Introduction
Type 2 diabetes is a major cause of morbidity and mortality in the United States and worldwide, affecting nearly 1 in 11 adults. Reference Zheng, Ley and Hu1 Although genetic predisposition partly determines individual susceptibility to type 2 diabetes, lifestyle factors, such as BMI and physical inactivity, are important drivers of the development of type 2 diabetes. Reference Zheng, Ley and Hu1,Reference Said, Verweij and van der Harst2 However, the effect of early life exposures, such as being born preterm, on the development of type 2 diabetes has been less well studied.
Preterm birth (delivery at <37 completed weeks of gestation) has increased in prevalence across the globe, currently affecting nearly 15 million births (10.6%) annually. Reference Chawanpaiboon, Vogel and Moller3 Because of dramatic improvement in treatment advances in recent decades, over 95% of all preterm infants who receive modern neonatal and pediatric care now survive into adulthood. Reference Raju, Pemberton and Saigal4 To best counsel these patients and guide their medical care across the life course, a comprehensive understanding of long-term health risks is necessary. Reference Crump5
The Developmental Origins of Health and Disease hypothesis, or “Barker hypothesis,” postulates that adverse in utero exposures and nutrition in early life increases the risk of certain diseases later in life. Reference Barker6 The hypothesis is supported by multiple studies showing an increased risk of chronic conditions, such as cardiovascular disease, cancer, autoimmune diseases, thyroid conditions, disability, and type 2 diabetes, among individuals with a history of low birth weight. Reference Monahan, Farland and Shadyab7-Reference Song, Huang and Song12 There is evidence that adverse in utero exposures and/or malnutrition during gestation may influence epigenetic changes and/or the development of the pancreas and metabolic processes, predisposing one to develop type 2 diabetes in adulthood. Reference Kadayifci, Haggard and Jeon13-Reference Reusens, Theys, Dumortier, Goosse and Remacle15 Epidemiologic studies have also shown fairly consistent associations between an individual’s gestational age at birth and risk for type 1 diabetes, even after adjusting for birthweight. Reference Cardwell, Carson and Patterson16-Reference Khashan, Kenny and Lundholm19 Fewer studies have considered associations between an individual’s gestational age at delivery and adult-onset type 2 diabetes, and nearly all of these studies have been conducted in Nordic or East Asian countries, Reference Crump, Sundquist and Sundquist20-Reference Yoshida-Montezuma, Stone and Iftikhar28 and the majority are registry-based, Reference Crump, Sundquist and Sundquist20-Reference Kajantie, Osmond, Barker and Eriksson24 limiting potential covariate information. The association between being born preterm and risk of type 2 diabetes may be diminished or strengthened in other race or ethnic groups, limiting the external validity of the prior studies.
Thus, in the current study, we sought to investigate the potential association between a personal history of being born preterm and risk for type 2 diabetes in a racially and ethnically diverse population. To evaluate the association, we used data from the Women’s Health Initiative (WHI), a large, cohort of postmenopausal women in the United States with extensive phenotypic information. We hypothesized that being born preterm would be associated with a higher likelihood of type 2 diabetes.
Methods
Study population
The Women’s Health Initiative (WHI) is a prospective cohort study of major causes of disease and disability in older women that recruited postmenopausal women aged 50–79 from 1993 to 1998 into either one or more of three clinical trials (WHI-CT; n = 67,932) or an observational study (WHI-OS; n = 93,676); the present study only included women enrolled in the WHI-OS. Details on the WHI’s study design, recruitment, and implementation have been described elsewhere. Reference Anderson, Manson and Wallace29,Reference Prentice and Anderson30 All study protocols were approved by the Institutional Review Board of each participating clinical center, and all participants provided written informed consent at study initiation. Participant selection for this study is described below and in Supplementary Figure 1.
