Introduction
Chronic fatigue syndrome (CFS), also known as myalgic encephalomyelitis (ME), is characterized by severe and persistent fatigue, leading to functional impairment (Reeves et al., Reference Reeves, Lloyd, Vernon, Klimas, Jason, Bleijenberg and Unger2003). Other common symptoms include cognitive difficulties, unrefreshing sleep, and post-exertional malaise (PEM). Cognitive behavior therapy (CBT) aimed at factors assumed to maintain ME/CFS symptoms has been found effective in reducing fatigue and disability in seven meta-analyses (Casson et al., Reference Casson, Jones, Cassar, Kwai, Lloyd, Barry and Sandler2022; Castell, Kazantzis, & Moss-Morris, Reference Castell, Kazantzis and Moss-Morris2011; Chou, McDonagh, Griffin, & Grusing, Reference Chou, McDonagh, Griffin and Grusing2022; Malouff, Thorsteinsson, Rooke, Bhullar, & Schutte, Reference Malouff, Thorsteinsson, Rooke, Bhullar and Schutte2008; Marques, De Gucht, Gouveia, Leal, & Maes, Reference Marques, De Gucht, Gouveia, Leal and Maes2015; Price, Mitchell, Tidy, & Hunot, Reference Price, Mitchell, Tidy and Hunot2008; Smith et al., Reference Smith, Haney, McDonagh, Pappas, Daeges, Wasson and Nelson2015) and one systematic review (Ingman, Smakowski, Goldsmith, & Chalder, Reference Ingman, Smakowski, Goldsmith and Chalder2022), although one meta-analysis revised its decision to support CBT after excluding trials using one particular case definition of ME/CFS (Smith et al., Reference Smith, Nelson, Haney, Pappas, Daeges, Wasson and McDonagh2016). This decision reflects the discussion whether patients meeting different case definitions and with different symptoms respond equally to CBT. More specifically, it is unclear whether evidence about the efficacy of CBT can be generalized to patients with PEM, considered by many a central feature of ME/CFS (National Institute of Clinical Excellence [NICE], 2021). We aimed to address these issues by investigating treatment effects and moderation of CBT for ME/CFS in a meta-analysis with individual patient data (IPD). The derived evidence may inform clinical decision-making regarding whether CBT can or cannot be recommended for patients with particular symptoms or characteristics.
Many case definitions of ME/CFS (Baker & Shaw, Reference Baker and Shaw2007) exist, most of which include the presence of severe, persisting fatigue leading to disability. Case definitions differ with respect to the presence of other symptoms required. According to the 2003 revised U.S. Centers for Disease Control and Prevention (CDC) case definition of CFS (Reeves et al., Reference Reeves, Lloyd, Vernon, Klimas, Jason, Bleijenberg and Unger2003), four out of eight accompanying symptoms have to be present, while the Oxford case definition of CFS (Sharpe et al., Reference Sharpe, Archard, Banatvala, Borysiewicz, Clare, David and Wright1991) does not require the presence of accompanying symptoms. The CDC and Oxford case definitions of CFS, widely used in research, have been criticized because patients without commonly reported symptoms such as PEM, unrefreshing sleep and cognitive impairment can be unjustly classified as case. The term Systemic Exertion Intolerance Disease (SEID) (Jason et al., Reference Jason, McManimen, Sunnquist, Brown, Newton and Strand2015) in which the presence of PEM, unrefreshing sleep and cognitive impairment or orthostatic intolerance are required aside from fatigue, was proposed by the U.S. Institute of Medicine (IOM). Also, the recent UK-based NICE (2021), generally highly influential in shaping clinical practice world-wide, published a guideline proposing that ME/CFS should only be diagnosed when PEM, unrefreshing sleep and cognitive difficulties are reported. The IOM criteria for SEID and the NICE criteria for ME/CFS overlap regarding symptoms required, a 6-months delay to diagnosis is built into SEID diagnosis while this is 3 months in the NICE case definition. NICE (2021) downgraded the evidence of CBT trials not mandating PEM. The CDC (Chou et al., Reference Chou, McDonagh, Griffin and Grusing2022) concluded that the evidence for CBT was inadequate in patients diagnosed with more current case definitions.
The discussion about the response to CBT in patients fulfilling different case definitions and with different symptoms highlights the need to establish to what extent the effect of CBT varies by patient characteristics. Several patient characteristics including clinical characteristics, demographics, and cognitive-behavioral responses to symptoms have previously been studied as potential moderators of CBT for ME/CFS. Two meta-analyses (Castell et al., Reference Castell, Kazantzis and Moss-Morris2011; Malouff et al., Reference Malouff, Thorsteinsson, Rooke, Bhullar and Schutte2008) and one randomized controlled trial (RCT) (White et al., Reference White, Goldsmith, Johnson, Potts, Walwyn, Decesare and Sharpe2011) found equivalent treatment outcomes when using different diagnostic criteria. They did however not apply the SEID diagnosis or recent NICE criteria (2021). Moderator analyses of RCTs showed that the effects of CBT were larger in patients who were younger, had less avoidance of activity, were more physically active, were less symptom focused and had higher self-efficacy with respect to fatigue at baseline (Prins et al., Reference Prins, Bleijenberg, Bazelmans, Elving, De Boo, Severens and van der Meer2001; Tummers, Knoop, van Dam, & Bleijenberg, Reference Tummers, Knoop, van Dam and Bleijenberg2013). Patients with more depressive symptoms benefitted less from a minimal CBT intervention, but the effect of an individual face-to-face CBT did not differ between patients meeting the criteria of a depressive disorder and those who did not (Prins, Bleijenberg, Rouweler, & van der Meer, Reference Prins, Bleijenberg, Rouweler and van der Meer2005; Tummers et al., Reference Tummers, Knoop, van Dam and Bleijenberg2013).
