Introduction
The profound global impact of the Covid-19 pandemic on healthcare systems is widely recognised, with worrying increases in adverse maternal, neonatal, and child health (MNCH) outcomes (Chmielewska et al., Reference Chmielewska, Barratt and Townsend2021; Pillay et al., Reference Pillay, Pienaar, Barron and Zondi2021; Townsend et al., Reference Townsend, Chmielewska and Barratt2021). Notwithstanding the direct impact due to pregnant women with symptomatic Covid-19 experiencing more severe outcomes than non-pregnant counterparts (Kotlar et al., Reference Kotlar, Gerson, Petrillo, Langer and Tiemeier2021), the indirect impact is likely to be substantial. The disruption and diversion of resources towards fighting the pandemic and away from essential MNCH care led to poor MNCH outcomes, including increased maternal and child morbidity and mortality (McGinn, Reference McGinn2000; Hall et al., Reference Hall, Samari and Garbers2020; Pfitzer et al., Reference Pfitzer, Lathrop and Bodenheimer2020). It was estimated that a 10% decline in the use of essential MNCH care due to Covid-19 would result in 1.7 million additional women and 2.6 million additional newborns experiencing major complications as a direct result of healthcare disruptions (Riley et al., Reference Riley, Sully, Ahmed and Biddlecom2020), resulting in hundreds of thousands of additional child and maternal deaths (Roberton et al., Reference Roberton, Carter and Chou2020). The impact of the pandemic is believed to have been particularly devastating in low- and middle-income countries (LMICs), especially sub-Saharan Africa (SSA), where additional strains on healthcare systems that were already overburdened and under-resourced even in normal times particularly exposed the vulnerabilities of high-risk population groups (Ameyaw et al., Reference Ameyaw, Ahinkorah, Seidu and Njue2021), especially pregnant women and children. Within the continuum of MNCH care, antenatal care (ANC) provides a platform for important healthcare functions, including health promotion, screening and diagnosis, and disease prevention (Ncube, Reference Ncube2021).
The current study aims to determine the impact of Covid-19 on ANC service utilisation in SSA using the case of Madagascar. Specific objectives are to (i) establish the extent of Covid-19 impact on ANC in Madagascar, (ii) examine sub-population variations of Covid-19 impact on ANC, and (iii) explore potential mediation of Covid-19 on multilevel predictors of ANC. The study strengthens the empirical evidence base for ANC, which is essential to boost national and sub-national preparedness for current and future pandemics in Madagascar and similar SSA settings. Despite the growing literature on the impact of Covid-19 on ANC and MNCH outcomes globally, substantial knowledge gaps remain about the population-level impact of the pandemic on ANC in SSA and the most at-risk sub-groups. Most of the existing empirical evidence on the extent of ANC impact of Covid-19 is largely based on health facility studies (Burt et al., Reference Burt, Ouma and Lubyayi2021; Goyal et al., Reference Goyal, Singh, Singh, Shekhar, Agrawal and Misra2021; Patabendige et al., Reference Patabendige, Gamage and Jayawardane2021; Pillay et al., Reference Pillay, Pienaar, Barron and Zondi2021; Rabbani et al., Reference Rabbani, Saigul, Sulaiman and Ibrahim2021; Ariani, Reference Ariani2022; Landrian et al., Reference Landrian, Mboya, Golub, Moucheraud, Kepha and Sudhinaraset2022; Yadollahi et al., Reference Yadollahi, Zangene and Heiran2022). However, health facility data in most SSA have well-recognised limitations of selection bias since such data exclude a sizeable proportion of the population who do not attend health facilities. There is a need for stronger empirical evidence for a nuanced understanding of the population-level impact of Covid-19 on ANC in SSA.
Madagascar provides an ideal setting for the study, being the first country in SSA to release data under the international Demographic and Health Surveys (DHS) programme, after the onset of the Covid-19 pandemic. Even before the pandemic, Madagascar had poor maternal health indicators, with maternal mortality remaining high at 426 deaths per 100,00 live births, largely due to delay or lack of use of maternal healthcare services, with only 30% of pregnant women receiving 4+ ANC visits as recommended by WHO (Andrianantoandro et al., Reference Andrianantoandro, Pourette and Rakotomalala2021). Like elsewhere in the world, Madagascar’s healthcare system was overwhelmed by Covid-19 (WHO, 2022), and the country endured severe disruptions in essential health services for safe births, putting years of health progress at risk (World Bank, 2022). The first cases of Covid-19, including community transmission in Madagascar, were detected in March 2020, around the same time when Covid-19 was declared a global pandemic by the WHO, and the country responded by adopting various interventions to prevent the spread of the virus in the country, including curfew, lockdowns, travel restrictions, closure of non-essential businesses, and social distancing (Randremanana et al., Reference Randremanana, Andriamandimby and Rakotondramanga2021). State-wide surveillance data from different types of high-risk individuals (including passengers and contacts based on WHO guidelines and patients visiting hospitals) showed 21% of 26,415 individuals tested positive during the first wave of the pandemic: March–September 2020, suggesting that despite stringent measures to prevent and control the spread of Covid-19, Madagascar was unable to stop the spread of the virus in the country (Randremanana et al., Reference Randremanana, Andriamandimby and Rakotondramanga2021). The pandemic exacerbated challenges faced by Madagascar’s health system, intensifying the need to accelerate the fight and prioritise the reduction of maternal mortality, among other key health needs in the country (WHO, 2023). However, little is known about the impact of the pandemic on women of childbearing age in Madagascar (Rakotosamimanana et al., Reference Rakotosamimanana, Mangahasimbola, Ratovoson and Randremanana2023), calling for stronger empirical evidence to inform strategies towards improved maternal/neonatal health in the country.