Baseline measures
When women enrolled into the WHI-OS, they completed structured, self-administered questionnaires that aimed to collect information on demographics, medical history, reproductive history, family history, personal habits such as drinking and smoking, diet, physical activity, and psychosocial factors. Women were asked to report if they were born “four or more weeks premature”; we consider women who responded "yes" to this question to be born preterm. They were also asked to report if they were born as a twin or triplet, and they reported their birth weight as one of the following categories: less than 6 pounds (lbs.), 6 lbs. to 7 lbs. 15 ounces (oz), 8 lbs. to 9 lbs. 15 oz, or 10 or more lbs. While the accuracy of self-report of one’s exact birthweight is poor, Reference Allen, Ellison, dos Santos Silva, De Stavola and Fentiman31,Reference Andersson, Niklasson and Lapidus32 the collection of birth weight by category has previously been validated (Spearman r = 0.75). Reference Troy, Michels and Hunter33 A physical assessment was performed at baseline by trained study staff to collect physical measurements, such as height, weight, and blood pressure, using standardized protocols for assessments. Participants were also asked to bring their medications with them to the in-person assessment to be recorded by the trained study staff.
Outcome definitions and measurement
Data on prevalent diabetes status were obtained at baseline through self-reported questionnaires. Women were asked to report if “a doctor had ever told them they had sugar diabetes or high blood sugar when they were not pregnant” (yes/no), their age when they were first told they had sugar diabetes by category (<21, 21–29, 30–39, 40–49, 50–59, 60–69, or 70 or older), and if they ever took insulin shots or oral diabetes medications (yes/no). To limit the diabetes cases to only those with type 2 diabetes, we used the following criteria: 1) self-reported physician diagnosis of "sugar diabetes or high blood sugar when they were not pregnant"; 2) ≥30 years of age at first diagnosis; and 3) self-reported using insulin or oral diabetes medication as a treatment for their diabetes. While it is possible that women with type 1 diabetes could still be included in our analyses, this definition has been validated in WHI and is consistent with medication inventories and fasting glucose measurements with a concordance of 77%. Reference Li, Liu and Li14,Reference Margolis, Lihong and Brzyski34 Incident cases of type 2 diabetes were reported by participants annually through in-person, mailed, and/or telephone questionnaires. Women were considered as an incident case of type 2 diabetes if they reported receiving type 2 diabetes treatment (either insulin shots, oral diabetes medication, or both) for the first time during the follow-up period.
Exclusion criteria
For our analyses, women were excluded if they reported being a twin or triplet (n = 1418), were <30 years of age at the time of their diabetes diagnosis (n = 215), or reported being hospitalized for a diabetic coma (n = 72). In analyses stratified by birth weight, race, or ethnicity, women were excluded if they were missing data on their birth weight, race, or ethnicity, respectively (Supplementary Figure 1).
Statistical analyses
Descriptive statistics for participants included in the analyses were generated using t-tests for continuous variables and chi-square tests for categorical variables. Because of the heterogeneity in data collection between the prevalent cases of type 2 diabetes reported at baseline and the incident cases of type 2 diabetes reported during the study period, including the case definition of type 2 diabetes, we performed statistical analyses separately for prevalent and incident type 2 diabetes. Multivariable logistic regression models estimated odds ratios (OR) and 95% confidence intervals (95% CI) for the association between being born preterm and prevalent type 2 diabetes with and without adjustments for demographic and lifestyle factors. Cox proportional hazards regression models were used to estimate hazard ratios (HR) and 95% CI between being born preterm and incident cases of type 2 diabetes that occurred during the follow-up period with and without adjustments for demographic and lifestyle factors. Person time was accumulated from the date at study entry until the date of the follow-up survey on which the type 2 diabetes was first reported or the date the last follow-up survey was completed, whichever came first. Due to the heterogeneity in type 2 diabetes case definition and ascertainment at baseline and follow-up, we excluded individuals with existing type 2 diabetes at enrollment in analyses examining incident type 2 diabetes. In all regression models, we used “full term birth” as the referent category. Controversy in the field of life course epidemiology remains unclear as to whether or not adjustment for adult lifestyle factors, such as BMI, in statistical models is appropriate; as such, we present results unadjusted, partially adjusted, and fully adjusted for demographic and lifestyle factors. Covariates selected for inclusion in our models are well-known risk factors for type 2 diabetes and include baseline measures for age, normalized neighborhood socioeconomic status (NSES), Reference Griffin, Eibner and Bird35 geographic region, educational level, race, ethnicity, family history of diabetes, BMI at baseline enrollment (kg/m2), smoking status, and alcohol use.
