Introduction
According to the World Health Organziation (WHO), 18% of children and adolescents globally are overweight and obese. 1 Childhood obesity often persists into adolescence and is predictive of adulthood obesity. Reference Biro and Wien2 Today, 39% of adults globally are obese 3 placing them at significant risk for other noncommunicable diseases (NCDs) including type 2 diabetes, mental illness, cancer, and cardiovascular disease. Reference Biro and Wien2 Early child obesity preventative initiatives are increasingly warranted. Expert opinion suggests obesity management approaches require a shift from focusing primarily on individual behavior change Reference Teixeira, Carraça and Marques4,Reference Epstein, Valoski, Wing and McCurley5 to also targeting modifiable factors that have been fueling the “obesogenic environment”. The pathogenesis of obesity can be rooted in various life systems as outlined by the biopsychosocial model of health 6,Reference Marmot7 and can include personal, economic, social, and environmental factors.
There is ever-growing evidence that exclusive breastfeeding (EBF) may be protective of obesity development in children. Reference Yan, Liu, Zhu, Huang and Wang8 The Developmental Origins of Health and Disease (DOHaD) describes chronic disease origins through programming during fetal development and early infancy where the first 1000 days of life are sensitive to epigenetic changes. Reference Godfrey, Costello and Lillycrop9 Preliminary research has shown that excess gestational weight gain and increased preconception adiposity significantly influences early childhood adiposity measures. Reference Oken, Taveras, Kleinman, Rich-Edwards and Gillman10,Reference Godfrey, Reynolds and Prescott11 Since the critical windows span from the prenatal to postnatal period, it is understandable why maternal growth patterns during pregnancy and lactation are relevant to the risk of childhood obesity. To comprehensively examine the relationship between maternal preconception-pregnancy body mass index (BMI), breastfeeding behaviors and early childhood growth trajectories we conducted a scoping review. Understanding the modifiable influence of maternal weight status and infant feeding behaviors on childhood obesity trajectories, coupled with risk factors in multilevel systems will enable the effective characterization of prevention strategies and aid in informing early targeted interventions.
Methods
A scoping review was conducted to analyze data from longitudinal cohorts which discuss maternal BMI status in conjunction with breastfeeding and their association with the risk of childhood obesity. We selected the scoping review study design as its framework allowed us to identify and synthesize a broad range of evidence. The Arksey and O’Malley scoping review framework was used to guide the literature search and review process and included the following steps: (1) identifying the research question; (2) identifying relevant studies; (3) study selection; (4) charting the data; (5) collating, summarizing, and reporting the results; and an optional stage (6) consultation with experts and stakeholders. Reference Arksey and O’Malley12 For consistency, transparency, and reproducibility, an a priori review protocol was developed, Reference Abrego Del Castillo, Wamithi, Dennis and Lye13 registered, and embargoed on Open Science Framework (OSF) on August 19, 2019. The findings of this review are reported following the Preferred Reporting Items for Systematic Review and Meta-Analysis for Scoping Reviews (PRISMA-ScR) guidelines. Reference Tricco, Lillie and Zarin14
Data sources and search strategies
After formulating the research question and review objectives, a literature search was conducted to identify relevant studies in MEDLINE Ovid, EMBASE (Excerpta Medica database) Ovid and CINAHL EBSCO (Cumulative Index to Nursing & Allied Health Elton B. Stephens Co.), and PubMed from January 1, 2009, to March 17, 2021. A search strategy was created with the assistance of an experienced librarian for MEDLINE using text keywords and the following Medical Subject Headings (MeSH) terms with Boolean operators in order to maximize the combinations of terms scoped: “Child Development,” “Pediatric obesity,” “overweight,” “body mass index,” “breastfeeding,” and “gestational weight gain”. The search was modified for the additional electronic databases; Table S1 outlines the search syntax and strategy.
