In recent years patients' participation in medical decisions regarding their care has been strongly advocated leading to a ‘shared’ decision-making process as opposed to the traditional approach of ‘doctor knows best’. Examples are the model of ‘shared decision-making’ Reference Charles, Gafni and Whelan1 and the concept of ‘concordance’. Reference Weiss and Britten2 Both consider the consultation as an information exchange of two experts, patient and doctor, with the aim of reaching concordant treatment decisions. Patients engaged in the decision-making process show greater satisfaction and collaboration. Reference Cox, Stevenson, Britten and Dundar3,Reference Swanson, Bastani, Rubenstein, Meredith and Ford4 Patient and public involvement are of interest also at policy-level in different countries. Reference Härter and Loh5 In the UK, the central government has invested considerable financial resources in the National Health Service to encourage initiatives to promote patient and public involvement. 6 In Italy, the importance of patient participation is recognised in the National Health Plan 2006–08: ‘Health services have to assess expectations and priorities of patients… and involve patients in treatment plans by means of a shared decision-making approach…’. 7
Shared decision-making concepts have been studied in different medical settings Reference Towle, Godolphin, Grams and Lamarre8,Reference Shepherd, Tattersall and Butow9 and for the assessment of patient involvement performance of doctors the OPTION (observing patient involvement) scale has been developed. Reference Elwyn, Hutchings, Edwards, Rapport, Wensing, Cheung and Grol10 In psychiatry this topic is still in its infancy. Reference Hamann, Leucht and Kissling11–Reference Goossensen, Zijlstra and Koopmanschap13 Poor treatment adherence among people with psychiatric illness Reference Nosè, Barbui and Tansella14 and their demands for more information and a collaborative relationship with their psychiatrist Reference Paccaloni, Pozzan and Zimmermann15,Reference McCabe, Heath, Burns and Priebe17 point to the potential importance of shared decision-making skills in psychiatry and the need to examine the extent to which decisions are shared in routine psychiatric practice.
The aims of this study were to assess how psychiatrists involve their patients in the decision-making process, and to explore the association of the observed involvement with patient and psychiatrist characteristics.
Method
Participants
All 17 psychiatrists (10 males), all with at least 3 years of psychiatric practice working in the South Verona community mental health service (CMHS), gave written informed consent to audiotape some of their out-patient consultations. In order to encourage their participation in the study they were asked to indicate the day(s) on which they would be available for audiotaping and were free to decide the number of consultations they wished to contribute. Psychiatrists were naïve to the concepts we were measuring and had received no formal training in shared decision-making techniques. They were asked to perform a first out-patient consultation as usual and were told that the audiotapes would be used to study the ways of responding to patients' reported problems. No other suggestions or information was given. The study was approved by the local ethics committee. The mean age of the psychiatrists was 38 years (range 29–57, s.d.=9.7); the mean years of psychiatric practice was 10.8 years (range 3–32, s.d.=9.2). The number of audiotaped consultations for each psychiatrist ranged from 1 to 11 with a mean of 5.
The 91 selected patients attended the out-patient service between December 2003 and March 2004, either for the first time or for a new illness episode, but were all new to the psychiatrists. Eighty-four patients gave written informed consent to be audiotaped. Four consenting patients seen by one psychiatrist were excluded because of poor audiotape quality so that the final sample comprised the consultations of 80 patients conducted by 16 psychiatrists.
The study was restricted to first contact appointments, a situation that typically included the exploration of patient's problems and decision about treatment, and would ensure sample homogeneity and minimise selection bias. The CMHS run by the Section of Psychiatry and Clinical Psychology of the Department of Medicine and Public Health at the University of Verona is the main agency providing comprehensive psychiatric care for the adult population.