The literature on Covid-19 impact on ANC in LMICs is rapidly expanding. With the emergence of the Covid-19 outbreak, access to quality ANC services in the SSA region was threatened due to the competition for limited healthcare resources and disruption due to the urgent need to shift limited resources to contain the Covid-19 pandemic (Ogunkola et al., Reference Ogunkola, Adebisi, Imo, Odey, Esu and Lucero-Prisno2021). The lack of in-person clinics during Covid-19 impacted the ability to screen for physical or psychosocial issues, such as elevated blood pressure and mental illness (Lucas and Bamber, Reference Lucas and Bamber2021). A number of health facility-based studies in different LMIC settings have shown a significant impact of Covid-19 on missed ANC appointments (Rabbani et al., Reference Rabbani, Saigul, Sulaiman and Ibrahim2021), delayed start of ANC (Pillay et al., Reference Pillay, Pienaar, Barron and Zondi2021; Landrian et al., Reference Landrian, Mboya, Golub, Moucheraud, Kepha and Sudhinaraset2022), and quality of ANC (Patabendige et al., Reference Patabendige, Gamage and Jayawardane2021). The impact of Covid-19 on MNCH service use and delayed care-seeking has been linked to worsened MNCH outcomes, including an increase in pregnancy complications and adverse foetal and infant outcomes (Burt et al., Reference Burt, Ouma and Lubyayi2021; Kassie et al., Reference Kassie, Wale and Yismaw2021), with some studies indicating a possible indirect effect rather than a causative relationship (Goyal et al., Reference Goyal, Singh, Singh, Shekhar, Agrawal and Misra2021; Yadollahi et al., Reference Yadollahi, Zangene and Heiran2022). Identified predictors of ANC use during Covid-19 include husband’s support, not being afraid of contracting Covid-19, easy access to transportation, ease of ANC fees, no lockdown policy, knowledge regarding Covid-19, Covid-19 information on social media, and Covid-19 prevention protocols in health facilities (Goyal et al., Reference Goyal, Singh, Singh, Shekhar, Agrawal and Misra2021; Ariani, Reference Ariani2022).
This paper builds on existing limited population-based evidence to quantify the extent to which Covid-19 and associated containment measures impacted ANC in SSA, using evidence from the 2021 Madagascar DHS. Ahonsi (Reference Ahonsi2020) underscores the need for stronger evidence base for ensuring adequate attention to the sexual and reproductive health (SRH) related fall-outs of the pandemic, adding that emerging and re-emerging infections are here to stay and that SRH researchers across SSA have an important role to play in boosting national preparedness for future pandemics. The current study focuses on the coverage, timing, and frequency of ANC before and during the Covid-19 pandemic and the sub-groups most impacted in Madagascar. The main research questions include: To what extent has Covid-19 impacted ANC in Madagascar? What sub-groups of the population were most impacted? The analysis of at-risk sub-groups takes into account multilevel (individual, household, and community) predictors of ANC established in existing literature (Magadi et al., Reference Magadi, Madise and Rodrigues2000; Appiah, Reference Appiah2022).
Data and methods
The data
This paper is based on a secondary analysis of the 2021 Madagascar DHS. The DHS is repeated cross-sectional nationally representative household-based surveys that provide data for a wide range of monitoring and impact indicators in the areas of population and health, including ANC in most LMICs, such as SSA. The 2021 Madagascar DHS was the first DHS to be released in SSA following the Covid-19 pandemic. As such, it is the first DHS in SSA where pregnancies cover the period of Covid-19 lockdown from March 2020. Despite the timing of 2021 Madagascar DHS in relation to Covid-19, both household and individual women’s response rates were high at 99% and 95%, respectively (INSTAT et ICF., 2022), and comparable to previous DHS (household – 94%, eligible women – 99%) in the country (INSTAT et ICF Macro. 2010). The analysis of the impact of Covid-19 in this paper focused on a comparison of births that occurred pre-Covid in 2019 and during the pandemic in 2021. To cater for seasonality effects, the sample before Covid-19 was extracted for births during the same months as births during Covid-19 sample (i.e. January–July 2019 pre-Covid-19 vs. January–July 2021 during Covid-19). A total of 2223 births were included in the analysis, 1201 cases pre-Covid-19, and 1022 cases during Covid-19.
