Introduction
Group therapies are offered across mental health services to people with psychosis-spectrum diagnoses (Caruso et al., Reference Caruso, Grassi, Fau-Biancosino, Biancosino, Fau-Marmai, Marmai and Priebe2013). Aside from being less resource intensive, groups are also thought to offer advantages such as social contact, group cohesiveness, normalising of experiences and sharing of information (Yalom & Leszcz, Reference Yalom and Leszcz2005). A meta-analysis by Orfanos, Banks, and Priebe (Reference Orfanos, Banks and Priebe2015) reviewed evidence from 34 clinical trials of group treatment for individuals with schizophrenia across a range of modalities. They found that group therapy, regardless of its psychotherapeutic orientation, was effective compared to treatment-as-usual (TAU) with a small to moderate effect size at reducing negative symptoms. The authors suggest that a non-specific ‘group effect’ may be supporting a reduction in such symptoms, regardless of the therapeutic orientation. Furthermore, this review also showed that this approach was beneficial in reducing social functioning difficulties compared to TAU.
In contrast to other mental health difficulties (e.g. depression and generalised anxiety disorder; National Institute for Health and Care Excellence, 2009), group modalities are not recommended for people with psychosis in many clinical guidelines because of insufficient good quality evidence. To develop good quality evidence, it is important to first establish if an intervention is feasible, before conducting sufficiently powered trials. This is in line with the UK Medical Research Council (MRC) guidelines for evaluating complex interventions. These guidelines cite that ‘evaluations are often undermined by problems of acceptability, compliance, delivery of the intervention, recruitment and retention’ (Craig et al., Reference Craig, Dieppe, Macintyre, Michie, Nazareth and Petticrew2008, p. 3).
In this review adherence, conceptualised as the average number of therapy sessions attended will be examined as a feasibility parameter for group therapies. Other feasibility measures have previously been explored; a meta-analysis indicated that there was no difference in drop-out rates for group v. individual therapy amongst people with schizophrenia (Villeneuve, Potvin, Lesage, & Nicole, Reference Villeneuve, Potvin, Lesage and Nicole2010). Adherence as a metric is distinct from drop-out as it indicates how well clients are able to sustain attendance over time. This may be particularly important in group interventions; many groups take a modular approach and deliver one theme per session, which is then often built upon in the next session. Poor attendance may mean clients are missing therapeutic content which could limit their ability to make meaningful gains from further sessions. In contrast, missed sessions in individual therapy can be flexibly re-arranged. Furthermore, regular attendance by clients is likely to build a sense of group cohesion, which is considered an essential element of group approaches (Yalom & Leszcz, Reference Yalom and Leszcz2005). A lack of consistent engagement from certain members may present a challenge to cohesion amongst group members. Lecomte, Leclerc, and Wykes (Reference Lecomte, Leclerc and Wykes2018) investigated a cognitive behaviour therapy (CBT) for psychosis group and found group cohesion was an important pre-requisite for improvements in symptoms and self-esteem, suggesting that cohesion may be important in mediating change.
Adherence barriers have been investigated in relation to psychological therapies for people with psychosis. There is indication that some mental health staff may perceive clients tobe unwilling or unable to engage with psychological interventions (Ince, Haddock, & Tai, Reference Ince, Haddock and Tai2016). The clinical presentation of people with psychosis may also present barriers to adherence; poor cognitive skills may confer a risk of missing appointments due to limited organisational abilities to plan and execute the journey, or simply forgetting about the appointment. Forgetting an appointment was the primary reason for non-attendance given amongst a sample of clients using a psychiatric outpatient clinic (Killaspy, Banerjee, King, & Lloyd, Reference Killaspy, Banerjee, King and Lloyd2018). Positive symptoms such as paranoia may make going out in public or meeting other group of participants distressing, whilst negative symptoms may present a barrier to attendance in terms of motivation or being able to meaningfully contribute.
Nosé, Barbui, and Tansella (Reference Nosé, Barbui and Tansella2003) reviewed the literature on adherence to treatment in individuals with psychosis, but this study focussed primarily on adherence to psychotropic medication as well as attending routine appointments, and did not report on adherence to specific therapies. This study showed that approximately one in four clients with psychosis fails to adhere to treatment programmes. Non-adherence was associated with a lack of insight, positive symptoms, younger age, male gender, history of substance abuse, unemployment and low social functioning. A subsequent review focussing on appointment attendance (not including medication adherence) found that more severe psychopathology was associated with appointment non-attendance (Daniels, Loganathan, Wilson, & Kasckow, Reference Daniels, Loganathan, Wilson and Kasckow2014). However, there is no review investigating adherence to group therapies.