Because of the prior association between birth weight and type 2 diabetes, Reference Song, Huang and Song12,Reference Ryckman, Rillamas-Sun and Spracklen36 we also present models with and without adjustment for birth weight category. However, because birth weight and gestational age (including preterm birth) are strongly correlated, adjustment for birth weight category can attenuate the association between preterm birth and type 2 diabetes; as such, we also present results stratified by self-reported birth weight category. Race and ethnicity are socio-political constructs that often serve as proxies for traditions and culture, as well as historical and ongoing disadvantage in social, economic, environmental, and structural factors. As such, we also present results stratified by self-reported race and ethnicity to examine possible effect modification. Statistical tests were two-sided, and p-values <0.05 were considered statistically significant. All analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Baseline characteristics were compared between participants born preterm and full term, and results are displayed in Table 1. Women born preterm were more likely to be younger at baseline and have a higher level of education than women born full term. Women born preterm also had a slightly higher mean BMI at baseline than women born full term. At baseline, women born preterm and those born at term were similar with respect to other characteristics, including family history of type 2 diabetes, geographic location, self-reported race and ethnicity, smoking status, and alcohol consumption.
Table 1. Baseline characteristics of 85,356 WHI participants by preterm birth status
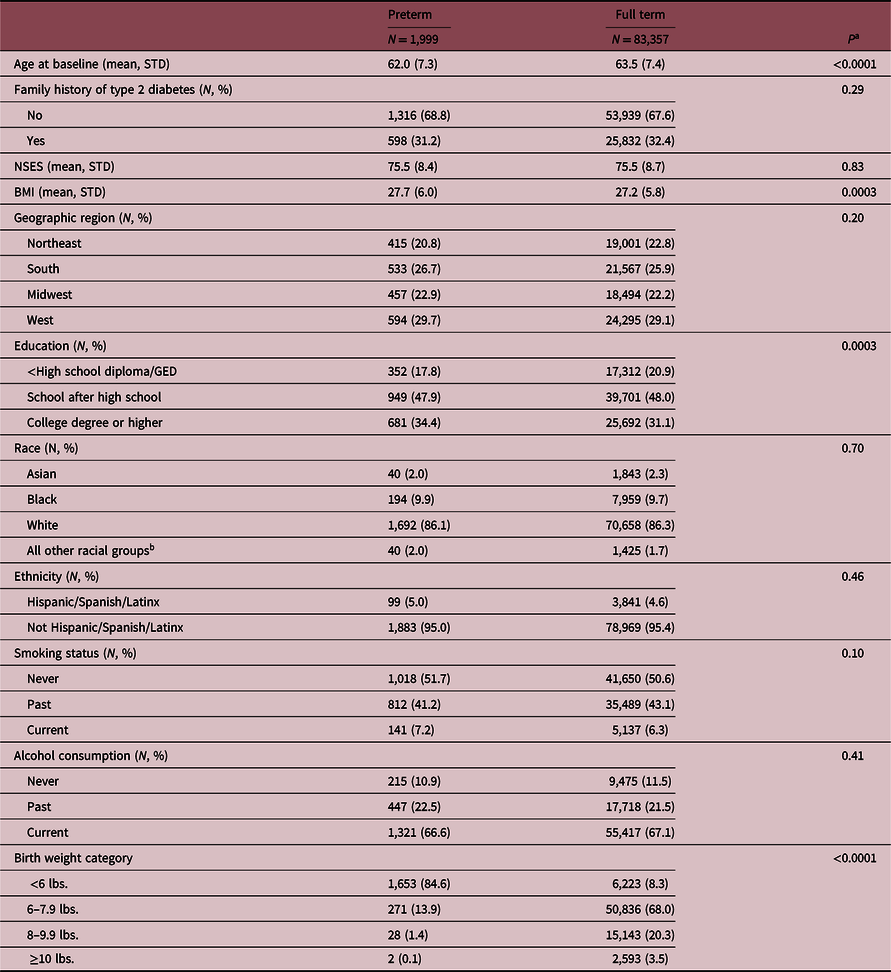
Numbers are N (%) for categorical variables or mean (standard deviation) for continuous variables. aP-values are from t-tests and chi-square statistics. bDue to small sample sizes, we collapsed the Native Hawaiian/Other Pacific Islander, American Indian/Alaskan Native, and Multi-racial categories into one “other” category. Abbreviation: NSES, normalized neighborhood socioeconomic status.
