annum.Reference Mansour 1 Australia reflects this international trend: 1 in 25 Australian births are now from infertility treatment.Reference Macaldowie, Wang, Chughtai and Chambers 2
While both practitioners and parents are heavily and emotionally focussed on increasing birth rates, the success of ART has been marred by an excess of birth defects and poor perinatal outcomes in children conceived using ART. Innovation has swept ahead of our knowledge of how infertility treatments affect the short- and long-term health of mother and child. Accumulating evidence suggest patient characteristics and infertility treatments are both associated with a profile of adverse outcomes such as low birth weight, preterm birth, stillbirth, neonatal death and major birth defects. Many of the poor outcomes associated with ART births are in principal preventable as they reflect patient and clinical choice, or are amenable to further targeted rapid technical development.
Encouragingly, clinicians in some jurisdictions have demonstrated a willingness to change practice in line with emerging evidence, such as the rapid adoption of single embryo transfer. However, further change in practice has been stymied by critical knowledge gaps and confusion over sources of risk, and is highly dependent on the funding model for treatment costs, as insurance tends to defray the significant cost and there by permit a more conservative treatment strategy.Reference Hart and Norman 3
Birth defects are the major cause of infant death and contribute to long-term disability in survivors. Defects occur at up to double the population rate for specific ART treatments, such as fresh intra-cytoplasmic sperm injection (ICSI).Reference Davies 4 Further, the use of multiple embryo transfer doubles the risk of cerebral palsy, where lifetime care averages $1 m per case, adding $4000 per ART twin child or $8000 per pregnancy. The rate increases from 2 out of 1000 births in naturally conceived singletons to 4 out of 1000 in naturally conceived twins, to 5 out of 1000 for ART singletons and 9 out of 1000 in ART twins. Outcomes such as cerebral palsy and very preterm birth and very low birth weight are potentially catastrophic and often result in significant family distress. They are also extremely expensive in terms of immediate medical costs as well as long-term care that may be required due to the presence of major disabilities. For instance, estimates of the cost of neonatal intensive care are $2000–$3000 per day, with a course of care for a very premature baby around $300,000.Reference Petrou, Eddama and Mangham 5 As the risk of very preterm birth is doubled in ART singletons (occurring in around 2%),Reference Marino, Moore and Willson 6 this equates to a cost of ~$600,000/100 ART births. There are at present no comprehensive cost data on the long-term disabilities and chronic disease that is likely to accrue. However, prematurity and poor growth are early indicators of vulnerability for conditions including poorer metabolic health and intellectual disability.Reference Hart and Norman 3 Therefore, identifying the specific contemporary ART practices that contribute to reductions in serious pregnancy complications and adverse neonatal outcomes has the potential to reduce significant healthcare costs immediately, and on a recurrent basis.
We propose that there is a hierarchy of risk associated with contemporary treatment strategies, with adverse outcomes more likely when children are conceived with more invasive treatment. The challenge to current practice is to identify the safest, minimal treatment strategy of known conception benefit to a couple before considering more invasive options. Where appropriate, encouraging and planning a course of tailored, stepped care would represent a significant change in focus for clinicians and patients in an era where 70% of all treatments globally involve highly invasive ICSI.
Australian clinicians have reacted positively to improved data and information, and our country’s strong base of world leading fertility researchers would be well positioned to develop improved ART treatment strategies as a result of this research. A shift to lower risk treatments will result in patients having healthier children while saving our healthcare system many millions of dollars per annum in neonatal and long-term care costs.
In Australia, use of ART for the treatment of infertility is increasing dramatically. Between 2002 and 2012 the number of ART treatment cycles doubled from 35,000 to 65,000 (see Fig. 1). One in 25 Australian births are now from infertility treatment.Reference Macaldowie, Wang, Chughtai and Chambers 2 This is a global phenomenon: more than five million babies have been born, a population that is now increasing at over one million per annum.Reference Mansour 1
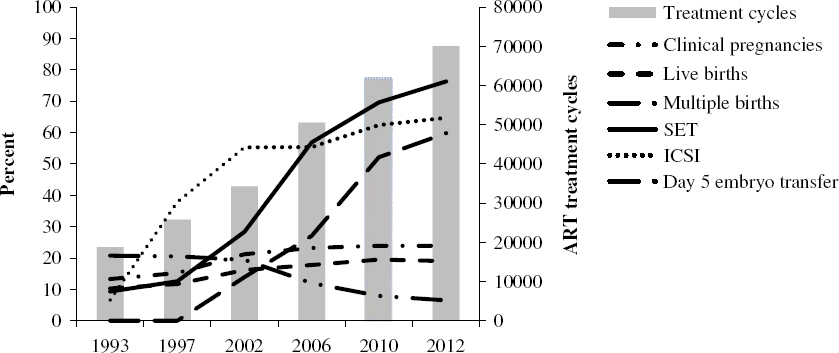
Fig. 1 Trends in assisted reproductive technologies (ART) treatments and outcomes in Australia and New Zealand, 1993–2012 (based on annual reports of the Australian and New Zealand Assisted Reproduction Database).
