Introduction
There is evidence that some migrant groups are at higher risk of psychosis than the host population (Morgan, Knowles, & Hutchinson, Reference Morgan, Knowles and Hutchinson2019; Selten et al., Reference Selten, Zeyl, Dwarkasing, Lumsden, Kahn and Van Harten2005). A recent meta-analysis reported that the risk for non-affective psychotic disorder among first- and second-generation migrants from countries outside Europe is approximately three times higher than that for the local European population (Selten, Van Der Ven, & Termorshuizen, Reference Selten, Van Der Ven and Termorshuizen2019). There is no evidence that these differences can be explained by an increased incidence in their countries of origin: studies conducted in Jamaica (Hickling & Rodgers-Johnson, Reference Hickling and Rodgers-Johnson1995), Trinidad (Bhugra et al., Reference Bhugra, Hilwig, Hossein, Marceau, Neehall, Leff and Der1996), Barbados (Mahy, Mallett, Leff, & Bhugra, Reference Mahy, Mallett, Leff and Bhugra1999) and Surinam (Selten et al., Reference Selten, Zeyl, Dwarkasing, Lumsden, Kahn and Van Harten2005) have found incidence rates of psychosis lower than those observed in migrants from these countries in the UK and the Netherlands. In addition, the magnitude of this risk increase varies by minority group and by host country: in the UK, the incidence is highest among black African and Caribbean groups, while in the Netherlands, the incidence is highest among North African migrants (Bourque, van der Ven, & Malla, Reference Bourque, van der Ven and Malla2011). Moreover, studies in Bologna (Tarricone et al., Reference Tarricone, Boydell, Kokona, Triolo, Gamberini, Sutti and Berardi2016), Turin (Cardano, Scarinzi, Costa, & d'Errico, Reference Cardano, Scarinzi, Costa and d'Errico2018) and Sweden (Price, Dalman, Zammit, & Kirkbride, Reference Price, Dalman, Zammit and Kirkbride2018) have shown that internal migration is also associated with a higher incidence of psychotic disorders. These studies taken as a whole suggest that environmental factors in the countries to which people migrated (post-migration phase) may play a part in the genesis of psychosis among migrants.
It is intriguing to examine the impact of social adversities during different phases of migration, which can be schematically divided into three phases: pre-migration, migration and post-migration (Bhugra & Becker, Reference Bhugra and Becker2005).
There is emerging evidence that specific indicators of social disadvantage, which may be related to the migration experience, are associated with psychosis, such as, unemployment, poor living conditions, single status and limited social networks (Stilo et al., Reference Stilo, Gayer-Anderson, Beards, Hubbard, Onyejiaka, Keraite and Morgan2017). Refugees have been shown to be at an increased risk of non-affective psychotic disorder compared with other migrants from the same region of origin, suggesting that pre-migratory traumas and disadvantage may be important determinants of risk (Hollander et al., Reference Hollander, Dal, Lewis, Magnusson, Kirkbride and Dalman2016). Moreover, most studies conducted after 2001 support an association between low SES at birth and psychosis (Kwok, Reference Kwok2014). Social disadvantages could be relevant in both the pre-migration and post-migration phases. However, some studies conducted in the UK showed that adjustment for socioeconomic status does not fully explain the risk of psychosis in black and minority ethnic groups (Kirkbride et al., Reference Kirkbride, Barker, Cowden, Stamps, Yang, Jones and Coid2008, Reference Kirkbride, Hameed, Ioannidis, Ankireddypalli, Crane, Nasir and Jones2017): these studies suggest that there are probably other social determinants of psychosis in these populations. One such example could be the subjective evaluation of a mismatch between expectations and achievements, which has been associated with psychosis onset (Reininghaus et al., Reference Reininghaus, Morgan, Simpson, Dazzan, Morgan, Doody and Craig2008); if such a mismatch was more pronounced in migrant groups, this could account for some of the excess risks here. Finally, some variables during the migration phase have been found to be associated with a higher risk of psychosis in migrants, such as lower age at the time of migration (Anderson & Edwards, Reference Anderson and Edwards2020; Veling, Hoek, Selten, & Susser, Reference Veling, Hoek, Selten and Susser2011), and other characteristics of the migration phase often ascribed to refugees and asylum seekers such as detention/trauma during the journey and leaving the country of origin without any chance of returning because of hostile conditions there (Abubakar et al., Reference Abubakar, Aldridge, Devakumar, Orcutt, Burns, Barreto and Zhou2018; Dapunt, Kluge, & Heinz, Reference Dapunt, Kluge and Heinz2017).
However, as already noted (Bhugra, Reference Bhugra2004), most of the studies available collected only post-migratory social disadvantages and apply to both migrants and more settled minorities, thus missing the opportunity of evaluating pre-migration social disadvantages and adversity during migration.
Along with the socio-developmental model (Morgan et al., Reference Morgan, Knowles and Hutchinson2019), we hypothesized that the likelihood of psychotic disorder in migrants may increase as a consequence of cumulative exposure to social disadvantages and adversities during the migration process and of mismatch between expectations and achievements.
To test these hypotheses, we examined whether social disadvantages in the country of origin, adversities during the migration process, social disadvantages in the country of arrival, and the mismatch between pre-migratory expectations (health, work, income, family, friends) and post-migratory achievements differed between first-generation migrant cases and controls. We tested whether these accounted for differences in odds of psychotic disorders after adjusting for ethnicity and known risk factors for psychosis (family history of psychosis, childhood trauma, education, lifetime cannabis use), length of stay following migration and language fluency in first-generation migrants. We used data from the six-country EUropean network of national schizophrenia networks studying Gene-Environment Interactions (EU-GEI; work package 2) case–control study, which included these exposure measures in an ethnically- and culturally-diverse sample.
