Childhood emotional abuse, characterized as rejecting, criticizing, threatening, humiliating, and berating caregiving (Behl et al., Reference Behl, Conyngham and May2003), has been linked to heavy and binge drinking as well as alcohol use disorders (AUD) in adulthood (Kisely et al., Reference Kisely, Mills, Strathearn and Najman2020; Murase et al., Reference Murase, Simons and Simons2021; Shin et al., Reference Shin, Lee, Jeon and Wills2015). Alcohol use disorders (AUD) is a common public health issue that places a considerable burden (over 5%) on the health and well-being of the general population around the globe, increasing the risk of non-communicable diseases, infectious diseases, mental health problems, injuries, and violence (World Health Organization, 2019). Numerous studies have shown a correlation between emotional abuse and AUD, and much evidence for the physiological, neurobiological, and epigenetic mechanisms underlying this relationship has been provided (see a review, Cicchetti & Handley, Reference Cicchetti and Handley2019). Although emerging studies have investigated the externalizing (e.g., conduct problems) and internalizing (e.g., personality profiles) psychological pathways (Handley et al., Reference Handley, Rogosch and Cicchetti2017; Shin et al., Reference Shin, Jiskrova and Wills2019), additional research is necessary for a further understanding of the psychological processes by which emotional abuse in childhood increase the risk for AUD. Borderline personality traits could be a reasonable guess for such mechanisms (Elliott et al., Reference Elliott, Stohl, Wall, Keyes, Skodol, Eaton, Shmulewitz, Goodwin, Grant and Hasin2016).
Although childhood emotional abuse is a phenomenon in almost all populations, there is a knowledge gap in cases from specific low- and middle-income countries. Nepal is one such country with a paucity of data on the adverse impact of childhood emotional abuse on AUD and borderline personality traits (Dhakal et al., Reference Dhakal, Niraula, Sharma, Sthapit, Bennett, Vaswani, Pandey, Kumari and Lau2019; Neupane et al., Reference Neupane, Bhandari, Thapa, Bhochhibhoya, Rijal and Pathak2018). There is mounting evidence that emotionally abused women have more substantial alcohol-related health issues than males (Cheng and Anthony, Reference Cheng and Anthony2018).
Hence, the primary objective of this study is to gather data on the relationship between childhood emotional abuse and AUD among Nepali women. A secondary aim is to explore the mediating role of borderline personality traits in this relationship.
Theoretical framework – a developmental psychopathology perspective
The developmental psychopathology framework holds considerable promise for helping us unravel the processes underlying the adverse outcomes. The socioemotional interactive setting of a child has both nurturing roles and protective functions, which are critical for successful adjustment. On the contrary, maladjusted development at a young age has a ripple effect on later development and adjustment (Cicchetti & Handley, Reference Cicchetti and Handley2019; Shin et al., Reference Shin, Lee, Jeon and Wills2015). The literature in the realm of developmental psychopathology suggests that exposure to childhood emotional abuse interferes with normative personality development and adult behavioral adaptation (Cicchetti & Toth, Reference Cicchetti and Toth1995; Cicchetti & Handley, Reference Cicchetti and Handley2019; Reich et al., Reference Reich, Vera, Marino, Levin, Yong and Frankenburg1997).
Specifically, many behavioral regulations and positive personality traits are difficult to develop for emotionally maltreated children who often live in adverse caretaking environments. Numerous studies have found that emotionally abused children were more prone to negative emotionality and showed more significant difficulties dealing with behavioral regulation in adulthood than non-abused children (Anda et al., Reference Anda, Felitti, Bremner, Walker, Whitfield, Perry, Dube and Giles2006; Cicchetti & Handley, Reference Cicchetti and Handley2019; Johnson et al., Reference Johnson, Cohen, Brown, Smailes and Bernstein1999).
One strategy to cope with emotional disruption and feelings of losing control is using alcohol to alleviate or suppress the suffering, called self-medication (Khantzian, Reference Khantzian1997). When self-medication is functional, alcohol consumption is negatively reinforced and may foster the later development of AUD.
Moreover, clinical researchers argued that emotional abuse experiences, such as denial, trivialization, or ridicule of the expression of private experiences, play an etiological role in borderline personality disorder (BPD; Linehan, 2018). Thus, across childhood and adulthood, emotional abuse poses an increased risk for various disturbances in socioemotional functioning and forms of psychopathology.
Childhood emotional abuse and alcohol use disorders
A few existing studies have shown that child emotional abuse increases an individual’s risk for AUD in adulthood (Edalati & Krank, Reference Edalati and Krank2016; Kisely et al., Reference Kisely, Mills, Strathearn and Najman2020; Murase et al., Reference Murase, Simons and Simons2021; Shin et al., Reference Shin, Lee, Jeon and Wills2015). For instance, in one retrospective study of 280 AUD patients and 137 healthy controls, a history of emotional abuse, compared with other child abuse types (e.g., physical and sexual abuse), was found to be the primary predictor of AUD, both directly and indirectly through the mediating effect of emotional impulsivity (Schwandt et al., Reference Schwandt, Heilig, Hommer, George and Ramchandani2013). Also, in the same study, exposure to emotional abuse in childhood was much more prevalent among AUD patients (47.5%) than in healthy controls (7.3%). Similarly, in a retrospective study of 268 nonclinical adults, Shin et al. (Reference Shin, Lee, Jeon and Wills2015) found that emotional abuse was related to alcohol use, binge drinking, alcohol-related problems, and AUD after controlling for demographics.