Whilst these previous studies provided some insight into the extent to which the effect of CBT varies with patient characteristics, these are not sufficient to draw firm conclusions. First, RCTs are generally not adequately powered to identify moderators of the treatment effect. Second, the previously conducted meta-analyses investigated moderation on aggregate data which is prone to ecological bias (Fisher, Copas, Tierney, & Parmar, Reference Fisher, Copas, Tierney and Parmar2011). An IPD meta-analysis is the preferred method to evaluate potential moderators of intervention effects (Debray et al., Reference Debray, Moons, van Valkenhoef, Efthimiou, Hummel and Groenwold2015). The large number of raw data points facilitates testing of interactions at the patient level, conducting subsequent stratified analyses, and standardizing analytic techniques across the included studies (Fisher et al., Reference Fisher, Copas, Tierney and Parmar2011). Third, studies included in previous meta-analyses used different treatment protocols and outcomes, which may cause variation in results and conclusions drawn (Worm-Smeitink et al., Reference Worm-Smeitink, Nikolaus, Goldsmith, Wiborg, Ali, Knoop and Chalder2016). It would be preferable to include studies which not only use the same outcome measures but also apply a similar treatment protocol.
The aim of this study was therefore to investigate whether the effect of CBT v. control varied by the following patient characteristics: (1) demographic factors, (2) clinical characteristics, and (3) cognitive-behavioral factors targeted in CBT. We conducted an IPD meta-analysis on RCTs comparable with respect to the outcome measure used to assess fatigue severity, comparison condition, i.e. waiting list or care as usual, and treatment protocol.
Methods
This meta-analysis was conducted in accordance with PRISMA-IPD guidelines (Stewart et al., Reference Stewart, Clarke, Rovers, Riley, Simmonds, Stewart and Tierney2015) and is registered in PROSPERO (CRD42022358245).
Eligibility criteria
Eligible RCTs included ME/CFS patients irrespective of case definition, and randomly assigned them to either CBT or a comparison condition, i.e. waiting list or care as usual. Further, fatigue had to be assessed with the Checklist Individual Strength (CIS) fatigue severity subscale (Worm-Smeitink et al., Reference Worm-Smeitink, Gielissen, Bloot, van Laarhoven, van Engelen, van Riel and Knoop2017) and the Dutch CBT protocol for ME/CFS had to be applied (Heins et al., Reference Heins, Knoop, Prins, Stulemeijer, van Der Meer and Bleijenberg2010; Knoop & Bleijenberg, Reference Knoop and Bleijenberg2010; Prins & Bleijenberg, Reference Prins and Bleijenberg1999).
In accordance with the PRISMA-IPD statement, we performed a systematic literature search using MEDLINE, EMBASE, PsycINFO, and Web of Science, for studies satisfying our eligibility criteria, see appendix for details.
Intervention
CBT for ME/CFS (Knoop & Bleijenberg, Reference Knoop and Bleijenberg2010) is based on the cognitive-behavioral model of fatigue in ME/CFS (Vercoulen et al., Reference Vercoulen, Swanink, Galama, Fennis, Jongen, Hommes and Bleijenberg1998) which discerns between factors that trigger fatigue and cognitive-behavioral factors assumed to perpetuate the symptom and associated disability. The intervention includes goal setting, sleep management, cognitive restructuring, reducing the focus on fatigue, regulation of activities (only for patients with a fluctuating activity pattern), a time contingent gradual increase in physical activity and other activities, and accomplishment of personal goals. See appendix for a detailed description.
Outcomes and putative moderators
Primary outcome
Fatigue severity was assessed with the subscale fatigue severity of the 20-item CIS (Worm-Smeitink et al., Reference Worm-Smeitink, Gielissen, Bloot, van Laarhoven, van Engelen, van Riel and Knoop2017). The CIS-fatigue consists of eight items which are scored from 1 to 7. The total score ranges from 8 to 56, a higher score indicating more severe fatigue (Worm-Smeitink et al., Reference Worm-Smeitink, Gielissen, Bloot, van Laarhoven, van Engelen, van Riel and Knoop2017).
Secondary outcomes
Functional impairment was assessed with the Sickness Impact Profile 8 (SIP8) (Bergner, Bobbitt, Carter, & Gilson, Reference Bergner, Bobbitt, Carter and Gilson1981), which assesses overall impairment in eight domains. A higher weighted total score indicates more severe overall impairment. Physical functioning was assessed with the subscale physical functioning of the SF–36 (Stewart, Hays, & Ware, Reference Stewart, Hays and Ware1988). The weighted subscale score ranges from 0 (maximum physical limitations) to 100 (ability to do vigorous activity).
Putative moderators
Patient characteristics investigated as putative moderators were assessed at baseline and included: (1) demographic factors, (2) clinical characteristics, and (3) cognitive-behavioral factors targeted in CBT. The demographic factors were age and sex. Clinical characteristics were duration of fatigue, functional impairment, symptoms that pertain to different case definitions of ME/CFS, total number of symptoms met which are mentioned in the CDC case definition, clinically relevant level of depressive symptoms, pain severity and impact, and case definition met (CDC, NICE and/or SEID). The CDC case definition is met if a patient is severely fatigued for a period of at least 6 months, leading to substantial functional impairment, without a known medical explanation, and reports four out of eight additional symptoms. Both the SEID and NICE case definition use being severely fatigued for a period of at least 3 months (NICE) or 6 months (SEID), leading to substantial functional impairment, without a known medical explanation and the presence of PEM, unrefreshing sleep and cognitive problems as criteria. The cognitive-behavioral factors were self-efficacy, focus on bodily symptoms, catastrophizing, sleep problems and sleep-wake pattern, and physical activity pattern.