Methods
Study design and participants
The aim of the EU-GEI case–control study was to assess in detail 1000 FEP cases and 1000 population-based controls during the same time span. Participants were recruited between 1 May 2010 and 1 April 2015 from 16 centres in England, the Netherlands, Spain, France, Italy and Brazil. All persons aged 18–64 years who made contact with mental health services for a probable first episode of psychosis (FEP) were invited to participate via their mental healthcare provider (Gayer-Anderson et al., Reference Gayer-Anderson, Jongsma, Di Forti, Quattrone, Velthorst, de Haan and Morgan2020). Cases were included if they met the International Classification of Disease (ICD)-10 criteria for non-affective or affective psychotic disorder (F20–33), ascertained using the Operational Criteria Checklist (OPCRIT) algorithm (Williams et al., Reference Williams, Farmer, Ackenheil, Kaufmann, McGuffin and Group1996).
In each centre, we recruited population-based first-generation migrants (controls) aged 18–64 years using a mixture of random and quota-sampling strategies, to maximize representativeness to the population-at-risk by age, sex and ethnicity in each catchment area. Quotas for control sampling were derived based on the most accurate local demographic data. Individuals with a history of psychotic disorder, or taking anti-psychotic medication, were not eligible (Di Forti et al., Reference Di Forti, Quattrone, Freeman, Tripoli, Gayer-Anderson, Quigley and van der Ven2019; Gayer-Anderson et al., Reference Gayer-Anderson, Jongsma, Di Forti, Quattrone, Velthorst, de Haan and Morgan2020). For the purpose of the present study, we included only first-generation migrants (i.e. people born outside the country where they lived at the time of the study). Migrant cases were included in the final study sample only if they had FEP after migration.
Ethical approval was granted in each centre. All participants gave written informed consent.
Measures
Our primary outcome was case–control status, with cases defined as receiving an OPCRIT-confirmed ICD-10 diagnosis of any psychotic disorder (ICD-10 codes F20-F33). Age at onset was determined using the Nottingham Onset Schedule (NOS) (Singh et al., Reference Singh, Cooper, Fisher, Tarrant, Lloyd, Banjo and Jones2005). Our main exposures were variables that operationalized the constructs of social disadvantages and adversities in pre-migration, migration and post-migration phases. Ethnicity was coded by self-ascription to six categories: White (Caucasian), Black, Mixed, Asian, North African and other, and dichotomized into white and non-white groups for analyses.
Data on the social disadvantage and adversity variables in the pre-migration, migration and post-migration phases were collected using an amended version of the Medical Research Council Socioeconomic Schedule (MRC SDS) (Mallet, Reference Mallet1997) and the Bologna Migration History and Social Integration Interview (Bo MH&SI Interview) (Tarricone et al., Reference Tarricone, Atti, Braca, Pompei, Morri, Poggi and Berardi2011) (see online Supplementary Materials). Based on previous evidence, we defined social disadvantage as a combination of low parental social class (Agerbo et al., Reference Agerbo, Sullivan, Vilhjálmsson, Pedersen, Mors, Børglum and Mortensen2015), unemployment (Reininghaus et al., Reference Reininghaus, Morgan, Simpson, Dazzan, Morgan, Doody and Craig2008), living arrangement dependent on the family of origin (Tarricone et al., Reference Tarricone, Mimmi, Paparelli, Rossi, Mori, Panigada and Berardi2012), absence of a long-term relationship (Huang et al., Reference Huang, Hou, Huang, He, Wang, Chen and Jia2019; Van Os, Driessen, Gunther, & Delespaul, Reference Van Os, Driessen, Gunther and Delespaul2000) and scarce social network (Gayer-Anderson & Morgan, Reference Gayer-Anderson and Morgan2013; Michalska Da Rocha, Rhodes, Vasilopoulou, & Hutton, Reference Michalska Da Rocha, Rhodes, Vasilopoulou and Hutton2018). Young age at migration, detention during migration and absence of any plans to return to the country of origin were characteristics chosen to describe adversities during migration phase (Anderson & Edwards, Reference Anderson and Edwards2020; Hollander et al., Reference Hollander, Dal, Lewis, Magnusson, Kirkbride and Dalman2016; Veling et al., Reference Veling, Hoek, Selten and Susser2011). We tried to disaggregate the timing of exposures to social disadvantages and adversities during the migration process and, thus, we defined a set of three indicators of social disadvantage for each phase of migration: the pre-migration social disadvantage index, the migration phase adversity index and the post-migration social disadvantage index (online Supplementary Fig. S1). For the pre-migration social disadvantage index (scoring 0–3), we used parental social class (salaried/intermediate v. working class/long-term unemployed), employment (ever/never employed before migration) and living arrangements (ever lived with people other than the family of origin; yes/no). For the migration adversity index (scoring 0–3), we used: migration prior to 18 years old (yes/no), detention during migration (yes/no), ever returned to the country of origin (yes/no). For the post-migration social disadvantage index (scoring 0–3), we used: employment (ever/never employed in the last 5 years of the post-migration phase), relationship status (ever/never in a long-term relationship in the last 5 years of the post-migration phase), and family and social network in the post-migration phase (any social network outside of their family of origin in the country of arrival: yes/no). The indices were treated as continuous variables in the statistical models. We also adjusted the statistical models with numbers of years spent in the country of arrival after migration. We assessed the self-evaluated mismatch between expectations and achievements following migration (scoring 1 – not at all satisfied, to 4 – completely satisfied). The interview covers five main domains (health, work, income, family and friends) and the possible values range is 1–20. Both years after migration and expectations/achievements mismatch were treated as continuous variables in the logistic regression models.