Treatments for infertility range from the simple oral administration of drugs to stimulate ovulation, to more invasive treatments such as IVF and ICSI that involve in vitro manipulation of gametes (oocytes and sperm). Since the first IVF birth in 1978, the field of ART has been characterized by continual and rapid innovation, and increasing success in pregnancy and live birth rates (see Fig. 1). However, this has been accompanied by ongoing concerns about the health impacts.
There is now a clear body of evidence demonstrating increased risks of poor perinatal outcomes among ART children,Reference Pinborg, Wennerholm and Romundstad 7 with evidence first emerging in 1985.Reference Lancaster 8 Historically, the risks have been attributed to an increased prevalence of multiple pregnancies arising in ART, largely due to the practice of multiple embryo transfer. However, relative to natural conceptions, ART singletons in particular have compromised health.Reference Pinborg, Wennerholm and Romundstad 7 , Reference Okun and Sierra 9 This includes our own reports of increased risks of stillbirth [odds ratio (OR) 1.82; 95% confidence interval (CI) 1.34–2.48], neonatal death (OR=2.04; 95% CI 1.27–3.26), preterm birth (OR=1.64; 95% CI 1.46–1.84), low birth weight (OR=1.98; 95% CI 1.77–2.20) and major birth defects (OR=1.30; 95% CI 1.16–1.45) among singletons conceived with any ART.Reference Davies 4 , Reference Marino, Moore and Willson 6
There is limited understanding of the causes of adverse ART outcomes. Parental characteristics related to infertility are likely to contribute to the risk of adverse outcomes including preterm birth and birth defects, which are increased in spontaneous conceptions among subfertile women.Reference Pinborg, Wennerholm and Romundstad 7 However, there is a risk from generalizing from the fertile to the infertile population as the assumed relationships may not apply. For instance, we have shown that he usual age–birth defect relationship is reversed in births after IVF and ICSI, and the associations for other maternal factors and defects vary between IVF and ICSI. The unadjusted prevalence of any birth defect was 7.1, 9.9 and 5.7% in the IVF, ICSI and natural conception groups, respectively. As expected, the risk of birth defects increased with maternal age among the natural conceptions. In contrast, for IVF and ICSI combined, relative to natural conceptions, births to women aged ⩽29 years had a higher risk [adjusted OR (aOR) 1.42; 95% CI 1.04–1.94], births to women aged 35–39 years had no difference in risk (aOR 1.01; 95% CI 0.74–1.37), and births to women aged ⩾40 years had a lower risk of defects (aOR 0.45; 95% CI 0.22–0.92).Reference Davies, Rumbold and Marino 10
Treatment-related factors, particularly ovulation induction and mode of fertilization, have also been proposed.Reference Pinborg, Wennerholm and Romundstad 7 , Reference Maheshwari, Pandey, Shetty, Hamilton and Bhattacharya 11 However, the current literature has been limited by a number of issues, including the pooling of ART exposure groups resulting in a lack of clarity about the specific aspects of treatment that may play a role. Recent meta-analyses confirm that pregnancies resulting from IVF/ICSI have worse perinatal outcomes than spontaneous conceptions, after controlling for patient factors.Reference Pinborg, Wennerholm and Romundstad 7 , Reference Hansen and Bower 12 However, as both IVF and ICSI comprise a complex set of laboratory and clinical procedures, it is difficult to determine which particular aspects of these treatments are associated with poor outcomes. For example a typical cycle of IVF or ICSI now involves: controlled ovulation induction, oocyte retrieval, fertilization (either IVF or with ICSI), embryo maturation in culture, embryo transfer and cryopreservation of excess embryos. As a result, there have been calls for research examining the specific treatment factors that are modifiable, rather than implicating IVF or ICSI overall as harmful.Reference Barnhart 13
We have previously demonstrated that the risk of adverse outcomes varied across individual treatment groups.Reference Marino, Moore and Willson 6
Relative to spontaneous conceptions, singletons from assisted conception were more likely to be stillborn (OR=1.82; 95% CI 1.34–2.48), while survivors as a group were comprehensively disadvantaged at birth, including lower birth weight (OR=2109 g; 95% CI 2129–289), very low birth weight (OR=2.74; 95% CI 2.19–3.43), very preterm birth (OR=2.30; 95% CI 1.82–2.90) and neonatal death (OR=2.04; 95% CI 1.27–3.26). The risk of neonatal death increased further for IVF singletons after fresh embryo transfer (OR=4.94; 95% CI 2.65–9.11) compared with spontaneous conceptions. Furthermore, singleton ICSI pregnancies were more likely to be complicated by pregnancy induced hypertension and an increased risk of macrosomia after embryo freezing (OR=1.54; 95% CI 1.0–2.28), which is consistent with previous studiesReference Pinborg, Henningsen, Loft, Malchau, Forman and Andersen 14 and may reflect an altered epigenetic signature in the embryo.Reference Whitelaw, Bhattacharya, Hoad, Horgan, Hamilton and Haggarty 15 Risk of major birth defects also varied substantially across treatments; for example the risk was non-significant in IVF singletons but elevated for ICSI (OR=1.55; 95% CI 1.24–1.94). We showed reduced risks of birth defects after frozen embryo cycles, particularly in ICSI (OR=1.10; 95% CI 0.65–1.85) and increased risks for non-invasive procedures involving ovulation induction drugs (OR=3.19; 95% CI 1.32–7.69). The defects were serious, including cardiac, urogenital, skeletal and neurological defects.