There are several reasons why groups may be more poorly attended and thus merit special focus. First, group approaches by their very nature could be considered to offer a less personalised intervention; spending time with a client to complete an individualised formulation may be more difficult, and thus the group may be perceived as less relevant. This may be particularly true for clients experiencing complex mental health difficulties such as psychosis, as problematic beliefs can be highly specific or idiosyncratic compared to difficulties such as depression where more common themes are more likely to emerge.
Second, the clinical presentation of people with psychosis can be very heterogeneous making it difficult to deliver the group at a level which is accessible and relevant for all. Third, group approaches necessitate social engagement and interaction between group members. Individuals with a diagnosis on the psychosis spectrum may have poor social skills (Mancuso, Horan, Kern, & Green, Reference Mancuso, Horan, Kern and Green2011), and people may find attending a group anxiety provoking. An analysis of responses given by individuals with psychosis when asked their opinions about whether they would like to join a group therapy identified that around a third of those asked had anxieties about attending a group (e.g. ‘I don't like talking in a group’) (Sumner et al., Reference Sumner, Haddock, Hartley, Kilbride, McCusker, Pitt and Barrowclough2014). Finally, people may be concerned about confidentiality and motivated to keep their difficulties private, particularly when such unusual experiences can result in stigma or discrimination (e.g. Dockery et al., Reference Dockery, Jeffery, Schauman, Williams, Farrelly, Bonnington and Clement2015). This may be especially marked in psychosis, as suspiciousness and mistrust are common problems.
This review will systematically examine adherence to group psychosocial therapies for people with psychosis and examine whether there are any specific demographic or clinical correlates of poor adherence. Following the findings of previous systematic reviews in this area (Daniels et al., Reference Daniels, Loganathan, Wilson and Kasckow2014; Nosé et al., Reference Nosé, Barbui and Tansella2003), the role client-related factors (age, gender and symptoms) have in influencing adherence will be investigated. Furthermore, group-related factors such as the therapeutic approach of the group and therapy duration will be explored. Finally, study methodological rigour will be evaluated to assess if adherence is influenced by study quality and also to assess the overall quality of the evidence in this field, or other methodological factors.
Method
Search strategy
Embase (1974–2019 week 12), Ovid MEDLINE (1946–2019 week 12) and PsycINFO (1806–2019 week 12) databases were searched up to the 25th March 2019 for cross-referencing terms related to group therapy and psychosis (see online Supplementary Table 1). The search was conducted within titles and abstracts, and was limited to: English language, human participantsand articles with an abstract.
The search returned 12 548 results. Following deduplication, 8751 articles remained. Titles and abstracts were screened for relevance, resulting in 358 full texts which were reviewed against the inclusion criteria. See Fig. 1 for the flowchart of literature selection.

Fig. 1. Flowchart of literature selection. *For example, attendance may be reported as ‘80% of participants attended at least 50% of sessions’, meaning an overall average percentage of sessions attended could not be recorded.
Inclusion criteria
(a) Reports the results of a trial (including pilot studies, randomised, non-randomised, controlled or uncontrolled, reports of evaluated clinical practice) for a group intervention from any therapeutic modality.
(b) >85% of participants included in the study have a diagnosis on the psychosis spectrum (i.e. schizophrenia-spectrum disorders including schizoaffective disorder, delusional disorder and first-episode psychosis).
(c) Participants are using adult mental health services.
(d) The rate of attendance at the group is reported, i.e. the mean/median number of sessions attended by participants.
(e) The study is a primary research report published in a peer-reviewed journal.
(f) Studies are published in English.
Exclusion criteria
(a) Studies which reported on systemic family therapy or which involve one or more family members attending, as this may provide an external motivation to attend.
(b) Studies which include individual therapy as part of the intervention (initial or follow-up individual sessions were allowed, so long as a discrete figure for attendance at the group alone was reported). This was because additional contact between sessions may influence motivation to attend and may increase participant burden in the intervention.
(c) Studies where attendance is reported, but this is not expressed as the mean/median number of sessions attended by participants. For example, attendance may be reported as ‘80% of participants attended at least 50% of sessions’ (e.g. Chadwick, Sambrooke, Rasch, & Davies, Reference Chadwick, Sambrooke, Rasch and Davies2000), meaning an overall average percentage of sessions attended could not be obtained.