We also adjusted for known risk factors for psychosis (Di Forti et al., Reference Di Forti, Quattrone, Freeman, Tripoli, Gayer-Anderson, Quigley and van der Ven2019; Esterberg, Trotman, Holtzman, Compton, & Walker, Reference Esterberg, Trotman, Holtzman, Compton and Walker2010; Frissen, Lieverse, Marcelis, Drukker, & Delespaul, Reference Frissen, Lieverse, Marcelis, Drukker and Delespaul2015; Ochoa, Usall, Cobo, Labad, & Kulkarni, Reference Ochoa, Usall, Cobo, Labad and Kulkarni2012; Varese et al., Reference Varese, Smeets, Drukker, Lieverse, Lataster, Viechtbauer and Bentall2012): sex, country, educational attainment (0 = higher, 1 college/vocational; 2 = school qualification/tertiary; 3 = no school qualifications), parental history of psychosis, lifetime cannabis use (all categorical), age, childhood trauma and language fluency (all continuous). Age, sex and education were derived from the MRC SDS. Parental history of psychosis was recorded using the Family Interview for Genetic Studies questionnaire (Maxwell, Reference Maxwell1992). Childhood total maltreatment score was derived from the Childhood Trauma Questionnaire (CTQ) (Bernstein et al., Reference Bernstein, Stein, Newcomb, Walker, Pogge, Ahluvalia and Zule2003). Lifetime cannabis use was derived from a modified version of the Cannabis Experience Questionnaire (Di Forti et al., Reference Di Forti, Morgan, Dazzan, Pariante, Mondelli, Marques and Murray2009). In addition, we also adjusted for the country where the sample was recruited, using UK as reference category (v. the Netherlands, Spain, France, Italy and Brazil). Finally, we also adjusted for fluency in the majority language of the country of residence as there is some evidence that linguistic distance may be associated with the odds of a psychotic disorder (Jongsma et al., Reference Jongsma, Gayer-Anderson, Tarricone, Velthorst, van der Ven, Quattrone and Kirkbride2020). Fluency in the majority language was self-rated on a 10-point scale and used as a continuous variable.
Missing data
We investigated patterns of missingness by using binary logistic regression to test associations between covariate missingness and case–control outcome. We also compared complete and non-complete cases for confounders and exposures using χ2 tests. Then, we used Multiple Imputation (MI) by chained equations to handle missing data. All covariates and our outcome were included in the MI algorithm (White, Royston, & Wood, Reference White, Royston and Wood2011). Following the rule of thumb that the number of imputations should be at least equal to the percentage of incomplete cases (White et al., Reference White, Royston and Wood2011), we imputed 55 data sets, and conducted our analyses combining estimates across them (Manly & Wells, Reference Manly and Wells2015). We also carried out complete-case analyses as a sensitivity analysis (see online Supplementary Materials).
Statistical analyses
Firstly, we calculated weights, which were applied in all analyses, to account for over-sampling of controls relative to the populations at risk. Weights were calculated using inverse probability and were applied in all analyses (Gayer-Anderson et al., Reference Gayer-Anderson, Jongsma, Di Forti, Quattrone, Velthorst, de Haan and Morgan2020). Following MI, we used binary logistic regression to examine the associations between ethnicity, pre-migration, migration and post-migration social disadvantages and adversities and other exposures and confounders as follows:
Unadjusted Model: Crude (univariable) odds ratios (OR) were estimated to quantify the associations between case–control status and pre-migration, migration, post-migration social disadvantage and adversity indices and mismatch between expectations and achievements.
Adjusted Model A: ORs were adjusted for country, age, sex, ethnicity, education, family history of psychosis, childhood trauma, cannabis use, language fluency, years after migration.
Adjusted Model B: Finally, to see which migration indices were still significantly associated with case–control status, ORs were adjusted for all above variables plus pre-migration and post-migration disadvantage indices, migration adversity index, and mismatch between expectations and achievements.
Finally, in order to examine the possible dose–response relationships, we calculated the total number of the migration disadvantages/adversities as the sum of the variables representing pre-migration and post-migration disadvantages and migration adversities. This variable was recoded as zero, one, two, three, four, five or six or more adversities. We treated this variable as an ordinal predictor and calculated unadjusted and adjusted OR of FEP for each level. We controlled for all covariates included in Model A plus achievements/expectations mismatch.
We presented OR and 95% confidence intervals (95% CI) where appropriate, and analysed data using IBM-SPSS-Statistics 25.
Role of the funding source
Study funders contributed to the salaries of the research workers employed but did not participate in the study design, data analyses, data interpretation or writing of the manuscript. All authors had full access to the study data and had final responsibility for the decision to submit for publication.
Results
Between 2010 and 2015, 1.130 cases and 1.497 controls were recruited and assessed across 17 sites in six countries (UK, the Netherlands, France, Spain, Italy and Brazil). Among them, 256 cases (22.7%) and 219 controls (14.6%) were migrants and were included in this study. Seven cases had FEP before migration and were thus excluded from the analyses. This resulted in a sample of 468 individuals (Table 1).
