Introduction. Converging Forces
Mental health disorders constitute the single largest source of health-related economic burden worldwide. Common disorders, including depression or anxiety, contribute most to this burden, with over one in four people affected with these conditions at some point in their lives.Footnote 1
We have a behavioral and mental health crisis in the United States, “…a crisis in our inability to prevent, identify, and treat mental illness and substance use and to support people who experience or are in recovery from these conditions.”Footnote 2 The term “behavioral health” broadly refers to mental health and addiction services, including outpatient and inpatient therapy, intellectual and developmental disability treatment, troubled teen treatment centers, autism clinics, psychiatric hospitals, methadone clinics, and detox centers. More than one-third of all adults report having a mental health condition or substance use disorder, but less than half receive treatment for their condition because of provider shortages, high out-of-pocket costs, and gaps in coverage and reimbursement for behavioral health services.Footnote 3
My focus in this article is on the financial and technological forces moving rapidly into this behavioral health field, a field marked by large vulnerable populations like autistic children and troubled teenagers. These forces—private equity financing and telemental health—offer money and new technologies to extend the reach of mental health services and make treatments more accessible to patients in need.Footnote 4 The convergence of an aggressive financial model and an arsenal of digital health tools promises improved access to care, as private equity finances more behavioral treatment centers.
The problem is that these forces may end up harming patients for reasons inherent in the structure of private equity financing and the motivations that underpin it, and the current limits of telemental therapies. Further research is needed as to what works best for psychotherapy, not only in live doctor-patient treatments but also in telemental health treatment; new regulatory tools are needed to control private equity ownership in the telemental health market generally.
The goal of this article is to examine the drivers of these forces, to test whether private equity and telemental health can be positive forces in promoting access at an acceptable level of qualityFootnote 5 and if not, what kinds of legal responses are needed to regulate the risks of patient abuses and poor quality therapeutic care.
I. Access to Behavioral Health Therapies Is Limited
The lack of access to psychiatric services across the health care service delivery field has been a cold, hard reality for decades and significantly delays treatment and reduces the quality of treatment received. This delay results in unacceptable patient experiences in care, poor outcomes and higher costs. The phenomena of “waiting lists” to see psychiatrists in outpatient clinic settings, the “boarder” waiting days in hospital EDs for an inpatient bed to open and the pockets of geographic isolation to any psychiatric services in many parts of the country all result in unacceptable patient experience, poor care and poor outcomes.Footnote 6
A. Demand for Mental Health Treatment Has Grown
The World Health Organization (WHO) reports that the COVID-19 pandemic has increased the prevalence of depression and anxiety, most likely due to feelings of loneliness, grief and bereavement, and fear of infection.Footnote 7 More people have sought help online: WHO found a “…103% increase in the number of people who completed an online mental health screen between 2020 and 2021and a nearly 500%W increase over 2019. Youth aged 11-17 represented 45% percent of individuals in the U.S. who took a screen in 2021, a 3% increase over 2020 and a 16% increase over 2019.”Footnote 8
The United States has experienced a substantial upswing in the need for mental/behavioral health therapies. The National Alliance on Mental Illness (NAMI) states that 1 in 5 U.S. adults experience mental illness, 1 in 20 adults experience serious mental illness and 17% of youth (6-17 years) experience a mental health disorder.Footnote 9
B. Shortages of Mental Health Professionals Have Grown
Access to mental health treatment is a substantial problem in the United States, which is short on mental health professionals. A psychiatrist shortage has developed, with estimates of up to 20,000 additional therapists needed.Footnote 10 One recent estimate states that “the psychiatrist workforce will contract through 2024 to a projected low of 38,821, which is equal to a shortage of between 14,280 and 31,091 psychiatrists, depending on the psychiatrist-to-population ratio used.” Behavioral psychologists, social workers and counselors are also overextended.Footnote 11 University counseling services report months-long waits before students can see a counselor.Footnote 12 The solutions commonly mentioned—both good ones—are to (1) increase reimbursement rates for psychiatrists and other mental health practitioners and (2) use a wider range of providers, including nurses and family support specialists.
Figure 1 demonstrates the wide range of professionals who are behavioral health professionals, from psychiatrists with prescribing power to clinical social workers.Footnote 13

Figure 1. A chart representing a wide range of behavioral health professionals.
This wide spectrum of behavioral health providers has relevance to the later analysis of private equity’s attraction to behavioral health as an investment vehicle.
II. Traditional Mental Health Therapies
Meta-analyses on the efficacy of different forms of psychotherapy suggest that up to 50% of the patients do not show clinically significant change, and in about 5–20% of patients, adverse events, including treatment failure and deterioration of symptoms, emergence of new symptoms, suicidality, occupational problems or stigmatization, changes in the social network or strains in relationships, therapy dependence, or undermining of self-efficacy, should be expected.Footnote 14
A. Definitions
The WHO defines mental health broadly as a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community. Mental disorders that are not directly related to or caused by behaviors are bipolar disorder, schizophrenia, depression, and generalized anxiety disorder.
The WHO definitions of mental health disorders are a good place to start.Footnote 15 The WHO defines a mental disorder “…as a clinically significant disturbance in an individual’s cognition, emotional regulation, or behavior. It is usually associated with distress or impairment in important areas of functioning.”Footnote 16 Some of the disorders the WHO lists are as follows: anxiety disorders, depression, bipolar disorder, schizophrenia, eating disorders, disruptive behavior and dissocial disorders, neurodevelopmental disorders, of which ADHD and autism spectrum disorder (ASD) are two examples.
Behavioral health disorders are caused by maladaptive behaviors that have a negative impact on a person’s mental condition. Behavioral health examines how a person’s habits impact her overall physical and mental wellbeing, as a subset of mental health. Symptoms of poor behavioral health are behaviors have negative impacts on well-being. Such behaviors include substance abuse, social isolation, and disordered eating.Footnote 17
B. Traditional Mental Health Therapy Approaches
1. Medication
Some mental illnesses respond well to medications such as antidepressants and antipsychotics. These medicines change the chemicals in the brain. Ketamine is one such medicine. In March 2019, the Food and Drug Administration (FDA) approved the nasal spray, esketamine (derived from ketamine), for major depression. Ketamine works by triggering glutamate production – a neurotransmitter responsible for mood regulation –and forming new neural connections.Footnote 18
Medication use assumes that mental illness has biological roots; psychiatry has engaged in a “troubled search” for such roots, as Anne Harrington writes.Footnote 19 Harrington argues that much drug company research in clinical trials has not proved clinically significant; the placebo results could not easily be distinguished from the drug results.Footnote 20 Such research on psychiatric cures has largely been abandoned by big pharma. Harrington argues that mental disorders are “not just medical, because the experiences of all human beings, ill or otherwise, are shaped by their cultural, social, and familial circumstances.” She argues for a cooperative ecosystem of mental health experts that includes psychiatrists, psychologists, counselors, nurses, social workers, social service providers, and patient-run organizations.Footnote 21 Will telebehavioral health and evidence-based therapies be part of this new ecosystem? Or will behavioral health providers be increasingly phased out in favor of digital tools used to provide therapy?