Inclusion criteria and study selection
Titles and abstracts identified from the search strategy were screened for relevancy by two authors and full-text articles reviewed for eligibility based on the inclusion criteria. Covidence, a systematic review software, was used to allow collaboration among reviewers. Review articles were not included but the reference lists of identified relevant reviews were scanned and relevant research studies identified were screened. At both stages of screening consistency of inclusion and exclusion were evaluated. Interrater agreement was tested with a subset of articles using Cohen’s kappa until substantial agreement was reached. Reference Landis and Koch15 Records were screened independently and in the event of an unsolvable discrepancy a third team member was consulted. Eligible studies were included if the following criteria were met: (1) longitudinal research studies that pertained to singleton pregnancies; (2) maternal BMI (exposure) and child BMI between the age of two and eighteen (outcome) were reported according to WHO 16–18 or Centers for Disease Control and Prevention (CDC) 19,20 classifications; (3) peer-reviewed; (4) in the English language; and (5) contained a subgroup of children who were breastfed. Studies were excluded from full text-review if (1) the exposure variables of interest (maternal BMI and breastfeeding) were not independent variables and (2) the full text was not available. Since quality assessment of the included studies was beyond the objectives of a scoping review, Reference Arksey and O’Malley12,Reference Levac, Colquhoun and O’Brien21 we forewent this aspect of analysis.
Data extraction
Data extraction was completed using customized Covidence data extraction forms to chart variables and summary statistics. Key data extraction variables were informed by the Joanna Briggs Institute (JBI) manual 22 and the Arksey and O’Malley framework. Reference Arksey and O’Malley12 The analysis structure and organizational hierarchy was created to characterize major themes identified from the review according to Bronfenbrenner’s theory of ecological systems in which human development unfolds. Reference Bronfenbrenner23,Reference Brofenbrenner24 Findings were further reported through a life course approach Reference Heikkinen25 beginning with preconception variables.
Results
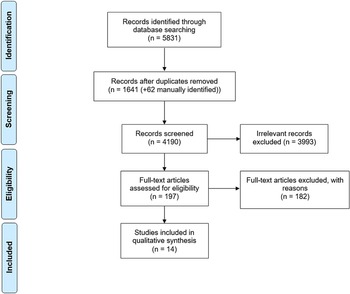
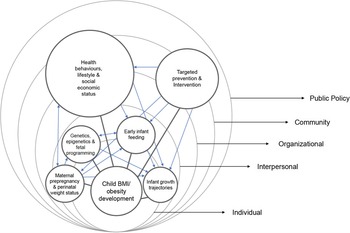
Of the 7384 records identified, 4190 records remained after removing duplicates and applying date restrictions resulting in 197 studies proceeding to full-text screening of which 14 met the review inclusion criteria (Fig. 1 PRISMA diagram). Reference Tricco, Lillie and Zarin26,Reference Shamseer, Moher and Clarke27 Characteristics of the included studies are presented in Table 1. The included studies were conducted primarily in the United States (US) (n = 5), Reference Gannon, Pollock, Allen and Kling28–Reference Weden, Brownell and Rendall33 Australia (n = 2), Reference Bell, Yew, Devenish, Ha, Do and Scott34,Reference Iguacel, Chung, Gearon, Moreno, Peeters and Backholer35 and Spain (n = 2), Reference Iguacel, Escartín and Fernández-Alvira36,Reference Ortega-García, Kloosterman and Alvarez37 while the remaining studies were carried out in Chile, Reference Rios-Castillo, Cerezo, Corvalán, Martínez and Kain38 Kuwait, Reference Al-Qaoud and Prakash39 Netherlands, Reference Sirkka, Vrijkotte and Halberstadt40 Turkey, Reference Ardic, Usta, Omar, Yildiz and Memis41 and the United Kingdom (UK). Reference Fairley, Santorelli and Lawlor42 The common primary outcome of the included studies were child and adolescent (ranging from 2 to 15 years of age) overweight/obese weight status (defined by WHO 43 or CDC 20 standards) and BMI status (measured as z-score, SDS, and/or percentiles). The studies examined the outcome primarily among maternal-child dyads, although three studies included paternal variables, Reference Ventura, Loken and Birch30,Reference Iguacel, Chung, Gearon, Moreno, Peeters and Backholer35,Reference Iguacel, Escartín and Fernández-Alvira36 with independent early life risk factors including health behaviors, ethnicity, income, parental anthropometrics, infant feeding practices, and childhood growth (Table S2). Each risk factor was organized into one of the five levels of influence (Fig. 2) of which eight studies identified organizational, community and/or policy risk factors affecting childhood obesity indirectly. All studies reported maternal BMI as the most significant predictor of overweight and obesity in children. The protective effect of breastfeeding was observed in a majority of the included studies (n = 8).

Fig. 1. PRISMA flow diagram of records throughout review process. Adapted From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. doi: 10.1371/journal.pmed1000097.