Data extraction
The following information was extracted: (i) the mean or median rate of attendance (the average number of sessions attended by all participants, expressed as a percentage of the total number of sessions offered), (ii) the type of therapy group (therapeutic model used), (iii) number and frequency of sessions, (iv) the mental health professional who facilitated the group (e.g. psychologists, nurses, research assistants, etc.), (v) number of people in study and in each therapy group, (vi) study design, (vii) gender proportions, (viii) diagnostic characteristics, (ix) average age, (x) whether participants were offered an incentive to attend sessions (e.g. payment and vouchers), (xi) setting of group (inpatient or outpatient, and country the study was conducted in) and (xii) symptom profile (where reported using standardised measure of symptoms, e.g. PANSS, BPRS, SAPS, SANS, etc.).
The data extraction for a random subset of the papers (i.e. 20%) was independently rated by another author (KN) with no inconsistencies identified.
Methodological quality rating
Studies were rated for quality using the Clinical Trials Assessment Measure (CTAM; Tarrier & Wykes, Reference Tarrier and Wykes2004). This is composed of 15 items grouped into six areas of trial design: sample size and recruitment method; allocation to treatment; assessment of outcome; control groups; description of treatments and analysis. It is suitable for methodology evaluation of psychological interventions and has been used previously in published reviews in people with psychosis (Cella, Preti, Edwards, Dow, & Wykes, Reference Cella, Preti, Edwards, Dow and Wykes2017; Grant, Lawrence, Preti, Wykes, & Cella, Reference Grant, Lawrence, Preti and Cella2017). All studies were rated independently with the CTAM by two authors (OS and KN) and discrepancies were resolved through discussion with a third rater (MC).
Data synthesis
To assess the average level of attendance, mean and median were calculated across the rate of attendance given for each therapy group. The extracted data were checked for the assumptions of normality by visual inspection of histograms and using Kolmogorov–Smirnov and Shapiro–Wilk's tests.
The contribution of a particular variable on attendance (e.g. methodological, client and group-related factors) was then assessed. In the case of categorical variables, subgroups were created using the factor of interest as the independent variable (e.g. incentivised groups v. non-incentivised groups; inpatient v. outpatient setting); mean attendance rates were then compared between subgroups using Mann–Whitney U tests. In the case of continuous variables (e.g. age and sample size), bivariate Spearman correlations were performed. All analyses were conducted in SPSS 25, and significance threshold was set at p < 0.05.
Results
Fifty-nine original research papers were included in this review, reporting on 52 independent studies which included 66 therapy groups. This comprised of 2109 participants. See online Supplementary Table 2 for included studies description. We note that a large number of studies identified by our search did not include an attendance rate (e.g. Borras et al., Reference Borras, Boucherie, Mohr, Lecomte, Perroud and Huguelet2009; Landa, Silverstein, Schwartz, & Savitz, Reference Landa, Silverstein, Schwartz and Savitz2006; Leclerc, Lesage, Ricard, Lecomte, & Cyr, Reference Leclerc, Lesage, Ricard, Lecomte and Cyr2000; Liberman et al., Reference Liberman, Lillie, Falloon, Harpin, Hutchinson and Stoute1984; Lysaker & Bell, Reference Lysaker and Bell1995; McLeod, Morris, Birchwood, & Dovey, Reference McLeod, Morris, Birchwood and Dovey2007; Owen, Sellwood, Stephen, Murray, & Sarsam, Reference Owen, Sellwood, Stephen, Murray and Sarsam2015; Spidel, Lecomte, Kealy, & Daigneault, Reference Spidel, Lecomte, Kealy and Daigneault2018; Wallace & Liberman, Reference Wallace and Liberman1985).
Overall adherence
The mean reported adherence across all groups was 76.4% (s.d. = 17.4). The median was 80.1% (range: 18.3–100%). A weighted mean was calculated for overall attendance so that each attendance rate was weighted according to the sample size of the study it was derived from. The weighted mean attendance level across all groups was 70.9%.
Do methodological factors of the study influence adherence?
Study quality
CTAM ratings were highly variable; the mean rating was 53.8 (s.d. = 22.7, range: 7–91, out of a possible score of 100). A score of below 65 on the CTAM is considered suggestive of bias (Cella et al., Reference Cella, Preti, Edwards, Dow and Wykes2017); 20 studies (38.4%) scored above 65, and 32 (61.5%) scored below. See Table 1 for a summary of CTAM ratings, and online Supplementary Table 3 for the rating given to each study.