Child emotional abuse is associated with AUD in both men and women, but there is increasing evidence arguing that maltreated women tend to experience more significant alcohol-related health problems than men (Cheng & Anthony, Reference Cheng and Anthony2018; Guinle & Sinha, Reference Guinle and Sinha2020; McCaul et al., Reference McCaul, Roach, Hasin, Weisner, Chang and Sinha2019; Oberleitner et al., Reference Oberleitner, Smith, Weinberger, Mazure and McKee2015). While men tend to consume excessive alcohol to enhance exciting feelings, women are more likely to consume excessive alcohol in response to insufferable negative emotions and stress (McCaul et al., Reference McCaul, Roach, Hasin, Weisner, Chang and Sinha2019). Especially for emotionally abused women, a recent study has shown that girls who reported a history of emotional abuse before adulthood are more vulnerable to developing AUD (Cheng & Anthony, Reference Cheng and Anthony2018).
Childhood emotional abuse and alcohol use disorders among Nepali women
Evidence of childhood emotional abuse and AUD from low-income and middle-income countries remains limited. This gap in the literature is particularly noteworthy in the case of Nepal, as there are only a few studies on emotional abuse, and no study to date has comprehensively explored the relationships between emotional abuse and AUD.
Nepal, classified as a low-income country with a high poverty rate and limited resources, is considered a high-risk environment for child maltreatment (Neupane et al., Reference Neupane, Bhandari, Thapa, Bhochhibhoya, Rijal and Pathak2018). Despite the high prevalence of child maltreatment in Nepal (Emery et al., Reference Emery, Thapa, Do and Chan2015, Reference Emery, Abdullah, Thapa, Do, Jordan, Huang, Men and Wekerle2022; Kandel et al., Reference Kandel, Kunwar, Karki, Kandel and Lamichhane2017), only one study specifically assessed the form of childhood emotional abuse in Nepal. This cross-sectional study on a sample of 962 public secondary school students in Kathmandu, Nepal, revealed that emotional abuse was the most prevalent (previous year: 75.19%; throughout lifetime: 76.15%) form of child abuse (Neupane et al., Reference Neupane, Bhandari, Thapa, Bhochhibhoya, Rijal and Pathak2018). Across Nepal, findings of AUD vary widely. An earlier survey with random sampling in Dharan, Nepal, revealed that nearly 15% of female respondents were screened positive for AUD (two or more positive responses in the CAGE questionnaire; Jhingan et al., Reference Jhingan, Shyangwa, Sharma, Prasad and Khandelwal2003). In a recently community-based cross-sectional study in a central district of Nepal, 5.3% of women screened positive for AUD (Rathod et al., Reference Rathod, Luitel and Jordans2018).
Borderline personality traits as a mediator for the relationship between childhood emotional abuse and alcohol use disorders in adulthood
From the developmental psychopathology perspective, research examining psychological mechanisms underlying childhood emotional abuse and AUD point to maladaptive and risky alcohol personality traits as key contributing factors (Johnson et al., Reference Johnson, Cohen, Brown, Smailes and Bernstein1999; Murase et al., Reference Murase, Simons and Simons2021; Wilson et al., Reference Wilson, Robb, Gajwani and Minnis2021). Borderline personality is one of the risky alcohol personalities (Kaufman et al., Reference Kaufman, Perez, Lazarus, Stepp and Pedersen2020).
Impulsivity, negative emotionality, disturbed interpersonal relationships, and self-harm behaviors characterize borderline personality disorder (BPD). Recent international investigations estimated that BPD is prevalent in nonclinical populations (1%–3%; Herman et al., Reference Herman, Perry and Van der Kolk1989; Wilson et al., Reference Wilson, Robb, Gajwani and Minnis2021). Emerging studies consider BPD as variants of personality traits on a continuum from normality to pathology. When measured continuously rather than categorically (yes/no diagnosis), even a single BP trait can cause clinically significant impairment in functioning (Ellison et al., Reference Ellison, Rosenstein, Chelminski, Dalrymple and Zimmerman2016; Zimmerman et al., Reference Zimmerman, Chelminski, Young, Dalrymple and Martinez2013).
Emotional abuse experienced in childhood, compared with other types of maltreatment (e.g., sexual and physical abuse), is more conducive to vulnerability to BP traits, and the bulk of studies have shown an association between childhood emotional abuse and BP traits or features (Ibrahim et al., Reference Ibrahim, Cosgrave and Woolgar2018; Quenneville et al., Reference Quenneville, Kalogeropoulou, Küng, Hasler, Nicastro, Prada and Perroud2020). Previous studies have also found that emotionally abused children are more likely to present with some borderline personality traits than those who have not been emotionally abused (Belsky et al., Reference Belsky, Caspi, Arseneault, Bleidorn, Fonagy, Goodman, Houts and Moffitt2012; Gratz et al., Reference Gratz, Latzman, Tull, Reynolds and Lejuez2011; Kuo et al., Reference Kuo, Khoury, Metcalfe, Fitzpatrick and Goodwill2015; Rosenstein et al., Reference Rosenstein, Ellison, Walsh, Chelminski, Dalrymple and Zimmerman2018). For example, in Gratz et al. (Reference Gratz, Latzman, Tull, Reynolds and Lejuez2011)’s study, emotional abuse (as assessed with the Childhood Trauma Questionnaire, Bernstein et al., Reference Bernstein, Stein, Newcomb, Walker, Pogge, Ahluvalia, Stokes, Handelsman, Medrano and Desmond2003) was independently associated with borderline personality traits among adolescents. Likewise, in a retrospective study, the structural equation model suggested that childhood emotional abuse directly relates to BP traits (Rosenstein et al., Reference Rosenstein, Ellison, Walsh, Chelminski, Dalrymple and Zimmerman2018). The same study showed no significant correlation between child sexual abuse experience and BP traits. Child physical abuse experience only showed a weak association with BP traits.