Table 1. Characteristics of included studies

1 Wang X, Martinez MP, Chow T, Xiang AH. (2020) examines the same cohort and variables as Bider-Canfield, Z. et al., (2017) for this reason it is being considered an extension of the earlier 2017 study and collectively examined as 1/14 of the included records.
a Iguacel I, et al. (2018) corresponds to reference #35.
b Iguacel I, et al. (2018) corresponds to reference #34.
Data collected from Covidence data extraction sheets.
N/A = Not applicable.
Definitions of full and exclusive breastfeeding vary across studies.
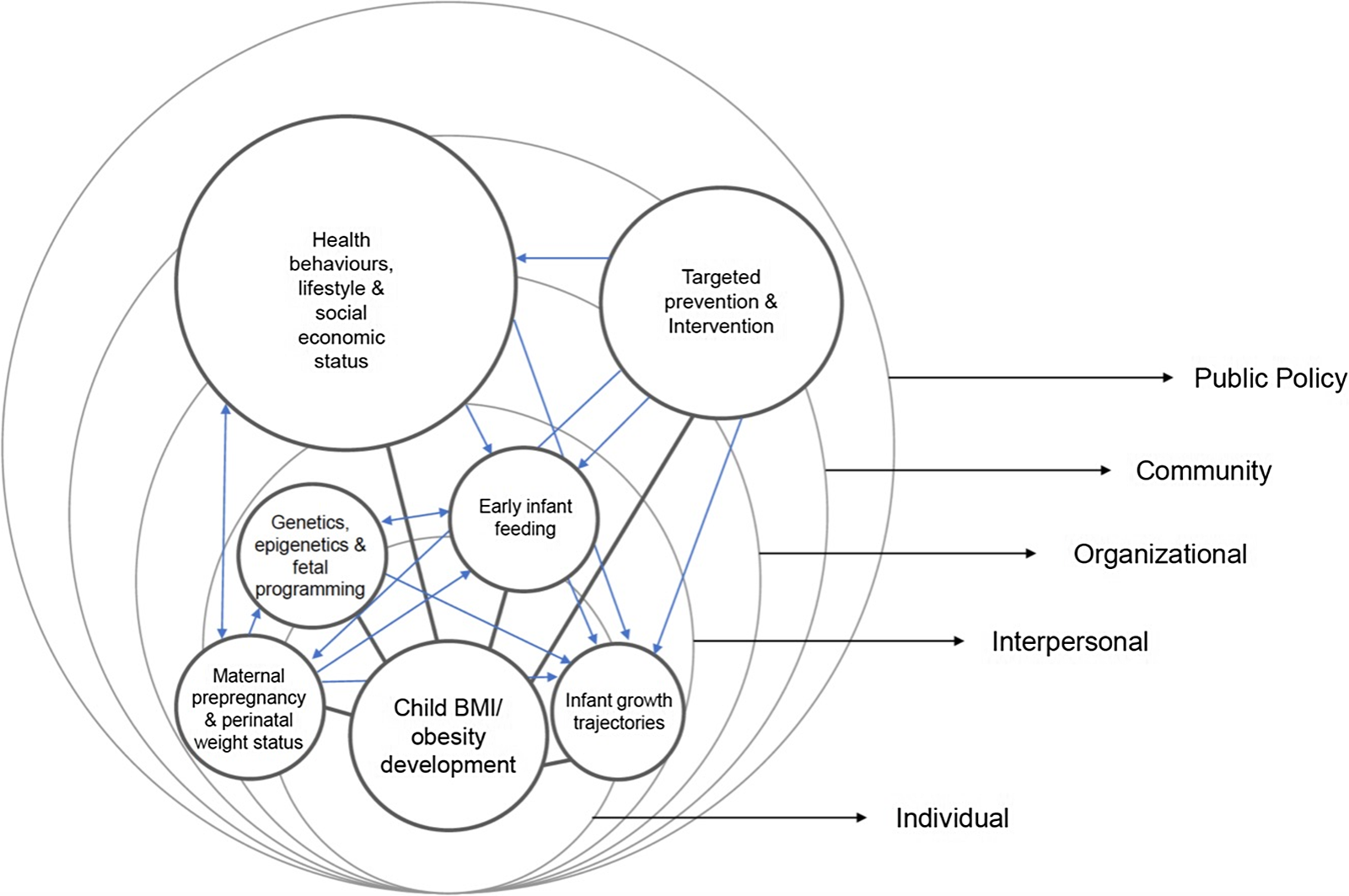
Fig. 2. Schematic of important themes to childhood obesity and their interactions on a multilevel system. Each arrow represents the interrelationship between the themes and their direction of influence. Size of the themes does not represent magnitude, but their reach across the multilevel systems.