2. Psychotherapy
Talking to a mental health professional may help a patient work through the challenges of an illness and manage its symptoms.Footnote 22 Psychotherapy can be effective in a one-to-one setting with a healthcare provider or a group setting. The problem is that psychotherapy is not always predictable in its effectiveness -- many patients fail to improve and instead deteriorate.Footnote 23 This problem has been recognized for decades; failures in psychotherapy includes a range of negative effects—attrition, non-response, deterioration, adverse outcomes, iatrogenic effects, and so on. Causes are under researched, but include poor treatment choice, therapist mistakes, and therapist skill limitations.Footnote 24 More on this later.
3. Alternative therapies
Claims are also made that some mental illnesses, such as depression, may improve with alternative therapies. Some examples include herbal remedies, massage, acupuncture, yoga, and meditation. Suggested benefits of these alternative therapies range from lower stress, improved sleep, better breathing and functioning, to improved wellbeing.Footnote 25 The lack of evidence-based studies is again problematic for alternative therapies; there is no consensus among scientists on the effectiveness of alternative therapies in treating depression. One clinical study on acupuncture has claimed “…clinically-relevant benefits in reducing the severity of depression at the end of treatment compared to sham acupuncture, usual care, and as an adjunct treatment to anti-depressant medication.Footnote 26 The study caveats however were substantial.
4. Brain stimulation therapies
Brain stimulation therapies change the way nerves and other cells in the brain process chemicals and respond to stimuli. Examples include electroconvulsive therapy (ECT) and transcranial magnetic stimulation (TMS). ECT and TMS are often used when individuals do not respond to other treatment options or require rapid treatment, such as in cases where the patient is suicidal.Footnote 27 Both treatments are effective, but neither therapy is permanent given the potential of the illness to return, and further treatments may be needed. Footnote 28 Evidence-based research is lacking to confirm the value of many of these approaches; studies are proliferating as patients and payors demand proof that therapies work.Footnote 29
C. Limits on Use of Behavioral Health Therapies
1. Therapist-Patient Models of Live Encounters are Costly
The optimal length of a psychotherapy session is uncertain. Sessions are usually set to a fixed time because of cost containment and feasibility issues, but evidence is not yet clear as to what the optimal session time should be. The longer the session, the few patients a therapist can see and treat.Footnote 30
2. Therapist-Patient Appointments are Hard to Get
The demand for therapy referrals surged during the pandemic for anxiety, depressive and trauma-related disorders. The survey also found that “…. 65 percent of the more than 1,100 psychologists who responded said they had no capacity for new patients and 68 percent said their wait lists were longer than they were in 2020.”Footnote 31 In 2020, a group of psychologists issued a call to action in the American Psychologist Journal to deal with the increasing unavailability of psychotherapists in the face of escalating demands.Footnote 32
D. Evidence of Efficacy of Treatment is Limited
Measuring outcomes in psychotherapy is difficult, leaving psychiatry behind other medical specialties.Footnote 33 Mental health treatments lack solid evidence-based research findings compared to other medical specialties.Footnote 34 As Cuijpers has noted: “It is not yet clear what mental disorders are and what are the causal pathways that lead to them.” That makes it difficult to decide what the targets and outcomes of psychotherapies should be.Footnote 35 The field of psychological research is an active one, and studies are ongoing on outcomes of psychotherapy—what works to produce good patient outcomes, why that is, and where is there room for improvement.Footnote 36
The difficulty of making strong claims for the effectiveness of particular therapies is demonstrated by looking closely at the research on cognitive behavioral therapy (CBT). CBT is a form of psychotherapy focusing on changing negative behaviors and thought patterns. CBT is claimed to be the “gold standard” in psychotherapy, effective in the short-term for the treatment of anxiety disorder, ADHD, physical conditions like IBS and breast cancer, bulimia nervosa, and behavioral problems.Footnote 37
As studies have been done on the efficacy of CBT, however, the claims of “high cost-effectiveness”Footnote 38 based on good evidence has faded. A 2014 study concluded that CBT interventions are cheaper than usual care, providing some support for its potential, but calling for better assessment. Footnote 39 Finally, a larger 2015 study of British primary care treatment of depression using CBT turned negative. The REEACT trial found that “…for the primary outcome of severity of depression at four months there was no significant benefit for supported CBT in addition to usual GP care.”Footnote 40 The authors went so far as to suggest that the routine promotion of CBT should be reconsidered for the British National Health Service (NHS). “Commercially developed computerized cognitive behavior therapy products confer little or no benefit over free to use products.” The authors recommended that other treatments be used instead, such as telephone guided self-help, bibliotherapy, low intensity psychological workers supporting self-help technologies, and therapist-delivered cognitive behavior therapy.
Assessing efficacy of psychotherapy has proved difficult. Studies have found that publication bias overstates the positive outcomes of therapy by a large amount.Footnote 41 Studies examining the placebo effect in medicine found a large effect in psychotherapy, as shown below in graphic form. The positive placebo effect is larger than “therapy specific effects.”Footnote 42 Figure 2 gives a vivid portrayal of the placebo effect.Footnote 43
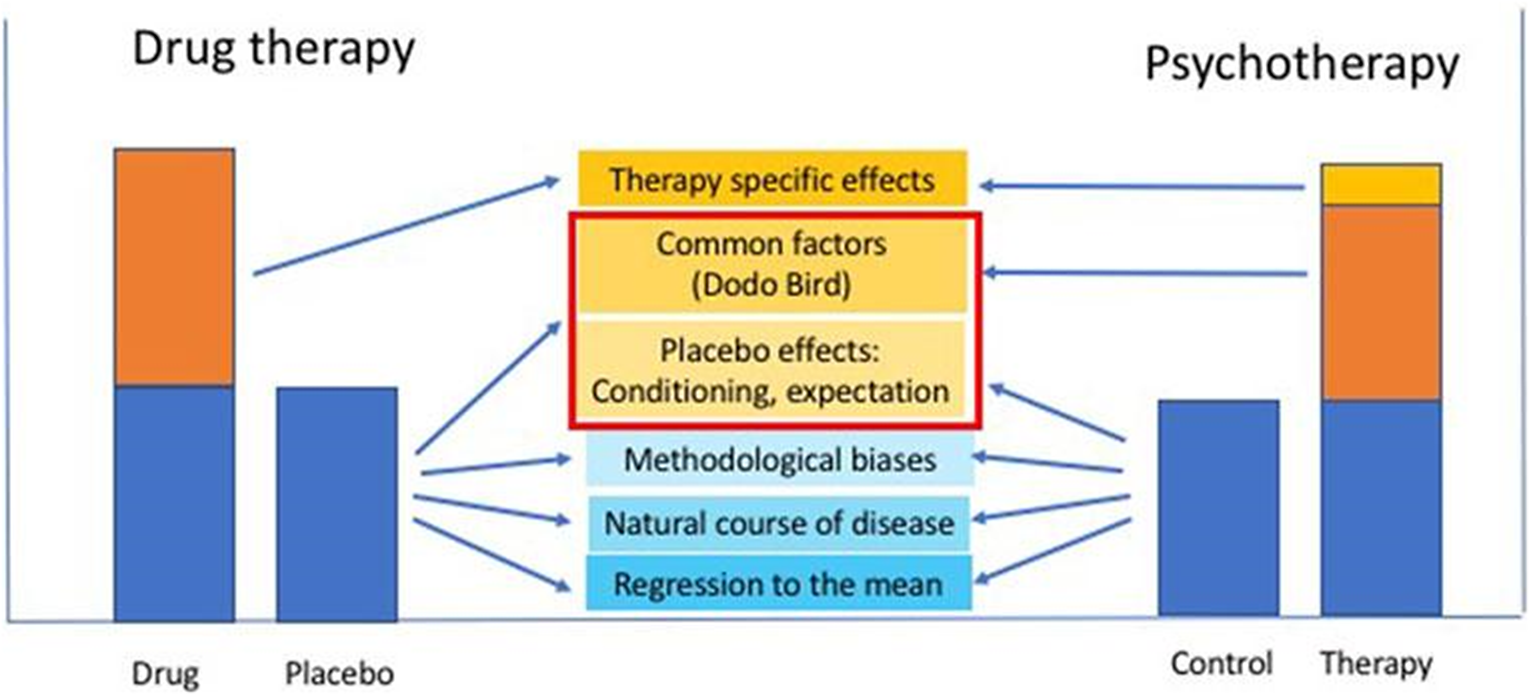
Figure 2. Schematic relationship between shared and non-shared nonspecific factors contributing to the placebo response in drug and psychotherapy: factors that are part of the (nonspecific) placebo effect in drug therapy (e.g., therapist empathy, intensity of patient-therapist communication, etc.) become “common factors” across all psychotherapies [Rosenzweig’s “Dodo Bird” (1936), or Lambert and Ogles’ “common factors” (2004)], addition to a (small) specific effect of the different psychotherapy modalities that may be composed of a specific combination of the factors…”
Proof of the efficacy of particular treatment models is indeed hard to come by.