Table 1. Descriptive characteristics of the case–control sample
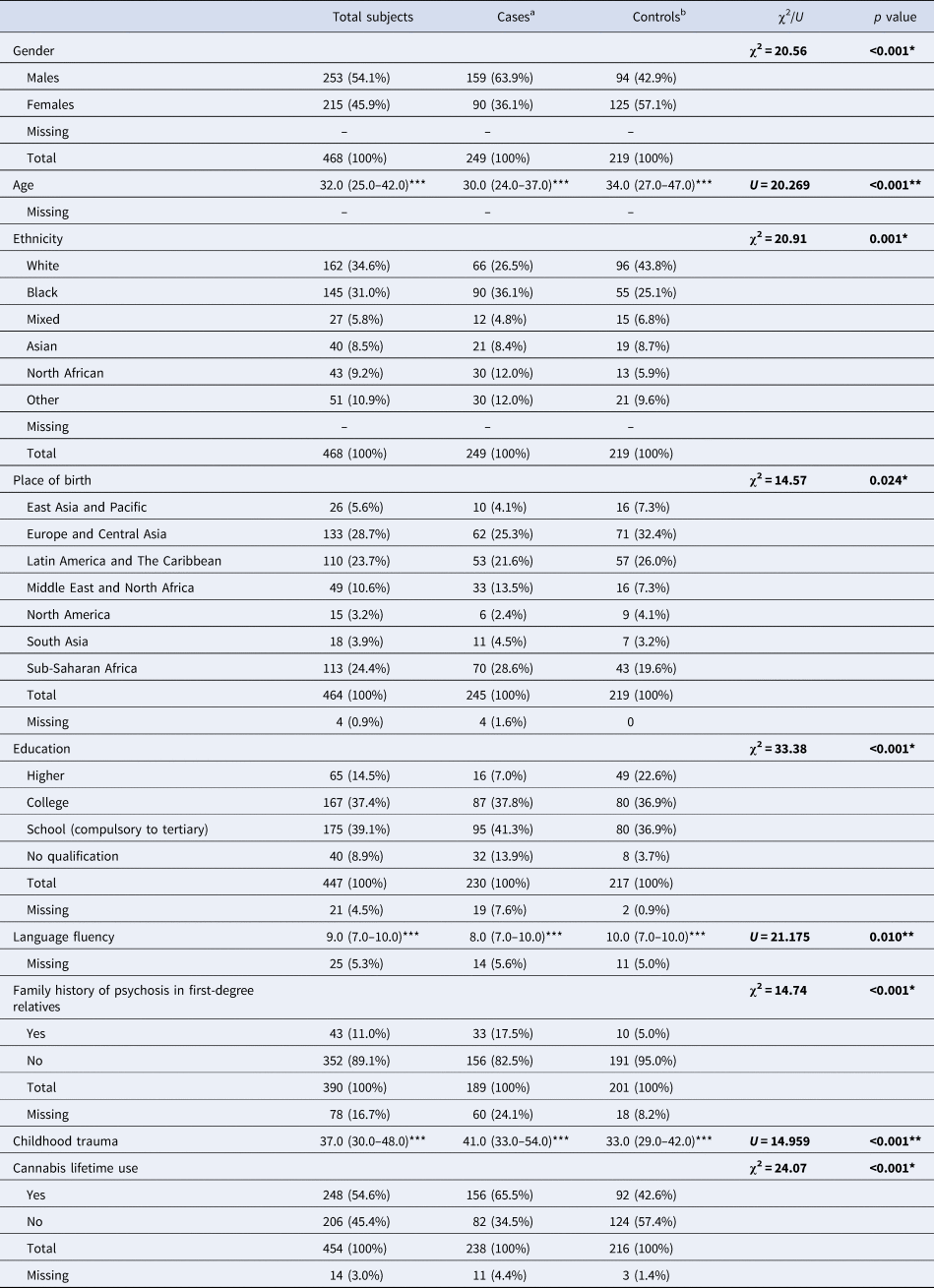
*Pearson's χ2 test; **Mann–Whitney U test; ***median and interquartile range; ****Fisher's exact test.
Bold values denote statistical significance at the p<0.05 level.
a First-generation migrants with FEP.
b Healthy first-generation migrants.
Missing data
The proportion of participants with missing data (Table 1, Table 2) for socio-demographic and migration variables collected with the Bo MH&SII interview ranged from none missing on sex, age and ethnicity to 145 (31.0%) on the mismatch between income expectations and achievements. Complete data were available for 209 individuals (44.66% of the total sample). Missingness was higher for cases than controls for the following variables: education (χ2 = 12.28, p < 0.001), family history of psychosis (χ2 = 21.15, p < 0.001), childhood trauma (χ2 = 29.67, p < 0.001), ever employed before migration (χ2 = 6.39, p = 0.011), living conditions before migration (χ2 = 5.39, p = 0.02), detention during migration (χ2 = 6.91, p = 0.009), presence of family of origin in the country of arrival (χ2 = 8.48, p = 0.004), expectations and achievements (χ2 = 4.73, p = 0.03). Cases were more likely to yield incomplete data and therefore to be excluded from the final logistic regression model (χ2 = 31.37, p < 0.001). Participants included in the final model had lower education (χ2 = 13.41, p = 0.004) and higher CTQ (χ2 = 11.08, p = 0.001). Analyses on the complete sample have also been carried out and results are reported in the online Supplementary Tables S1 and S2.