Healthy behaviours lifestyle and social economic status
Eight studies examined the relationship between maternal smoking and child obesity of which five found significant results (Table S2). Reference Demment, Haas and Olson29,Reference Bell, Yew, Devenish, Ha, Do and Scott34–Reference Ortega-García, Kloosterman and Alvarez37 Children whose mother smoked were significantly more likely to develop obesity than those not exposed to maternal smoking. Three studies attributed this relationship to fetal programming. Reference Bell, Yew, Devenish, Ha, Do and Scott34,Reference Iguacel, Escartín and Fernández-Alvira36,Reference Ortega-García, Kloosterman and Alvarez37 One study found the relationship between maternal smoking and child growth trajectory was mediated by birth weight. Reference Demment, Haas and Olson29 Three studies reported family eating practices influenced child eating patterns and food preferences. Reference Weden, Brownell and Rendall33,Reference Ardic, Usta, Omar, Yildiz and Memis41,Reference Fairley, Santorelli and Lawlor42 In a US study of 4815 children, Black children were significantly less likely to have daily family dinners together and more likely to have a higher BMI when compared to White children. Reference Weden, Brownell and Rendall33 In a UK study, indulgent caregiver feeding style was related to a significantly higher child BMI z-score. Reference Fairley, Santorelli and Lawlor42 Three studies highlighted the influence of parental and child sedentary behaviors (e.g., TV viewing time, physical inactivity) on child growth trajectories. Reference Demment, Haas and Olson29,Reference Bell, Yew, Devenish, Ha, Do and Scott34,Reference Al-Qaoud and Prakash39
Children who were from families that reported a low social economic status (SES) and identified as belonging to a Black, Indigenous and People of Colour (BIPOC) groups are significantly more likely to have poor health behaviours (e.g., maternal smoking, excess parental weight, and sedentary lifestyles). Reference Weden, Brownell and Rendall33 In an Australian study of 2186 families, a significant negative relationship was found between low SES, maternal smoking, maternal overweight/obesity, paternal overweight/obesity, shorter breastfeeding duration, and early introduction to solid foods, all which have been implicated in the development of childhood obesity. Reference Iguacel, Chung, Gearon, Moreno, Peeters and Backholer35 Six studies found that children whose mothers had lower education achievement, were of low SES, and lived in low-income housing were significantly more likely to have a higher BMI and be classified overweight or obese; these children were also more likely to be of Hispanic or Black ethnicity. Reference Demment, Haas and Olson29,Reference Wang, Martinez, Chow and Xiang32–Reference Bell, Yew, Devenish, Ha, Do and Scott34,Reference Ortega-García, Kloosterman and Alvarez37,Reference Sirkka, Vrijkotte and Halberstadt40
Parental preconception anthropometrics and perinatal weight status
Regardless of SES or ethnicity, all 14 studies found maternal preconception and perinatal BMI consistently predicted childhood obesity. Women who were overweight were twice as likely to have a child who was also overweight or obese compared to children from normal weight women; this risk increased even further when the mother was obese supporting a genetic and fetal programming interrelationship. Three studies examined the influence of paternal BMI and found that paternal overweight or obesity status also increased the risk for child obesity when compared to normal weight fathers. Reference Ventura, Loken and Birch30,Reference Iguacel, Chung, Gearon, Moreno, Peeters and Backholer35,Reference Iguacel, Escartín and Fernández-Alvira36 Further, there is growing evidence that maternal excess gestational weight gain (EGWG), as defined by WHO/IOM, 44 influences child growth trajectories. Two cohort studies conducted in the US and Chile reported EGWG was significantly more likely among women who were overweight and obese Reference Bider-Canfield, Martinez and Wang31,Reference Wang, Martinez, Chow and Xiang32,Reference Rios-Castillo, Cerezo, Corvalán, Martínez and Kain38 and in a US study, children whose mothers experienced EGWG were twice as likely to be overweight BMI trajectory between the ages of 2 and 15. Reference Demment, Haas and Olson29
Genetics, epigenetics and fetal programming
Environmental factors can result in intergenerational epigenetic changes to the developing fetus which can alter metabolic trajectories over the lifespan. Four studies examined the effect of parental ethnicity and found children who were Hispanic and Spanish Roma compared to other ethnicities; Reference Iguacel, Escartín and Fernández-Alvira36 Turkish compared to Dutch; Reference Sirkka, Vrijkotte and Halberstadt40 Black compared to White; Reference Weden, Brownell and Rendall33 and White compared to Pakistani Reference Fairley, Santorelli and Lawlor42 were more likely to have high BMI z-scores or be overweight and obese, respectively. It was hypothesized that overweight and obesity risk was enhanced in these ethnicities due to the exposure to a great number of risk factors such as lower SES, shorter breastfeeding durations, high parental BMI, and maternal smoking. Reference Iguacel, Escartín and Fernández-Alvira36,Reference Fairley, Santorelli and Lawlor42 While none of the review studies included genetic data, the social trends found suggest epigenetic changes among these ethnicities may be attributable to weight gain through family health behaviors that promote obesogenic environments.