On the other hand, effective therapists exist. The authors of the Handbook of Psychotherapy and Behavior Change conclude in 2021 that “…there are sufficient numbers of studies, in RCTs and in naturalistic settings, to conclude that therapist effects exist: “Some therapists consistently achieve better outcomes than other therapists.”Footnote 44 And they continue: “The evidence discussed in this chapter show clearly that some therapists consistently achieve poor outcomes, attenuating the overall effect of agencies and systems of care.”Footnote 45 The patient “deterioration effect” is also a real result of poor therapists. Others look at the therapeutic relationship, concluding that it “…makes substantial and consistent contributions to psychotherapy outcomes independent of the type of treatment. The relationship acts in concert with treatment methods, patient characteristics, and practitioner qualities in determining effectiveness.” The authors concluded that it is the therapeutic relationship that explains for why patients improve or not, rather than the particular treatment method.Footnote 46
We are left with cautious optimism as to value of psychotherapy, but still lack confidence in the benefits of particular therapeutic approaches separate from the personality and skills of the therapist. Competence-based therapeutic models seem to be emerging from the traditional world of psychotherapy.Footnote 47 What we don’t see is an evidence-based effective modality of treatment that can be used by any therapist to achieve consistent treatment success. Owners and managers of behavioral treatment facilities cannot assume that their therapists can just grab a treatment modality like CBT off the shelf and guarantee good outcomes. The history of CBT illustrates how it takes time and good studies to finally confirm whether a treatment works or note, or more likely, what it takes to make an effective therapist, independent of the therapy chosen.
This debate over the existence of effective treatment templates in mental health matters, since governments and insurers want to know if an evidence-based answer as to what works does exist. Private equity wants the same reassurance, viewing the investment potential of behavioral medicine therapies to reduce the costs of mental health treatment; PE is however more willing to gamble that if therapies like CBT work, telepsychiatry can just plug into behavioral treatments like a miracle drug that cures while reducing the costs of hiring therapists. Virtual Therapists will then in theory go all the way toward psychotherapy without psychotherapists at a tremendous saving in costs.
III. Digital Telehealth Promises Both Improved Access and Efficacy
Despite a rush to build applications using it, emotionally intelligent computing remains in its infancy and is being introduced in the realm of therapeutic services as a fix-all solution without scientific validation nor public consent. Scientists still disagree over the over the nature of emotions and how they are felt and expressed among various populations, yet this uncertainty has been mostly disregarded by a wellness industry eager to profit on the digitalization of health care. If left unregulated, AI-based mental-health solutions risk creating new disparities in the provision of care as those who cannot afford in-person therapy will be referred to bot-powered therapists of uncertain quality.Footnote 48
A. Modes of Telehealth
Telemental health (DMHI) is “the use of electronic information and telecommunication technologies to support long-distance clinical health care, patient and professional health-related education, public health, and health administration.”Footnote 49 It is sometimes referred to as telepsychiatry or telepsychology. Research suggests that telemental health services can be effective for many people, including but not limited to those with ADHD, post-traumatic stress disorder (PTSD), depression, and anxiety.“Footnote 50
Telemental health is nothing new. As Hannah Zeavin writes in The Distance Cure: A History of Teletherapy Footnote 51, the history of psychotherapy as person-to-person conversations has always been enriched by other communication technologies. She writes: “…[P]sychotherapy has always operated through multiple communication technologies and media, including advice columns, radio broadcasts, crisis hotlines, the earliest mainframe networks, home computing, the Internet, and mobile phones.” She notes that Freud worked with patients by mail; advice columns, radio broadcasts, crisis hotlines are examples of the use of communication technology.”Footnote 52 Crisis hotlines allow for therapeutic help; advice columns, radio broadcasts, soap operas, early computer programs like Eliza—all allowed people needing mental health help multiple modes of communication. Zeavin argues that the traditional therapeutic relationship is a triad: therapist, patient, and communication technology.
Digital interventions have the potential to improve access to treatment for underserved groups. Crucially, however, such digital technologies are proliferating in an environment lacking in regulatory scrutiny as to what works. Research needs to be funded as to what works, how make the tools engaging and effective for underserved populations who have low levels of digital literacy, and how to use digital tools in clinical pathways to better predict relapse and early intervention.Footnote 53
B. Digital Tools Are Seen as a Solution to Therapist Shortages Footnote 54
Digital mental health interventions (DMHIs) are therapies that use technologies such as computer programs, cellphones or smartwatches to support an individual by providing information, support, or treatment for mental health. Such DMHIs can stand alone as self-help tools, or can couple with standard therapy to create blended therapy. DMHIs are attractive to governments and investors given their apparent potential to provide mental health services, particularly for young people who use such technology comfortably and who have high levels of mental health needs. DMHIs are advocated particularly for youth with limited access to mental health services.Footnote 55
Telemental health tools are already in use because of the need during the pandemic.Footnote 56 These tools have a high transaction value since they require less capital on their face to treat a higher volume of patients. Telemental health (DMHI) tools promise much improved access to mental health treatment for populations that could not get such careFootnote 57 because of travel distance, costs, and time limitations.