Table 2. Characteristics of the migratory process
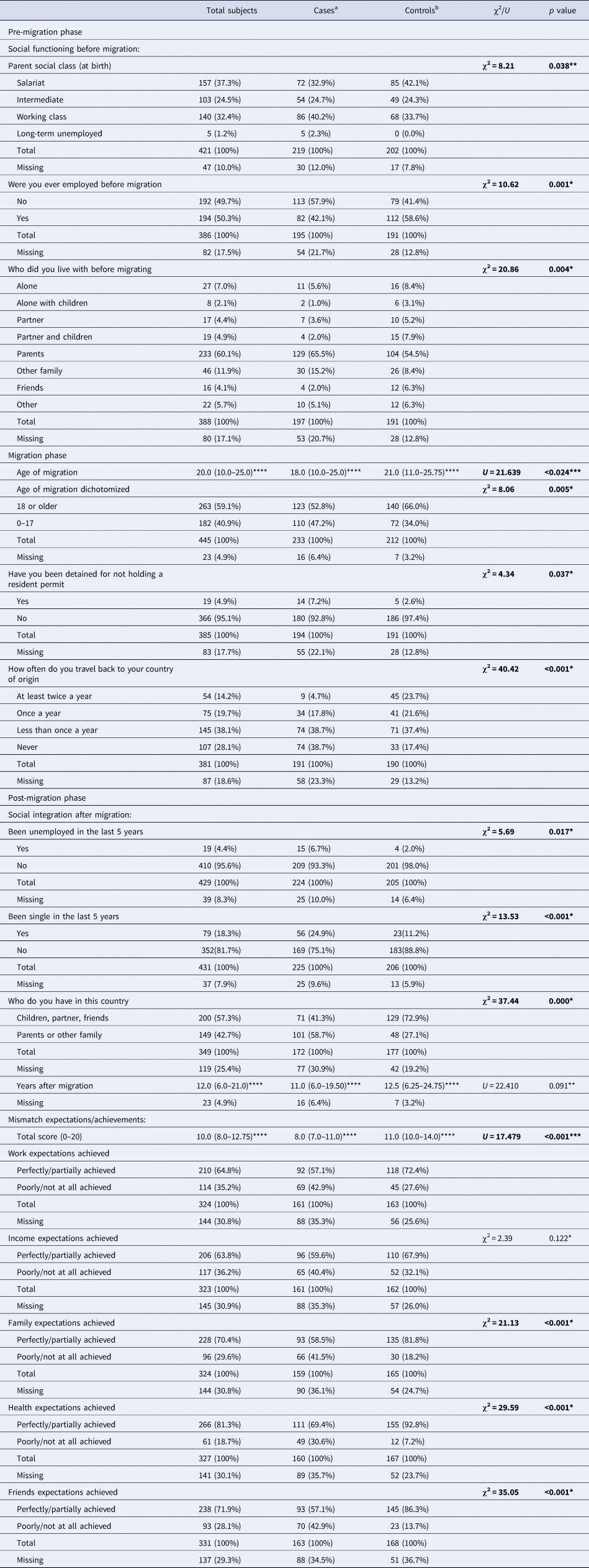
*Pearson's χ2 test; **Fisher's exact test; ***Mann–Whitney U test; ****median and interquartile range.
Bold values denote statistical significance at the p<0.05 level.
a First-generation migrants with FEP.
b Healthy first-generation migrants.
Characteristics of the sample
Cases were more frequently men (159, 63.9% v. 94, 42.9%; χ2 = 20.59; p ⩽ 0.001), black (90, 36.1% v. 55, 25.1%) or North African (30, 12.0% v. 13, 5.9%; χ2 = 20.1, p ⩽ 0.001) and they were younger (median 30.0, interquartile range 24.0–37.0 v. median 34.0, interquartile range 27.0–47.0; U = 20.269; p ⩽ 0.001) (Table 1). Cases had lower education (p ⩽ 0.001) and lower language fluency (p = 0.01) than controls.
Pre-migration phase
Cases were more likely to have lower parental social class at birth (126, 57.6% v. 134, 66.4%; χ2 = 8.21, p = 0.038) and less likely than controls to have lived with someone other than their family of origin (68, 35.5% v. 87, 45.5%; χ2 = 20.86, p = 0.004) or to have been lifetime-employed in the pre-migration phase (82, 42.1% v. 112, 58.6%; χ2 = 10.62, p = 0.001) (Table 2). A single-point increase in the pre-migration social disadvantage index (range 0–3) was associated with increased odds of psychosis in the unadjusted (OR 1.61, 95% CI 1.19–2.17, p = 0.002, Nagelkerke's R 2: 0.058) and in the final model (ORA 1.55, 95% CI 0.99–2.41, p = 0.051, Nagelkerke's R 2: 0.392; ORB 1.61, 95% CI 1.06–2.44, p = 0.027, Nagelkerke's R 2: 0.485) (Table 3).
Table 3. Unadjusted and adjusted odds ratios for first-episode psychosis
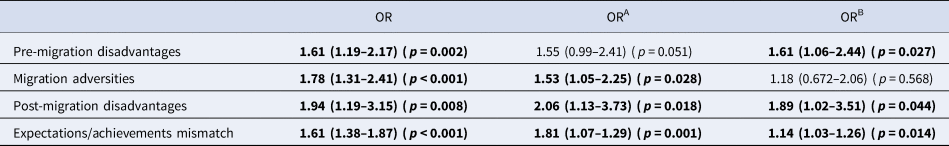
OR = unadjusted.
ORA = adjusted for site, age, gender, ethnicity, education, family history of psychosis, childhood trauma, cannabis use, language fluency, years after migration.