Table 2 shows the unadjusted and adjusted odds ratios for the association between personal history of being born preterm and prevalent type 2 diabetes reported at study entry. Being born preterm was significantly and positively associated with odds for type 2 diabetes at baseline (unadjusted: OR = 1.51, 95% CI 1.24, 1.83; P < 0.0001). The association remained significant and strengthened after adjustment for demographic (OR = 1.78, 95% CI 1.44–2.21; P < 0.0001) and lifestyle factors (OR = 1.79, 95% CI 1.43–2.24; P < 0.0001). Covariates with the largest impact on effect estimates were age at baseline, family history of type 2 diabetes, and education. As expected, models that included adjustment for birth weight category demonstrated an attenuated association between being born preterm and type 2 diabetes. To consider the potential relationships of birth weight and preterm birth status with type 2 diabetes separately (P interaction(BWxPTB) = 0.23), unadjusted and adjusted odds ratios for the association between personal history of being born preterm and type 2 diabetes stratified by birth weight category are shown in Table 3. Even when limiting our analyses to women born in the lowest birth weight category (<6 lbs.), a significant, positive association between being born preterm and prevalent type 2 diabetes at baseline was observed in both the demographic- (adjOR = 1.43, 95% CI 1.10–1.84) and demographic and lifestyle-adjusted models (adjOR = 1.43, 95% CI 1.09–1.87).
Table 2. Relationship between being born preterm and odds of self-reported prevalent type 2 diabetes among postmenopausal women in the WHI at baseline
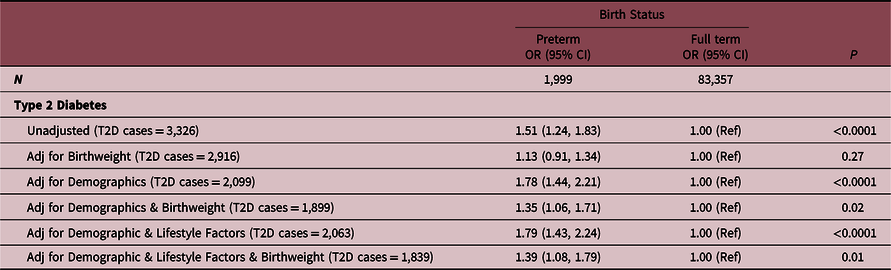
Demographic factors include age, race, ethnicity, normalized socioeconomic status, education, region, and family history of diabetes. Lifestyle factors include BMI, smoking status, and alcohol use.