The variables
The outcome variable of interest is ANC, focussing on three measures: skilled ANC coverage, timing of first ANC, and frequency of visits, all of which have established links with maternal/neonatal outcomes. Attending ANC remains an integral part of maternity care as it allows for close monitoring of pregnancy development and management of disorders associated with pregnancy and birth preparedness. The WHO recommends a minimum of eight ANC contacts starting during the first semester for a positive pregnancy experience (WHO, 2018) and promotes a model of reduced but ‘focused’ or ‘basic’ ANC (WHO, 2011) consisting of at least four visits targeting LMICs. Among essential tests for maternal and foetal assessments during ANC include regular blood pressure monitoring for all pregnancies to enable detection of dangerous conditions such as preeclampsia and context-specific full blood count testing for diagnosing anaemia in pregnancy and urine test for diagnosing asymptomatic bacteriuria in pregnancy (WHO, 2018). Existing research evidence in diverse LMIC settings has established a significant impact of professional ANC coverage and content on the risk of neonatal and infant mortality in SSA (Arunda et al., Reference Arunda, Emmelin and Asamoah2017; Tekelab et al., Reference Tekelab, Chojenta, Smith and Loxton2019; Islam and Tabassum, Reference Islam and Tabassum2021). A systematic review of the impact of ANC in SSA established that ‘utilization of at least one antenatal care visit by a skilled provider during pregnancy reduced the risk of neonatal mortality by 39%’, highlighting the need for all pregnant women to receive professional antenatal care in order to accelerate progress towards the reduction of neonatal deaths (Tekelab et al., Reference Tekelab, Chojenta, Smith and Loxton2019).
Routinely collected DHS data on birth/pregnancy history during the five years preceding the survey provided key data for the analysis, including data on ANC timing and frequency. All women who had a last birth within the five years preceding the DHS were asked specific questions on ANC for the most recent birth. Specific data on ANC were (i) source/provider of ANC received during pregnancy (doctor, nurse/midwife, community health worker [CHW], traditional birth attendant, or no one), (ii) timing of first ANC (in months), and (iii) frequency of visits. These measures were used to derive specific binary outcome variables for skilled ANC (doctor, nurse/midwife, or CHW as ANC provider), early initiation of ANC (timing of first ANC during the first trimester), and frequent ANC (4+ visits). A final outcome variable for ‘adequate ANC’ was derived for early start and frequent ANC, with ‘adequate ANC’ defined as at least 4 ANC visits starting during the first trimester. Additionally, data on the content of ANC included tests on blood pressure and blood/urine samples.
The main explanatory variable was the period of birth, classified as pre-Covid (i.e. January to July 2019) or during Covid-19 (i.e. from January to July 2021). Births during 2020 include pregnancies where ANC may have been partially affected by the pandemic, while those in different months from the comparison of Covid-19 may have been subject to seasonality effects and therefore excluded from the analysis to avoid contamination. Pregnancies for births during January–July 2021, and associated ANC, will have taken place within the nine months preceding the birth, hence during the Covid-19 period from March 2020. July 2021 is used as the cut-off date, being the last date for births reported in 2021 Madagascar DHS. To ensure comparability, births pre-Covid are for the same months in 2019 to account for seasonality effects. Births during January–July 2020 are excluded from the comparison since most of the pregnancies will have been partly before and partly during Covid-19, contaminating the comparison and masking Covid-19 impact. Only pregnancies that ended in a live birth are included in the analysis since the DHS only collects detailed ANC data on recent live births.
Besides Covid-19, a number of variables known to be associated with ANC based on previous literature were included in the analysis as controls. These included a range of demographic factors, namely: age, parity, marital status, birth interval, and pregnancy intention, as well as socio-economic factors: education, wealth, occupation, and urban/rural residence (Magadi et al., Reference Magadi, Madise and Rodrigues2000; Okedo-Alex et al., Reference Okedo-Alex, Akamike, Ezeanosike and Uneke2019; Appiah, Reference Appiah2022; Andegiorgish et al., Reference Andegiorgish, Elhoumed, Qi, Zhu and Zeng2022). The classification of demographic and socio-economic predictors of ANC included in the analysis are consistent with categories used in previous studies (Appiah, Reference Appiah2022; Andegiorgish et al., Reference Andegiorgish, Elhoumed, Qi, Zhu and Zeng2022), while merging similar risk categories with few cases, to facilitate comparison and ensuring sufficient cases in each category (e.g. age groups) for statistical inference. The distribution of the study sample (classified by ‘pre-Covid-19’ and ‘during Covid-19’) by key characteristics included in the analysis is presented in Table 1.