In addition, BP traits predicted an increased risk for adult maladaptive behaviors, consistent with the impulsivity and poor coping strategies associated with borderline personality (Elliott et al., Reference Elliott, Stohl, Wall, Keyes, Skodol, Eaton, Shmulewitz, Goodwin, Grant and Hasin2016; Stepp et al., Reference Stepp, Trull and Sher2005). One particularly typical maladaptive behavior is AUD. An earlier 2-year longitudinal study on young adults in the United States found that BP traits significantly predicted AUD two years later after controlling for a family history of maladaptive behaviors (e.g., SUD, AUD) and their non-BPD counterparts (Stepp et al., Reference Stepp, Trull and Sher2005). Recent studies have indicated that of those individuals who met the diagnostic criteria for BPD, 46%–49% also met the diagnostic criteria for AUD, and 12%–17% of individuals with AUD met the criteria for BPD (Helle et al., Reference Helle, Watts, Trull and Sher2019; Kaufman et al., Reference Kaufman, Perez, Lazarus, Stepp and Pedersen2020; Trull et al., Reference Trull, Freeman, Vebares, Choate, Helle and Wycoff2018). Specifically, current rates of co-occurrence of BPD and AUD were elevated among clinical samples, with some studies recording up to 64% of adults experiencing both conditions (see a review: Trull et al., Reference Trull, Freeman, Vebares, Choate, Helle and Wycoff2018). However, research on BP traits or the prevalence of BPD in Nepal is lacking.
In sum, what is clear from the research reviewed above is that BP traits might appear related to childhood emotional abuse experience and AUD in adulthood. What remains unclear is whether BP traits mediate between childhood emotional abuse and later AUD. Until now, few studies have directly examined the mediating role of BP traits in the relationships between childhood emotional abuse and AUD, except for one recently conducted by Elliott and her colleagues. This was a three-year longitudinal study on a nationally representative sample of the United States, and it was found that borderline personality disorder symptoms, as mediators, explained the association between childhood maltreatment and persistent AUD (Elliott et al., Reference Elliott, Stohl, Wall, Keyes, Skodol, Eaton, Shmulewitz, Goodwin, Grant and Hasin2016). However, since they conducted the study with a clinical sample, it remains unknown whether their findings could be generated for the nonclinical population. A sample with a broader range of experiences may provide a more complete picture of these associations. Also, they did not specify the type of child maltreatment in the study. Thus, researchers are still unclear about the relationships among childhood emotional abuse, BP traits, and AUD in a nonclinical population. More evidence is needed.
Present study
Our goal was to determine whether borderline personality traits mediate the relationship between childhood emotional abuse and AUD using a large and nationally representative data set among Nepali women. Based on previous research and extant theoretical literature, we hypothesized that (H1) childhood emotional abuse would be associated with BP traits and AUD among Nepali women. Further, consistent with a developmental psychopathology framework, we hypothesized that (H2) borderline personality traits would mediate the relationship between childhood emotional abuse and AUD among Nepali women.
Method
Participants
The study used a women sample from a national cross-sectional project, with the original sample consisting of 1,100 Nepali mother-child dyads recruited in 2021. Adult women participants’ inclusion criteria included 18 years or above, being a mother with a child aged 13–15, and providing informed consent. Urban and rural populations stratified the sample to reflect the reality that 83% of the population lives in rural districts. Using the probability proportional to size sampling method, we selected 27 municipalities. Data were collected during in-person door-to-door interviews by trained and certified interviewers. Each mother in this study received 40 HKD as compensation for their time. Interviewers employed refusal conversion techniques to minimize the non-response rate. For the residents who were not home, the interviewer used multiple contacts to rearrange the interview, such as leaving a letter informing the resident of the study and returning at another time. For the residents who initially said “no” to agreeing to participate, the interviewers tried to help the residents understand the study’s value or assigned this case to a different interviewer. To secure participants’ privacy, we assigned each participant a data identifier and stored the contact information in a separate, secure file with the only identifier.
Measures
The measures were first translated from English into Nepali by a Nepali-English bilingual team member, then back-translated into English by another bilingual research team member. In order to make sure that the meaning of the questionnaire in Nepali accurately captured the concepts provided in English, the research team members held an informal focus group with the data collection team.