DMHIs can also be misused more easily to create fraudulent billing, if coupled with private equity owned practices. And they lack solid evidence-based research findings compared to other medical specialties, as does live psychotherapy in general.Footnote 58 DHMIs risk quick adoption before evidence of effectiveness is clear. Digital tools attract entrepreneurs who hope to sell them as a therapy product, and the marketing environment of such products tends, in the words of Health Education England, to make “…spurious claims and overhyped technologies that fail to deliver for patients.”Footnote 59
C. The Digital Telemental Health Therapy Spectrum
Digital technologies, including the Internet, smartphones and wearables can connect patients, services and health data in novel ways not previously available and through combination with existing treatments. One recent study lists seven digital technologies as examples of digital telemental health.Footnote 60 DMHI potentially increases access to mental health care for underserved populations.Footnote 61 DMHI is comparable to in-person care and effective for both diagnosis and assessment in many settings. Patients report comparable satisfaction between DMHI and in-person care, and DMHI treatment can produce equal clinical outcomes to face-to-face treatment.Footnote 62
Access is also improved for underserved populations.Footnote 63 DMHI reduces transportation barriers by allowing access to remote providers without the need to travel—this is particularly helpful to vulnerable individuals who are home-bound, have child care responsibilities, or have mobility limitations due to illness or disability; DMHI provides minorities with different cultural and linguistic backgrounds access to provides who share those backgrounds; DMHI reduces wait times for appointments and allows far more flexible scheduling.Footnote 64
Digital telemental health tools are proliferating, as are the categories into which such tools fit. I will use the categories developed by Imogen Bell and her colleagues, with some modifications of my own, to begin to sort out the levels of access created by digital telemedicine, and some of its limits.Footnote 65 I use three large distinctions: (1) self-help digital tools, such as wellness apps that can be downloaded to a person’s phone or computer; (2) telemental health tools that require the linkage of a live therapist and the patient; and (3) digital replacements for therapists. I note that “[m]ost Web-based interventions provide primarily didactic information and some interactive tools—essentially more sophisticated, digital versions of self-help manuals.”Footnote 66 The categories break down in the following ways.
1. Self-Help Digital Tools
Self-help tools leave the patient alone with her laptop or phone to search for helpful mental health programs. These tools include web-based self-help, mobile self-help, and social media. Web-based self-help includes web-based therapy, mental health websites, and web-based employment support. Online CBT programs offer screen-by-screen step-by-step guided therapies by mobile phone or computer; examples include iHelp, Overcome Social Anxiety, Thinking Patterns, and Self Help for Anxiety Management.Footnote 67 Mobile self-help tools move the patient to their mobile phones, using apps to support mental health, and wearables such as smartwatches. Social media has since its origins allowed young people in particular to connect with connect with clinicians about mental health.
2. Telehealth Tools Linking Therapist and Patient
DMHIs bring the live therapist into the therapeutic world, often mixing modalities such as video chats, or both chatbots and live therapists interacting at various times with a patient, texting with a clinician, and mental health support lines. This blends live therapy with a method of sharing mental health information with clinicians on the web, and has been popular with therapists. Such blended care approaches—combining routine in-person therapy with online treatments— are considered more effective than pure online therapies or pure live treatments, with some studies arguing that blended care can reduce the frequency, duration and cost of treatment, while producing the same therapeutic benefits as traditional face-to-face care from a psychologist.Footnote 68
These blended DMHIs are a modest evolution of the traditional platform model of telehealth, with the doctor and patient connecting through a video link (or audio at times), using programs that make the connection easy. See, for example, AGNES Connect®, AMD’s premiere software offering. In the vendor’s words, “[t]his secure and encrypted cloud-based telemedicine platform enables remote clinical healthcare providers to capture and share medical device data, exchange documents and medical images in real-time, and participate in a live video conference – all in a single web-based platform.”Footnote 69
Some programs are hybrid but move one step closer to total reliance on the chatbot to deliver telemental health. One example here is Wysa, a “companion” that has conducted over 100 million conversations; it has both human-to-human texting and overlapping bot-texting, with interfaces that look the same.
3. Immersive Virtual Reality Technologies
Here I locate Virtual Reality (VR) for mental health strategies primarily.Footnote 70 The vendors are enthusiastic about the use of such virtual reality technologies:
Virtual humans inhabit the virtual world exactly as we inhabit our real world, the only difference being that we have created them and their world. They are computer programs programmed to be smart and intelligent in every possible manner, enabling them to hold a meaningful conversation with a real human under all circumstances. In a nutshell, virtual humans are a fine blend of computer graphics and Artificial Intelligence.Footnote 71
Automated therapies for therapy, both online and mobile, are human-presenting automated therapists, such as Ellie, a diagnostic system using an avatar of a professional woman sitting in a therapist’s chair; she is nonthreatening and seems approachable. The Ellie program can read the features of a patient and adjust the response to more accurately adapt to the patient’s tensions and worries. The AI program uses sensors and webcams detect “the affect in speech, postures, and gestures” and facial expression recognition and word analysis is compared to a database, this to gauge patient depression levels and recalibrate the avatar’s responses.Footnote 72 Avatars can address a variety of conditions, including persistent auditory hallucinations for patients with psychosis, using computer-generated images of faces on computer screens or tablets that interact with a patient via intelligent algorithms.
One can be skeptical of vendor enthusiasm, but some studies have found that such Virtual Humans (VHs) do improve clinical interviews by increasing patient willingness to disclose information, overcoming a significant barrier to obtaining truthful patient information.Footnote 73 AI avatars also provide opportunities for different forms of engagement with children suffering from autism spectrum disorders (ASDs), since children with autism often react positively to robots even when they struggle to interact with others. The authors expect that “…therapeutic chatbots, avatars, socially assistive devices, and sex robots will soon translate into broader clinical applications in earnest.”Footnote 74
Access to mental health treatment using such AI applications sounds promising. Like other telemental health modalities, they can reach rural populations, or any area where mental health services are scarce.Footnote 75 The author concludes that “…embodied AI interventions may offer entirely new modes of treatment that are potentially more successful than traditional modalities either because they address hard-to-reach populations or because patients respond better to them.”Footnote 76
AI programs can also scan data such as patient emails to spot suicidal risks. In one study, the authors’ goal was “…to understand how well different machine learning algorithms performed compared to humans who were asked to distinguish between elicited and genuine suicide notes. We confirmed that, at least in part, machine algorithms could do as well as humans.”Footnote 77 Another study of automated analysis of free speech was found to predict psychosis onset in high-risk youths. The authors of the study concluded that “[i]n this initial, proof-of-principle study using a novel combination of automated semantic and syntactic speech analyses, we found that speech recorded and transcribed at baseline could accurately predict subsequent transition to psychosis in a clinical high-risk cohort. Moreover, classification based on automated analysis outperformed that based on clinical ratings, indicating that automated speech analysis can increase predictive power beyond expert clinical opinion.”Footnote 78
The enthusiasm for these DMHIs has flooded the mental health “market” with tempting tools. The tools tempt governments desperately trying to controls costs while providing better services; they are very tempting for private equity seeking an efficient, standardizing set of tools that reduce or eliminate the need for human therapists to serve patients; and they dazzle a public used to the promises of technologists.