Table 1. Summary of CTAM ratings

There was no significant relationship observed between study quality and group adherence (rho = −0.177, p = 0.156).
Study design
Thirty-nine groups were randomised controlled trials (RCTs), whilst 27 used another study design including pre-post experimental designs, and non-RCTs. There was no significant difference in attendance levels (Z = −0.130, p = 0.896) between RCT studies (75.7%, s.d. = 17.4) and other designs (77.4%, s.d. = 17.8).
Sample size
The mean sample size reported for the therapy groups was 32.0 (s.d. = 29.0, range: 4–140). There was a statistically significant negative correlation between the sample size and adherence (rho = −0.324, p = 0.008).
Incentives
Sixteen groups reported an incentive to attend such as money, food vouchers or transportation, whilst 50 did not. Those which offered incentives were better attended (86.0%, s.d. = 9.41) than those which did not (73.4%, s.d. = 18.3; Z = −2.88, p = 0.004).
Do client-related factors influence adherence?
Age, sex and diagnosis
Average participant age was reported for 64 groups. The mean age was 39.2 (s.d. = 8.25, range: 23.6–66.1 years). There was a significant positive correlation between average adherence and age (rho = 0.266, p = 0.031).
Fifty-three groups gave a diagnostic breakdown of the sample; on average 80.3% (s.d. = 19.5) of participants were diagnosed with schizophrenia. There was no significant association between adherence and percentage of the sample diagnosed with schizophrenia (rho = 0.043, p = 0.761).
Sixty-four groups reported participants’ gender; 64.7% (s.d. = 17.9) of participants were male. There was no significant association between adherence and gender (rho = 0.053, p = 0.676).
Symptoms
Thirty-four groups used the Positive and Negative Syndrome Scale (PANSS) to report mean baseline (pre-treatment) symptoms. This was the most widely used measure of symptoms, and thus was selected to examine the relationship between symptoms and adherence. The mean (s.d.) PANSS scores across all the participants was: positive: 16.1 (3.25), negative: 18.0 (3.84), general: 33.3 (5.67) and total: 68.4 (13.6).
There were no significant correlations between positive, negative, general or total symptoms and adherence (all p > 0.533).
Do group-related factors influence adherence?
Therapeutic approach
The therapeutic approach across the reported groups was varied; 18 social skills or social cognition groups, 13 CBT, 7 ‘multimodal’ (combining different approaches), 7 cognitive remediation, 4 psychoeducational, 3 art/music therapy, 3 skills training (illness management skills, independent living skills and coping skills), 2 body psychotherapy, 2 metacognitive training, 2 supportive counselling, 3 third wave CBT approaches [mindfulness and acceptance and commitment therapy (ACT)], 1 positive psychotherapy and 1 described as a problem solving group.