Alcohol Use Disorders (AUD). Alcohol use disorder (AUD) is officially diagnosed based on the criteria set by the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (APA, 2013). The term alcohol abuse/dependence has been substituted with AUD. Alternatively, a short form of screening test, such as the CAGE (Cutting down, Annoyance by criticism, Guilty feeling, and Eye-openers) (Ewing, Reference Ewing1984), is more convenient and specific than systematic diagnosis tests to identify risk for AUD among nonclinical samples. In current study, participants completed the Cut Down, Annoyed, Guilty, and Eye-opener (CAGE) questionnaire, a 4-item screener for AUD (Ewing, Reference Ewing1984). Item responses on the CAGE questions are scored 0 for “no” and 1 for “yes” answers, with a higher score indicating alcohol use problems. For the present study, items were summed to create a total score (with possible scores ranging from 0 to 4). The more items endorsed, the more severe the risk for AUD. In the current study, two or greater is considered high risk for AUD. Hence, the original total CAGE scores were recoded to create a “risk for AUD” 0-1 dummy variable indicator (1 = AUD; 0 = no AUD). Internal consistency in this sample was good (α = .84).
Childhood Emotional Abuse. Participants completed the emotional abuse subscale of CTQ (Bernstein et al., Reference Bernstein, Stein, Newcomb, Walker, Pogge, Ahluvalia, Stokes, Handelsman, Medrano and Desmond2003), a 5-item self-report measure of childhood emotional abuse. In the measure, childhood emotional abuse is defined as “verbal assaults on a child’s sense of worth or well-being or any humiliating or demeaning behavior directed toward a child by an adult” (Bernstein et al., Reference Bernstein, Stein, Newcomb, Walker, Pogge, Ahluvalia, Stokes, Handelsman, Medrano and Desmond2003). Each item is rated on a five-point Likert scale, with higher scores indicating a stronger agreement with the statement (never true = 1, rarely true = 2, sometimes true = 3, often true = 4, very often true = 5). In the current study, items were added together to calculate a total childhood emotional abuse score (with possible scores ranging from 5 to 25). Participants with a score of at least 16 were identified to have experienced severe emotional abuse. A participant scoring five was considered not to have been emotionally abused. This sample’s internal consistency for childhood emotional abuse was good (α = .82).
Borderline Personality Traits. Participants completed the Mclean Screening Instrument for Borderline Personality Disorder (MSI-BPD; Zanarini, Reference Zanarini2003), a 10-item self-report inventory based on DSM-5 criteria for BPD. A recent meta-analysis of 11 studies found that the MSI-BPD has an overall sensitivity of 80% and a specificity of 66% at a cutoff point 7 (Zimmerman & Balling, Reference Zimmerman and Balling2021). Items are answered with either “yes” or “no.” Example items are “Have you felt chronically empty?” and “Have you frequently felt unreal or as if things around you were unreal?” Since it was the first study to utilize McLean Screening Instrument to examine borderline personality traits in Nepal, we ran a polychoric correlation matrix to test its’ factor quality. Exploratory factor analysis indicated one component that explained 81.0% of the variance, suggesting the unidimensionality of the MSI-BPD. The Kuder-Richarson Coefficient of Reliability in this sample was good (α = .81). For the present study, items were summed to create a total score (with possible scores ranging from 0 to 10). In addition, we also reported the prevalence of borderline personality disorders (BPD) by recoding the raw data into a dichotomous variable, where a total score of 7 or above was considered the cutting-off threshold.
Control variables
There are risk factors associated with AUD, specifically for Nepali women, including a divorce status and aged 50-year-old and above (Niraula et al., Reference Niraula, Shyangwa, Jha, Paudel and Pokharel2004). On the other hand, higher economic status, stability of residence, employment status, and education were known as protective factors against experiencing child maltreatment (Atteraya et al., Reference Atteraya, Ebrahim and Gnawali2018) and developing AUD in Nepali women (Jhingan et al., Reference Jhingan, Shyangwa, Sharma, Prasad and Khandelwal2003; Rathod et al., Reference Rathod, Luitel and Jordans2018; Thapa et al., Reference Thapa, Aryal, Puri, Shrestha, Shrestha, Thapa, Mehata, Thapa, Banjara and Stray-Pedersen2016). As a negative home experience in adulthood, experiencing husband’s domestic violence has been associated with Nepali women’s drinking problem (Manandhar et al., Reference Manandhar, Shrestha and Joshi2017). Additionally, 83% of Nepal’s population lives in rural districts (Central Bureau of Statistics, Nepal (CBS, N), 2014). Therefore, we utilized the husband’s domestic violence, participants’ age, rural or urban residence, years of residence, marital status, participants and their partner’s annual income, participants and their partner’s education level, and participants and their partner’s employment status in the current study.
Husband’s Domestic Violence. Participants reported physical violence from their husband on seven items from the Short Form of the Revised Conflict Tactics Scales (CTS2S), including being (a) slapped; (b) hit with something; (c) punched or kicked or bit; (d) pushed, grabbed, or shoved; (e) beat-up and (f) choked by their husband, and (g) their husband used or threatened to use a knife or gun on them (Straus & Douglas, Reference Straus and Douglas2004). In the current research, we also asked the participants to report the frequency of domestic violence from their husband in the past year. Possible responses were “never = 0”, “once = 1”, “twice = 2”, “3-5 times = 3”, “6-10 times = 4”, “11-20 times = 5”, “more than 20 times = 6”, “not in the past year, but it did happen before = 7”, and “this has never happened = 8”. The husband’s domestic violence is scored by summing the midpoints for the response category chosen by the participant. The midpoints correspond to the answer category numbers for 0, 1, and 2. The midpoint of Category 3 is 4; for Category 4, it is 8; for Category 5, it is 15; for Category 6, we recode it as 25; for Category 7 and 8, it is 0. In addition, we also reported the prevalence of domestic violence by recoding the raw data into a dichotomous variable, coding it as one when there was at least one domestic violence incident from the husband in the past year and zero when there was no domestic violence.