A limitation of our published workReference Davies 4 , Reference Marino, Moore and Willson 6 is the age of the data, as the most recent births occurred in December 2002. As a result, the findings may not be a reliable guide for contemporary practice (laboratory and clinical) because the intervening years have seen a number of significant changes in culture media, laboratory procedures and clinical practice. We have also seen an expansion of the patient group to a range of aetiologies which may alter patterns of risk over time.
Recent analysis of Nordic birth registry data for the years 1998–2007Reference Henningsen, Gissler and Skjaerven 16 identified a steep decline over time in the prevalence of preterm birth among ART singletons (~14–8%), as well as smaller declines in small for gestational age, stillbirth and infant death (in singletons and twins). The authors suggest that the improvements reflect changes in treatment mix, including greater use of SET, embryo cryopreservation, ICSI, as well as changes in the health profile of couples accessing treatment. However, the temporal trends were not analysed specifically by these factors, and so the authors could only speculate about their possible impact. There is also some evidence of improved perinatal outcomes (preterm birth, low birth weight) in more recent ART cohorts examining singleton births from IVF and ICSI.Reference Pinborg, Wennerholm and Romundstad 7 The latest of these cohorts includes ART births until 2006.Reference Sazonova, Källen, Thurin-Kjellberg, Wennerholm and Bergh 17 Therefore, there is a major gap internationally in knowledge of the safety and effectiveness of ART treatments commonly used in the most recent decade. The extent to which specific changes in ART treatment mix contribute to variation in outcomes, controlling for patient profile, is unknown. This makes it imperative to create a more contemporary datasets, in order to capture the key innovations and rapid changes in practice that have occurred, and in our case, since 2002.
The dramatic rise in the use of ICSI deserves specific comment, as it is no longer used exclusively for severe semen defects (in ~15% of cases), and now accounts for ~70% of all treatment cycles in AustraliaReference Macaldowie, Wang, Chambers and Sullivan 18 (see Fig. 1). This procedure is used to improve fertilization rates, but bypasses a number of biological checkpoints. While ICSI appears useful for assuring fertilization, there is also new evidence from the CDC in Atlanta that the ‘take home baby rate’ is actually no better after ICSI, and there are worse perinatal outcomes compared with IVF,Reference Boulet, Mehta, Kissin, Warner, Kawwass and Jamieson 19 which suggests misinformed enthusiasm for ICSI. Internationally, there have been calls for quantification of the risks of ICSI (beyond examination of pregnancy and live birth rates) when used for non-male factor infertility.Reference Barnhart 13
Within the last 10 years there has been a significant increase in elective SET, such that now it accounts for the majority (76%) of treatment cycles (see Fig. 1). This significantly reduces iatrogenic multiple birth and associated adverse outcomes.Reference Henningsen, Gissler and Skjaerven 16 , Reference van Heesch, Evers and Dumoulin 20 , Reference Toshimitsu, Nagamatsu and Nagasaka 21 It is important to examine whether the shift to use of SET in Australia has improved perinatal outcomes. First, even though SET is standard practice in Australia for younger women, multiple embryo transfer still occurs in one in four cycles. Therefore, demonstrating the benefits of SET (beyond reduction in multiple pregnancies) may increase SET uptake. Second, there is evidence that singletons born after SET have higher birth weight than singletons born after DET, and fewer neonatal deaths.Reference Okun and Sierra 9 , Reference Henningsen, Gissler and Skjaerven 16
Consistent with literature on fetal loss and birth defectsReference Pinborg, Lidegaard and Andersen 22 we have shown that following double embryo transfer, the presence of a non-progressing fetal co-twin at the 8 week ultrasound (e.g. an empty sac) is associated with a significantly increased risk of multiple major birth defects in the survivor (OR=2.78), and an overall 18% prevalence of major birth defects.Reference Davies, Rumbold and Whitrow 23 Therefore, there is a need to further clarify the risks of multiple embryo transfer, even when this practice results in a singleton birth. We propose that there will be a reduction in the risk of birth defects after SET, but specific to couples with more than one embryo available for cryopreservation.