Regulation of DMHIs is difficult. Telemental health has been in use for six decades. It may be effective in some settings, although much more research is needed.Footnote 79 This technology— driven by vendor desires to capture market share and government desires to improve access to mental health care in a system that is sadly lacking in therapists—leaves confirmatory evidence-based research far behind. The evolution of chatbots, or avatars, seems to have matured into a full formed therapeutic approach, with possible dissemination of these tools occurring long before studies can be done as to safety, efficacy, and issues of privacy and confidentiality. The world of medical health apps has swollen far beyond any confirmative research as to safety and efficacy. Safety, usability, confidentiality, clinical- and cost-effectiveness are largely untested.Footnote 80
Public policy discussions focus more on cost-saving and resource management than on the implications of these tools of patient surveillance. Footnote 81 News coverage of algorithmic health systems rarely if ever discusses the individual and social harms of algorithmic datafication — the fact of being rendered into statistical formulae for the training of machine learning models.Footnote 82 Many interventions are designed to manipulate or capitalize on the mental states of their users; online advertisers, mental health apps and suicide watch services may be surveilling users without their consent. Critics contend that the design and implementation of algorithmic systems to help people in a mental health crisis are too often predatory, seizing private information for commercial use.Footnote 83
The fever surrounding DMHIs, particulary AI tools of emotionally intelligent computing, is premature. As Bossewitch and his co-authors contend, the market for mental health tools is driving wellness industry entrepreneurs to digitalized care models. They worry that “[i]f left unregulated, AI-based mental-health solutions risk creating new disparities in the provision of care as those who cannot afford in-person therapy will be referred to bot-powered therapists of uncertain quality.”Footnote 84
I will next discuss the amplification of such risks as private equity finance continues to move into the behavioral health market. Tools such as chatbots and human-appearing avatars are irresistible to private equity goals of efficiency at low cost. Chatbots require no salary, just updates and monitoring of larger computer server farms.Footnote 85 What harm do they possibly do?
IV. Private Equity Financing of Behavioral Health Risks Patient Harms
The forest was on fire and all the animals swam across the river to escape the fire. The scorpion could not swim and begged the fox to help him.
“Please take me across the river on your back – or I will die.”
“I am not a fool” said the fox “you will sting me and I will drown.”
“No,” replied the scorpion. “I promise that if you help me – I will not sting you – after all, if you drown then so will I.”
“Okay” the fox agreed, and the scorpion climbed on his back. Halfway across the river, at the deepest part – the scorpion stung the fox.
“Why did you do that?” the fox shouted. “I just couldn’t help it,” cried the scorpion as they both drowned. “It’s just my nature!”Footnote 86
Private equity firms pool money from investors, ranging from wealthy people to college endowments and pension funds. They use that money to buy into businesses they hope to flip at a sizable profit, usually within three to seven years, by making them more efficient and lucrative. Private equity has poured nearly $1 trillion into nearly 8,000 health care transactions during the past decade, according to fund managers who back the deals. Their claims are that they have the expertise to reduce waste and turn around inefficient, or moribund, businesses, and they tout their role in helping to finance new drugs and technologies expected to benefit patients in years to come. Critics see a far less rosy picture. They note that “…private equity’s playbook, while it may work in some industries, is ill suited for health care, when people’s mental health and lives are on the line.” Footnote 87
A. Private Equity Characteristics
Private equity firms are the Goliaths in the world of venture capital financing. In a typical private equity business structure, investors have the status of limited partners.Footnote 88 They tend to be primarily large institutional investors, such as pension funds and endowments, but they may also include some wealthy individuals.Footnote 89 The private equity firm serves as general partner.Footnote 90 Ninety-eight percent of invested capital flows to one or more private equity funds owned by the firm, and two percent goes as fees to the general partner.Footnote 91 The funds in turn create portfolio companies that acquire the facilities.Footnote 92
Private equity companies use invested funds and loans from banks and other financial institutions to finance the acquisitions.Footnote 93 They also pay management and advisory fees to the firm for its services as general partner.Footnote 94 Profits from operations flow to the funds, which distribute them to the limited partners and the firm. The goal is to improve an acquired business, make changes to make the business more efficient, and then flip it in five to seven years to another investor buyer.
Private equity firms claim to have success outside of health care. Private equity comes into a business and promptly implements models of operational reform.Footnote 95 This means that a health care practice might gain expertise in management to build a sales and marketing team, improve or even rebuild software platforms, upgrade information technology (IT) security, or address holes or deficiencies in the executive management team.Footnote 96 A new technology may be imposed that supports scalable operational improvements like standardized workflows that facilitate effective and efficient clinical activities.Footnote 97
Several practice areas and health care models have proved attractive targets for private equity investment in the last decade.Footnote 98 These include physician practices,Footnote 99 telemedicine,Footnote 100 health care information and other technology,Footnote 101 behavioral health,Footnote 102 and aging at home.Footnote 103 Private equity claims success in implementing new technology to improve operational efficiency, including in health care organizations.Footnote 104 Because of this, health care technology is an area of growing investment interest for private equity and a draw for providers with outdated technology systems.Footnote 105 One example is LifeStance, a behavioral health company and a large provider of virtual and in-person mental health care across the country.Footnote 106 LifeStance increased their online presence, driving increased patient volume;Footnote 107 profits could increase through such increased patient utilization and higher prices for care also occurs.
Much of health care provides services to vulnerable populations, such as nursing home and hospice patients…and behavioral health patients.Footnote 108 Health care generally is a poor choice for private equity from a patient health point of view. Private equity’s investments in healthcare have led to increased costs in hospitals and dental practices and also to higher patient deaths in nursing homes.Footnote 109 Recent research found that private equity ownership increases 90-day mortality by 2.4 percents, or 15% of baseline mortality among Medicare residents.Footnote 110 Applying these percentages, the result is around 20,150 deaths over the course of 12 years, beginning in 2005 until 2017.Footnote 111
Private equity interest in behavioral health has focused on a few key areas: autism, eating disorders, and addiction treatment. Firms employ a familiar model in behavioral health: they typically buy or create a platform investment, such as a large treatment center, and then acquire add-on investments to expand the company. Consolidation and improvements to technology and administrative functions are claimed to drive value creation.Footnote 112 But the strategies of private equity owners are often clumsy--private equity marketing has led to a surplus of eating disorder beds and results in pressures to fill these beds.Footnote 113
If PE firms follow their usual model, private equity’s enthusiastic entry into the behavior health market will harm the patient population seeking mental health services. In the words of one commentator, “[F]irms’ tendency to demand outsized returns in a sector that is already vastly underfunded, and serves vulnerable populations, raises serious concerns about the private equity model’s potential impact on patient care.”Footnote 114
B. Why is Behavioral Health Attractive to Private Equity?
Behavioral health care has six features that make it especially appealing for private equity investors. First, demand for behavioral health services is strong and growing. This market is noncyclical.Footnote 115 Treatments will always be needed. As a result, demand and revenue remain steady regardless of the state of the broader economy, and this market is largely immune from recessions.Footnote 116 The COVID pandemic increased mental health demands in the U.S. population quite substantially. Patient demand as a result exceeds the supply of mental health services; mental and behavioral health problems are pervasive in our society, guaranteeing demand growth over time.
Second, stigma attached to mental health treatment has decreased. People are more aware of the pervasiveness of depression and other conditions.Footnote 117 They are willing to seek mental health treatments.