Analytic strategies
Analyses were performed using STATA software version 16 (StataCorp, Reference StataCorp2015). The analyses began with presenting the descriptive statistics for all variables included in the study. Then, we used random effects logistic/linear regressions to include a random cluster effect that estimates the influence of the cluster (municipalities) on the outcomes. First, we ran a logistic regression model without the mediator to test H1, i.e., the association between childhood emotional abuse on AUD. Second, we ran a logistic regression with the mediator to test H2, i.e., the mediating effect of BP traits in the relationship between childhood emotional abuse and AUD. Finally, to test the direct and indirect effects, we used Karlson-Holm-Breen (KHB) method (Karlson et al., Reference Karlson, Holm and Breen2012). The direct effect refers to the impact of emotional abuse on AUD, whereas the indirect effect indicates the influence of AUD through the development of BP traits. We implemented the method newly developed by Karlson, Holm, and Breen (KHB) to decompose the overall effect of emotional abuse on AUD into direct and indirect effects (Karlson et al., Reference Karlson, Holm and Breen2012). KHB method permits a mediation effect to be analyzed in a nonlinear model (e.g., random effects logistic regression), which is appropriate for us to analyze the binary outcome. The bootstrapping mediation method is used to check the robustness of the mediation effect, with 95% bias-corrected confidence intervals (CIs, 5000 replications). In the bootstrapping test, a significant indirect effect occurs when confidence intervals do not include zero (Hayes, Reference Hayes2009).
Results
The descriptive statistics for all variables in the analyses are presented in Table 1. Additionally, Table 1 suggests that 8.63% of the sample reported severe emotional abuse during childhood, and 60.63% reported no emotional abuse experience during childhood. About one in ten (10.09%), indicated by a CAGE score of 2 or more, was reported to have a risk for AUD. The rate of BPD, indicated by the screening tool MSI-BPD score of 7 or more, was 5.91%.
Table 1. Descriptive statistics of all variables
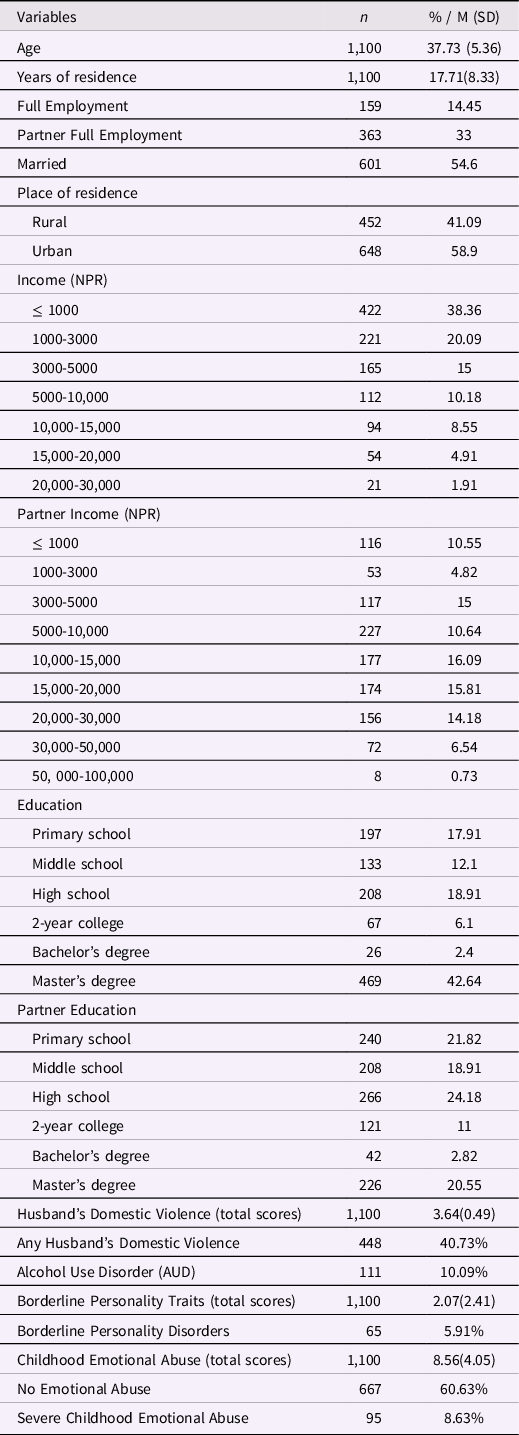
N = 1,100.