Statistical analyses
One-stage IPD meta-analyses were conducted to study the effect of CBT v. control conditions on the primary outcome fatigue and secondary outcomes functional impairment and physical functioning and to examine moderators of the effect. The effects of CBT v. control were evaluated by regressing the post-intervention value of the outcome on condition adjusted for the baseline value using linear mixed model analyses. The models included a random intercept and a random slope on study level to account for clustering within studies. Effect sizes, expressed in Cohen's d, were calculated by dividing the between-group estimated marginal means by the pooled standard deviation (s.d.) of the second assessment and interpreted as small (0.2), medium (0.5) and large (0.8) (Cohen, Reference Cohen1992).
To investigate clinical relevance of main effects, we determined the number of patients who were no longer severely fatigued, i.e. scoring < 35 (adults) or < 40 (adolescents) on the CIS-fatigue (Worm-Smeitink et al., Reference Worm-Smeitink, Gielissen, Bloot, van Laarhoven, van Engelen, van Riel and Knoop2017); no longer functionally impaired, i.e. scoring < 700 on the SIP8 (Bergner et al., Reference Bergner, Bobbitt, Carter and Gilson1981); or no longer impaired in physical functioning, i.e. scoring > 70 on the SF-36 subscale physical functioning (Stewart et al., Reference Stewart, Hays and Ware1988) at the second assessment. We compared the percentages of patients in CBT with the control condition by calculating relative risks with 95% confidence intervals (CI).
To examine whether the effect of CBT v. control was moderated by patient characteristics, the potential moderator and its interaction with condition (CBT v. control) were added to the regression models. To prevent ecological bias for patient-level interactions, we centered the individual values of potential moderators around their mean study values (Debray et al., Reference Debray, Moons, van Valkenhoef, Efthimiou, Hummel and Groenwold2015). The putative moderators were examined one-by-one in separate models. We considered a characteristic to be a moderator if the likelihood ratio test (LRT) indicated a statistically significant improvement (p < 0.05) of the model fit by adding the interaction term. Regression coefficients and 95% CI of the interaction tests are reported.
When a significant moderator was identified, the intervention effects were studied within moderator subgroups which were based on validated cut-off points or a median split.
All analyses were performed on complete cases. Moderator effects of physical activity were investigated without data of the study of Prins et al. (Reference Prins, Bleijenberg, Bazelmans, Elving, De Boo, Severens and van der Meer2001), because this study used an earlier version of the treatment protocol not distinguishing between patients with a low and fluctuating activity pattern.
For the description of our sensitivity analyses, see appendix.
Analyses were conducted in R version 4.0.3, with the packages lme4 and lmtest. The R code is provided in the appendix.
Results
Eight RCTs (Janse, Worm-Smeitink, Bleijenberg, Donders, & Knoop, Reference Janse, Worm-Smeitink, Bleijenberg, Donders and Knoop2018; Knoop, van der Meer, & Bleijenberg, Reference Knoop, van Der Meer and Bleijenberg2008; Nijhof, Bleijenberg, Uiterwaal, Kimpen, & Putte, Reference Nijhof, Bleijenberg, Uiterwaal, Kimpen and Putte2012; Prins et al., Reference Prins, Bleijenberg, Bazelmans, Elving, De Boo, Severens and van der Meer2001; Stulemeijer, de Jong, Fiselier, Hoogveld, & Bleijenberg, Reference Stulemeijer, de Jong, Fiselier, Hoogveld and Bleijenberg2005; Tummers, Knoop, van Dam, & Bleijenberg, Reference Tummers, Knoop, van Dam and Bleijenberg2012; van der Schaaf et al., Reference van der Schaaf, Schmits, Roerink, Geurts, Toni, Roelofs and Knoop2015; Wiborg, van Bussel, van Dijk, Bleijenberg, & Knoop, Reference Wiborg, van Bussel, van Dijk, Bleijenberg and Knoop2015) fulfilled our eligibility criteria. Their IPD were obtained allowing us to include all studies in this IPD meta-analysis. All studies were from our own research group. No additional RCTs from other researchers fulfilling our eligibility criteria were found. See the appendix for details of the selection process. In a risk of bias analysis, four studies were classified as having ‘some concerns’ with respect to risk of bias, three as ‘high risk of bias’, and one could not be assessed as the outcome paper has not been published yet (van der Schaaf et al., Reference van der Schaaf, Schmits, Roerink, Geurts, Toni, Roelofs and Knoop2015). See the appendix for details on the risk of bias analysis. See Table 1 and the appendix for study characteristics.