ORB = adjusted for all above variables plus pre-migration and post-migration disadvantages, migration adversities and expectations/achievements mismatch.
ORs in bold are significant (p < 0.05).
Migration phase
Cases were younger than controls when they migrated (median 18.0, interquartile range 10.0–25.0 v. median 21.0, interquartile range 11.0–25.75; U = 21.639; p ⩽ 0.024) and had been detained more often during the migration process (14, 7.2% v. 5, 2.6%; χ2 = 4.34; p = 0.037) (Table 2). More cases than controls had never travelled back to their countries of origin (74, 38.7% v. 33, 17.4%; χ2 = 40.42; p ⩽ 0.001) and considered the country of arrival as the last step in their migration (128, 69.2% v. 98, 53.6%, p = 0.002) (Table 2).
A single-point increase in the migration phase adversity index (range 0–3) was associated with increased odds of psychosis (OR 1.78, 95% CI 1.31–2.41, p ⩽ 0.001, Nagelkerke's R 2: 0.090). This was attenuated in the adjusted models (ORA 1.53, 95% CI 1.05–2.25, p = 0.028, Nagelkerke's R 2: 0.394; ORB 1.18, 95% CI 0.672–2.06, p = 0.568, Nagelkerke's R 2: 0.485) (Table 3).
Post-migration phase
Cases were more likely never to have been employed in the last 5 years of the post-migration phase (15, 6.7% v. 4, 2.0%; χ2 = 5.69; p = 0.017), to be single (56, 24.9% v. 23, 11.2%; χ2 = 13.53; p ⩽ 0.001), and to have only family of origin in the country of arrival (101, 58.7% v. 48, 27.1%; χ2 = 37.44; p ⩽ 0.001). Cases also reported a higher mismatch between expectations and achievements compared with controls (Table 2). A single-point increase in both the post-migration social disadvantage index (range 0–3) and the mismatch between expectations and achievements (range 0–20) was associated with increased odds of psychosis in first-generation migrants in unadjusted (post-migration disadvantages OR 1.94, 95% CI 1.19–3.15, p = 0.008, Nagelkerke's R 2: 0.119; mismatch OR 1.61, 95% CI 1.38–1.87, p ⩽ 0.001, Nagelkerke's R 2: 0.185) and adjusted models (post-migration disadvantages ORA 2.06, 95% CI 1.13–3.73, p = 0.018, Nagelkerke's R 2: 0.437; ORB 1.89, 95% CI 1.02–3.51, p = 0.044, Nagelkerke's R 2: 0.485; mismatch ORA 1.81, 95% CI 1.07–1.29, p = 0.001, Nagelkerke's R 2: 0.419; ORB 1.14, 95% CI 1.03–1.26, p = 0.014, Nagelkerke's R 2: 0.485) (Table 3).
The cumulative effect of social disadvantages and adversities during all phases of the migration history
As reported in Table 4, we found a dose–response relationship between the number of disadvantages/adversities and odds of psychosis. Adjusted OR of FEP increased from 1.21 (95% CI 0.308–4.72, p = 0.788) for migrants reporting two adversities to 14.09 (95% CI 2.06–96.47, p = 0.007) for those reporting six or more social adversities. Nagelkerke's R 2 increased from 0.180 (crude) to 0.479 (adjusted).
Table 4. Dose–response effect of cumulative exposure to disadvantages/adversities
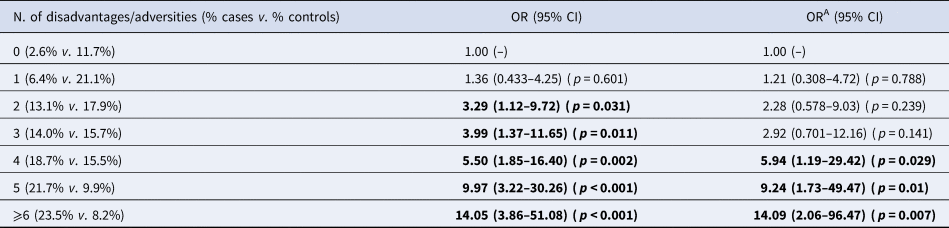
ORA = adjusted for site, age, gender, ethnicity, education, family history of psychosis, childhood trauma, cannabis use, fluency, years after migration, and achievements/expectations mismatch.
ORs in bold are significant (p < 0.05).
Discussion
Main findings
Our findings provide support for the hypothesis that social disadvantages and adversities during different phases of migration are associated with increased odds of psychosis in first-generation migrants, even when other risk factors are controlled for. Mutual adjustment for different phases suggested that social disadvantages during pre- and post-migration phases were associated with two times increased odds of psychosis. Moreover, our results support the hypothesis that the subjective evaluation of a mismatch between expectations and achievements is associated with increased odds of psychosis in first-generation migrants, even when adjusted for disadvantages and adversities and other exposures.
Pre-migration and post-migration social disadvantages seem to be more strongly associated with the odds of psychosis than adversities during the migration journey. Interestingly, length of stay in the country of arrival did not change the associations found between social disadvantages and psychosis odds. The cumulative effect of the migration social disadvantages and adversities further increased the odds of psychosis in migrants, suggesting a dose–response relationship in first-generation migrants (Stilo et al., Reference Stilo, Gayer-Anderson, Beards, Hubbard, Onyejiaka, Keraite and Morgan2017).