The OPTION scale
The OPTION scale is a 12-item rating scale developed by Elwyn et al Reference Elwyn, Hutchings, Edwards, Rapport, Wensing, Cheung and Grol10 to evaluate the extent to which clinicians involve patients in the decision-making process. It is based on qualitative studies of the skills that according to practitioners are required in order to involve patients in decision-making processes, with reference to the conceptual framework of shared decision-making. Reference Charles, Gafni and Whelan1 The scale is applied by trained raters to audio or videotaped consultations or transcripts of consultations. The items refer to the distinct patient involvement abilities of the doctor, operationally defined (Table 1). In summary, it examines whether problems are well defined, whether options are formulated, information provided, patient understanding and role preference evaluated, and decisions examined from both the professional and patient perspective. The items are rated on a five-point scale: 0 corresponding to ‘behaviour not observed’; 1, ‘a minimal attempt is made to exhibit the behaviour’; 2, ‘the behaviour is observed and a minimum skill level achieved’; 3, ‘the behaviour is exhibited to a good standard’; and 4, ‘the behaviour is exhibited to a very high standard’. The total score ranges from 0 (0 in all items) to 48 (4 in all items) and is transformed into a 0–100 score.
Table 1 Distribution of the OPTION scores per item in the 80 interviews

| OPTION score | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Item | Not observed 0 n (%) | Minimal attempt 1 n (%) | Minimum skill level 2 n (%) | Good standard 3 n (%) | High standard 4 n (%) | ||||
| 1. The clinician draws attention to an identified problem as one that requires a decision-making process | 2 (2.5) | 25 (31.2) | 39 (48.8) | 7 (8.8) | 7 (8.8) | ||||
| 2. The clinician states that there is more than one way to deal with the identified problem | 46 (57.5) | 24 (30) | 6 (7.5) | 3 (3.8) | 1 (1.2) | ||||
| 3. The clinician assesses the patient's preferred approach to receiving information to assist decision-making | 80 (100) | 0 | 0 | 0 | 0 | ||||
| 4. The clinician lists ‘options’, which can include the choice of ‘no action’ | 17 (21.2) | 25 (31.3) | 29 (36.2) | 6 (7.5) | 3 (3.8) | ||||
| 5. The clinician explains the pros and cons of options to the patient | 24 (30) | 28 (35) | 15 (18.8) | 12 (15) | 1 (1.2) | ||||
| 6. The clinician explores the patient's expectations about how the problems are to be managed | 28 (35) | 17 (21.2) | 25 (31.3) | 7 (8.8) | 3 (3.7) | ||||
| 7. The clinician explores the patient's concerns about how the problem(s) are to be managed | 46 (57.5) | 14 (17.5) | 10 (12.5) | 6 (7.5) | 4 (5) | ||||
| 8. The clinician checks that the patient has understood the information | 15 (18.7) | 32 (40) | 24 (30) | 9 (11.3) | 0 | ||||
| 9. The clinician offers to the patient explicit opportunities to ask questions during the decision-making process | 5 (6.2) | 68 (85) | 6 (7.5) | 1 (1.3) | 0 | ||||
| 10. The clinician elicits the patient's preferred level of involvement in decision-making | 69 (86.2) | 11 (13.8) | 0 | 0 | 0 | ||||
| 11. The clinician indicated the need for a decision-making (or deferring) stage | 1 (1.3) | 29 (36.3) | 46 (57.5) | 4 (5) | 0 | ||||
| 12. The clinician indicates the need to review the decision (or deferment) | 13 (16.2) | 39 (48.8) | 15 (18.7) | 10 (12.5) | 3 (3.8) | ||||
The scale has been applied in observational and intervention studies Reference Elwyn, Edwards, Hood, Robling, Atwell, Russell, Wensing and Grol18–Reference Loh, Simon, Hennig, Hennig, Harter and Elwyn20 and is generic enough for use it in all types of medical consultations. The original version of the scale has been validated in general practice and shows acceptable psychometric characteristics, particularly reliability, with kappa scores between 0.45 and 0.98, an intraclass correlation coefficient (ICC) for the total score of 0.77 and Cronbach's alpha coefficient of 0.79. Reference Elwyn, Hutchings, Edwards, Rapport, Wensing, Cheung and Grol10 The Italian version of the scale has also been validated in a general practice setting showing satisfactory psychometric properties (kappa scores between 0.29 and 0.73, ICC on total score 0.85 and Cronbach's alpha coefficient 0.82). Reference Goss, Fontanesi, Mazzi, Del Piccolo, Rimondini and Zimmermann21 Goossensen et al Reference Adams and Drake12 confirmed the internal consistency of the scale in psychiatry reporting a Cronbach's alpha of 0.73.