Regression analysis results are shown in Table 2 and Table 3. In Table 2, the results of the basic logistic regression model (without a mediator) revealed that child emotional abuse was significantly associated with a higher risk of AUD (B = 0.09, p = 0.041, OR = 2.04, 95% CI [0.004, 0.17]), controlling for husband’s domestic violence and other demographic variables. The results of the mediation model (with mediator BP traits) revealed that childhood emotional abuse was not significantly associated with AUD (B = 0.03, p = 0.099, OR = 0.62, 95% CI [−0.06, 0.12]), controlling for BP traits, husband’s domestic violence and demographic variables. BP traits were significantly associated with AUD in the expected directions (B = .34, p < 0.001, OR = 4.78, 95% CI [0.20, 0.47]). Table 3 shows that emotional abuse was significantly associated with BP traits (B = 0.12, p = 0.004, 95% CI [0.08, 0.16]), controlling for demographic variables and husband’s domestic violence.
Table 2. Random effects logistic regression (dependent variable: alcohol use disorders; cluster: municipalities)
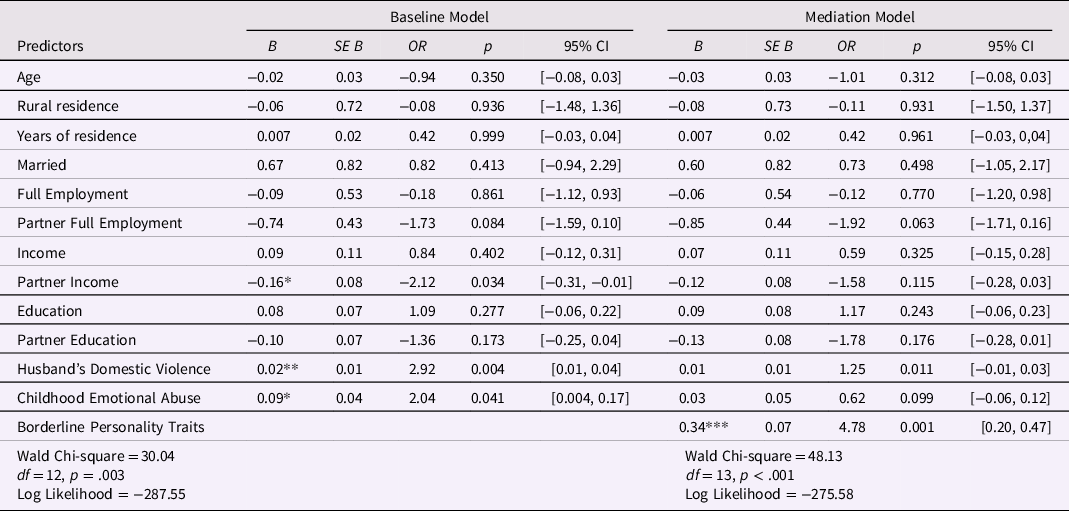
CI = confidence interval; OR = odds ratio.
***p<0.001.
**p<0.01.
*p<0.05.
Table 3. Random effects linear regression (dependent variable: borderline personality traits; cluster: municipalities)
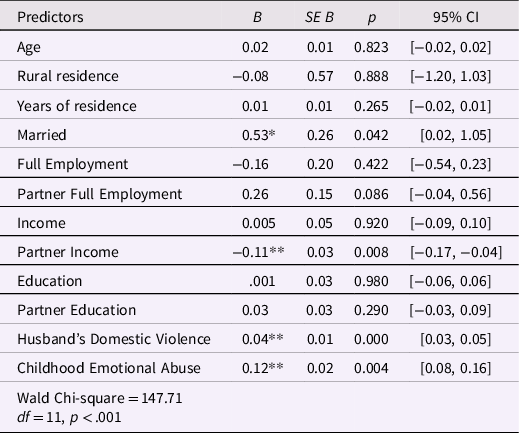
CI = confidence interval; OR = odds ratio.
***p<0.001.
**p<0.01.
*p<0.05.
The mediation effects using the bootstrapping and KHB method are presented in Table 4. The KHB with bootstrapping results indicated that the direct effect of childhood emotional abuse on AUD during adulthood (direct effect: B = 0.04, p = .400, 95% CI [−0.05, 0.13]) was not significant when borderline personality traits were included as a mediator in the model. Furthermore, the analyses revealed, with 95% confidence, that the indirect effect (i.e., the difference between the total and direct effects) of emotional abuse on AUD through borderline personality disorder was significant (B = .07, p = .001, 95% CI [0.05, 0.10]).
Table 4. Mediation effects (KHB method)
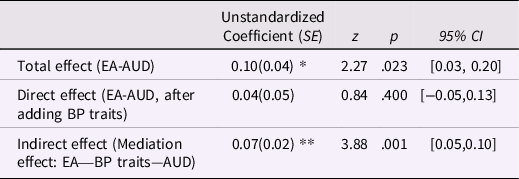
95%CI = 95% bias-corrected bootstrapping confidence interval; AUD = alcohol use disorders; BP traits = borderline personality traits; EA = Childhood Emotional Abuse; KHB = The Karlson-Holm-Breen method.
***p<0.001.
**p<0.01.
*p<0.05.
Discussion
Despite the growing literature on the effects of childhood emotional abuse on AUD in adulthood, no studies have examined this association in Nepal. Also, whether this relationship in Nepali women could be attributed to BP traits has been uncertain. The current study examined the mediating role of BP traits in this association between childhood emotional abuse and AUD among Nepali women.