Table 1. Study characteristics
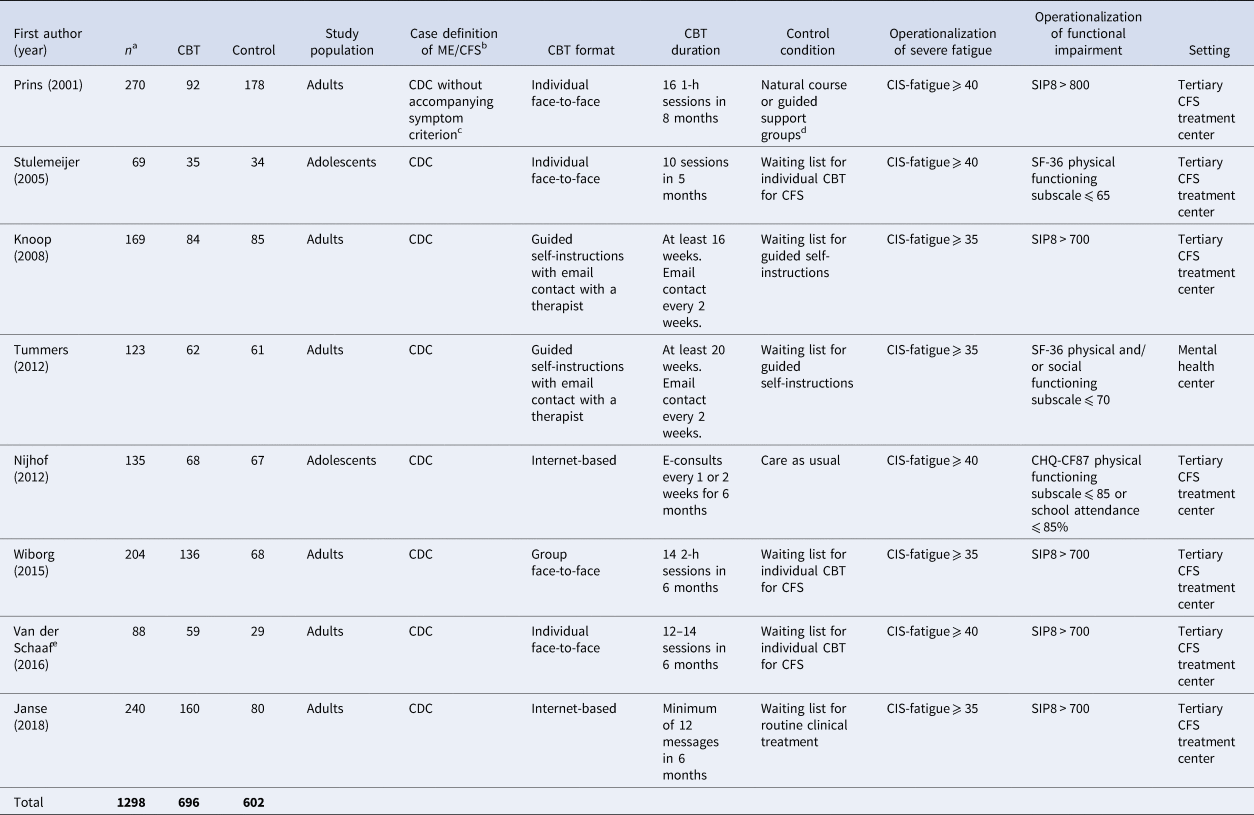
a The same patients as analyzed in the original studies were included in this study.
b As proposed by the NICE guideline 2021 the term ME/CFS is used throughout the text. Only when we refer to a specific case definition we use the specific term used for this definition.
c 18 patients were included with the diagnosis idiopathic chronic fatigue instead of ME/CFS, i.e. reporting less than 4 accompanying symptoms.
d We considered the natural course group as equivalent to the waiting list/care as usual comparison of the other studies. We added the support group condition, which had similar outcomes as the natural course group, to the comparison condition.
e Of this study, baseline data have been reported but data on the efficacy of the treatment have not yet been published.
CBT, cognitive behavior therapy; CDC, Centers for Disease Control and Prevention; CHQ-CF87, Child Health Questionnaire (Raat, Landgraf, Bonsel, Gemke, & Essink-Bot, Reference Raat, Landgraf, Bonsel, Gemke and Essink-Bot2002); CIS-fatigue, Fatigue severity subscale of the Checklist Individual Strength (Worm-Smeitink et al., Reference Worm-Smeitink, Gielissen, Bloot, van Laarhoven, van Engelen, van Riel and Knoop2017); ME/CFS, myalgic encephalomyelitis/chronic fatigue syndrome; SF-36, Short Form Health Survey (Stewart et al., Reference Stewart, Hays and Ware1988); SIP8, Sickness Impact Profile 8 (Bergner et al., Reference Bergner, Bobbitt, Carter and Gilson1981).
The total sample consisted of 1298 patients, see Table 2 for all sample characteristics. Data on the second assessment were missing for 106 patients (8.2%) on the primary outcome fatigue severity, for 89 patients (9.2%) on functional impairment, and 78 patients (8.7%) on physical functioning.
Table 2. Baseline characteristics
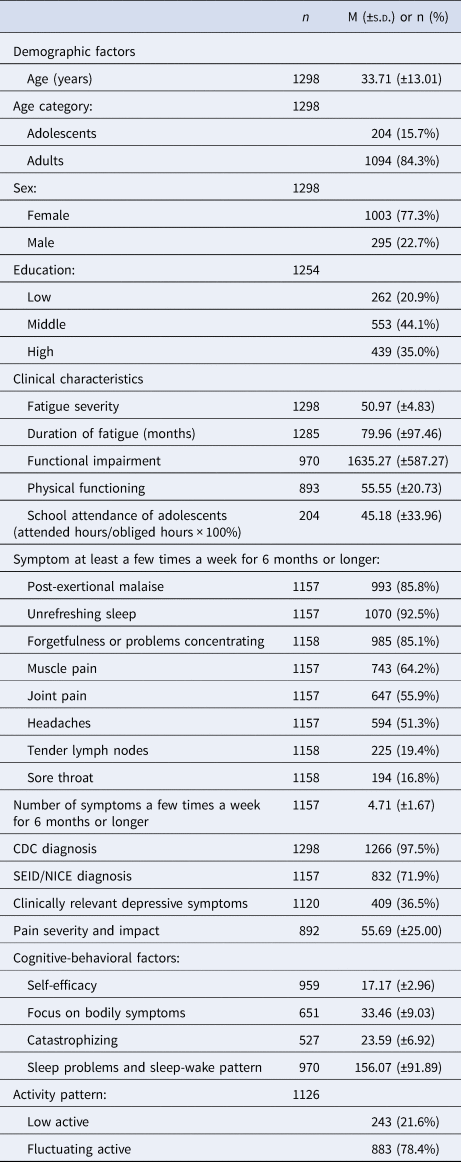
For all used measures, see appendix.