Early infant feeding
Recent studies suggest early infant feeding practices such as breastmilk intake and solid food introduction have lasting effects on child weight status in later life. Two studies reported breastfeeding duration was significantly shorter among women with obesity when compared to those who were normal weight. Reference Bider-Canfield, Martinez and Wang31,Reference Iguacel, Chung, Gearon, Moreno, Peeters and Backholer35 Four studies found a shorter duration of breastfeeding, predominantly defined as less than 6 months postpartum, significantly increased a child’s obesity risk. Reference Gannon, Pollock, Allen and Kling28,Reference Ventura, Loken and Birch30–Reference Wang, Martinez, Chow and Xiang32,Reference Rios-Castillo, Cerezo, Corvalán, Martínez and Kain38 Four studies found that when breastfeeding was not exclusive there was no significant protection and the risk of being overweight/obese remained. Reference Demment, Haas and Olson29,Reference Iguacel, Escartín and Fernández-Alvira36,Reference Al-Qaoud and Prakash39,Reference Fairley, Santorelli and Lawlor42 The importance of breastfeeding exclusivity to the recommended 6 months was demonstrated in four studies. Reference Bell, Yew, Devenish, Ha, Do and Scott34,Reference Ortega-García, Kloosterman and Alvarez37,Reference Sirkka, Vrijkotte and Halberstadt40,Reference Ardic, Usta, Omar, Yildiz and Memis41 These studies observed that when children were exclusively breastfed for ≥6 months they were less likely to become overweight or obese. A dose–response relationship was reported between breastfeeding and risk of child overweight/obesity. Reference Weden, Brownell and Rendall33,Reference Bell, Yew, Devenish, Ha, Do and Scott34,Reference Ortega-García, Kloosterman and Alvarez37 Six studies examined the effect of complementary feeding of which four studies found a significant result. Reference Bell, Yew, Devenish, Ha, Do and Scott34,Reference Al-Qaoud and Prakash39–Reference Ardic, Usta, Omar, Yildiz and Memis41 Solid food introduction before 5–6 months was also found to be an obese risk factor, Reference Bell, Yew, Devenish, Ha, Do and Scott34,Reference Al-Qaoud and Prakash39,Reference Sirkka, Vrijkotte and Halberstadt40 while the delay of formula introduction was seen to reduce the risk of overweight and obesity. Reference Ortega-García, Kloosterman and Alvarez37
Infant growth trajectories
Five studies examine the effects of birthweight on child obesity of which four found a significant relationship. Reference Gannon, Pollock, Allen and Kling28,Reference Bell, Yew, Devenish, Ha, Do and Scott34,Reference Rios-Castillo, Cerezo, Corvalán, Martínez and Kain38,Reference Al-Qaoud and Prakash39 Three studies reported rapid infant weight gain to be associated with adverse weight status and metabolic outcomes. Reference Demment, Haas and Olson29,Reference Ventura, Loken and Birch30,Reference Iguacel, Escartín and Fernández-Alvira36 Children who had a rapid weight gain, determined by age specific weight z-scores from birth to 6 months, were almost four times more likely to be obese at 6 years of age in comparison to those who did not have an early rapid weight gain. Reference Iguacel, Escartín and Fernández-Alvira36 Similar results were seen at 15 years of age, when weight-for-length from birth to 2 years was rapid Reference Demment, Haas and Olson29 and when rapid weight gain occurred between the ages of 5 and 9 years. Reference Ventura, Loken and Birch30 One study observed that when rapid infant weight gain occurred in females their high BMI trajectories were accompanied by increased fat mass and adverse total cholesterol, low-density lipoprotein cholesterol, insulin resistance, fasting insulin, triglyceride levels, and blood pressure. Reference Ventura, Loken and Birch30
Targeted prevention and intervention
