Introduction
Since Bilroth first described laryngectomy in 1873, several options for post-operative voice restoration have been implemented. The current ‘gold standard’ in rehabilitation is the use of a voice prosthesis following a tracheoesophageal puncture procedure, popularised by Singer and Blom in the early 1980s.Reference Singer and Blom 1 Benefits of tracheoesophageal puncture over other alaryngeal speech methods include longer phonation time, more syllables per breath and greater maximum intensity level.Reference Roxburgh and Perry 2
More contentious, however, is the timing of the tracheoesophageal puncture. The original description of tracheoesophageal puncture insertion was as a secondary procedure in patients post-laryngectomy, but increasingly it has been performed primarily as part of the laryngectomy. This is conducted with the intention of eliminating a second surgical intervention and to accelerate voice rehabilitation.Reference Emerick, Tomycz, Bradford, Lyden, Chepeha and Wolf 3 However, traditionally, a secondary puncture is preferred for patients at higher risk of complications such as wound breakdown and fistula formation,Reference Singer and Blom 1 as it provides more time for adequate healing of the laryngostoma prior to formation of the tracheoesophageal puncture.
It has been established that both primary and secondary tracheoesophageal puncture techniques are safe in the long term,Reference Chone, Gripp, Spina and Crespo 4 with high rates of successful voice rehabilitation. However, there is considerable variation in the voice success rate reported among studies,Reference Kao, Mohr, Kimmel, Getch and Silverman 5 , Reference Cocuzza, Bonfiglio, Grillo, Maiolino, Malaguarnera and Martines 6 which typically ranges from 70 to 90 per cent. Differences in surgical experience, technique and preference, population demographics, and follow-up periods make comparisons of studies evaluating the outcomes of primary and secondary tracheoesophageal puncture difficult.
Critically, no consensus has been reached with respect to whether one approach is more efficacious than the other in terms of voice success, or whether one approach results in a more complicated post-operative period. This systematic review and meta-analysis aimed to evaluate the evidence comparing primary and secondary tracheoesophageal puncture, in terms of voice outcomes, overall complication rate and complication type, with a view to establishing any differences in patient outcome reflected in the literature.
Materials and methods
A comprehensive literature search was conducted of databases including Medline, Embase (Ovid), Cumulative Index to Nursing and Allied Health Literature (‘CINAHL’; Ebsco collections) and the Cochrane Library. The search terms used were: ‘total laryngectomy’, ‘tracheooesophageal puncture’, ‘Blom-Singer prosthesis’, ‘esophageal speech’, ‘laryngectomy’, ‘alaryngeal speech’, ‘larynx, artificial’ or ‘laryngeal prosthesis’, and ‘voice restoration’, ‘speech rehabilitation’, ‘voice prosthesis rehabilitation’, ‘voice rehabilitation’ or ‘speech restoration’. The final search was carried out on 3rd February 2016. The primary outcomes of this study were: voice quality/success, overall complication rate and pharyngocutaneous fistula rate. The inclusion and exclusion criteria are shown in Table I.
Table I Inclusion and exclusion criteria

Blom and Singer described the first tracheoesophageal puncture in 1980. Given the impact on voice outcomes, articles evaluating partial or total glossectomy were excluded. No exclusions were made on the basis of study design alone.
All studies identified by the initial literature search were reviewed independently by two authors (PDC and AELM). All titles and abstracts were assessed, and when in doubt the full text was scrutinised. Data were independently extracted from papers that met the inclusion criteria by two authors, using a piloted proforma. Any differences in extracted data and study eligibility were discussed, and if a dispute remained this was resolved by a senior author. Extracted data included: study type, sample size, follow-up period, loss to follow up, patient characteristics, complications and voice outcomes. Information regarding other treatment modalities (chemo/radiotherapy, neck dissection and reconstruction) was also collated.
After data collection, the two independent reviewers carried out an assessment of the risk of bias in each study. As all the papers studied were non-randomised, a validated measure of the methodological quality features of non-randomised data, the Downs and Black instrument,Reference Downs and Black 7 was used.
Review Manager software (RevMan version 5.3, 2014), available from the Cochrane Library, was used to analyse data collected from the included studies, to produce statistical outcomes and figures.
Results
Literature search
An initial key word search of the listed databases yielded 902 articles in total. After de-duplication and assessment of relevance, 867 articles were excluded. Thirty-five articles were deemed to be relevant. Eleven of these studies, with a total of 937 subjects, met the inclusion and exclusion criteria, and were analysed, as shown in Figure 1.