Table 1. Distribution of study sample by key demographic and socio-economic ANC risk factors, classified by period before and during Covid-19

* Overall sample of all births within five years preceding the survey, including cases excluded from the analysis.
Analytical methods
The analytical strategy in this paper is guided by a socio-ecological model for understanding barriers and facilitators of health service access, which has been widely applied in public health research, including maternal health care (Ma et al., Reference Ma, Chan and Loke2017; Kaiser et al., Reference Kaiser, Fong and Hamer2019). In the context of ANC, existing evidence has established that utilisation is influenced by factors operating at multiple levels, including individual, household, community, and wider societal levels (Magadi et al., Reference Magadi, Madise and Rodrigues2000; Appiah, Reference Appiah2022). The emergence of the Covid-19 pandemic and the associated containment measures adopted by various governments may have modified how the factors operating at various levels influence ANC access and utilisation.
The analysis first examined the distribution of the study sample by key demographic and socio-economic ANC risk factors, classified by period before and during Covid-19 to assess the representativeness of the study sample. This was followed with a descriptive analysis of comparisons between pre-Covid and during Covid-era of ANC measures on uptake, timing, and frequency of visits, as well as essential tests (blood pressure and blood/urine samples) taken during ANC to establish the potential impact of Covid-19 on ANC. Chi-square tests were used to assess significant differences in ANC measures pre-Covid and during the Covid-19 era. Bivariate analysis of sub-population variations in Covid-19 impact was then used to identify sub-groups most impacted by Covid-19. This involved a comparison of factors associated with coverage, early start, and adequate ANC before and during Covid-19, with chi-square tests used to identify significant demographic and socio-economic factors associated with ANC before and during Covid-19.
The bivariate analysis was followed with multilevel logistic regression models to examine individual, household, and community-level predictors of ANC. The multilevel analysis was considered appropriate to account for the hierarchical DHS data structure, which involves a multi-stage sampling design, starting with the selection of clusters, followed by the selection of households and individuals within households. The Madagascar DHS has an additional data hierarchy, with clusters nested within regions. Thus, the analysis sample consists of individual births/mothers (Level 1) nested within clusters (Level 2), which are in turn nested within regions (Level 3). The DHS clusters are normally equivalent to census enumeration areas covering a group of households in a geographic locality (ICF International, 2012). The term clusters and communities are used interchangeably in this paper, as in previous studies (Magadi et al., Reference Magadi, Madise and Rodrigues2000). The analysis involved the application of three-level random intercepts logistic regression models of the form:
where π ijk is the probability of an ANC outcome (no ANC, early ANC start, adequate ANC) for an individual birth i, in the j th cluster in the k th region; B 0 is the regression constant; X 1ijk – X nijk are covariates at individual, cluster, or region level; β 1…B n are the associated regression parameter estimates; and the measures v k, and u jk are the residuals at region and cluster level, which are assumed to be normally distributed with means of zero and variances of σ 2v and σ 2u, respectively (Goldstein, Reference Goldstein2011).
Estimates of region- and cluster-level variances were used to derive intra-cluster and intra-region correlation coefficients to estimate potential clustering of ANC outcomes within communities and regions in Madagascar. Since individual births/mothers in the same cluster are also in the same region, the intra-cluster correlations include region variances (Siddiqui et al., Reference Siddiqui, Hedeker, Flay and Hu1996). Hence, estimates of intra-region (ρ v) and intra-cluster (ρ u) correlation coefficients are obtained as:
where σv2 is the region-level variance, σu2 is the cluster-level variance, and σe2 is the individual-level variance. For multilevel logistic regression models, the level-1 residuals, e ijk, are assumed to have a standard logistic distribution with mean zero and variance
![]() $\pi $
2/3, where
$\pi $
2/3, where
![]() $\pi $
is the constant 3.1416 (Hedeker and Gibbsons, Reference Hedeker and Gibbsons1996).
$\pi $
is the constant 3.1416 (Hedeker and Gibbsons, Reference Hedeker and Gibbsons1996).
The modelling strategy began with an examination of Covid-19 effect on ANC coverage, early start, and adequate ANC using pooled samples before and during Covid-19. The key study variable for Covid-19 period was first added to the model before introducing sets of covariates to the model in sequential stages to establish mechanisms through which Covid-19 may have been linked to ANC outcomes. Interactions of the period (pre-Covid and during Covid) with other ANC risk factors were considered to examine potential mediation of Covid-19 on multilevel predictors of ANC and to identify sub-groups most impacted by Covid-19. To ease interpretation of potential interaction effects, risk factors of adequate ANC for equivalent time periods were compared before and during Covid-19 using separate samples, rather than interaction effects presented based on pooled sample. The MLwiN software was used to run the multilevel models and estimation of parameters based on second-order penalised quasi-likelihood procedure (Rasbash et al., Reference Rasbash, Steele, Browne and Goldstein2020).