Of these categories, skills training reported the highest level of average adherence (84.8%, s.d. = 4.78, three studies), and body psychotherapy reported the lowest (38.8%, s.d. = 23.0, two studies) (see Fig. 2).
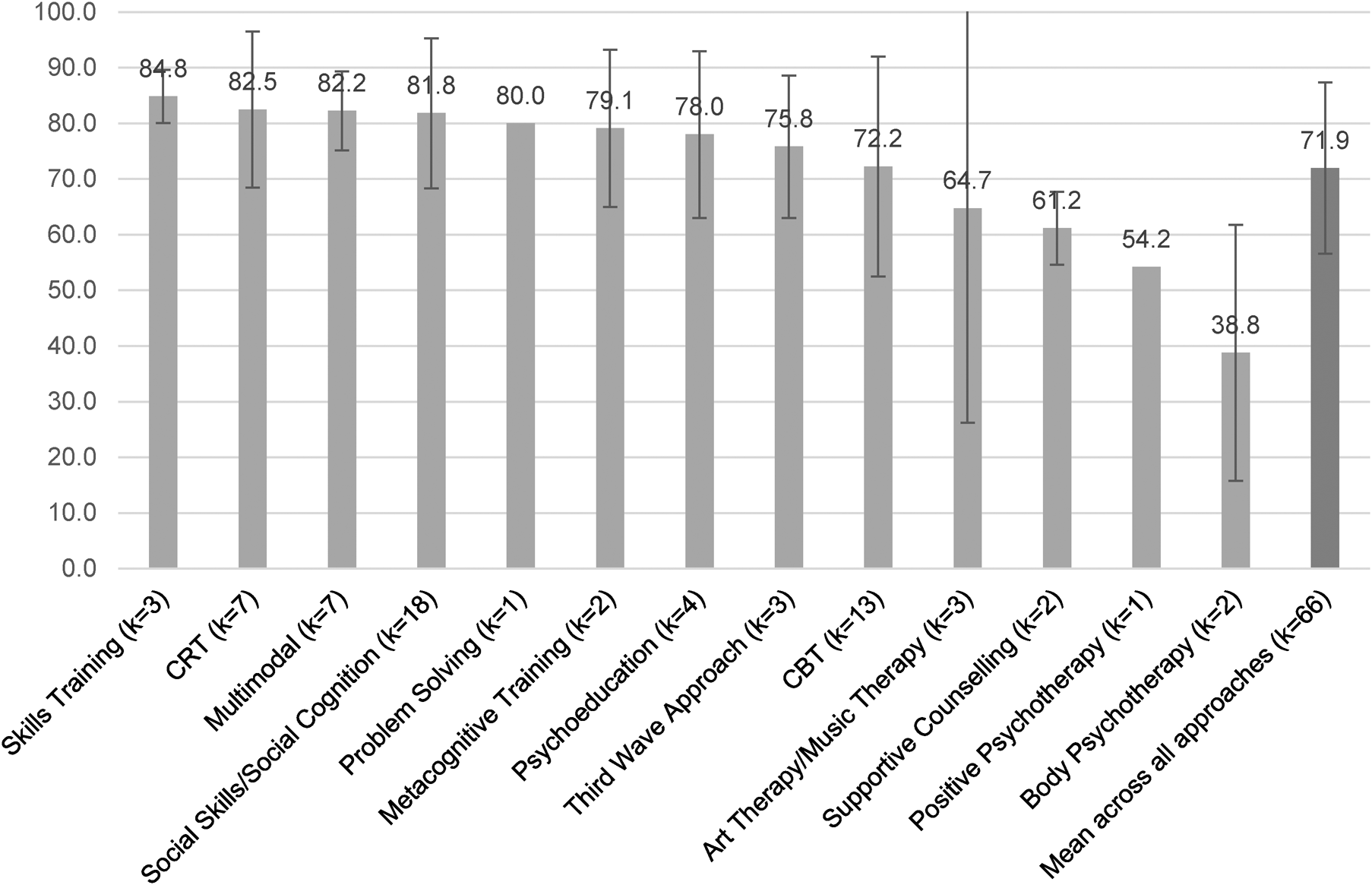
Fig. 2. Average adherence rate across therapeutic modality.
Session frequency
Thirty groups met weekly and had an average adherence of 74.1% (s.d. = 19.3), whilst 28 groups met twice weekly and had an adherence of 79.4% (s.d. = 19.6). There was no significant difference in adherence between these frequency types (Z = −1.24, p = 0.216).
Number of sessions
The mean number of sessions offered across all groups was 20.7 (s.d. = 20.9), with the maximum number of sessions offered being 156 (open-ended CBT group) and the minimum being four (ACT group). There was no significant association between the number of sessions and adherence (rho = −0.146, p = 0.242).
Number of participants per group
Forty-six groups reported the number of participants per group (i.e. number of clients in each clinical group, as opposed to overall study sample size). Studies tended to give a maximum number (i.e. ‘up to eight participants’) or gave a range for this figure (i.e. ‘between six and eight participants’). In the case where a range was given, the upper number was recorded as the group size to be consistent with studies which gave an upper limit. The mean number of participants was 8.13 (s.d. = 3.03), with the size ranging between 4 and 20. There was no association observed between the group size and adherence (rho = −0.022, p = 0.883).
Setting
Twelve of the groups were run in inpatient settings and 47 were run in outpatient settings. Five groups were composed of both inpatients and outpatients, and two were run in ‘mental health centres’, but it was unclear whether this was a community or inpatient setting. Those run on inpatient wards were on average better attended (84.4%, s.d. = 12.4) compared to community run groups (75.5%, s.d. = 18.8), however this difference was not statistically significant (Z = −1.52, p = 0.129).
Group facilitator(s)
The facilitator(s) were described for 49 of the groups. The majority of groups (24) were facilitated by combinations of professionals of different disciplines, classified as ‘Mixed Healthcare Professionals’, which could include a member of psychology staff. Thirteen were facilitated by solely psychology staff (including clinical psychologists, graduate psychologists, assistant psychologists or ‘Ph.D. level’ psychologists), three by nurses and two by psychiatrists. Seven groups were facilitated by professionals grouped as ‘Other’ such as body psychotherapists.