CDC, Centers for Disease Control and Prevention; M, mean; NICE, National Institute of Clinical Excellence; S.D., standard deviation; SEID, Systemic Exertion Intolerance Disease.
See Table 3 for the effect of CBT v. control on all outcomes. CBT showed beneficial effects on fatigue severity (β = −11.46, 95% CI −15.13 to −7.79); p < 0.001, functional impairment (β = −448.40, 95% CI −625.58 to −271.23), p < 0.001; and on physical functioning (β = 9.64, 95% CI 3.30 to 15.98), p < 0.001. Relative risk analyses showed that CBT leads more often to a clinically relevant reduction of fatigue and functional impairment, and improved physical functioning than the control condition.
Table 3. Effect of CBT v. control
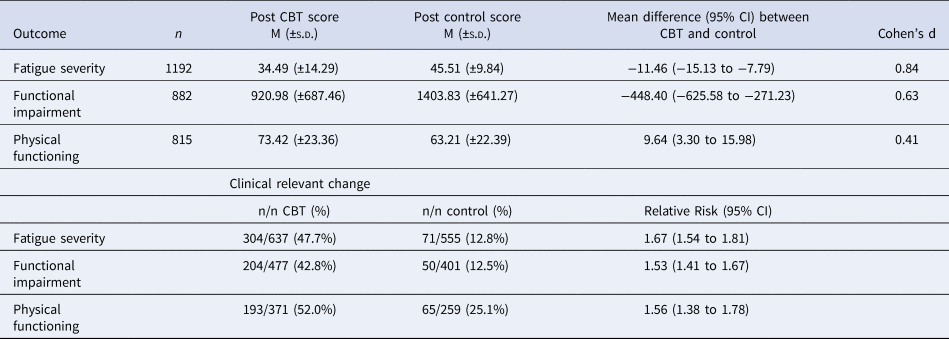
CBT, cognitive behavior therapy; CI, confidence interval; M, mean; s.d., standard deviation.
Table 4 presents the results of the moderation analyses, i.e. the extent to which effects of CBT v. control varied by patient characteristics. In Fig. 1, results of subgroup analyses for the identified moderators are presented. Of the demographic factors, the effect of CBT v. control on fatigue severity varied by age (p interaction = 0.003). Adolescents benefitted most from CBT (β = −18.35, 95% CI −22.08 to −14.62), followed by young adults (β = −11.61, 95% CI−15.57 to −7.65), and relatively older adults (β = −7.93, 95% CI −11.24 to −4.62).
Table 4. Moderator effects on fatigue severity, functional impairment and physical functioninga
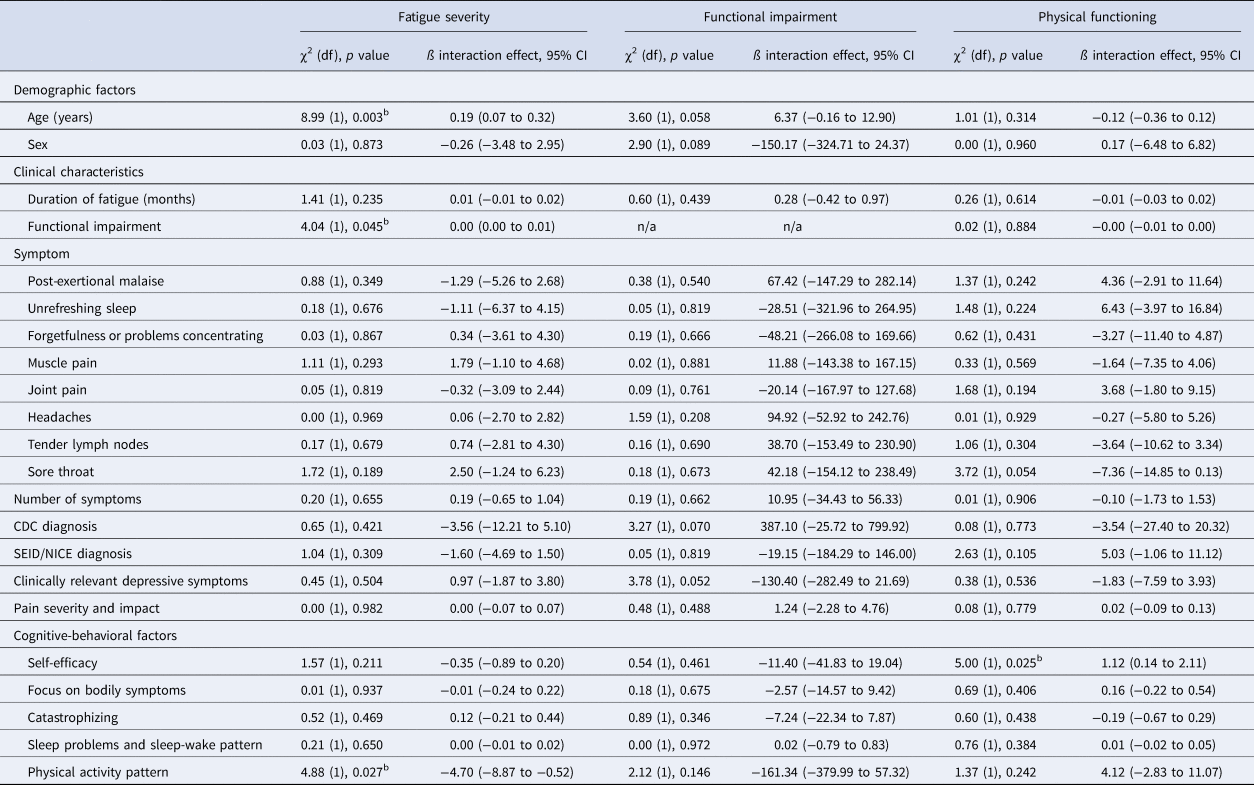
CDC, Centers for Disease Control and Prevention; CI, confidence interval; n/a, not applicable; NICE, National Institute of Clinical Excellence; SEID, Systemic Exertion Intolerance Disease.