Measures
For the psychiatrists the key descriptive variables were age, gender, years of psychiatric practice and length of consultation (number of words as an approximate index).
The patient data obtained from the South Verona psychiatric case register were age, gender, marital status, living conditions, occupational status, previous psychiatric contacts and diagnosis (ICD–10 22 ). The main problem reported by the patient during the consultation was noted and used as the index problem in the OPTION scale.
Procedure
The audiotaped consultations were fully transcribed. The interrater reliability of the OPTION scale was assessed on a random subsample of 30 consultations (one to four interviews per psychiatrist) which were rated independently by two raters trained in the use of the scale. After establishing satisfactory reliability indices, one rater rated the remaining 50 consultations.
Statistical analysis
Interrater agreement was calculated using weighted Cohen's kappa and percentages of agreement on each OPTION item. Intraclass correlation coefficient Reference Gleason23 and concordance coefficient Reference Lin24 were performed on the OPTION total score. Internal consistency was measured by inter-item correlations, item-total correlations and Cronbach's alpha, and was performed on the whole sample. Histogram and boxplot of the OPTION score distributions were drawn to represent the patient involvement performance of the psychiatrists.
The associations between OPTION scores and patient and psychiatrist variables were assessed by Pearson's correlation coefficient for the continuous variables (age, years of psychiatric practice, length of the consultation), by t-test (with Welch's approximate degree of freedom in case of unequal variances) or by ANOVA for the categorical variables (gender, index problem, psychiatrist) and intracluster correlation coefficient. Analyses were preformed using the software STATA 8.2 for Windows. Reference Strull and Charles25
Results
Patient and consultation characteristics
The majority of patients were female (61%, 49/80), married (41%, 33/80), employed (45%, 36/80) and had received a primary or secondary school level of education (59%, 47/80). Mean age was 43.6 years (range 23–76, s.d.=13). About a half of the patients were return patients but were seeing this psychiatrist for the first time (53%, 42/80). Clinical problems, as identified by the OPTION ‘index problem’, were mainly anxiety symptoms (55%, 44/80) and depressive disorders (39%, 31/80). The diagnoses according to ICD–10 were panic and phobic anxiety disorders (36%, 29/80), depressive reaction or depressive episodes (33%, 26/80), mixed anxiety and depressive disorder (14%, 11/80). The mean length of the interviews was 4245 words (range 711–9582, s.d.=1989) which corresponds roughly to 40 min (10 min for every 1000 words approximately).
Interrater reliability and internal consistency of the OPTION scale
The percentage agreement between the two raters for the single OPTION items was between 77% and 95% (mean 80.8%). Mean weighted Cohen's kappa was 0.57 (range 0.22–0.81). Pearson's correlation coefficient for the total score was 0.96, the corresponding ICC 0.95, and the concordance coefficient (Lin's rho) 0.95. Inter-item correlation coefficient was 0.35 and item-total correlation ranged from 0.43 to 0.86. Cronbach's alpha coefficient was 0.85, indicating a good internal consistency with little redundancy in the scale.
The involvement of psychiatric patients in decision-making
The OPTION total scores showed a skewed distribution (Fig. 1), characterised by scores in the lower range of total scores, suggesting a generally modest performance in involving patients. The scores ranged from 6 to 65, with a mean score of 26.7 (s.d.=13) and a median of 25 (range 20–40) indicating a skill level defined by the OPTION manual as ‘minimal attempt of patient involvement’.

Fig. 1 Distribution of OPTION scores in 80 consultations.