As the majority of groups included could be considered a type of psychological therapy, a comparison of psychology staff with all other professions was conducted to see whether this expertise influenced adherence. There was a non-significant trend for there to be a higher rate of adherence (Z = −1.89, p = 0.059) at groups facilitated by psychology staff (mean adherence = 82.7%, s.d. = 7.51) compared to all other professional categories combined (mean adherence = 74.1%, s.d. = 18.8).
Individual alongside group sessions
Although not included in the overall summaries of attendance reported in this paper, we examined the two papers (Horan et al., Reference Horan, Dolinsky, Lee, Kern, Hellemann, Sugar and Green2018; Kukla, Bell, & Lysaker, Reference Kukla, Bell and Lysaker2018) excluded for combining both individual and group sessions to examine whether there was an indication this may have influenced attendance.
Horan et al. (Reference Horan, Dolinsky, Lee, Kern, Hellemann, Sugar and Green2018) added two additional individual sessions to their group intervention focussed on social cognition skills; some participants received these sessions in public community settings (e.g. café) to facilitate direct practice of the skills, whereas some participant's sessions were held in clinic. A rate of attendance for the group alone was not reported, but the attendance across all sessions (both group and individual combined) tended to be higher in the group that practised skills in clinic compared to in public (83.3% v. 77%, respectively). Another study by Kukla et al. (Reference Kukla, Bell and Lysaker2018) offered an individual session for each group session offered (this was 26 group and 26 individual sessions) in a CBT-based intervention to support employment. A subset of participants also received cognitive remediation therapy alongside the group and individual sessions. Those who also had Cognitive Remediation Therapy (CRT) tended to attend more group sessions (63.5%) compared to those who did not (47%).
Discussion
The aim of this systematic review was to explore adherence to group therapy amongst people with psychosis. The results indicate that the average rate of adherence, conceptualised as attendance at group therapy, is 76.4%. This reduced to 70.9% when groups were weighted for sample size; this could be considered an important correction as studies with a small sample size were more likely to be reporting results from a single group and therefore perhaps reflecting a lessaccurate rate. This rate is not dissimilar to published estimates of adherence to group interventions for other groups of mental health service users. For example, a study of group behavioural activation for individuals with depression found the average rate of attendance was 64.9% (Kellett, Simmonds-Buckley, Bliss, & Waller, Reference Kellett, Simmonds-Buckley, Bliss and Waller2017), and a university counselling service offering group therapy found an average attendance of 79% (MacNair-Semands, Reference MacNair-Semands2002). These preliminary comparisons support the assertion that individuals experiencing more severe and enduring mental health difficulties can attain similar levels of adherence to group interventions compared to people with mild to moderate problems.
As this review relied on published reports of group therapy studies it may be difficult to assess the relevance of its results to clinical practice. Favourably, there was no significant difference in adherence between groups which were conducted as part of an RCT compared to other study designs. This suggests that using designs which may be more reflective of frontline clinical services situations report similar adherence levels, and increases confidence that the results are applicable to both research and clinical contexts.
Studies which incentivised participant adherence (e.g. participants were paid, transport was provided, etc.) were better attended. The substance misuse field has routinely used this type of contingency management approach to improve attendance in routine clinical practice and groups or for the provision of negative urine drug screens (e.g. Dunn et al., Reference Dunn, Sigmon, Reimann, Badger, Heil and Higgins2010; Petitjean et al., Reference Petitjean, Dürsteler-MacFarland, Krokar, Strasser, Mueller, Degen and Farronato2014), including in interventions for people with substance misuse and schizophrenia diagnoses (Tidey, Rohsenow, Kaplan, Swift, & Reid, Reference Tidey, Rohsenow, Kaplan, Swift and Reid2011). However, ethical concerns about this approach have been raised, especially in a state-funded health system such as the UKNHS (Sinclair, Burton, Ashcroft, & Priebe, Reference Sinclair, Burton, Ashcroft and Priebe2011). It may be that incentivising adherence with external factors is a useful strategy to support service users to access therapy; however, the rate of adherence at non-incentivised groups (70.6%) suggests that this may not make a meaningful difference. It may also cause difficulties with engagement if the motivation to attend is purely externally reinforced, a more helpful strategy is to make the therapy internally reinforcing, by optimising the value of the group content to support engagement.