a χ2 tests with corresponding degrees of freedom, p values, regression coefficient and 95% CI are presented.
b p < 0.05. For all used measures, see appendix.
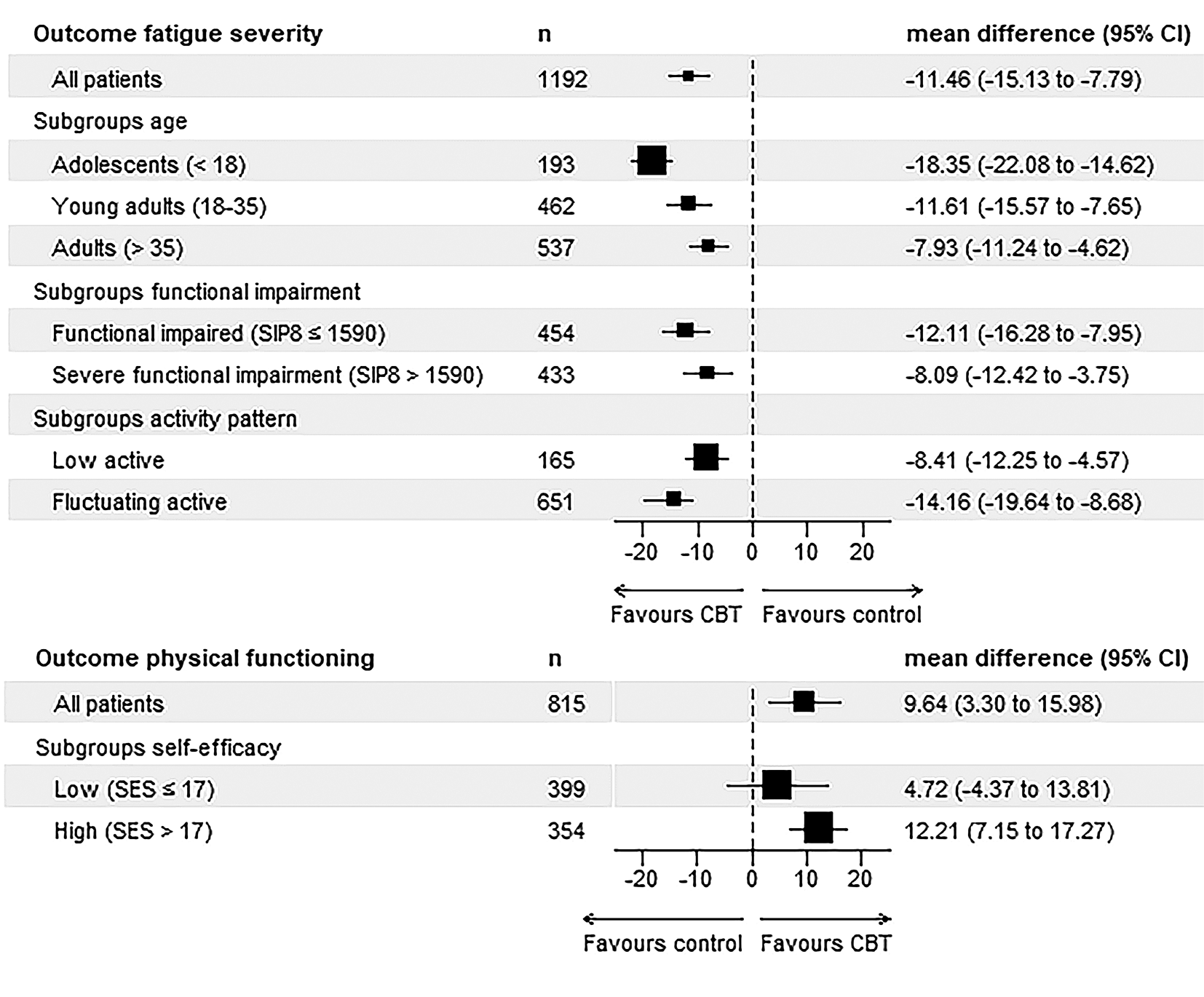
Figure 1. Effect of CBT v. control in subgroups on outcomes fatigue severity and physical functioning. CBT, cognitive behavior therapy; CI, confidence interval; SES, Self Efficacy Scale (Prins et al., Reference Prins, Bleijenberg, Bazelmans, Elving, De Boo, Severens and van der Meer2001); SIP8, Sickness Impact Profile 8 (Bergner et al., Reference Bergner, Bobbitt, Carter and Gilson1981). No figure for the outcome functional impairment is displayed as no moderation effect on this outcome was found.