Ten studies highlighted the need for early targeted intervention of modifiable risk factors among preconception women as well as those during pregnancy. Reference Gannon, Pollock, Allen and Kling28,Reference Demment, Haas and Olson29,Reference Bider-Canfield, Martinez and Wang31,Reference Weden, Brownell and Rendall33–Reference Iguacel, Escartín and Fernández-Alvira36,Reference Sirkka, Vrijkotte and Halberstadt40,Reference Fairley, Santorelli and Lawlor42 A Netherland study found infant feeding and child BMI differ according to risk groups, encouraging the need for group-specific interventions. Reference Sirkka, Vrijkotte and Halberstadt40 An Australian study suggested that interventions that promote healthy lifestyles and behaviors may aid in reducing socioeconomic inequalities in excessive child weight gain. Reference Iguacel, Chung, Gearon, Moreno, Peeters and Backholer35 To limit the accumulative load of early life risk factors, one study suggested to preemptively intervene by summing the early life risk factors and use their cumulative risk as predictive tool. Reference Gannon, Pollock, Allen and Kling28 Some of the included studies describe two risk factors that are important to public health strategies, (1) the promotion of sustained EBF Reference Weden, Brownell and Rendall33,Reference Bell, Yew, Devenish, Ha, Do and Scott34 and (2) supporting healthy weight gain among parents Reference Bider-Canfield, Martinez and Wang31,Reference Weden, Brownell and Rendall33,Reference Iguacel, Escartín and Fernández-Alvira36 to prevent childhood obesity. The collective call for early intervention effectively summarizes the community and policy influences on childhood obesity and how they are essential in helping prevent childhood obesity.
Discussion
This scoping review is the first to examine maternal anthropometrics and breastfeeding behaviors together and their effect on childhood growth trajectories. Of 4190 eligible records, 14 records met the final inclusion criteria and were reviewed. The scoping review found parental preconception, pregnancy BMI, and breastfeeding behaviours to significantly influenced to child obesity rates. All studies included found maternal BMI to be the most significant predictor of childhood overweight or obesity. The strength of the influence of maternal BMI over other early life risk factors likely correlates with the direct influence of the gestational environment and a mother’s control of the early postnatal environment, both of which occur during early critical developmental periods. Reference Godfrey, Costello and Lillycrop9,Reference Kuzawa and Thayer45,Reference Arenz, Rückerl, Koletzko and von Kries46 More than half of the included studies found breastfeeding had a protective effect on child obesity. Reference Gannon, Pollock, Allen and Kling28,Reference Ventura, Loken and Birch30–Reference Bell, Yew, Devenish, Ha, Do and Scott34,Reference Ortega-García, Kloosterman and Alvarez37,Reference Sirkka, Vrijkotte and Halberstadt40,Reference Ardic, Usta, Omar, Yildiz and Memis41 The studies in which breastfeeding was not found to be protective breastfeeding was poorly defined and did not conform with WHO standards. 47 The importance of exclusivity and duration of breastfeeding was confirmed in this review and is consistent with previous research where child obesity risk was found to be dose-dependent with duration of exclusive breastfeeding. Reference Yan, Liu, Zhu, Huang and Wang48 Many of the studies also identify risk factors across the early life course and at multiple levels of influence that can help in successful targeted intervention programs. Finally, this review identified other modifiable and nonmodifiable key risk factors of childhood obesity, those of which encompass healthy lifestyle behaviors as well as sociodemographic variables. Six risk factor themes were identified in this review which were consistent with a socioecological perspective Reference Bronfenbrenner23 to provide excellent guidance in the future development of prevention strategies based on modifiable factors.