With regards to client factors, the hypothesised relationship between greater psychopathology and poorer adherence (Daniels et al., Reference Daniels, Loganathan, Wilson and Kasckow2014; Fanning et al., Reference Fanning, Foley, Lawlor, McWilliams, Jackson, Renwick and O'Callaghan2012) was not supported. However, information about symptoms was only available for a small number of the included groups, and it is likely that clients recruited into research studies demonstrated a level of clinical stability which gave their referring clinician confidence in their ability to participate. Therefore, there may be a restricted range of symptom severity in the included studies. Notably, an exploration of the PANSS data revealed similar average PANSS scores between inpatient and outpatient groups (positive symptoms: 16.3 and 16.6, respectively) which may not be representative of inpatient populations more generally. Yet, it is promising that tentatively no specific clinical factors (symptoms and diagnosis) emerged as negatively influencing adherence, suggesting that this approach could be used with a range of clinical presentations. The suggestion that CRT may have supported attendance at both group and individual sessions (Kukla et al., Reference Kukla, Bell and Lysaker2018) suggests that cognitive symptoms may be relevant in influencing attendance.
The association between young age and poor adherence observed in previous reviews was also supported here, with a significant negative correlation identified (Daniels et al., Reference Daniels, Loganathan, Wilson and Kasckow2014; Nosé et al., Reference Nosé, Barbui and Tansella2003). This highlights particular challenges for services working with younger clients, such as early intervention services. It may be that strategies to support adherence to psychological therapy can be employed in such services, such as text message reminders which have found to be effective at supporting attendance (Kravariti et al., Reference Kravariti, Reeve-Mates, Da Gama Pires, Tsakanikos, Hayes, Renshaw and McGuire2018). An additional consideration may be using emerging technologies to augment the face to face interaction with digital therapy elements delivered online or on a mobile phone. Interventions such as this are being developed for individuals with psychosis (e.g. Bell et al., Reference Bell, Fielding-Smith, Hayward, Rossell, Lim, Farhall and Thomas2018; Garety et al., Reference Garety, Ward, Freeman, Fowler, Emsley, Dunn and Hardy2017). Such approaches may support the client to feel more connected to the intervention when they are not physically in the room, hence supporting subsequent attendance, or could allow the delivery of therapeutic material even if the client is not able to attend. Such initiatives are being taken forward in current innovative research programmes; for example, one group in the UK is co-producing a social cognition intervention with service users which can be delivered in a ‘virtual space’ to support the delivery of psychological therapies to ‘hard to engage’ groups, such as those with high levels of negative symptoms (Realpe et al., Reference Realpe, Elahi, Bucci, Birchwood, Vlaev, Taylor and Thompson2020). It remains to be established whether remotely-delivered interventions confer similar benefits to face to face interventions for this client group. The issue of attendance, in those virtual or remote contexts, may need to be reconceptualised as attendance to the session content rather than physical presence in a session.
This review adds support to the feasibility of groups as a therapeutic modality, as on the whole, there does not appear to be significant difficulties with adherence to group therapy when assessed by attendance. Feasibility is a key aspect of developing and evaluating complex interventions (Craig et al., Reference Craig, Dieppe, Macintyre, Michie, Nazareth and Petticrew2008), and should be considered alongside high-quality efficacy/effectiveness studies to inform future clinical guideline development. Although group approaches have longstanding use in clinical practice, and evidence suggests they offer benefits (Orfanos et al., Reference Orfanos, Banks and Priebe2015), the quality of studies remains lower compared to individual therapies. Indeed, the study quality of the included studies in this review was highly variable, with approximately 61% of papers found to be at risk of bias based on the CTAM. The current quality of evidence may explain why this therapeutic modality is not widely recommended in clinical guidelines.
Before recommendation can be included in clinical guidelines clear evidence of efficacy for specific therapeutic approaches in a group format is required. Future studies need to consider the relative contribution of therapy format (e.g. group) and orientation (e.g. CBT) to outcomes. We hope that the evidence presented here will guide future efforts to conduct high-quality trials to address relevant questions including disentangling the role of format and therapy orientation, evaluating different therapy modalities and evaluating effectiveness and implementation. Preliminary evidence suggests that group and individual approaches may have comparable effects: for example, a meta-analysis concluded that there was no difference in effect size for group v. individual CBT for psychosis (Wykes, Steel, Everitt, & Tarrier, Reference Wykes, Steel, Everitt and Tarrier2008).
Poor study quality also limited the questions we could explore with regards to therapy (e.g. whether therapy characteristics influenced adherence, such as level of interaction, structure, etc.). Poor ratings were obtained for treatment description, with 40% of the studies not scoring the maximum points on our methodological quality measure. In relation to therapeutic modality, some approaches may be more suited to a group format (such as social skills training), compared to therapies usually offered in an individual format (e.g. CBT). This may increase their appeal and relevance, and thus adherence. However, the conclusion is tentative given the low number of studies included for each therapeutic orientation.