Increasing use of cryopreservation has accompanied SET to reduce multiple pregnancy rates, the risks of low birth weight and birth defects. What is less clear from the older data is the extent to which this is due to selection bias, as in the past couples needed to have multiple high-quality embryos to successfully use cryopreservation. There has also been modification to the freezing protocols with changes in the cryoprotectant agents that the embryos are exposed to and a shift over the last 5 years away from a ‘slow’ freezing method to vitrification whereby the embryo is plunged into liquid nitrogen. More recent data, particularly from ‘freeze all’ protocols, indicate that children born following the transfer of vitrified embryos may have a higher birth weight when compared with those of fresh or slow frozen embryos.Reference Liu, Teng, Fu, Li, Zheng and Sun 24 The effect of this technique on perinatal outcomes and birth defects has not been evaluated in detail with the most recent meta-analysisReference Liu, Teng, Fu, Li, Zheng and Sun 24 reporting that only one study had included congenital abnormalities as an end-point. The meta-analysis did not address perinatal outcomes beyond live birth rates.
There has been an increased use of extended embryo culture and transfer of blastocysts (i.e. day 5 transfer) to select for longer surviving and potentially euploid embryos.Reference Vega, Breborowicz, Moshier, McGovern and Keltz 25 However, this may also alter the pattern of development, as shown by AI Kissin’s group where blastocyst transfer is associated with increased monozygotic twinning, which is a risk factor for major adverse outcomes in pregnancy and for the child.Reference Kanter, Boulet, Kawwass, Jamieson and Kissin 26 , Reference Wright, Schieve, Vahratian and Reynolds 27 Blastocyst transfer has also been associated with an increased risk of birth defectsReference Pinborg, Henningsen, Malchau and Loft 28 , Reference Kallen, Finnstrom, Lindam, Nilsson, Nygren and Olausson 29 which is proposed to occur due to non-physiologic oxygen exposure.Reference Gardner 30 Adverse perinatal outcomes were not observed in a recent Australian study,Reference Chambers, Chughtai, Farquhar and Wang 31 however, birth defects were not been examined. Therefore, whether day of transfer impacts on perinatal outcomes requires verification, while the risk for birth defects is unresolved.Reference Pinborg, Wennerholm and Romundstad 7
Changes in culture media have seen improvements in fertilization rates, and clinical pregnancy rates. Even small alterations in laboratory parameters results in altered fetal growth in utero in animal models.Reference Zander-Fox, Lane and Hamilton 32 , Reference Banwell, Lane, Russell, Kind and Thompson 33 Assessment of birth outcomes in humans is scarce and inconsistent. In three studies the composition of the culture media for embryo development to the blastocyst stage altered the birth weight of the babiesReference Kleijkers, van Montfoort and Smits 34 , Reference Eskild, Monkerud and Tanbo 35 which is contradicted in a more recent small studies.Reference Pinborg, Henningsen, Loft, Malchau, Forman and Andersen 14 , 37 We have since undertaken preliminary investigations of congenital cardiac defects in our existing cohort, and identified that a certain brand of culture media were associated with an increased risk of any cardiac defect (OR=2.56; 95% CI 1.05–6.23), and of Tetralogy of Fallot (OR=4.16; 95% CI 1.16–14.9) compared with natural conceptions, controlling for mode of conception and other treatment factors. It is imperative that these and other adverse outcomes be investigated in a contemporary context, as there have been rapid developments in culture media context in the past decade.
Conclusions
ART emerged as a ‘breakthrough’ technology that was translated successfully from animal production without the benefit of a pre-existing knowledge base in humans. A series of further changes in specific techniques have occurred in the absence of high-quality evidence on the effectiveness, beyond rapidly apparent outcomes of pregnancy and live birth rates.Reference Allen, Wilson and Cheung 36 – Reference Myers, McCrory and Mills 38 This is because of the difficulties undertaking large, well-controlled studies in this area with adequate sample size and long-term follow-up including uncommon but critically important outcomes.Reference Barnhart 13 As a consequence, there is a lack of reliable contemporary evidence on safety and effectiveness, to inform ART policy and practice internationally.
Financial Support
This research was supported by grants from the National Health and Medical Research Council (349475, 349548, 453556, and 465455) and the Australian Research Council (FT100101018).
Conflicts of Interest
None.