Findings
An examination of the distribution of the study sample by background demographic and socio-economic characteristics (Table 1) suggests that the study sample is generally representative of the national population based on the overall DHS sample, apart from a few exceptions. There is evidence that births during Covid-19 comprised a higher proportion of young mothers aged 15–24, rural residents, unemployed/self-employed mothers, or unintended births compared to overall births or births before Covid-19. Furthermore, the study sample before or during Covid-19 had a slightly higher proportion of births in lower socio-economic groups (i.e. mothers with no education or in the lowest household wealth quintile) compared to overall births in Madagascar. These patterns may have important implications on the interpretation of findings presented in this paper in relation to national representativeness.
To what extent has Covid-19 impacted ANC?
A comparison of ANC measures pre-Covid (births in Jan–July 2019) and during Covid-19 (births in Jan–July 2021) shows that ANC coverage, timing, and frequency of visits were all significantly impacted by the pandemic (Table 2a). Approximately 16% of births received no ANC during Covid-19, a significant increase from 12% pre-pandemic (p=0.009). Early start of ANC during the first trimester was significantly lower (p=0.017) during the pandemic (29%) than before the pandemic (34%). Furthermore, a lower proportion of births (p=0.007) had received at least four ANC visits during the pandemic (52%) compared to pre-pandemic (58%). Consequently, a lower proportion of births (p=0.011) received adequate ANC (at least four visits, starting during the first trimester) during the pandemic (21%), compared to pre-pandemic (25%).
Table 2a. Comparison of ANC coverage, timing, and frequency before and during Covid-19(ns)

* – significant at 5% level (chi-square p<0.05);
** – significant at 1% level (chi-square p<0.01);
ns – not significant.
A later start of ANC, coupled with less frequent visits during the pandemic, is likely to lead to a lack of essential tests done during pregnancy to safeguard the health of the mother and newborn. Essential tests, including blood pressure, blood, and urine tests all significantly reduced during the pandemic (Table 2b). Among those who attended ANC, about 21% of births had no blood pressure taken during the pandemic, compared to 17% before the pandemic (p=0.027). Similarly, a significantly higher (p<0.001) proportion of births during the pandemic did not have blood samples taken during ANC (58%), than before the pandemic (50%). Overall, approximately 27% of births before the pandemic had all three essential tests taken during ANC, while less than a quarter (23%) did so during the pandemic.
Table 2b. Comparison of essential ANC tests not taken before and during the Covid-19 pandemic
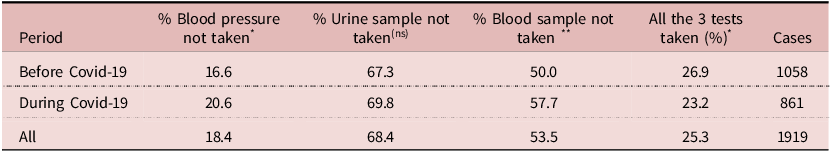
* – significant at 5% level (chi-square p<0.05);
** – significant at 1% level (chi-square p<0.01);
ns – not significant.
A comparison of the number of essential ANC tests taken before and during the Covid-19 pandemic (Fig. 1) confirms that a lower proportion of pregnancies during the pandemic (compared to pre-pandemic) had at least two of the three ANC tests taken, while the reverse was the case for having only one or no test taken.

Figure 1. Number of essential ANC tests taken before and during Covid-19.
How has Covid-19 moderated ANC risk factors/which population sub-groups have been disproportionately affected by Covid-19?
A comparison of bivariate associations between key demographic and socio-economic factors known to be associated with ANC from previous literature, before and during Covid-19, show associations largely consistent with expected patterns (Table 3). Findings confirm generally poorer ANC both before and during Covid-19 among higher order births of parity 5+, shorter preceding birth interval, rural residence, lower socio-economic status (i.e. lower educational attainment or poorest/poorer wealth quintiles), and those who are self or unemployed. Although births during Covid-19 were more likely to have been unintended (wanted later or no more) than births before Covid-19 (Table 1), there was no evidence of poorer ANC among unintended births during or before Covid-19.
Table 3. Comparison of factors associated with coverage, early start, and adequate ANC before and during Covid-19

** Chi-square p<0.01;
* p<0.05;
$ p<0.1;
(ns) p>0.05.