Our primary findings were consistent with our hypotheses that Nepali women’s emotional abuse experience in childhood is associated with AUD and BP traits. A significant indirect effect of childhood emotional abuse exposure on AUD via BP traits was found, controlling for demographic information and the husband’s domestic violence. The findings reveal that particular essential signs of these BP traits may hinder AUD remission among Nepali women who were emotionally abused in childhood.
Prevalence of alcohol use disorders, BPD, and emotional abuse
Using the child traumatic questionnaire (CTQ) to measure retrospective self-report childhood emotional abuse, 60.63% of the sample reported no emotional abuse, and 8.63% reported severe emotional abuse. The 8.63% means that nearly one out of every eleven Nepali women has experienced severe emotional abuse. This finding, aligned with previous findings in Neupane et al. (Reference Neupane, Bhandari, Thapa, Bhochhibhoya, Rijal and Pathak2018)’s study, revealed that emotional abuse significantly burdens Nepal. Nevertheless, the retrospective self-report of emotional abuse is likely to be a conservative estimate of emotional abuse as it is much lower than Neupane et al. (Reference Neupane, Bhandari, Thapa, Bhochhibhoya, Rijal and Pathak2018) finding of a 76.15% emotional abuse prevalence. Differences in prevalence may be due to random sampling, utilizing the CTQ versus Neupane et al. (Reference Neupane, Bhandari, Thapa, Bhochhibhoya, Rijal and Pathak2018) use of the International Society for Prevention of Child Abuse and Neglect measure.
Of the national Nepal women sample, 10.09% reported two or more positive responses of CAGE, which were considered AUD. The prevalence figure in the current study appears lower than the 15.7% of female participants reported in a random sampling study in Dharan, situated in eastern Nepal (Jhingan et al., Reference Jhingan, Shyangwa, Sharma, Prasad and Khandelwal2003). This study also used CAGE as the measurement for AUD detection. The prevalence of AUD among the national Nepal women sample in the current research offers a complete picture of the population-level epidemiologic features of female alcohol use in Nepal.
In the current sample, 5.91% were likely to meet the criteria for BPD. This high prevalence rate reinforces the perspective that BPD is a significant public health problem and requires more attention as a prevention and treatment target. As indicated by the MSI-BPD measure in current research, the prevalence is higher than most previously published studies looking at personality disorders in the general population (range 1%–3%) (e.g., Trull et al., Reference Trull, Freeman, Vebares, Choate, Helle and Wycoff2018; Wilson et al., Reference Wilson, Robb, Gajwani and Minnis2021). Differences in prevalence may be due to the measures utilizing the self-report MSI-BPD versus Structured Clinical Interview for DSM-5 (Trull et al., Reference Trull, Freeman, Vebares, Choate, Helle and Wycoff2018). Although it is globally used as an effective screening test, MSI-BPD’s response setting remains susceptible to fixed dichotomous choices.
The current research also found that 40.7% of Nepali women reported having experienced IPV in the past. IPV victimization is well-recognized as public health and human rights problem. The high prevalence of IPV raises serious short- and long-term public health concerns, ranging from direct physical trauma, depression, and even suicide attempts and behaviors (Collison & Lynam, Reference Collison and Lynam2021). It is worth noting that our results revealed that IPV victimization was significantly associated with BP traits and AUD, which aligned with previous empirical findings (Collison & Lynam, Reference Collison and Lynam2021; Ogden et al., Reference Ogden, Dichter and Bazzi2022). These findings suggest that IPV victimization could be a risk factor for AUD and that women may drink more alcohol to cope with their traumatic experiences of IPV. The findings also indicate that women with higher BP traits may choose partners prone to violence---an essential question that warrants further exploration. Therefore, given its pervasive public health concerns and high prevalence among Nepali women, it is crucial for future studies to assess the role of IPV in the association between BP traits and AUD.
Emotional abuse and alcohol use disorders
The present study found that childhood emotional abuse was significantly related to AUD in Nepali women, which was consistent with previous studies conducted in other countries (e.g., Australia, United States; Edalati & Krank, Reference Edalati and Krank2016; Kisely et al., Reference Kisely, Mills, Strathearn and Najman2020; Mills et al., Reference Mills, Alati, Strathearn and Najman2014; Shin et al., Reference Shin, Lee, Jeon and Wills2015). Previous research on the effects of child abuse focused more on physical and sexual abuse rather than emotional abuse, presumably because physical and sexual maltreatment are thought to be more prevalent, detrimental to mental health, and more salient to the victim (Shin et al., Reference Shin, Lee, Jeon and Wills2015). The effects of emotional abuse have been less studied, probably because emotional abuse, at first glance, cannot be considered a crime. Emerging studies, however, showed that compared with adults who experienced other forms of maltreatment (e.g., sexual abuse, physical abuse, neglect) during childhood, adult participants who had experienced childhood emotional abuse were significantly more likely to report high risk for AUD (Edalati & Krank, Reference Edalati and Krank2016; Kisely et al., Reference Kisely, Mills, Strathearn and Najman2020; Mills et al., Reference Mills, Alati, Strathearn and Najman2014; Shin et al., Reference Shin, Lee, Jeon and Wills2015). Our findings and these previous findings mirror the growing prospective evidence of the long-standing harm of childhood emotional abuse. One possible explanation of the association between emotional abuse and AUD would be the limited parental support and the insecure parent-child relationship that emotionally abused children experienced, which has been linked with later poor emotional regulation and socioemotional functioning. The consistent experience of unstable mood coupled with increased negative experiences in interpersonal relationships may be a driving force behind heavy alcohol consumption and, thus, lead to a higher risk for AUD.