Table 3. Relationship between being born preterm and odds of self-reported prevalent type 2 diabetes among postmenopausal women in the WHI at baseline, stratified by birthweight
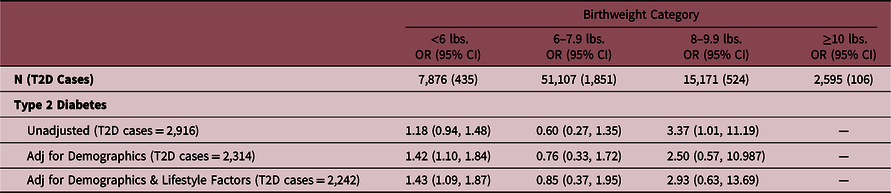
Referent group for each analytical model is full term births. There were an insufficient number of preterm participants born weighing ≥10 pounds, as expected; therefore, these results are left blank ("---"). Demographic factors include age, race, ethnicity, normalized socioeconomic status, education, region, and family history of diabetes. Lifestyle factors include BMI, smoking status, and alcohol use.
Results from stratification by race and by ethnicity are presented in Table 4. Similar to the combined results, we observed a positive association between being born preterm and type 2 diabetes in women who identified as White in both the unadjusted (OR = 1.58, 95% CI 1.28–1.95) and adjusted models (adjOR = 1.87, 95% CI 1.47–2.37). We also observed positive associations between being born preterm and type 2 diabetes when stratifying by women who did (adjOR = 2.77, 95% CI 1.05, 7.34) and did not (adjOR = 1.75, 95% CI 1.40, 2.18) identify as Hispanic/Spanish/Latinx. While not statistically significant, the risk estimates for women who identified as Black also suggests a positive relationship between preterm birth and type 2 diabetes.
Table 4. Relationship between being born preterm and odds of self-reported prevalent type 2 diabetes among postmenopausal women in the WHI at baseline, stratified by self-reported race/ethnicity

Referent group for each analytical model is full term births. Due to small sample sizes, we were unable to consider other self-identified race categories in the stratified analyses, which include: Native Hawaiian/Other Pacific Islander, American Indian/Alaskan Native, and multi-racial. Demographic factors include age, normalized socioeconomic status, education, region, and family history of diabetes. Lifestyle factors include BMI, smoking status, and alcohol use.
Results from models stratified by age at enrollment suggest that the relationship between preterm birth and type 2 diabetes wanes with age (Table 5). Among women who were <50–59 years of age at enrollment, we observed a positive association between being born preterm and type 2 diabetes (adjOR = 2.13, 95% CI 1.43–3.15). With increasing age group at enrollment, the odds for type 2 diabetes becomes attenuated (60–69 years; adjOR = 1.88, 95% CI 1.37–2.58) and non-significant in the oldest age group (70–79+ years; adjOR = 1.27, 95% CI 0.75–2.17).
Table 5. Relationship between being born preterm and prevalent self-reported type 2diabetes among postmenopausal women in the WHI, stratified by age group at enrollment

Referent group for each analytical model is full term births. Demographic factors include age, race, ethnicity, normalized socioeconomic status, education, region, and family history of diabetes. Lifestyle factors include BMI, smoking status, and alcohol use.
Unadjusted and demographic- and lifestyle-adjusted hazards ratios of incident type 2 diabetes are presented in Table 6 (maximum follow-up period: 16.9 years). No statistically significant associations were detected within the incident models for type 2 diabetes. Similarly, non-significant interactions were found with birthweight category (Supplemental Table 1; P interaction = 0.12) and self-reported race (P interaction = 0.99) or ethnicity (Supplemental Table 2; P interaction = 0.61). No statistically significant associations were observed in models stratified by age at enrollment (Supplementary Table 3).
Table 6. Relationship between being born preterm and incident self-reported type 2 diabetes among postmenopausal women in the WHI
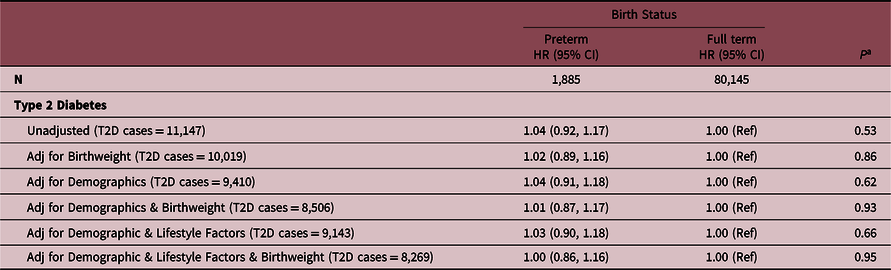
Demographic factors include age, race, ethnicity, normalized socioeconomic status, education, region, and family history of diabetes. Lifestyle factors include BMI, smoking status, and alcohol use.