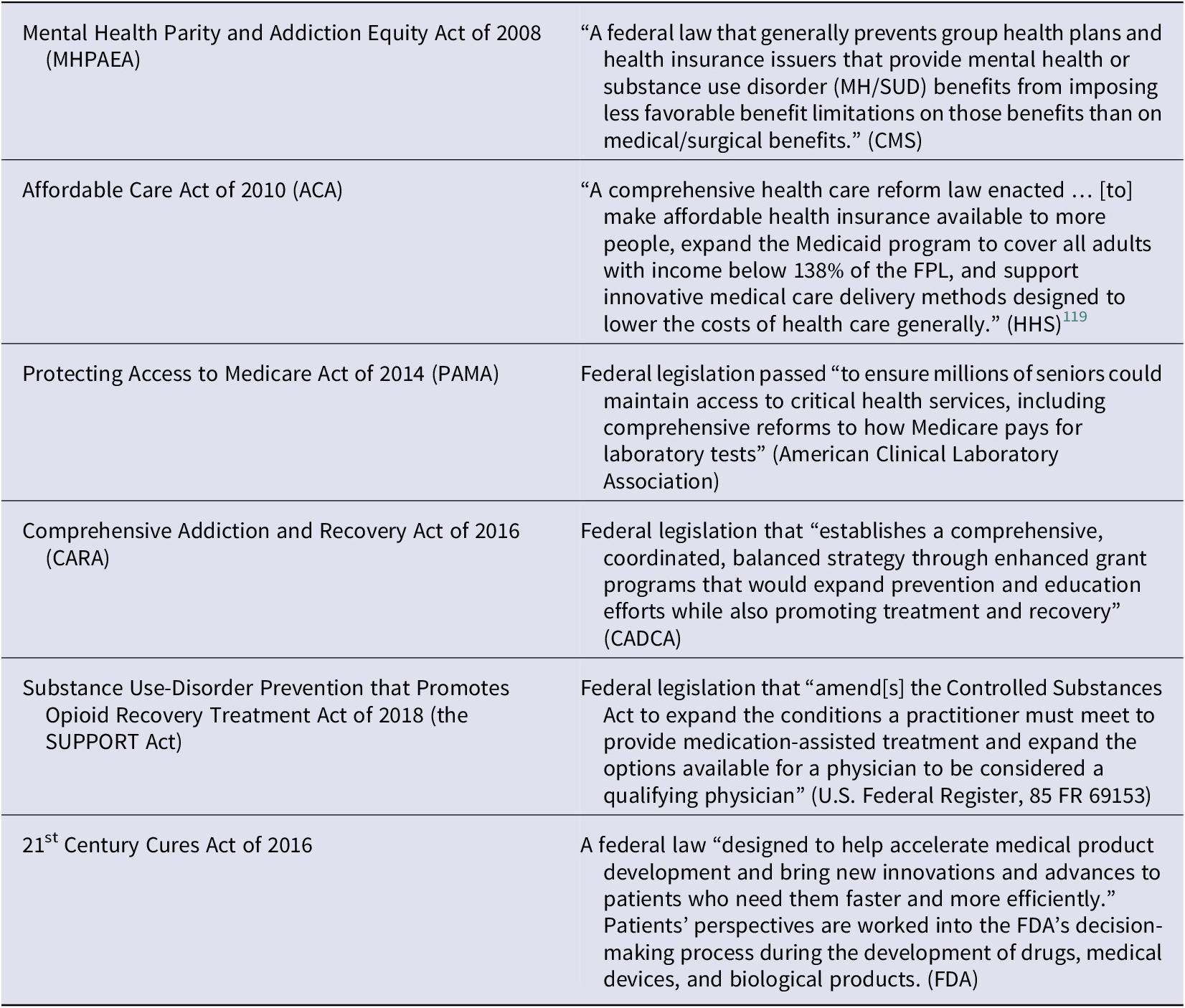
Third, reimbursement for behavioral health treatment has expanded. A variety of government programs such as Medicaid, and employer private insurance, now offer coverage. This means that this is an attractive area, such as nursing homes and hospice care have proved to be –such steady reimbursement insulates private equity from both patient financial inadequacy and the vagaries and risks of financing firms in the retail consumer markets, where customer demand can fluctuate because of competition or changes in market taste. Table 1 illustrates the range of federal programs that either impose parity of payment on private payers or directly reimburses for behavioral health one way or another.Footnote 118
Table 1. A chart illustrating the range of federal programs that either impose parity of payment on private payers or directly reimburses for behavioral health one way or another.
Fourth, behavioral health Footnote programs can in theory switch to less qualified mental health professions as a cost-cutting strategy. Behavioral health is offered by a full range of credentialed mental health professionals, as Figure 1 illustrated. For private equity, the initial temptation is to substitute less-credentialed counselors for expensive psychiatrists and higher paid psychotherapists. The risk is that the owners of a therapy center may be liable under the False Claims Act; see for example the $25 million settlement by South Bay Mental Health Center, Inc. for providing services to patients by unlicensed, unqualified, and improperly supervised staffs members at the company clinics across Massachusetts.Footnote 120
Fifth, the telemental health tools are now covered by federal and private programs. Medicare rules allow remote prescribing of medicine and verbal therapies. Innovative telehealth programs can reduce therapist costs—or eliminate the need for live therapy at all. Behavioral health facilities have historically been small operations, slow to adopt new technologies. Private equity firms enter this market with a dual ambition: lower staff requirements for therapists and whenever possible switch to hybrid treatment to reduce the need for live therapy, or go purely virtual, using only Avatars/chatbots to treat patients.
Sixth, less capital will be required to run a large behavioral health platform. (See reasons 1-5 above). The huge demand for therapy and the attraction to PE owners of shrinking staff and virtualizing therapy has triggered private equity’s fascination in the area.Footnote 121 This promise of substitution of telemental health tools over staff treatment by psychologists and other mental health-quality professionals whenever possible, regardless of evidence as to the merits of such uses in behavioral health treatments, meets the private equity metric of cost conservation by staff reduction.
C. CASE STUDIES: Autism and Troubled Teen Programs
1. Autism treatment
Autism treatment is one of the hottest markets for private equity investors.Footnote 122 It is fragmented and undersupplied, but demand for treatment is high and reimbursement coverage has improved. Because it is a market offering good reimbursement, private equity investors have over the past few years seen an opportunity for investment. The vendors want to expand autism platforms, professionalize the industry and create benefits of scale in recruiting and training, payer relationships and systems to support the patients and staff.
More than $700 million in venture money has gone into autism-focused digital health startups since 2017, with 28 deals, including 17 in the last two years.Footnote 123 That includes a $219 million round for Elemy in October 2021, a $105 million round for Brightline in March and a $60 million round for Cortica in June 2021. TPG Capital formed Kadiant Inc., a behavioral health platform focusing on autism. Recently acquired private equity acquisitions have undertaken “add-on” expansions, such as KKR-backed BlueSprig Pediatrics’ acquisition of Thrive Autism Solutions.Footnote 124
Why are millions of dollars flooding into autism therapy? Because autism treatment centers meet the tests for private equity investment: large demand, reimbursement guarantees, evidence-based therapies, and telemental health tools.
-
A. Large Demand. Demand for autism treatment is huge, with the number of children diagnosed with autism tripling over the past twenty years;
-
B. Reimbursement Guarantees. All 50 states require insurers to pay for autism care, and the state Medicaid programs have to cover it as well. Parity of payment rules have increased reimbursement levels.