The association showing a clear difference between before and during Covid-19 is variation in ANC by age. Before Covid-19, births to women aged 25–34 years were more likely to receive adequate ANC, compared to births to younger or older women. However, during Covid-19, there was evidence of births among younger women having better ANC, such that the youngest age group of 15–24 years was associated with the best ANC. For instance, while before Covid-19 adequate ANC was lowest among the youth aged 15–24 years (i.e. <22% vs. 30% for 25–34 years and 22% for 35+ years), this age group had the highest proportion of births receiving adequate ANC during Covid-19 (i.e. 25% vs. 18% for 25–34 years and 13% for 35+ years). Consequently, while adequate ANC among the oldest age group (35+ years) reduced by almost half during Covid-19 (from 22% to 13%), the youngest age group (15–24 years) saw a slight improvement (from 22% to 25%).
An examination of Covid-19 risk factor on ANC, taking into account other significant ANC predictors, based on multilevel logistic regression analysis (Table 4) suggests that the impact of Covid-19 on ANC remains largely unexplained by factors considered in the analysis. Before taking into account other predictors (results not shown), Covid-19 was associated with a 39% increase in the odds of receiving no ANC. After controlling for other predictors, including pregnancy intention (unintended pregnancies more likely during Covid-19 and generally associated with poorer ANC), Covid-19 was still associated with an average of 42% increase in the odds of having no ANC across communities and regions in Madagascar, suggesting that the effect of Covid-19 on receiving no ANC was not explained by the covariates considered.
Table 4. Multilevel logistic regression of Covid-19 and other predictors of ANC in Madagascar: 2019 and 2021

R – reference category;
* – significant at 5% level (p<0.05);
** – significant at 1% level (p<0.01);
$ – p<0.1.
With respect to the timing of ANC, the multilevel logistic regression analysis confirms a significant reduction in the early start of ANC during the first trimester. Before controlling for any covariates, births during Covid-19 had an average of 20% lower odds of an early start of ANC across clusters and regions compared to births before the pandemic. After controlling for other significant covariates, births during Covid-19 still had 22% lower odds. For adequate ANC, the reduction in the odds during Covid-19 was 21% in the null model and 22% in the model controlling for other significant covariates.
The effect of the other covariates on ANC was largely as expected. Births to older women were less likely to receive early ANC, and higher order births were more likely to receive no ANC, while higher socio-economic status (educational attainment and wealth) was associated with reduced odds of receiving no ANC and increased odds of adequate ANC. There was also evidence of preceding birth intervals less than two years being more likely to receive no ANC. Besides the observed demographic and socio-economic predictors of ANC, there was evidence of significant variations in receiving no ANC, early, or adequate ANC across clusters and regions in Madagascar. There was evidence of strong variations in ANC coverage across regions and across clusters within regions in Madagascar. Before taking into account any covariates, 15% (i.e. 0.921/(0.921 + 1.798 + 3.29) of the total variation in ANC coverage was attributable to regional differences, while 45% (i.e. (0.921+1.798)/(0.921+1.798+3.29)) was attributable to community/cluster-level variations, with the remaining 40% attributable to individual birth/woman differences. The regional variations were largely explained by covariates included in the model but remained marginally significant at a 10% level and accounted for only 6% of the total unexplained variation in antenatal coverage. However, community/cluster-level differences remained strong. After controlling for significant covariates, 32% of the total unexplained variation in ANC coverage was attributable to unobserved community/cluster-level factors. The regional and community/cluster-level variations for early and adequate ANC were less strong but remained significant for adequate ANC even after significant covariates were accounted for.
The multilevel analysis considered random coefficient models, allowing the effect of Covid-19 to vary across different regions and clusters. However, there was no evidence from the random coefficient models that the effect of Covid-19 on ANC significantly varied across clusters or regions in Madagascar. Finally, a comparison of risk factors of adequate ANC before and during Covid-19 to further understand how Covid-19 may have moderated ANC risk factors and to identify population sub-groups disproportionately affected by Covid-19 is presented in Table 5.
Table 5. Comparison of adequate ANC risk factor before and during Covid-19

R – reference category;
* – significant at 5% level (p<0.05);
** – significant at 1% level (p<0.01);
$ – p<0.1.
Although the effect of age on having adequate ANC was not significant before Covid-19 once other significant factors were controlled for, the relationship appears reversed for the 25–34 age group, such that while before Covid-19 births to women aged 25–34 tended to have higher odds of adequate ANC than births to youth aged 15–24 years, the pattern was reversed and significant during Covid-19, with youth mothers being more likely to have adequate ANC than older mothers.
The other risk factor for adequate ANC showing different patterns before and during Covid-19 was educational attainment, the effect being stronger during than before Covid-19. Higher educational attainment was associated with significantly higher odds of adequate ANC during Covid-19 (p<0.01), but the effect was not significant before Covid-19 once household wealth was controlled for. While primary or secondary education was not significantly different from no education before Covid-19, births to women with primary or secondary education had on average more than double the odds of adequate ANC than births to women with no education during Covid-19. Another socio-economic factor associated with adequate ANC was household wealth, significant for both before and during Covid-19 samples. However, the effect was stronger before than during Covid-19.