Discussion
In the well-established WHI cohort of postmenopausal women, we found that women born preterm were at 50-70% increased odds of reporting type 2 diabetes at enrollment compared to women born full term. Findings were robust against a comprehensive set of confounders including age, race, ethnicity, normalized socioeconomic status, education, region, family history of diabetes, BMI, smoking status, and alcohol use. However, the association was not significant in models of incident type 2 diabetes diagnosed during the study period (HR 1.00–1.04; P ≥ 0.53).
There are several possible explanations for the discrepant results between our prevalent and incident models. We hypothesize that the key reason for the discrepant results is age of diagnosis. Participants classified as having type 2 diabetes at baseline would have been diagnosed prior to enrollment while those newly diagnosed with type 2 diabetes after enrollment would have been diagnosed later in life. Unfortunately, we cannot test this hypothesis with the data currently available, as WHI did not collect detailed age at type 2 diabetes diagnosis at enrollment (10-year age windows); however, stratification by the 10-year age windows does demonstrate some support for our hypothesis (Supplementary Table 1). It is also possible that heterogeneity in type 2 diabetes ascertainment at enrollment and during follow-up could have resulted in women with type 1 diabetes included in our prevalent analyses but not our incident analyses. While unlikely, given our exclusion criteria, preterm birth is a known risk factor for type 1 diabetes Reference Crump, Sundquist and Sundquist20 and could impact our results. Additionally, preterm birth, as a condition, is also very heterogeneous, as individuals born at 36 weeks are very different from those born very or extremely preterm. It is possible that our prevalent analyses included individuals born at earlier gestational ages.
To our knowledge, eight epidemiologic studies have evaluated the relationship between being born preterm and risk of type 2 diabetes, including five registry-based cohorts Reference Crump, Sundquist and Sundquist20-Reference Kajantie, Osmond, Barker and Eriksson24 and three cross-sectional studies. Reference Lawlor, Davey Smith, Clark and Leon25-Reference Xiao, Zhang and Cohen27 Consistent with our cross-sectional results from baseline (ORs ranging from 1.5 to 1.7), all prior studies identified statistically significant associations between being born preterm and type 2 diabetes (HR/OR range: 1.26–2.49). The range in effect size is likely explained by methodological differences in study design and sample sizes (2,01927≤ n ≤ 4,193,069 Reference Crump, Sundquist and Sundquist20 ). Model adjustments also varied considerably, with one study presenting only unadjusted estimates Reference Xiao, Zhang and Cohen27,Reference Li, Zhang, Tian, Liu, Yin and Xi37 while all other studies adjusted for a range of covariates. Further, birth weight, which is known to be associated with the risk of type 2 diabetes, Reference Ryckman, Rillamas-Sun and Spracklen36 was only considered as an exclusionary criteria in three studies Reference Crump, Winkleby, Sundquist and Sundquist21,Reference Kaijser, Bonamy and Akre23,Reference Kajantie, Osmond, Barker and Eriksson24 (birth weight for gestational age z-score > 2 or > 4 SD beyond the mean) or as a covariate in one study. Reference Lawlor, Davey Smith, Clark and Leon25
An additional explanation for the wide range of effect estimates from prior studies may be explained, at least in part, by the average age of the participants within each of the studies, providing further evidence to our hypothesis that the relationship between preterm birth and risk of type 2 diabetes is specific to younger age at onset. Our study included women with an average age of 63 at baseline, which is perhaps the oldest population examined to date for this research question. Of the two additional studies that considered older adults, one reported an average age of 62 ± 8 years Reference Xiao, Zhang and Cohen27 and the other reported that all of their participants were between the ages of 58-68 Reference Kajantie, Osmond, Barker and Eriksson24 ; both studies reported hazards ratios between 1.59 and 1.64, which is similar to our cross-sectional results of OR = 1.51–1.75. The other studies focused on younger age groups, including children and adolescents, Reference Crump, Sundquist and Sundquist20,Reference Huang, Lin, Wang, Su and Lin22 young adults, Reference Crump, Winkleby, Sundquist and Sundquist21 and middle aged adults, Reference Kaijser, Bonamy and Akre23,Reference Lawlor, Davey Smith, Clark and Leon25,Reference Pilgaard, Færch and Carstensen26 Further research is needed to answer this question.