Fig. 1 Flow chart showing literature search strategy.
Study characteristics and quality
The 11 articles included were all case series in design; 2 were prospectiveReference Maniglia, Lundy, Casiano and Swim 8 , Reference Lukinović, Bilić, Raguz, Zivković, Kovac-Bilić and Prgomet 9 and 9 were retrospective.Reference Boscolo-Rizzo, Zanetti, Carpené and Da Mosto 10 – Reference Wenig, Mullooly, Levy and Abramson 18 The articles were published across a period of 30 years (1985–2015). Sample size ranged from 23 to 145 patients in total. Timing of secondary tracheoesophageal puncture ranged both within and between studies, from one month to over three years. There was a significant male preponderance (83.8 per cent) among the participants included in this analysis. Baseline characteristics are shown in Table II.
Table II Baseline characteristics and quality features
NS = not specified
Data were collected on a range of confounding factors, and reporting of these was variable, as shown in Table III. Every study, except that by Moon et al.,Reference Moon, Raffa, Ojo, Landera, Weed and Sargi 14 reported the total number of patients who underwent chemo/radiotherapy either pre-operatively or post-operatively, but there was variable reporting of the proportion of patients in each group undergoing these treatments. Five of the 11 studies reported did not specify if patients underwent neck dissection at the same time as laryngectomy, and 3 studies did not specify whether there was any concurrent surgical reconstruction.
Table III Major confounding factors
NS = not specified
The articles included provided level 4 evidence 19 and were of generally poor methodological quality. There was no randomisation or blinding, nor any significant effort to eliminate allocation bias across the studies. The mean Downs and Black score was 18.25 (range, 11–22), as shown in Table II.
Follow-up duration ranged from one month to three years, and there was up to 23 per cent loss to follow up across the studies.
Voice outcomes
All the studies included compared voice success/quality between the two groups; however, the definitions used to compare success were very different. Similarly, a range of groups undertook assessment of voice outcome, including speech and language therapists, surgeons, and lay people. Table IV shows the methods of assessment employed.
Table IV Voice assessment and comparison of voice success
*P-values presented when available. SALT = speech and language therapist; HRS = Harrison–Robillard–Schultz tracheoesophageal puncture rating scale
Three studies employed a cut-off score using a voice rating scale to determine successful voice rehabilitation. Other methods of determining success were: use of a voice prosthesis as main means of communication, and ‘excellent’, ‘good’ or ‘intelligible’ use of voice post-operatively. The percentages of patients reaching these standards were compared, some in the immediate post-operative period and others at one year and beyond. None of the studies analysed demonstrated a significant difference in voice outcomes between primary and secondary tracheoesophageal puncture individually.