-
C. Evidence-based Therapies. Live therapy has been the model of treatment for this complex behavioral condition, with patients presenting with a wide range of autism traits on the spectrum of autism. Treatments like Applied Behavior Analysis (ABA) offer a template for an evidence-based approach that clinicians hope can be a standard of care for autism therapists, and ABA is now a common treatment modality for autism. The claim is that ABA can help an autistic child improve social interaction, learn new skills, maintain positive behaviors, and minimize negative behaviors.Footnote 125
-
D. Telemental Health Tools. ABA can readily become a digital tool, delivered by telemental health tools; this reduces the need to hire more therapists and the resulting salary costs, instead allowing (or forcing) staff therapists to cover more patients, many through the telemental health modality.
The critique of private equity ownership of autism programs is not surprising, given the analysis above. Private-equity owned facilities are accused of forcing therapists to provide set hours of therapy for autistic clients, as part of billing strategies that lead to fraud.Footnote 126 Providers are trained to provide highly individualized treatment plans for each patient but are pressured into cookie-cutter templates. Facilities pressure patients into more therapy for their children; turnover is constant among burnt-out clinicians.
Autism programs have been discovered to have been billing insurers for more therapy than they could possibly deliver, or even double billing, according to lawsuits and audits in multiple states. The reports of billing fraud have led the Government Accounting Office (GAO) to investigate the industry’s practices.Footnote 127
Digital health has already encountered substantial criticism. Telemental health therapy using ABA is now drawing intense private equity interest in autism therapies, since it offers not only a template for treatment but also the cost-saving benefits of expanding the caseloads of the existing therapist staff in facilities, as noted above. Critics say that autism is too complicated to dispense with live therapy and use ABA as a generic template for treatment.Footnote 128 And even if ABA does allow for “efficiencies” in dispensing care, studies of ABA are often flawed or limited.Footnote 129
Autism treatment is too highly variable to allow for the shortcuts and so-called efficiencies of telemental health. Researchers and professionals contend that therapy must be targeted towards a child’s age and condition.Footnote 130 Therapists must spend time with their patients face-to-face, and virtual approaches have yet to be validated. And if behavioral treatment companies try to use less-qualified therapists as a way to save money on staff expenses, it is likely that the virtual tools will likely be less effective as applied by less-trained therapist. Aaron Blocher-Rubin, founder and CEO of Arizona Autism United, a community-based nonprofit that provides ABA and other services to families, and other critics, does not trust the virtualized board-certified behavioral analyst model. Blocher-Rubin notes: “Autism is way too complex. Therapists are way too underqualified to be expected to [only receive virtual support]. There’s no research on a model like this.”Footnote 131

Gabriel Perna, How Autism Became the Latest Target for Disruption, DigitalHealth, December 6, 2022, https://digitalhealth.modernhealthcare.com/digital-health/autism-digital-health-startups-aim-disrupt-amid-aba-challenges
Private equity has responded to economic downturns, refocusing on rolling up existing small behavioral health companies.Footnote 132 Private equity is now ubiquitous in this mental health industry. The large number of “mom and pop” behavioral health providers continue to tempt private equity as firms make “tuck-ins”Footnote 133 popular across the industry, consolidating their treatment platforms..
Startups have responded to the increase in behavioral health investment. Entrepreneurs have emerged to offer everything from virtual therapy services to creating platforms that aid job hunting for autistic adults. Applied behavioral analysis (ABA), a treatment method for autistic children, has become increasingly digitized through telehealth assessments. Research on the autism spectrum proposes new modalities of treatment which may hold promise, such as Hybrid parent/therapist modalities.Footnote 134 A recent randomized clinical trial found that a telehealth-delivered parenting intervention with real-time therapist coaching led to improvements for young children with Development Delay and their caregivers--a promising use of telehealth for underserved families in particular.Footnote 135 The problem is that once private equity consolidates smaller companies into much larger operations, it is reaching the end of the private equity profit life cycle.
The financial playbook for private equity needs to be emphasized, as PE more intensely focuses on rate of return than do venture capital firms generally. The financial elements of PE are predictable: PE demands a 300% rate of return after 5-7 years, and typically a firm moves on at that point, selling the new consolidated firm after having extracted value from the firm and often leaving it in poor condition.
PE typically loads up acquired firms with high levels of debt. The strategy is to leverage debt on the firms acquired in order to pay themselves and other shareholders dividends in the order of magnitude of hundreds of millions of dollars.Footnote 136 Such financing destabilizes the new behavioral health companies, often resulting in their closing. Two private equity-backed companies—Delphi Behavioral Health Group and Mindpath Health—announced in 2023 that they were closing large parts of their operations.Footnote 137 This debt-driven rapid growth often proves destructive to the patients of behavioral health facilities, who must find new sources for treatment.
Cost-cutting is also a central PE tool which helps to hit their rate-of-return metrics; for example, it may combine billing, legal and human resource departments to cut “wasteful” overhead; such companies typically push prompt billing aggressively, alienating families that need the therapy. Staffs are reduced in size to save salary costs. As a result, companies are tempted to migrate to telemental health platforms, with companies like Elemy now using board-certified behavioral analysts purely through telemental health platforms.Footnote 138 The norm in autism treatment is one therapist for ten children, and the elimination of live therapy and the use of remote digital treatments is troubling.
The evidence of harms from private equity ownership is discouraging. Autism treatments need more providers, and there has been optimism about the creation of new programs for treatment funded by private equity. But the overbilling frauds that seem to have become commonplace, the rush to adopt hybrid approaches that overtax the live therapist, and the limits of ABA therapy leave an observer to expect another distressed industry in the making in the hands of private equity owners. The playbook has not changed; it is the very nature of private equity to rush toward profit while damaging the company it created.
2. The Troubled Teen Industry (TTI)
A second case study is provided by the Troubled Teen Industry (TTI). Private equity firms are increasingly investing in companies specializing in behavioral services for children and adolescents. The Troubled Teen Industry (TTI) refers to a collection of companies and services designed to change and control the behavior of youth with behavioral challenges, youth with depression, anxiety, or addiction disorders, and youth who act out in ways their parents have difficulty managing. These services include therapeutic boarding schools, residential treatment centers, religious academies, wilderness programs, boot camps, and drug rehabilitation centers.Footnote 139
For-profit companies, including those that are private equity owned, increasingly make up a significant share of providers. Privatization has long been characteristic of Troubled Teen facilities, as states struggle to balance their budgets by offloading state-run facilities, considering this troubled teen population as less central to state health care spending. Footnote 140 One critic notes: “Anyone on the street hearing that these children were being exploited as a profit center for wealthy financiers would recoil. Yet foster care and other services have been almost entirely privatized, as a way to lighten strained government budgets. The horror show of private equity bottom-feeding is the result.”Footnote 141
State obligations to provide safe environments for troubled, orphaned, or developmentally disabled youth seems to have been abandoned.Footnote 142 These for-profit youth behavioral health facilities and for-profit foster care have been criticized by youth justice and disability rights advocates. The list of mistreatments by such facilities is quite remarkable: inadequate counseling or education services; physical, sexual, and emotional abuse; forced isolation; use of physical and chemical restraints; and squalid living conditions. Footnote 143
Private equity is now increasing its share of the market, investing in not only “troubled teen” centers, but also for-profit foster care services, and services for young people with intellectual and developmental disabilities. The steady supply of at-risk youths coupled with government health care dollars is attractive. Private equity has also used its business model, the rollup, to expand their platforms and consolidate the small firms that generally have offered behavioral programs for troubled teens.Footnote 144
Private equity’s goal as discussed above is primarily to make outsize returns from health care activities that meet its goals: steady federal and private insurance availability with little due diligence monitoring for quality, high demand for these mental health services, a fragmented market, and the ability to use debt financing to rollup or other create and consolidate care—for resale in five to seven years.