It is also important to consider if better attendance is associated with improved outcomes. Few included studies examined this, and conclusions were mixed: whilst this relationship was supported by some studies (Vidarsdottir et al., Reference Vidarsdottir, Roberts, Twamley, Gudmundsdottir, Sigurdsson and Magnusdottir2019), it was not in others (Crawford et al., Reference Crawford, Killaspy, Barnes, Barrett, Byford, Clayton and Waller2012a), or was inconclusive (Roberts et al., Reference Roberts, Combs, Willoughby, Mintz, Gibson, Rupp and Penn2014). It may be that adherence is more relevant to outcome for certain group approaches, for example cognitive remediation, which relies on the principles of massed practice (Cella & Wykes, Reference Cella and Wykes2019). Further development of group delivery methods may open possibilities for alternative models of care. Some primary care services offer a ‘stepped care’ approach; in this model group approaches may be offered as a first-line approach, and if further intervention is indicated upon completion individual therapy can be offered. This may be a helpful model to implement to improve access to psychological therapies for psychosis (Johns et al., Reference Johns, Jolley, Garety, Khondoker, Fornells-Ambrojo, Onwumere and Byrne2019). It could be that the enhancement in motivation gained from attending group therapy would allow better engagement with individual therapy in the future, and thus providing initial group interventions may be helpful for people with psychosis.
Strengths and limitations
Limitations must also be considered. First, publication bias may have influenced the findings. Studies which reported high levels of adherence, alongside other positive outcomes, are arguably more likely to be published. Similarly, studies with poor levels of adherence may be abandoned. An inclusion criterion for this study was that the paper included an attendance rate which may also have introduced a source of bias for those who omitted this information due to poor attendance. Yet, studies do exist in this literature which report difficulties with client adherence (Crawford et al., Reference Crawford, Killaspy, Barnes, Barrett, Byford, Clayton and Waller2012b; Parker, Foley, Walker, & Dark, Reference Parker, Foley, Walker and Dark2013), suggesting that not all poorly attended groups fail to be published.
Second, this review was not able to consider all factors which may have impacted adherence. For example, acceptability of the therapeutic approach for the individual as well as external factors (such as scheduling, travel arrangements and financial costs of attendance). Third, due to differences in the way that adherence was reported, some studies could not be included. Relatedly, studies classified ‘attendance’ in different ways, for example including or not including individuals who did not attend any sessions in their average attendance calculations. This may have introduced bias into the findings. Furthermore, the results reflect only groups which do not include additional individual intervention, which may limit to scope of generalisation. Finally, many of the analyses reported are correlational and descriptive and therefore do not allow causation inference. Exploration of the variables considered using a multivariate approach, such as a multiple regression model, would allow assessment of different variable's contribution to overall adherence. Primary empirical research may be better suited to use these methods and answer questions such as whether incentives are equally effective on wards as in community settings, or whether age is relevant to adherence across therapeutic modalities.
The strengths of the review must also be considered. This review included any trial of a group therapy which reported session adherence, and therefore can be considered more wide-ranging than previous reviews in this area. It is hoped that this will allow the consideration of evidence across a larger number of participants, with designs which may reflect more naturalistic adherence rates found in frontline services. In addition, a wide range of other factors have been considered, including demographic, clinical and group-related factors which may have influenced adherence based on reports in previous literature. The amalgamation of this evidence across the large number of participants (n = 2109) allowed investigating potential relationships. Finally, this review has considered adherence which is a clinically applicable and useful concept for clinicians considering service planning, or researchers seeking funding for RCTs who may need to demonstrate the likely feasibility of their proposed intervention.
In conclusion, this review supports the feasibility of group interventions for people with psychosis in relation to adherence, compared to published estimates in different groups. The results suggest that groups may be better attended by older clients and when incentives are offered. Future research should implement high-quality, RCT designs to further the evidence base for this intervention delivery-method which may allow a more efficient way to deliver psychological interventions , and give specific consideration of how to engage specific groups e.g. younger, first-episode clients.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291721000404.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors. MC would like to acknowledge the support of the National Institute for Health Research (NIHR) Biomedical Research Centre in Mental Health at the South London and Maudsley Foundation Trust and the Institute of Psychiatry, Psychology and Neuroscience at King's College London.
Conflict of interest
There are no conflicts of interest to declare