Several of the risk factors identified that are modifiable include maternal smoking status, Reference Demment, Haas and Olson29,Reference Wang, Martinez, Chow and Xiang32–Reference Ortega-García, Kloosterman and Alvarez37,Reference Fairley, Santorelli and Lawlor42 preconception weight, gestational weight gain, and family feeding styles. Maternal smoking has been linked to childhood obesity as it exposes the developing fetus to intrauterine smoke which has been associated with fetal undernutrition, growth retardation, Reference Oken, Levitan and Gillman49 and low birth weight. 50 Intrauterine smoke exposure has also been discovered to alter the appetite regulation of the fetus, Reference Oken, Levitan and Gillman49,Reference Moschonis, Grammatikaki and Manios51 leading to dysregulated eating patterns and fatty food preferences later in life. In terms of gestational weight gain, keeping within the guidelines for weight gain during pregnancy is recommended, recognizing that previous work has found limited to moderate impact of interventions to manage gestational weight gain. Reference Ruchat, Mottola and Skow52,Reference Shieh, Cullen, Pike and Pressler53 Nevertheless, staying within the recommended guidelines should be encouraged through regular monitoring during pregnancy as well as education preconceptionally. Dietary factors related to childhood obesity revolve around breastfeeding and solid food introduction, in which caregivers have a key role. It has been suggested that women with obesity are more likely to provide their children with more “adult” like food at an earlier age increasing their adiposity risk. Reference Brophy, Cooksey and Gravenor54 Early food intake has been associated with the early cessation of EBF, Reference Grummer-Strawn, Scanlon and Fein55,Reference Dennis56 as well as an increased caloric intake at a young age. 57 Additionally, studies have shown that married couples are at an increased risk of obesity if their partner is or becomes obese, Reference Cobb, McAdams-Demarco and Gudzune58 suggesting that there may be an obesogenic environmental influence on familial weight patterns that requires further exploration in its potential impact on how obesogenic environments may further increase the risk or mitigate the predisposition for infants. The role of culture was seldom explored in these studies despite culture often dictating health behaviors.
Other risk factors identified were nonmodifiable such as our finding that children of obese parents have a higher risk of becoming obese themselves implies a genetic transmission of obesity. This may occur via obesity-related genes with the ability to alter appetite control as seen through neuropeptide Y (NPY) gene expression in the brain, Reference Zain, Mohamed, Jalaludin, Fauzi, Hamidi and Zaharan59,Reference Hunt, Hasstedt and Xin60 or through adiposity related genes such as the (fat mass and obesity) FTO gene altering BMI trajectories. Reference Wu, Lye and Briollais61,Reference Abarin, Yan Wu, Warrington, Lye, Pennell and Briollais62 Despite genetic endowment being a nonmodifiable risk factor, variants in the FTO gene and other genes implicated in the risk of high BMI are mitigated by EBF. Reference Wu, Lye and Briollais61 While beyond the scope of this review, existing work suggests that infant gut microbiome could be important pathway between maternal BMI, breastfeeding, and infant growth. Reference Kapourchali and Cresci63,Reference Woo and Martin64 Future work is needed to understand this specific relationship more.
Another modifiable risk factors could be through long-term upstream approaches that requires systematic changes to dismantle disparities. Risk factors posed by sociodeterminants of health such as race, ethnicity, and low-income status are typically influenced by larger social systems rendering it important to acknowledge the risks stemming from health equity and social justice. Reference Braveman, Cubbin, Egerter, Williams and Pamuk65 Weden et al. Reference Weden, Brownell and Rendall33 found Black children were disproportionately exposed to short breastfeeding durations in comparison to Whites leading to increased risk of being overweight or obese. However, further work is needed to understand the role that systematic racism plays in shorter durations of breastfeeding and what changes are necessary to remove barriers for breastfeeding for at risk families. In addition to, and potentially combined with, race, familial SES and maternal employment commitments during the early postnatal periods have the potential to create an obesogenic environment for children affecting infant feeding, physical activity and childcare. The risk to childhood obesity may be socially patterned which cannot be address unless taken from a system-wide, population-level change to dismantle racism and other barriers. Identifying group-specific targeted interventions for groups disproportionately at high-risk might provide early opportunities to protect a child from modifiable exposures in their environment. Reference Demment, Haas and Olson29,Reference Bell, Yew, Devenish, Ha, Do and Scott34
It is evident that childhood obesity may be a result of a transgenerational transmission, via maternal weight status, parental genetics, ethnicity, and SES. High growth trajectories may persist if they are reinforced by adverse health behaviors and family eating practices, which are often socially patterned according to income and ethnicity. Without early intervention these children, may carry high BMI into adulthood and reproduce the next generation of offspring with similar growth patterns. The implementation process becomes complex because of the need to elucidate potential mechanisms to understand why certain components of a multilevel intervention were ineffective. Reference MacKinnon, Fairchild and Fritz66 However, wide-reaching intervention to various high-risk groups would be dependent on further evidence of effectiveness.