Taking score 1 (minimal attempt) as a cut-off score for the presence of ability assessed by the single OPTION items, in more than half of the consultations patient involvement behaviours, except those defined by item 1, 8 and 11, were absent or only minimally attempted. When patient involvement abilities were performed, a minimal skill level was achieved (score 2) and prevailed over a good or high standard performance (score 3 and 4) which was observed in no more than 14 (17.6%) consultations (Table 1). For example, psychiatrists rarely attempted to state that there was more than one option (item 2) or to elicit the patient's preference level of involvement (item 10) and never assessed the patient's preferred approach to receiving information to assist decision-making (item 3). When they offered the patients the opportunity to ask questions (item 9), this was scored in 85% of the consultations as a minimal attempt only. The patient's concerns about how the problem(s) were to be managed (item 7) were never explored in 58% of consultations and minimally attempted in 17.5%. These results were confirmed when looking at the mean of each item: with the exception of items 2, 3 and 10, all other items obtained a mean score of about 1, which correspond to a minimal attempt to involve the patient (Fig. 2).
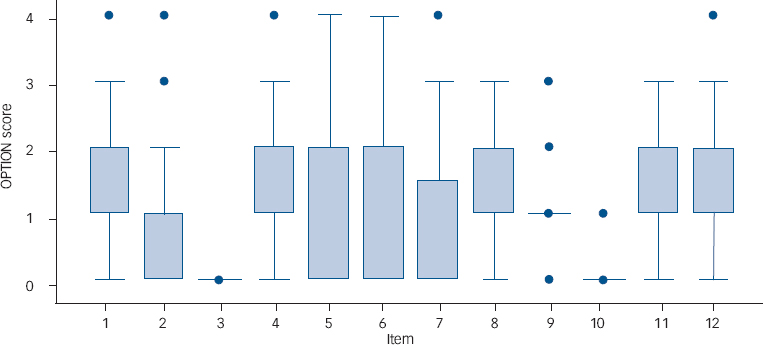
Fig. 2 Score distribution for each item. Boxes represent values between 25th and 75th percentiles, whiskers the upper and lower adjacent values, circles the outside values. 0=not observed; 1=minimal attempt; 2=minimum skill level; 3=good standard; 4=high standard.
Differences between psychiatrists
The differences between psychiatrists was significant (F(15,79)=3.88, P<0.01) (Fig. 3) and remained significant after excluding the six psychiatrists (1, 4, 12, 13, 14, 16) with fewer than three interviews (F(9,71)=5.51; P<0.01).

Fig. 3 Distribution of the OPTION scores for each psychiatrist. Boxes represent values between 25th and 75th percentiles, whiskers the upper and lower adjacent values, horizontal line the median.
The intracluster correlation coefficient was 0.46. The post hoc analysis showed that the differences were a result of psychiatrist number 3 (mean 15.4, s.d.=4.5), number 8 (mean 43.2, s.d.=9.68) and number 15 (mean 39, s.d.=15.41). There was also a significant difference among psychiatrists in the length of the interviews (F(15,64)=5.0, P<0.05).
Associations
The OPTION total score was unrelated to both patient and psychiatrists' characteristics. At the single-item level, psychiatrist gender was related to item 10 (eliciting the patient's preferred level of involvement in decision-making), and item 12 (indicating the need to review the decision), with female doctors tending to reach higher scores (mean=0.34 v. 0.05, t(16)=2.2, P=0.03 and mean=2.12 v. 1.14, t(14)=2.40, P=0.03 respectively).
Psychiatrists' age and years of experience were significantly related to item 6 (exploring patient's expectations about how the problems are to be managed) and item 10 (eliciting the patient's preferred level of involvement in decision-making), younger doctors with fewer years of experience obtained higher scores for both items (Pearson's r=–0.64, P<0.01 and r=–0.59, P=0.02; and r=–0.52, P=0.04 and r=–0.49, P=0.05 respectively). Psychiatrists' age was significantly related to item 12 (indicating the need to review the decision), with younger psychiatrists showing higher scores (r=–0.51, P=0.04).