Of the clinical characteristics, the effect of CBT v. control on fatigue varied by functional impairment (p interaction = 0.045). Effects were larger in patients with less functional impairment (β = −12.11, 95% CI −16.28 to −7.95) than in patients with severe functional impairment (β = −8.09, 95% CI −12.42 to −3.75).
Of the cognitive-behavioral factors, the effect of CBT v. control on physical functioning varied by self-efficacy (p interaction = 0.025). CBT resulted in a significant improvement in physical functioning in the subgroup of patients with a high self-efficacy at baseline (β = 12.21, 95% CI 7.15 to 17.27) while there was no significant effect of CBT in patients with a low self-efficacy (β = 4.72, 95% CI −4.37 to 13.81). The effect of CBT v. control on fatigue severity further varied by activity pattern (p interaction = 0.027) with patients with a fluctuating activity pattern benefitting more (β = −14.16, 95% CI −19.64 to −8.68) than patients with a low activity pattern (β = −8.41, 95% CI −12.25 to −4.57).
Results of all sensitivity analyses showed the same pattern of findings, see appendix.
Discussion
CBT leads to a significant and clinically relevant reduction of fatigue and functional impairment, and improvement of physical functioning in ME/CFS patients. This is in accordance with findings of one systematic review (Ingman et al., Reference Ingman, Smakowski, Goldsmith and Chalder2022) and of seven previous meta-analyses using aggregate data (Casson et al., Reference Casson, Jones, Cassar, Kwai, Lloyd, Barry and Sandler2022; Castell et al., Reference Castell, Kazantzis and Moss-Morris2011; Chou et al., Reference Chou, McDonagh, Griffin and Grusing2022; Malouff et al., Reference Malouff, Thorsteinsson, Rooke, Bhullar and Schutte2008; Marques et al., Reference Marques, De Gucht, Gouveia, Leal and Maes2015; Price et al., Reference Price, Mitchell, Tidy and Hunot2008; Smith et al., Reference Smith, Haney, McDonagh, Pappas, Daeges, Wasson and Nelson2015). Our IPD meta-analysis showed that age, functional impairment and physical activity pattern moderated the effect of CBT on the outcome fatigue severity. Self-efficacy moderated the effect of CBT on physical functioning, and was the only patient characteristic associated with non-response to CBT on one of the three outcomes of interest, i.e. physical functioning. No moderators for the outcome functional impairment were found.
This IPD meta-analysis does not support the assumption that CBT is less effective in subgroups of patients meeting different case definitions for ME/CFS or in patients with often occurring symptoms aside from fatigue. Our findings do not support the decision of NICE to downgrade evidence from studies not mandating the presence of PEM in their updated guideline. And they are in line with previous studies finding no effect of case definition on the treatment effect of CBT (Castell et al., Reference Castell, Kazantzis and Moss-Morris2011; Malouff et al., Reference Malouff, Thorsteinsson, Rooke, Bhullar and Schutte2008; White et al., Reference White, Goldsmith, Johnson, Potts, Walwyn, Decesare and Sharpe2011).
The moderating effect of CBT on fatigue severity of age showed that younger patients benefitted more with adolescents benefitting most. This replicates findings of a previous study (Tummers et al., Reference Tummers, Knoop, van Dam and Bleijenberg2013). One might assume that the relationship between older age and longer symptom duration is an explanation for this result. However, symptom duration did not moderate the effect of CBT in our IPD meta-analysis.
Functional impairment also moderated the effect of CBT on fatigue severity, with patients with less severe functional impairment benefitting more as compared to patients with severe functional impairment. This also replicates previous findings (Knoop et al., Reference Knoop, van Der Meer and Bleijenberg2008). Severe functional impairment may reflect more severe disease and this subgroup of patients might need additional interventions or more intensive treatment.
Regarding the moderating effect of cognitive-behavioral factors hypothesized to perpetuate ME/CFS symptoms it was found that patients with a low self-efficacy did not benefit from CBT with respect to physical functioning. A low level of self-efficacy was the only characteristic associated with non-response to CBT on an outcome. As this subgroup still reported significant treatment gains with respect to fatigue severity and functional impairment, CBT seems to remain an appropriate treatment for them. A low level of self-efficacy may be associated with more severe symptoms. We did not correct for symptom severity in determining the relation between self-efficacy and outcome. Alternatively, low self-efficacy may make it more challenging to engage in the behavior changes incorporated within CBT for ME/CFS.
Patients with a low activity pattern benefitted from CBT with respect to fatigue severity, but less than patients with a fluctuating activity level. This indicates further work is needed in developing interventions for patients with a low activity level. This echoes the findings of a recent study in which patients with extreme avoidance and resting behavior benefitted less from CBT for fatigue in long-term medical conditions (de Gier et al., Reference de Gier, Picariello, Slot, Janse, Keijmel, Menting and Knoop2022).