Private equity’s goal is not to provide care and treatment when needed in a safe and healthy environment; instead, the goal is driven by the beating heart of private equity—outsized returns for investors. Firms have earned hundreds of billions in dividend and management payments, while evidence proliferates of inadequate staffing, little of no training of counselors, substandard living conditions, abuse of all kinds, use of restraints and confinement, and even deaths of children less unsupervised.Footnote 145
The industry response to this critique is provided by Mark Zitter, owner of a private equity firm, who argues that the health care system has misaligned incentives that are not unique to PE activities: “[p]rivate equity activity mainly amplifies the best and worst aspects of U.S. healthcare. Many people rail against profit in healthcare, but profit seeking is not the main problem; it’s revenue seeking, which happens just about as much with not-for-profit as with for-profit healthcare organizations.”Footnote 146 My earlier discussion makes clear that private equity defenders like Zitter refuse to acknowledge that private equity finance is an order of magnitude beyond venture capital in its vampire-like ability to extract value from health care industries, too often leaving nothing left but the shell.
My conclusion is that health care service settings with vulnerable populations, illustrated by the case studies, are the wrong places for private equity investment. Private equity financing is not just any for-profit approach to a market need: it is a special form of investing on steroids, creating investment and management targets that move patients to a secondary role to. Reforms are needed to protect the vulnerable.
V. Strategies For Improving Behavioral and Mental Health Therapies Footnote 147
A scorpion and a tortoise became such fast friends that they took a vow that they would never separate. So when it happened that one of them was obliged to leave his native land, the other promised to go with him. They had traveled only a short distance when they came to a wide river. The scorpion was now greatly troubled.
“Alas,” he said, “you, my friend, can easily swim, but how can a poor scorpion like me ever get across this stream?”
“Never fear,” replied the tortoise; “only place yourself squarely on my broad back and I will carry you safely over.”
No sooner was the scorpion settled on the tortoise’s broad back, than the tortoise crawled into the water and began to swim. Halfway across he was startled by a strange rapping on his back, which made him ask the scorpion what he was doing.
“Doing?” answered the scorpion. “I am whetting my sting to see if it is possible to pierce your hard shell.”
“Ungrateful friend,” responded the tortoise, “it is well that I have it in my power both to save myself and to punish you as you deserve.” And straightway he sank his back below the surface and shook off the scorpion into the water.Footnote 148
Do we have it in our power to channel the large financial resources of private equity investors while still protecting the vulnerable populations in the health care areas such as behavioral health?
Let’s start with the reluctant assumption that we don’t want to prohibit private investors generally from investing in health care enterprises, since the investment resources of investors interested in good investments available are huge.Footnote 149 We have also largely privatized whole elements of our health care system, from nursing homes to hospices, with hospitals hanging on to their non-profit status often just for tax breaks. We have generally tolerated privatization without effective regulation and policing of the side-effects of private equity.
Let’s assume further that investors are willing to risk a lower rate of return in order to actually serve the health and welfare of vulnerable health care populations, as private equity investors sometimes assert.Footnote 150 Let’s further assume that we can impose a fiduciary duty on private equity owners to put the interests of their wards first. Can the tools of private equity then be sufficiently restrained, refined, regulated, and restricted to put those investment resources to good use? I suggest eight regulatory ideas (including private law as well as state and federal regulatory approaches) to enhance the obligations of private equity to act ethically, while disciplining and restraining its playbook of profiteering.Footnote 151
First, federal pre-merger review should be required of all private equity-backed merger and acquisition practices. No dollar value will be required – this will require amendment of the Hart-Scott-Rodino threshold of $101 millionFootnote 152. This review will be conducted by the Federal Trade Commission (FTC) and Department of Justice (DOJ), and the US Department of Health and Human Services (HHS) should also be authorized to review such activities for quality and access risks. (PESP).Footnote 153
Second, state health departments should have multi-agency healthcare transaction approval processes for healthcare transactions. This should “…include state attorneys general, administrative agencies, and patient advocates and labor organizations.” (PESP)Footnote 154 Such state regulators should have pre-transaction notice; time to review transactions; the ability to approve, conditionally approve, or block transactions; and the means to oversee conditionally approved transactions.Footnote 155
Third, the Food and Drug Administration (FDA) should be tasked with more aggressive review authority. Mental health programs and apps should be evaluated to confirm both their safety and effectiveness.Footnote 156
Fourth, the Securities and Exchange Commission (SEC) should impose enhanced disclosure requirements on the investments and activities of private equity funds.Footnote 157 A proposed rule is awaiting comments.
Fifth, the federal False Claims Act should be aggressively applied to police the actions of private equity firms. False claims enforcement is a fully developed tool in the federal arsenal, for firms that submit false claims for payment to Medicare and Medicaid. Furthermore, during the investigation phase of a false claims matter in which the health care company being targeted is owned by private equity, discovery should be directed at the private equity firm itself — and not just the health care company.Footnote 158
Sixth, tort civil suits should be encouraged against bad actors in behavioral health, applying theories of corporate negligence and fiduciary doctrine.Footnote 159 These civil law tools have the potential to reach higher in the chain of ownership beyond an individual facility.
Seventh, research on evidence-based behavioral therapy tools and on the use of virtual and telehealth should be better funded. Regulatory agencies including CMS need to better ensure both quality and cost effectiveness.Footnote 160 Clinical practice guidelines must be one goal of such research, using metrics such as quality of care, cost, and access.
Eighth, accreditation should be required of all programs. The Troubled Teen Industry and Autism Programs should require Joint Commission or NCQA accreditation— to force private owners to pay attention to clinical practice guidelines and best practices for therapies.Footnote 161 Such accreditation will also force more transparency in the ownership structure of private equity firms.
Conclusion
The mental health needs of patients in the U.S. are large and growing. One could wish for nonprofit entities to step into this market and meet this demand; one could hope that the federal government would expand its own federal clinics to meet the demand. However, we have moved too far down the path of privatization of major portions of our health care system to expect such dramatic changes in ownership of health care facilities. Private investors such as venture capitalists and private equity firms offer investors a way to put their money to work in health care (with expected high rates of return on investment). What could go wrong?
The history of private equity in health care is unfortunately a troubling one— shortchanging patient needs for effective treatment as the owners push aggressively to meet profit metrics that often weaken or even destroy the health care entities they have built. We need to create a more robust regulatory environment to better police private equity investment and to fund more research into evidence-based mental health treatments.