All of the prior studies were conducted in predominantly Non-Hispanic White or East Asian populations, including China, Reference Xiao, Zhang and Cohen27 Denmark, Reference Pilgaard, Færch and Carstensen26 Finland, Reference Kajantie, Osmond, Barker and Eriksson24 Sweden, Reference Crump, Sundquist and Sundquist20,Reference Crump, Winkleby, Sundquist and Sundquist21,Reference Kaijser, Bonamy and Akre23 Taiwan, Reference Huang, Lin, Wang, Su and Lin22 and the United Kingdom. Reference Lawlor, Davey Smith, Clark and Leon25 The association between being born preterm and type 2 diabetes may be diminished or strengthened in other race or ethnic groups, limiting the external validity of the previous studies. With our diverse cohort, we stratified our results by race and ethnicity and also considered race and ethnicity as effect modifiers. Among individuals identifying as White and Black, we observed similar significant associations between being born preterm and odds for type 2 diabetes. Furthermore, the observed association between being born preterm and odds for type 2 diabetes was stronger among women who identified as Hispanic/Spanish/Latinx than those who identify as non-Hispanic/Spanish/Latinx. Taken together, our results suggest that the previously described association between being born preterm and subsequent risk for type 2 diabetes holds true in our diverse study population.
The exact mechanism(s) by which being born preterm may increase a person’s risk for developing type 2 diabetes is unknown. Type 2 diabetes is a metabolic disease characterized by insulin resistance, where the cells in the body do not properly respond to insulin secreted by the pancreas and cannot easily take up glucose from the blood. Reference Zheng, Ley and Hu1 The Barker hypothesis suggests that intrauterine and other environmental exposures may permanently alter the body’s metabolism, resulting in early life “programming” alterations that can predispose individuals for type 2 diabetes. Reference Barker6 Because pancreatic beta-cell development occurs during the third trimester, individuals born prematurely may have a reduced number or function of beta cells. Reference Gregg, Moore and Demozay38 Other studies have also reported reduced insulin sensitivity in individuals born prematurely. Reference Hofman, Regan and Jackson39-Reference Rotteveel, van Weissenbruch, Twisk and Delemarre-Van de Waal41 Additionally, individuals born preterm often receive intensive care at birth, including medications, medical procedures, and suboptimal nutrition, which may also impair glucose metabolism. Reference Raju, Buist, Blaisdell, Moxey-Mims and Saigal42
Strengths of our study include use of the large national WHI study with extensive phenotypic data. The prospective design of the WHI also allowed us to evaluate the incident cases of type 2 diabetes with up to 16.9 years of follow-up available. We were also able to consider numerous covariates in our analyses, as the WHI included self-reported data on many potential confounders, as well as sensitivity analyses stratified by birth weight category, race, and ethnicity.