A meta-analysis was undertaken, which showed a trend favouring better voice outcomes with primary tracheoesophageal puncture, but there was no significant difference in voice success between the two groups (odds ratio = 0.81 (95 per cent confidence interval (CI), 0.50–1.30); Figure 2).
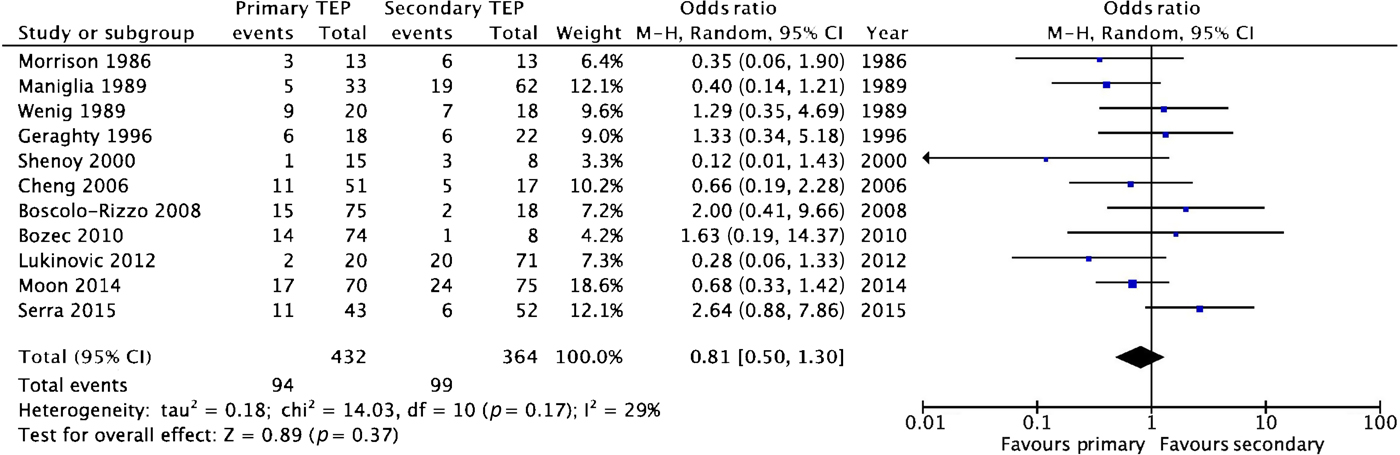
Fig. 2 Forest plot showing meta-analysis of voice outcomes. Percentages of patients with voice failure following primary and secondary tracheoesophageal puncture (‘TEP’) are compared. Voice failure was more prevalent after secondary puncture, though this difference is not significant. M–H = Mantel–Haenszel value; CI = confidence interval
Complications
Data were collected with respect to the total complications in all studies. Only surgical complications were included, with pharyngocutaneous fistula included within the overall complication rate analysis. Other typical complications were: wound infection, bleeding, fistula migration and stomal stenosis. Again, none of the studies independently found any significant difference in overall complication rate between patients undergoing primary and secondary puncture (Table V). Meta-analysis revealed trends towards a generally higher overall complication rate in the primary procedure group, but the difference was not significant (odds ratio = 1.46 (95 per cent CI, 1.00–2.11)), as shown in Figure 3.
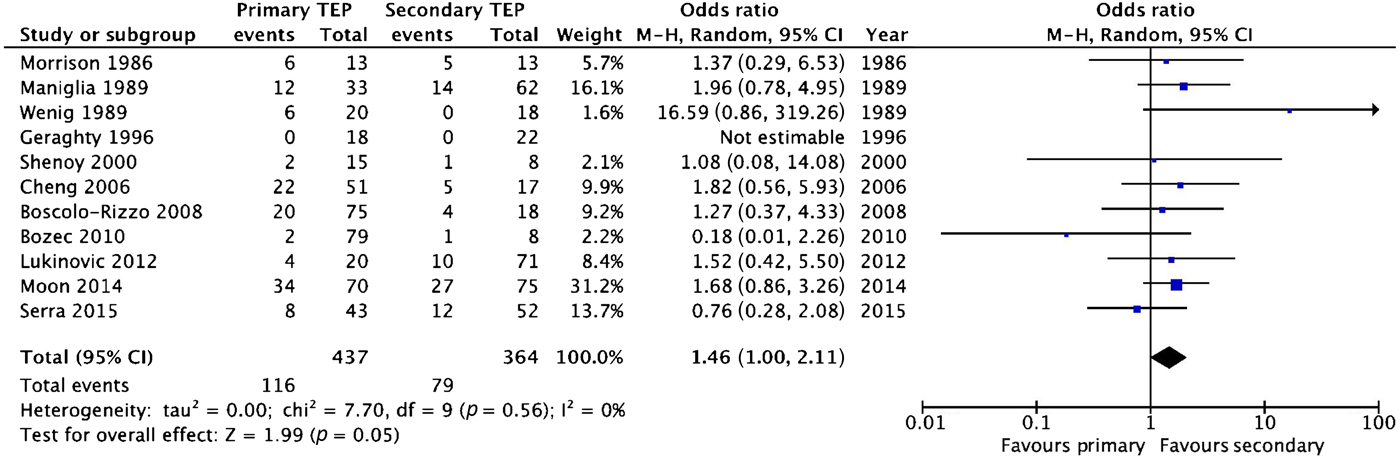
Fig. 3 Forest plot showing meta-analysis of overall complication rates after primary and secondary puncture. The trend suggests the overall complication rate may be lower with secondary puncture, though this was of borderline significance. TEP = tracheoesophageal puncture; M–H = Mantel–Haenszel value; CI = confidence interval
Table V Overall complication rate and pharyngocutaneous fistula incidence
*P-values presented when available.
Pharyngocutaneous fistulae
Five of 11 studies recorded pharyngocutaneous fistula as an individual complication among their analysed population. Generally speaking, these were more prevalent in the studies performed in the 1980s. When reported as a complication, it was quite common, occurring in more than 15 per cent of punctures. None of the studies had statistically compared the rate of fistulae between the two groups. Meta-analysis suggested that pharyngocutaneous fistulae are significantly more common following primary tracheoesophageal puncture (odds ratio = 1.99 (95 per cent CI, 1.07–3.70); Figure 4). Table VI compares the characteristics of the five studies that compared pharyngocutaneous fistula between patients who underwent primary or secondary punctures.