Besides the fixed effects, there was evidence of significant variations in adequate ANC across clusters and across regions in Madagascar before and during Covid-19. However, these were largely explained by observed covariates included in the model and ceased to be significant once these factors were controlled for.
Discussion and conclusions
Overall findings presented in this paper suggest that all ANC measures considered (having no ANC, early start of ANC, frequent (4+) visits, and adequate ANC) were significantly worse during Covid-19 than before the pandemic. The effect of Covid-19 remains significant after other significant demographic and socio-economic risk factors were controlled for, suggesting that observed differences could not be attributed to potential changes in any of these factors. Population sub-groups disproportionately affected during Covid-19 include births to older mothers and mothers with no education. While youth aged 15–24 had poorer ANC compared to older women before the pandemic, the pattern was reversed during the pandemic, with older mothers being associated with poorer ANC. There was further evidence that the protective effect of education was stronger during than before the pandemic. For instance, primary or secondary education was not significantly different from no education before the pandemic, once household wealth was controlled for, but those with primary or secondary education had more than double the odds of receiving adequate ANC than those with no education during the pandemic. Observed findings on the extent of the pandemic’s impact on ANC and sub-groups disproportionately affected have important implications for policy/practice and further research.
Unique contribution of the current paper to existing knowledge
This paper makes an important contribution to existing knowledge on the impact of Covid-19 on ANC in Madagascar and similar LMIC settings, especially SSA. First, the nature of the data used and intuitive analytical approach have led to an improved understanding of the extent/magnitude of the population-level impact of the pandemic on ANC, clarifying previous patterns based largely on health facility data and at the same time helped unmask important salient features of the pandemic’s impact based on overall patterns presented in routine DHS reports. Explicit comparisons to illustrate this are provided below under ‘Extent of Covid-19 impact’.
Second, it has revealed novel findings in relation to population sub-groups disproportionately impacted, with important implications for policy/practice. In particular, the patterns observed in relation to the mother’s age have important implications for adolescent/youth maternal health care policy/practice in SSA and similar settings. The existence of youth-friendly reproductive/maternal health (RMH) care policies has not often translated into youth-friendly services in many SSA countries, with unmarried youth seeking RMH often facing stigma and discrimination from healthcare personnel, discouraging them from seeking care (Onukwugha et al., Reference Onukwugha, Agaba, Hayter and Orton2022). In some instances, the implementation of some of the RMH policies that were meant to encourage male participation in RMH (including ANC) compromised care for unmarried youth who were often made to wait long hours or denied ANC altogether (Onukwugha et al., Reference Onukwugha, Agaba, Hayter and Orton2022). It is possible that ANC processes adopted during Covid-19 may have overcome existing barriers and worked better for the youth, especially where services were provided remotely or in less crowded facilities. There are potentially useful lessons to learn from the Covid-19 era for improved RMH service provision for adolescents and youth who bear a disproportionate burden of poor maternal/neonatal health care and outcomes in LMICs. This is particularly relevant in the context of Madagascar, where there have been expressed concerns about adolescents experiencing poor RMH, including early marriage, high fertility, and maternal mortality, with approximately 20% of maternal deaths being among adolescents aged 15–19 years (Gurman and Fohl, Reference Gurman and Fohl2017). Furthermore, observed patterns relating to ANC disparities with respect to mothers’ educational attainment reinforce existing socio-economic inequalities. The findings underscore the particular vulnerability of mothers with no education (or illiterate) during Covid-19 when miscommunication or lack of essential information was a major barrier to seeking and accessing essential care.
While the analysis presented in this paper has provided important insights on the overall impact of Covid-19 on ANC and population sub-groups disproportionately affected by Covid-19, it is important to bear in mind the distribution of the study sample by background demographic and socio-economic sub-groups reported earlier. There was evidence that births during Covid-19 comprised a higher proportion of younger mothers aged 15–24, rural residents, those with no education, in the lowest wealth quintile households, unemployed/self-employed mothers, or unintended births compared to overall births or births before Covid-19. These patterns suggest that the lower use of ANC during Covid-19 observed in this paper may be partly explained by the higher proportion of births during Covid-19 comprising a higher proportion of disadvantaged groups associated with lower ANC. Although the higher proportion of unemployed/self-employed mothers may be attributable to job losses during Covid-19, the higher proportion of births among other disadvantaged groups of mothers (i.e. youth, rural residents, lower socio-economic status) may suggest that these sub-groups were less able to take appropriate action to prevent unintended pregnancies/births during Covid-19. It is encouraging that some of these groups (i.e. the youth) were associated with better ANC during Covid-19. However, the higher proportion of births among some of the disadvantaged groups associated with the worst ANC during Covid-19 (e.g. mothers with no education) reinforces the widely expressed concern of Covid-19 penalising the most vulnerable in society, especially those living in poverty, further amplifying existing deep inequalities in SSA (Okoi and Bwawa, Reference Okoi and Bwawa2020; Anas and Musah, Reference Anas and Musah2023). This underscores the threat of Covid-19 to global efforts to maintain progress towards the SDG health targets by 2030 (Amouzou et al., Reference Amouzou, Maïga and Faye2022).