Strengths and limitations
Our study was based on a large, multi-centre, international sample, using population-based control samples. Controls were recruited with a mixture of random and quota-sampling strategy to maximize the representativeness of at-risk population in terms of age, sex and ethnicity [see Gayer-Anderson et al., Reference Gayer-Anderson, Jongsma, Di Forti, Quattrone, Velthorst, de Haan and Morgan2020 (Gayer-Anderson et al., Reference Gayer-Anderson, Jongsma, Di Forti, Quattrone, Velthorst, de Haan and Morgan2020) for details]. Participants included in the final logistic regression model were about 44.7% of the total sample.
To the best of our knowledge, our study is the first to investigate pre-migration exposures. Case–control studies are typically the most feasible for rare outcomes such as psychosis. The cross-sectional design limits any inferences about causality; however, the case–control study was nested in a population-based incidence study (Jongsma et al., Reference Jongsma, Gayer-Anderson, Lasalvia, Quattrone, Mulè and Szöke2018) and this is an effective approach for measuring exposures at psychosis onset. The novelty of our paper lies in trying to disaggregate the timing of exposures of pre-, during and post-migration disadvantages and adversities. While the cross-sectional retrospective design itself represents a significant limitation and this design is subject to recall bias, a stronger longitudinal prospective design to study pre-migration and migration exposures would be very difficult to perform, since participants would have to be followed while moving between different countries.
The total EU-GEI case–control comprised over 1000 cases and 1000 controls. A sample of this size has over 90% power to detect OR of 1.5 or greater at p < 0.05 when the prevalence of the exposure is 15% or greater. Migrants, though, represented only 22.7% of cases (256) and 14.6% of controls (219), resulting in a smaller sample. This may have led to the reduced power of detecting relevant associations.
Although many factors make up the picture of social disadvantages and adversities during the three different migratory phases, the characteristics we have chosen are those most investigated by previous studies and most representative of social disadvantage and migratory adversities (Agerbo et al., Reference Agerbo, Sullivan, Vilhjálmsson, Pedersen, Mors, Børglum and Mortensen2015; Anderson & Edwards, Reference Anderson and Edwards2020; Frissen et al., Reference Frissen, Lieverse, Marcelis, Drukker and Delespaul2015; Gayer-Anderson & Morgan, Reference Gayer-Anderson and Morgan2013; Hollander et al., Reference Hollander, Dal, Lewis, Magnusson, Kirkbride and Dalman2016; Huang et al., Reference Huang, Hou, Huang, He, Wang, Chen and Jia2019; Michalska Da Rocha et al., Reference Michalska Da Rocha, Rhodes, Vasilopoulou and Hutton2018; Tarricone et al., Reference Tarricone, Mimmi, Paparelli, Rossi, Mori, Panigada and Berardi2012; Van Os et al., Reference Van Os, Driessen, Gunther and Delespaul2000; Veling et al., Reference Veling, Hoek, Selten and Susser2011). Moreover, we operationalized the post-migration social disadvantages index considering the 5 years pre-psychosis onset (pre-study inclusion for controls). The 5-year period was conservatively chosen over simple observation at the onset, since when positive symptoms occur, functioning is often compromised already (Stilo et al., Reference Stilo, Di Forti, Mondelli, Falcone, Russo, O'Connor and Morgan2013).
In the final model, all the associations found were also adjusted for years after migration. The study's power to detect statistically significant associations could have been reduced by the multiple factors investigated; on the other hand, the statistically significant associations found are strengthened by this method.
The most investigated risk factor in the post-migration phase which showed cross-cultural consistency is ethnic density in the country of settlement: both in the UK and the Netherlands, minorities who live in areas with low ethnic density and are therefore exposed to conditions of low social capital and greater isolation have a higher risk of psychosis (Agerbo et al., Reference Agerbo, Sullivan, Vilhjálmsson, Pedersen, Mors, Børglum and Mortensen2015; Tarricone et al., Reference Tarricone, Mimmi, Paparelli, Rossi, Mori, Panigada and Berardi2012). We did not use a direct measure of ethnic density but investigated the migrants' relationships in the countries of arrival. We found that migrants relating only with the family of origin are at a higher risk of psychosis. Finally, other risk factors for psychosis, such as discrimination and racism, were not included in the present analysis and further studies should specifically evaluate the role of these exposures for psychosis onset in first-generation migrants.
Comparison with previous evidence
Several studies already support the hypothesis that a personal history of migration is associated with an increased likelihood of psychosis (Cantor-Graae & Pedersen, Reference Cantor-Graae and Pedersen2007), but, to the best of our knowledge, no previous studies have simultaneously evaluated the risk factors of the three migration phases. Findings indicating that refugees have a higher risk of developing psychosis compared to non-refugee migrants provide indirect evidence that the circumstances before and during migration matter (Brandt et al., Reference Brandt, Henssler, Müller, Wall, Gabel and Heinz2019; Hollander et al., Reference Hollander, Dal, Lewis, Magnusson, Kirkbride and Dalman2016). We evaluated the risk factors pre-, during and post-migration directly and provide preliminary evidence that social disadvantages across different migration phases, along with the subjective evaluation of a mismatch between achievements and expectations, may be important factors in the development of psychosis in migrants. These findings add to previous evidence from our study that greater social distance from the majority population negated some of the excess odds of psychosis in migrant and ethnic minority groups (Jongsma et al., Reference Jongsma, Gayer-Anderson, Tarricone, Velthorst, van der Ven, Quattrone and Kirkbride2020). The present study suggests that these forms of psychosocial disempowerment may impact on mismatches between achievements and expectations. Moreover, our results are consistent with those of a recent meta-analysis (Selten et al., Reference Selten, Van Der Ven and Termorshuizen2019) showing a small difference in risk between first- and second-generation migrants: this suggests that the role of the adversities during the migration phase is small compared with the impact of social disadvantages. Further longitudinal evidence will be required to replicate and confirm this possibility.