In interpretation of our findings, it is imperative to consider the historical context of preterm birth identification and survival. Presently, the American College of Obstetrics and Gynecology classifies preterm birth as an infant born prior to 37 weeks gestation, as determined from the first ultrasound in combination with the last menstrual period (LMP). 43,44 However, women in the WHI study were born in 1910s–1940s, prior to the development of fetal ultrasounds. Instead, gestational age was often estimated from LMP alone, which is frequently inaccurate and assumes a 28-day menstrual cycle with ovulation at day 14, and the size of the infant at birth. Reference Barr and Pecci45-Reference Wegienka and Baird47 As such, it is probable that the preterm birth exposure is subject to unknown degree of misclassification. It is also important to consider that the survival of infants born extremely preterm was low during that time frame, as incubators, knowledge, appropriately sized equipment, and surfactant was not readily available. Reference Baker48 As such, it is likely that only the “healthiest” of preterm infants survived to be eligible for inclusion in our study. With dramatic improvement in treatment advances of preterm birth, over 95% of all preterm infants who receive modern neonatal and pediatric care now survive into adulthood; thus, the results of our study may not be generalizable to individuals born preterm in subsequent birth cohorts.
Another limitation is the categorical nature of the prematurity variable in the WHI dataset. We hypothesize that the gestational age at delivery across the preterm spectrum impacts the strength of the association with future type 2 diabetes risk. For example, an infant born at 28 weeks is likely to have a different risk profile than a late-preterm infant born at 36 weeks. However, given the categorical nature of the prematurity variable in the WHI dataset we are unable to investigate this association.
We were limited to measuring exposure and outcome by self-report, and the accuracy of all self-reported variables is unknown. The validity of self-reported type 2 diabetes status has previously been demonstrated in the WHI cohort, with high concordance to medical records (77%). Reference Margolis, Lihong and Brzyski34 While self-reported birth weight category has been validated, Reference Troy, Michels and Hunter33 it has not always demonstrated a high validity. Reference Tehranifar, Liao, Flom and Terry49 Further, the validity of self-reported preterm birth, particularly among individuals born in the 1910s–1940s, is unknown as we were unable to identify any studies that validated an individual’s ability to recall their own preterm birth status.
Despite our large sample size, there were a limited number of individuals born preterm (n = 1,999). Additionally, it is possible that our study was limited by survivor bias, as both being born preterm and being diagnosed with type 2 diabetes can cause adverse health effects that may have prevented women from enrolling in the WHI because of illness or early death. However, the magnitude of association between preterm birth and type 2 diabetes would likely be stronger if the women had been available for inclusion in our study. Data on biochemical predictors of diabetes incidence, such as measures of insulin resistance and impaired fasting glucose, were not available for consideration as covariates in analytical models. Finally, we did not have data on other pregnancy exposures or conditions (e.g., in utero tobacco smoke exposure, gestational diabetes) our participants were exposed to in utero that may explain the observed relationship, as these data were not collected as a part of the WHI.
In conclusion, we found that being born preterm was significantly associated with an elevated odds ratio of self-reported type 2 diabetes at enrollment, but not significantly associated with the incidence of type 2 diabetes over the 16.9 years of follow-up for women in the WHI, suggesting the relationship wanes over time. However, further research examining the association between being born preterm and subsequent risk of earlier age at type 2 diabetes is needed. Our research further supports the role of early life exposures in the risk of later-life conditions. Individuals born prematurely may require early evaluation and long-term follow-up for the prevention, detection, and treatment of diabetes and other chronic health conditions. However, the healthcare landscape has changed significantly in the last 75–100 years from when our study participants were born, and our results may not be applicable to all individuals born preterm today. Nonetheless, interventions targeting pre-pregnancy and prenatal care to prevent and reduce complications associated with diabetes may reduce the intergenerational impact of prematurity.
Supplementary materials
For supplementary material for this article, please visit https://doi.org/10.1017/S2040174423000089
Acknowledgements
We thank the WHI investigators and staff for their dedication and the study participants for making the program possible.
Funding statement
The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through 75N92021D00001, 75N92021D00002, 75N92021D00003, 75N92021D00004, 75N92021D00005.
Conflicts of interest
None.