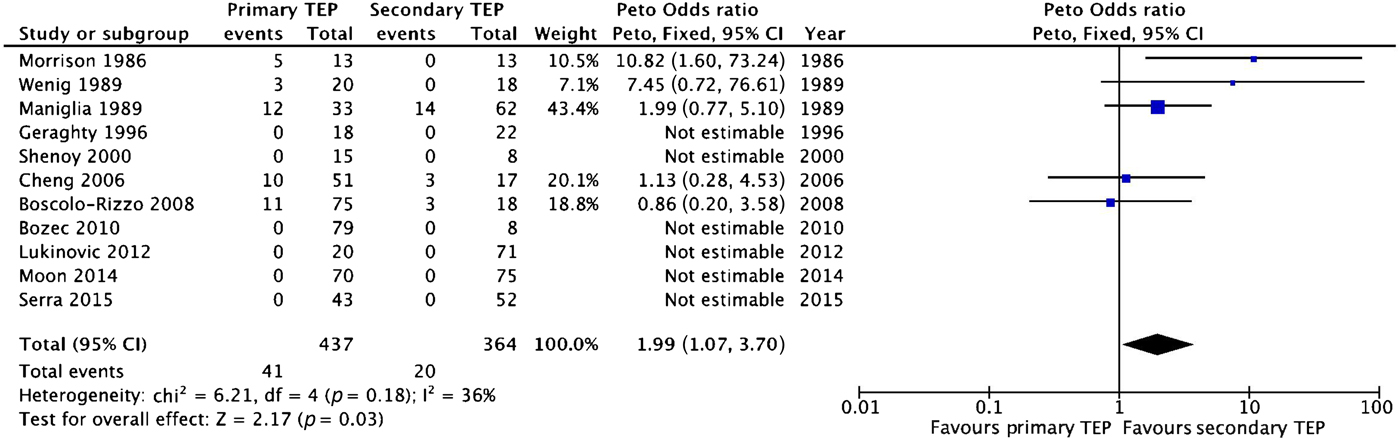
Fig. 4 Forest plot showing meta-analysis of pharyngocutaneous fistula rates after primary and secondary puncture. It appears to be significantly more prevalent after primary puncture. TEP = tracheoesophageal puncture; CI = confidence interval
Table VI Specific characteristics of studies comparing pharyngocutaneous fistula between primary and secondary puncture groups
*This finding was reported, but it was not possible to determine distribution among primary and secondary puncture groups. †Mean time to puncture was not reported in this study.
Discussion
This systematic review and meta-analysis suggests that the outcomes of primary and secondary tracheoesophageal puncture are quite similar. Timing of the tracheoesophageal puncture did not significantly affect voice outcomes, though the trend favours greater voice success with a primary puncture. There was no difference in overall complication rate; however, meta-analysis of the five studies that reported pharyngocutaneous fistula as an outcome found it to be significantly more prevalent following primary punctures.
To our knowledge, this will be the first published meta-analysis comparing the outcomes of primary and secondary tracheoesophageal puncture. A robust literature search strategy was employed, which yielded a sufficient number of studies that directly compared the two interventions to undertake a systematic review and meaningful evaluation. Primary outcomes and study design were similar throughout the included studies, and the data yielded were homogeneous enough to allow for statistical analysis. Baseline characteristics were generally similar. The studies included spanned 30 years and encompass the entire history of the technique.
There were, however, several shortcomings to this study. Baseline characteristics were reported poorly in most cases; only age was reported universally. It was not possible to determine gender distribution in 2 studies,Reference Bozec, Poissonnet, Chamorey, Demard, Santini and Peyrade 11 , Reference Moon, Raffa, Ojo, Landera, Weed and Sargi 14 and only 4 of 11 studies reported the stage of the primary cancer. The overall quality of the data was poor, with studies only providing level 4 data across the board. The reliability of the results is hampered by generally small sample sizes, missing data and variable follow up. No steps were taken to eliminate selection bias among both the retrospective and prospective case series. As mentioned previously, voice outcomes were reported very differently in these studies, and the only measurement tool used consistently was voice success/failure. We were unable to comment on time to voice or voice quality based on the studies included.
The significant finding that pharyngocutaneous fistula seems to be associated with primary tracheoesophageal puncture is limited by the fact that only 5 of 11 studies report this as a complication, despite this being a common issue affecting 10–34 per cent of patients after laryngectomy.Reference Sayles and Grant 20 This may be because the articles included focused on voice outcome, a factor not typically affected by pharyngocutaneous fistula.