Borderline personality traits as a mediator in the relationship between emotional abuse and alcohol use disorders
In the present study, Nepali women with a history of childhood emotional abuse were more likely to be detected as having BP traits. The findings were consistent with previously established models of BP traits development, emphasizing the impact of a disrupted social-rearing environment on a child’s later social functioning. Emotional abuse experience might cause gradual damage to positive beliefs about the self and develop maladaptive models of self, others, and self-in-relation to others (Cicchetti & Handley, Reference Cicchetti and Handley2019; Quenneville et al., Reference Quenneville, Kalogeropoulou, Küng, Hasler, Nicastro, Prada and Perroud2020). Previous studies also highlighted the similarities of particular symptoms or features in individuals who have been emotionally maltreated and in adults with BPD. These symptoms include affective instability, identity problems, poor interpersonal relationship, and self-harm behaviors (see a systematic review: Ibrahim et al., Reference Ibrahim, Cosgrave and Woolgar2018).
Most importantly, we found that BP traits mediated the relationship between emotional abuse and AUD in Nepali women. There is growing evidence that emotionally abused individuals may be prone to AUD partly because they are unlikely to deal with their intense emotional impulsivity and interpersonal stress, which are the core BP traits. One possible explanation is that through a negative self-medication process (Khantzian, Reference Khantzian1997), the misuse of alcohol may be one of the leading motivations for regulating their frequently aroused emotional impulsivity and relieving interpersonal tension, one of the borderline personality features. In addition, according to the common cause model (Bornovalova et al., Reference Bornovalova, Verhulst, Webber, McGue, Iacono and Hicks2018), emotional impulsivity and affective dysregulation among emotionally abused women may be the shared etiological features that contribute to developing both BP traits and AUD symptoms. Hence, future researchers could further examine the underlying common traits like emotional dysregulation, impulsivity, and interpersonal stress in the mechanism, which can guide research in assessing shared etiology, treatment, and clinical course.
Strengths and limitations
The strengths of the current study are the sizeable national sample size and participant selection through simple random sampling. Also, we utilized internationally validated tools to assess emotional abuse, AUD, and BP traits, which allows future researchers to compare the findings of similar studies.
Our study findings need to be considered with their limitations. One limitation would be that the data are self-reported, cross-sectional, and non-experimental, precluding us from reflecting rigid and causal relationships. Second, our sample only included women who are mothers, which precludes the generalization of our findings to all Nepali women. Third, our mediation model does not exhaustively analyze the association between childhood emotional abuse and AUD. The direct path could be mediated by other psychological factors, such as other personality disorders (e.g., antisocial PD, dependent PD) (Elliott et al., Reference Elliott, Stohl, Wall, Keyes, Skodol, Eaton, Shmulewitz, Goodwin, Grant and Hasin2016) and other non-personality disorders (e.g., depression, anxiety, and stress) (Cicchetti & Handley, Reference Cicchetti and Handley2019). Fourth, we used screening instruments to evaluate BP traits and AUD. Previous studies consistently found that multidimensional diagnosis of BPD and AUD is more sensitive and valid (Fazzino et al., Reference Fazzino, Rose, Burt and Helzer2014; Zimmerman & Balling, Reference Zimmerman and Balling2021). Measuring BPD dimensionally (e.g., negative emotionality, impulsivity, and antagonism) may be especially reliable in nonclinical populations (Zimmerman et al., Reference Zimmerman, Chelminski, Young, Dalrymple and Martinez2013). We recommend that future diagnosis requires additional evaluations such as formal interviews based on DSM-5 criteria and multidimensional rather than categorical approaches. Moreover, given that different forms of childhood abuse are associated with AUD and BP traits (Cicchetti & Handley, Reference Cicchetti and Handley2019), future research should delineate which facets of childhood abuse are unique to AUD and BP traits and which are shared factors across psychopathologies.
Implications
The contribution of the current research is that, to our knowledge, it is the first study to examine the mediating role of BP traits in the relationship between childhood emotional abuse and AUD among women in Nepal. The findings suggest that the consequences of AUD and borderline personality traits should be included in Nepal’s estimated societal burden of childhood emotional abuse. In addition, a focus on borderline personality therapeutic intervention (e.g., dialectical behavior therapy, dual-focused schema therapy) may be helpful in efforts to prevent drinking problems among women who experienced childhood emotional abuse in Nepal. Given that treatments for borderline personality disorders among adults are usually costly, providing earlier prevention services for emotionally abused children can be considered a more practical next step for Nepal. The roles of parents are critical for optimal personality development. Psychoeducation-oriented intervention for parents and caregivers about emotional abuse and its adverse outcomes is necessary to reduce the prevalence of emotional abuse. These early interventions for children and parents in Nepal may reduce the likelihood of emotionally abused children developing severe and enduring mental and physical health problems during adulthood.
Funding statement
This study was funded by the General Research Fund, Research Grants Council, Hong Kong Government (Reference No. GRF17615120).
Competing interests
None.