Rather than adopting a traditional approach where obesity is targeted at an individual level, these findings support a holistic approach in which interventions and policies target common risk factors across the life course. Interventions that have been suggested throughout the literature include monitoring early infant rapid weight gain, Reference Iguacel, Escartin and Fernandez-Alvira67 encouraging healthy parental weight, Reference Ventura, Loken and Birch30,Reference Iguacel, Chung, Gearon, Moreno, Peeters and Backholer35,Reference Iguacel, Escartin and Fernandez-Alvira67 healthy gestational weight gain, Reference Bider-Canfield, Martinez and Wang31 and increased support and promotion of breastfeeding. Reference Bider-Canfield, Martinez and Wang31,Reference Weden, Brownell and Rendall33 Close members of the mother’s support network (e.g., partner and maternal grandmother) are among the most influential sources for her decision to initiate and maintain EBF behaviours, Reference Mok, Multon and Piguel68 but are not often included in breastfeeding promotion programs. The effectiveness of such programs would likely be improved by including a mother’s support network. Our review has shown children who are exposed to an increased number of risk factors are more likely to be overweight and obese compared to those who have no risk factors. Reference Iguacel, Escartin and Fernandez-Alvira67 These results were not seen in children who were 2 or 4 years old suggesting early obesity intervention in the first year of life might reduce long-term risk exposure. The role of ethnicity and the influence of social determinants of health were examined but additional research is need to develop preventive interventions that are culturally sensitive. A multilayered system of health and disease links genetic inheritance, nutrition and diet; physical inactivity; food security; cultural practice and traditions; and policy to childhood obesity. Though the common risk factor approach is used widely in public health, empirical data supporting a multitiered, targeted approach are not yet available. However, at least one of the studies included in the review calls for a similar approach to tackle common risk factors. Reference Gannon, Pollock, Allen and Kling28
Limitations
Despite numerous strengths of this review, including a systematic approach and the inclusion of studies that use statistical logistic regression analysis to estimate the strength of the relationship between risk factors and child obesity, our review also has a few limitations. Due to the nature of the scoping review, our study did not assess the quality of the studies that were analyzed. Our review also only included longitudinal observational cohorts; inherently, this study design is limiting as causal inferences cannot be made. An RCT study design would be more effective in providing the highest quality of evidence and minimizing bias. Future reviews would be strengthened by including RCT study designs as an inclusion criterion. It is likely that our results regarding breastfeeding protection were discordant due to the fact the many modes of breastfeeding may vary according to sociocultural practice Reference Scott and Binns69 and for this reason, the definition of exclusive, nonexclusive, full- or any breastfeeding can differ based on culture and region. The universal adoption of the definition of exclusive and nonexclusive breastfeeding would allow for better comparison and analysis between studies. Finally, we acknowledge our synthesis was based on outcomes reported as BMI measurements of growth or weight status, because we did not consider other measurements of weight or fat mass the generalization of our results may be limited.
Conclusions
Maternal overweight and obesity coupled with an obesogenic environment can lead to an intergenerational cycle of obesity accompanied by consequential comorbidities. Thus, there is a need to prioritize obesity prevention efforts during early critical periods of development and target multiple levels of influence, especially community and policy levels for cooperation and support in providing effective programs to families of varying risk. Interventions should focus on promoting exclusive breastfeeding, healthy weight gain, and healthy lifestyle behaviours that can aid in the healthy development of their children. Due to inconsistent uptake of the universal definition of exclusive breastfeeding, the protective effects on childhood obesity require further research. Future studies should gather evidence that exclusive breastfeeding may moderate the risk of obesity in different high-risk populations. Addressing these research gaps may provide policy makers and stakeholders with the necessary evidence to make informed programs aimed at decreasing the risk of early childhood obesity.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S2040174421000726
Acknowledgments
We would like to thank Kaitlin Fuller, MLIS, University of Toronto Libraries for training and informing KA on how to develop a rigorous search strategy methodology for the review. Thanks to all reviewers during the screening process. Gratitude is also extended to KA’s supervisory committee: SL CLD, LB, and PM. All authors edited and revised manuscript. All authors read and approved the final manuscript.
Financial support
The study was supported by funds from the Canadian Institutes for Health Research (FDN-143262). Kayla Abrego received the University of Toronto Physiology Research Studentship grant.
Conflicts of interest
None.