In terms of confounding factors, we sought to reduce operative heterogeneity by excluding articles comprising patients who underwent partial or total glossectomy, on the basis of effects on voice outcomes.Reference Rentschler and Mann 21 However, five articlesReference Boscolo-Rizzo, Zanetti, Carpené and Da Mosto 10 , Reference Bozec, Poissonnet, Chamorey, Demard, Santini and Peyrade 11 , Reference Morrison and O'Grady 15 , Reference Serra, Di Mauro, Spataro, Maiolino and Cocuzza 16 , Reference Wenig, Mullooly, Levy and Abramson 18 included patients who underwent circular or non-circular pharyngolaryngectomy (6.4–36 per cent of participants). The distribution of these patients within primary and secondary tracheoesophageal puncture groups was not described in four instances. Serra et al. performed secondary tracheoesophageal puncture on all patients with pharyngolaryngectomy (10 out of 52 patients who received secondary tracheoesophageal puncture).Reference Serra, Di Mauro, Spataro, Maiolino and Cocuzza 16 Bozec et al. performed pharyngolaryngectomy on 37 of 103 patients studied, though not all of these received a tracheoesophageal puncture.Reference Bozec, Poissonnet, Chamorey, Demard, Santini and Peyrade 11 These studies found secondary tracheoesophageal puncture to be significantly associated with pharyngolaryngectomy.
The effect of chemoradiotherapy, reconstruction and neck dissection was not well studied in the articles included. Five studies made mention of all of these factors, and only four of these specified the prevalence of these factors in primary and secondary tracheoesophageal puncture groups. We were unable to control for the effects of these confounding factors, which impairs our ability to study the true impact of timing of puncture.
The trend of our meta-analysis supports a non-inferior voice outcome with primary puncture, and this is reflected in the literature. Chone et al. concluded that voice success rate was significantly higher with primary puncture.Reference Chone, Gripp, Spina and Crespo 4 Gitomer and colleagues concluded that fluency and voice success were similar after primary and secondary puncture, after a mean follow up of 4.7 years.Reference Gitomer, Hutcheson, Christianson, Samuelson, Barringer and Roberts 22 Sinclair and colleagues reported a median time to voice following primary puncture of 56 days versus 200 days for patients who underwent secondary puncture.Reference Sinclair, Rosenthal, McColloch, Magnuson, Desmond and Peters 23 They also found no difference in overall surgical complication rate, which was consistent throughout every paper in the meta-analysis, and was the overall trend.
As pharyngocutaneous fistula is the most serious common complication after laryngectomy, its rates and risk factors have been extensively studied. Our findings suggest an increased risk with primary puncture. This finding is supported by Emerick and colleagues’ study, which concluded an increased risk of fistula in salvage laryngectomy. Conversely, studies by Dowthwaite et al.Reference Dowthwaite, Penhearow, Szeto, Nichols, Franklin and Fung 24 and Parikh et al.Reference Parikh, Irish, Curran, Gullane, Brown and Rotstein 25 found that timing of puncture had no effect on pharyngocutaneous fistula rate. A recent large meta-analysis found that this risk is most marked with combined chemoradiotherapy over simply radiotherapy.Reference Sayles and Grant 20
Future work should focus on exploring risk factors for failing to use a voice prosthesis, as long-term success rates have now been established in both primary and secondary puncture. More emphasis should also be placed on improving the outcomes of salvage laryngectomy given the increasing prevalence of primary chemoradiotherapy treatment for head and neck cancers.
On the basis of this systematic review and meta-analysis, and the supporting literature, there are two main conclusions to be drawn. The non-inferiority of voice outcomes with primary puncture, combined with improved time to voice and no increase in overall complication rate, leads us to advocate the use of primary tracheoesophageal puncture as a safe and efficient method of voice rehabilitation. However, the increased risk of pharyngocutaneous fistula after primary tracheoesophageal puncture found on meta-analysis, albeit based on a small sample size, is supported in the literature, particularly after chemoradiotherapy.
It is our recommendation that the benefits of a primary puncture should be balanced against the risk of pharyngocutaneous fistula. Undertaking a second intervention is prudent following chemoradiotherapy, and should be considered in patients with other risk factors for fistula formation, which include anaemia, chronic obstructive pulmonary disease and concurrent neck dissection, among others.Reference Dedivitis, Aires, Cernea and Brandão 26