Consistently with previous evidence, all the factors analysed under the construct of social disadvantages and adversities were found more frequently in cases than in controls (Corcoran et al., Reference Corcoran, Walker, Huot, Mittal, Tessner, Kestler and Malaspina2003; Howes & Murray, Reference Howes and Murray2014; Morgan, Charalambides, Hutchinson, & Murray, Reference Morgan, Charalambides, Hutchinson and Murray2010; Stilo et al., Reference Stilo, Gayer-Anderson, Beards, Hubbard, Onyejiaka, Keraite and Morgan2017). Independent of migrant status, many studies have looked at the association between single indicators of social disadvantage and psychosis, while only a few studies have specifically evaluated cumulative effects and long-term associations (Agerbo, Byrne, Eaton, & Mortensen, Reference Agerbo, Byrne, Eaton and Mortensen2004; Morgan et al., Reference Morgan, Kirkbride, Hutchinson, Craig, Morgan, Dazzan and Fearon2008; Stilo et al., Reference Stilo, Di Forti, Mondelli, Falcone, Russo, O'Connor and Morgan2013, Reference Stilo, Gayer-Anderson, Beards, Hubbard, Onyejiaka, Keraite and Morgan2017). The AESOP study conducted in the UK (Cooper et al., Reference Cooper, Morgan, Byrne, Dazzan, Morgan, Hutchinson and Fearon2008; Morgan et al., Reference Morgan, Kirkbride, Hutchinson, Craig, Morgan, Dazzan and Fearon2008) pointed out that social disadvantage/adversities following migration were associated with a higher risk of FEP in ethnic minorities. Mismatch between expectations and achievements was also found to be associated with psychosis onset in ethnic minorities in the UK (Reininghaus et al., Reference Reininghaus, Morgan, Simpson, Dazzan, Morgan, Doody and Craig2008).
Relevance and implications
We found a higher burden of social disadvantage and adversities in all phases of the migration history in migrants who develop psychosis compared with those who do not, consistent with the socio-developmental pathway to psychosis proposed by Morgan et al. (Reference Morgan, Charalambides, Hutchinson and Murray2010). This result, along with the cumulative effect of the history of social disadvantages/adversities on the likelihood of psychosis, may indicate that the burden of socio-environmental risk factors during the migration history contributes to the high rates of psychosis in migrants.
Our findings seem to indicate that social disadvantages and stress during the entire migration history, more than adversities and trauma during the migration travel (e.g. migration phase), put migrants at higher risk of psychosis following a dose–response mechanism. This hypothesis is also consistent with those arising from studies showing that both striatal stress-induced dopamine release and dopamine synthesis capacity are elevated in migrants compared with non-migrants, independent of clinical status (Egerton et al., Reference Egerton, Howes, Houle, McKenzie, Valmaggia, Bagby and Mizrahi2017). This is in accordance with the social defeat hypothesis of psychosis, which posits that long-term experience of outsider status or inferior position leads to a sensitization of the mesolimbic dopamine system and thereby increases the risk for psychosis (Gevonden et al., Reference Gevonden, Booij, Van Den Brink, Heijtel, Van Os and Selten2014).
In conclusion, social vulnerability through the whole migration process and the negative post-migration experiences was associated with double the odds of psychosis in first-generation migrants. Social and public health strategies aiming to reduce the negative socio-environmental factors and increase psychological support in the post-migration phase are needed to more effectively address the social drivers of high rates of psychosis among migrants.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S003329172000495X.
Acknowledgements
The European Network of National Schizophrenia Networks Studying Gene-Environment Interactions (EU-GEI) Project was funded by grant agreement Health-F2-2010-241909 (Project EU-GEI) from the European Community's Seventh Framework programme. The Brazilian study was funded by grant 2012-0417-0 from the São Paulo Research Foundation. We deeply thank the whole EU-GEI WP2 GroupFootnote †
Author contribution
All the authors in the EU-GEI group collected or supervised the data collection. IT was responsible for the conception and design of the study. IT, GD, FS, CG-A, HEJ and ST cleaned and prepared the data for this paper analysis. IT, GD and FS did the data analysis and wrote the findings in the initial manuscript. GD and FS contributed to the creation of the figures and tables. CM, RMM, J-PS, DB, JBK, HEJ, CI, LdH and EvdV provided a careful statistical and methodological revision of the manuscript and contributed to the final draft. IT, RMM, CM, J-PS and DB contributed to the interpretation of the results. All authors had full access to all data (including statistical reports and tables) in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of interest
MDF reports personal fees from Janssen, outside the submitted work. RMM reports personal fees from Janssen, Lundbeck, Sunovion and Otsuka, outside of the submitted work. PML reports personal fees from Janssen, Lundbeck and Otsuka, outside of the submitted work. CA has been a consultant to or has received honoraria or grants from Acadia, Angelini, Gedeon Richter, Janssen Cilag, Lundbeck, Minerva, Otsuka, Roche, Sage, Servier, Shire, Schering Plough, Sumitomo Dainippon Pharma, Sunovion and Takeda. HEJ is supported by the Economic and Social Research Council (grant number ES/S011714/1). All authors declare no competing interests. JBK is supported by the National Institute for Health Research University College London Hospital Biomedical Research Centre.