Patient gender showed a significant association (t(54,6)=2.52, P=0.01) with item 9 (offering explicit opportunities to ask questions during the decision-making process) with higher scores for female patients (1.19 v. 0.94).
Length of consultations
The OPTION total score correlated significantly with the length of the interview: the longer the consultation time the higher the total score (r=0.79, P<0.01). Most of the single item scores showed a similar relationship with length of the interview (item 2: r=0.52, P=0.04; item 7: r=0.86, P<0.01), excluding item 8 (checking that the patient has understood the information), item 9 (offering the patient explicit opportunities to ask questions during the decision-making process) and item 11 (indicating the need for decision-making).
Discussion
In measuring patient involvement performance, the OPTION scale showed satisfactory psychometric properties when applied to psychiatric out-patient consultations. Our sample of psychiatrists at the South Verona CMHS displayed a generally low level of patient involvement. Although psychiatrists differed significantly in their performance, for the majority patient involvement was scored as only minimally attempted or minimally achieved. As observed in other studies Reference Adams and Drake12,Reference McCabe, Heath, Burns and Priebe17 the general performance was independent of patient and psychiatrist characteristics, but tended to improve with the length of consultation. Of note, the five psychiatrists in our study with a higher performance score had a longer mean consultation time. Some patient involvement behaviours were more likely to be attempted when psychiatrists were female, of younger age or had less years of psychiatric practice but were unaffected by patient characteristics, with the exception of patient gender.
Our findings parallel those observed in general practitioners (GPs) Reference Goss, Fontanesi, Mazzi, Del Piccolo, Rimondini and Zimmermann21 who showed a similar low level of patient involvement in terms of total scores, although some differences emerged in the use of single skills: psychiatrists were slightly better in five, GPs in two patient involvement behaviours. In particular, GPs more often explored patients' concerns, although at a minimal skill level, whereas psychiatrists performed this skill at a higher level, although less often.
To our knowledge this is the second study after that of Goossensen et al Reference Adams and Drake12 that has assessed the performance of patient involvement in psychiatry, using a standardised measure of patient involvement. Goossensen et al observed a somewhat higher level of involvement of out-patients attending for first-contact consultations, despite a much shorter mean consultation time of 13 minutes. Eight psychiatrists achieved, for a sample of 61 patients, a mean OPTION score of 43, which would correspond to the achievement of only a minimum performance and therefore not dissimilar to our findings. The slight difference in favour of Dutch psychiatrists may be due to smaller samples sizes and different sample characteristics. Dutch patients were younger and mostly male, the characteristics of their psychiatrists not being specified by the authors. However, both the Dutch and Italian psychiatrists very seldom explored to what extent patients preferred to be involved (OPTION item 3 and 10). This finding, together with that of the overall modest extent of patient involvement behaviours based on psychiatrist rather than on patient characteristics, raises issues that invites more systematic future research on the subject. Given that patients were not asked their preference and assuming that psychiatrists one-sidedly decided to what extent to involve the patient, these decisions tended against involvement as shown by the low OPTION scores in the two studies. Health professionals most often inaccurately guess that patients do not want to participate Reference Strull and Charles25 and behave accordingly. A low patient involvement performance in psychiatry could suggest a ‘defensive routine’ Reference Goossensen, Zijlstra and Koopmanschap13 hiding lack of patient involvement skills, or reflecting psychiatrists' convictions that shared decision-making strategies in psychiatry are of limited use. Reference Paccaloni, Rimondini, Pozzan and Zimmermann26
The difference in the overall performance level observed among psychiatrists, mainly as a result of a different performance on each composite item, suggests a rather personal style in handling this topic with patients and fits with previous findings that showed that without specific training in interviewing skills GPs and psychiatrists display an idiosyncratic self-made approach in conducting consultations. Reference Rimondini, Del Piccolo, Goss, Mazzi, Paccaloni and Zimmermann27,Reference Del Piccolo, Mazzi, Saltini and Zimmermann28
Limitations