Some characteristics previously found as a predictor or moderator of the outcome of CBT, did not moderate the effect of CBT in the current study. Pain has been repeatedly found as a predictor of treatment success (Cella, Chalder, & White, Reference Cella, Chalder and White2011; Collin, Heron, Nikolaus, Knoop, & Crawley, Reference Collin, Heron, Nikolaus, Knoop and Crawley2018; Knoop, Stulemeijer, Prins, van der Meer, & Bleijenberg, Reference Knoop, Stulemeijer, Prins, van der Meer and Bleijenberg2007), but apparently pain predicts a less favorable prognosis irrespective of CBT. Further, a previous study found severity of depressive symptoms to be a moderator of the effect in a minimal CBT intervention (Tummers et al., Reference Tummers, Knoop, van Dam and Bleijenberg2013), while patients with a depressive disorder were not less responsive to individual face-to-face CBT (Prins et al., Reference Prins, Bleijenberg, Rouweler and van der Meer2005). Clinically relevant depressive symptoms were not found as a moderator in this study. It might be that other factors influence the effects of treatment in depressed patients, for example treatment format.
Our study has several strengths. It is an IPD meta-analysis, the preferred method to evaluate potential moderators of intervention effects. By including eight RCTs with a similar design resulting in a large sample size, our study was adequately powered.
This first conducted IPD meta-analysis on CBT for ME/CFS has also limitations. We investigated multiple putative moderators and outcomes, which increased the chance on type I errors due to multiple testing. However, in research investigating moderation with IPD, often a more liberal p value, i.e. p = 0.10, is used to make sure no putative moderator is missed. We decided to apply a p value of 0.05, to reduce the risk of type I error. Further, we wanted to prevent a type II error, i.e. missing a putative moderator in order to wrongly conclude that CBT might be recommended for a subgroup which in fact does not benefit from CBT.
To reduce heterogeneity in this IPD, we used specific eligibility criteria regarding the outcome measure used and the CBT protocol applied. As a result, a substantial number of RCTs investigating CBT for ME/CFS, e.g. the PACE trial (White et al., Reference White, Goldsmith, Johnson, Potts, Walwyn, Decesare and Sharpe2011), were excluded. Replication of our results with studies using other treatment protocols and other measures of fatigue is warranted.
In all included trials, a specific CBT protocol was used. All CBT protocols for ME/CFS are based on the cognitive-behavioral model of fatigue assuming that cognitive-behavioral factors perpetuate fatigue and associated disability. They generally focus on similar perpetuating factors. Further, all CBT protocols for ME/CFS contain graded exposure to activity, a central element of the intervention. There are also differences between protocols as can be expected with a complex intervention (Worm-Smeitink et al., Reference Worm-Smeitink, Nikolaus, Goldsmith, Wiborg, Ali, Knoop and Chalder2016). They can differ in which perpetuating factors are addressed and in how these are influenced during CBT. However, the different protocols have more similarities than differences. Therefore, it is likely that our findings are generalizable to other CBT protocols of CBT for ME/CFS.
There are many different case definitions proposed and used to diagnose ME/CFS and we only investigated moderation related to CDC and SEID/NICE criteria. Previous research, however, showed considerable overlap between case definitions (Lim & Son, Reference Lim and Son2020). Therefore, it is likely that the absence of moderation will also be found when other case definitions are applied. Another limitation pertains to our operationalization of the SEID diagnosis without orthostatic intolerance, which was not assessed. This might have led to an underestimation of the number of patients meeting the SEID criteria but including orthostatic intolerance as a criterion would make finding moderation even more unlikely.
Further, accompanying symptoms that pertain to different case definitions, including PEM, were assessed with a single item based on patient report. For PEM, multi-item assessments like the Fatigue and Energy Scale (Keech et al., Reference Keech, Sandler, Vollmer-Conna, Cvejic, Lloyd and Barry2015) do exist. However, single-item measures can be as valid and reliable as multi-item measures (Allen, Iliescu, & Greiff, Reference Allen, Iliescu and Greiff2022).
Another limitation is that none of the included studies were rated as having a low risk of bias. All included studies used patient-reported outcomes, namely subjectively experienced symptoms and functional impairments. All case definitions of ME/CFS rely on reports of patients of subjectively experienced symptoms. Therefore the efficacy of interventions aimed at symptoms of ME/CFS can only be determined with patient-reported outcome measures. Further, all included studies used care as usual or waiting list as comparison condition. A placebo condition matched with respect to the attention given and offering of a treatment rationale is preferable to rule out that effects of CBT are non-specific. However, in one of the included studies (Prins et al., Reference Prins, Bleijenberg, Bazelmans, Elving, De Boo, Severens and van der Meer2001) the outcomes of the guided support group, an active control condition, were significantly different from the CBT condition, the latter being more favorable. In all included studies blinding was not possible because both patient and therapist were aware of the allocated treatment. In the Cochrane risk of bias tool studies are penalized if the outcome assessor (the patient) was aware of the intervention received. However, this limitation is inherent to the evaluation of behavioral/psychotherapeutic interventions using a subjective outcome measure.
In sum, CBT leads to a significant reduction of fatigue and functional impairment, and to improvement of physical functioning in ME/CFS patients. There is no indication that subgroups of ME/CFS with certain patient characteristics do not respond to CBT.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291723003148
Author's contributions
TAK drafted this article, which was supervised by HK, FM and AMJB. TAK and IC collated the data. TAK and IC performed the statistical analyses, which was supervised by LMB. TAK and IC conducted the search. FM and PN conducted the risk of bias analysis. All authors edited the manuscript. All authors read and approved the final manuscript.
Funding statement
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Competing interests
HK and GB receive royalties for a published manual of CBT for ME/CFS. TAK, LMB, AMJB, IC, PN, RMM, FM declare no competing interests.
Ethical standards
An ethics statement is not applicable because this study is based exclusively on published literature.