Several limitations of the study have to be acknowledged. The participating junior and senior psychiatrists might be considered representative of those working in psychiatric university settings. Nevertheless, the sample size is small and the study should be replicated with larger samples, different centres and a greater and comparable number of consultations. The selection of the participating patients, as well as their number per psychiatrist, was left to the psychiatrists and this facilitated their consent to be audiotaped, but this had drawbacks. First, because of the selection criteria of convenience and the resulting sample size, the 80 participating patients cannot be considered as representative for the population of psychiatric out-patients. They presented 19% of all first contact or new illness episode out-patients who attended during the observation period. The sample appears similar to the population of first contact out-patients whose problems are mainly depressive and anxiety disorders. Patients suffering from other, more severe disorders generally have their first contact with the service through other pathways (e.g. emergency ward, home visits, contact with families first). Reference Rossi, Sandri, Bianco, Marsilio, Tansella and Amaddeo29 Second, the number of audiotaped contributions per psychiatrist varied widely and the observed patient involving skills are not equally representative for the ‘true’ performance of each psychiatrist, so that the collected data have not the same degree of accuracy. Although it is unlikely that a comparable, adequate number of consultations would have altered our findings of a low patient involvement performance, it would have allowed us to examine the performance variability in each psychiatrist or the combined effect of the explanatory variables on the observed performance level.
Limitations concerning the instrument are similar to those observed for the original instrument and have been discussed in detail. Reference Elwyn, Hutchings, Edwards, Rapport, Wensing, Cheung and Grol10,Reference Goss, Fontanesi, Mazzi, Del Piccolo, Rimondini and Zimmermann21 In particular, the good agreement, ICC and kappa scores may be biased by the skewed distribution. It is easier to agree on an absent behaviour (0 score) rather than to agree on a different skill level. Moreover, it could be argued that the observed low level of patient involvement may be because of a poor sensitivity of the scale, but data from a controlled trial Reference Elwyn, Edwards, Hood, Robling, Atwell, Russell, Wensing and Grol18 demonstrate that the scale is capable of detecting changes in performance.
Clinical implications and future directions
Implementation of the shared decision-making model in psychiatry via assessment tools and specific interventions could provide an important step towards meeting patients' needs and improving adherence to treatment. The observed low patient involvement performance suggests that psychiatrists may not be aware of the potential benefits of sharing treatment decisions with their patients.
Helpful interventions to encourage greater patient participation may range from providing information, feedback on psychiatrists' current performance and an increase in consultation time to more complex training courses in patient-involving communication skills. There is evidence that a specific training course can increase shared decision-making performance in general practice. Reference Elwyn, Edwards, Hood, Robling, Atwell, Russell, Wensing and Grol18 This might also apply to psychiatry, although in this setting some skills may be more or less relevant. In a recent review on intervention studies to improve treatment adherence in psychiatric patients, all studies failed to consider the role of patient-involvement communication skills. Reference Nosé, Barbui and Tansella30 Maybe such skills are taken for granted in psychiatry; this risks losing an important opportunity to improve health outcomes via patient satisfaction and adherence.
Involving the patient is a process that requires a number of skills: first, information gathering and relationship building skills; second, information giving skills; and third, specific abilities to involve the patient in the shared decision-making process. Research on how to adapt the shared decision-making framework to psychiatry is needed with regard to patients with different disorders at different stages and in different settings. A clearer picture of the situation will help us find answers to the questions which might arise and design the appropriate educational interventions. Do certain types of mental illness preclude patient involvement? Is it a lack of training, lack of time, prejudice, an intentional act or is it the patient's genuine wish to not participate that stops psychiatrists from involving patients? The OPTION scale can be one of the instruments to assess the efficacy of interventions in increasing patient involvement and to relate such improvement to patient outcomes.
Acknowledgements
We thank Giovanni Austoni who was one of the raters of the interrater reliability assessment.







eLetters
No eLetters have been published for this article.