Extent of Covid-19 impact on ANC
The findings on the extent of Covid-19 impact reveal a substantial and significant impact of Covid-19 on ANC in Madagascar. These findings are consistent with other studies in SSA, which also demonstrate significant reductions in the use of ANC care during the Covid-19 pandemic. In a systematic review from Ethiopia, Mekonnen and Yirdaw (Reference Mekonnen and Yirdaw2023) reported a 13% reduction in ANC coverage during the Covid-19 pandemic because of women experiencing additional access barriers during the Covid-19 pandemic. In the Ethiopian context, key access barriers included a lack of transportation to facilities, fear of getting Covid-19 in health facilities, and maternal adherence to movement restriction measures (Mekonnen & Yirdaw, Reference Mekonnen and Yirdaw2023). It is likely that women in Madagascar encountered similar access barriers, leading to significant reductions in the use of ANC services during the Covid-19 pandemic. However, more studies are needed to further understand barriers to accessing maternal and child health services specific to the context in Madagascar, especially given the substantial reduction in ANC coverage of 42% revealed by the MDHS-2021 analysis.
The need for further research to better understand the extent of Covid-19 impact is reinforced by the fact that existing overall ANC patterns tend to mask important salient features of the pandemic’s impact. For instance, ANC trends reported in the Madagascar DHS report show an upward trend of the three ANC key indicators over the last three decades: an increase of 10 percentage points in the proportion of mothers receiving professional ANC, from 79% in 1992 to 89% in 2021; an increase in the percentage of women who made at least four ANC visits, from 42% to 60% in the same period; and an increase in the percentage of women who had their first ANC visit during the first trimester of pregnancy, from 21% in 1992 to 31% in 2021 (INSTAT et ICF. 2022). These patterns largely reflect patterns for births within the last five years of the survey before Covid-19, masking important features of Covid-19 impact evident from the analysis presented in this paper: a 42% reduction in ANC coverage and a 22% reduction in early start or adequate ANC. This calls for a more comprehensive analysis to provide a better understanding of salient features of the impact of the pandemic in individual countries and wider SSA to inform national and international preparedness for current and future pandemics.
Population sub-groups disproportionately affected by Covid-19
The findings presented in this paper suggest that population sub-groups disproportionately affected during Covid-19 include births to older mothers and mothers with no education. Youth aged 15–24 had poorer ANC compared to older women before the pandemic, but the pattern was reversed during the pandemic, with older maternal age being associated with poorer ANC. Also, the protective effect of education was stronger during than before the pandemic. For instance, mothers with primary or secondary education were not significantly different from those with no education before the pandemic, once household wealth was controlled for. However, those with primary or secondary education had more than double the odds of receiving adequate ANC than those with no education during the pandemic (p<0.01). These findings underscore the importance of targeting the most at-risk groups adversely affected by pandemics (e.g. older mothers during Covid-19) when formulating effective strategies to mitigate the devastating impact of pandemics on MNCH outcomes. Furthermore, there is a need for essential information, education, and key messages during pandemics to be available in formats accessible to non-literate mothers.
Further research is needed to better understand the population sub-groups most impacted by Covid-19. The analysis presented in this paper on what population sub-groups were most impacted by Covid-19 was limited by the small sample size for births after Covid-19 in the multilevel analysis. Hence, most of the associations were not statistically significant due to lack of adequate statistical power. Pooling relevant DHS data across SSA countries may be necessary to achieve sufficient samples to enable more detailed sub-group analysis.
ANC and adverse maternal/neonatal and child health outcomes amidst Covid-19
Overall findings underscore the need for urgent attention and action. The lack of access to ANC is detrimental to downstream maternal and child health outcomes. Earlier predictions suggested that a 10% decline in the use of essential MNCH care due to Covid-19 would result in hundreds of thousands of additional child and maternal deaths (Riley et al., Reference Riley, Sully, Ahmed and Biddlecom2020; Roberton et al., Reference Roberton, Carter and Chou2020), and there is compelling empirical evidence of poorer maternal and child health outcomes during the Covid-19 pandemic. A recent systematic review demonstrated significant increases in stillbirths (OR=1.28, 95% CI 1.22–1.53) and maternal deaths (OR=1.37, CI 1.22–1.53) during the Covid-19 pandemic across multiple regions (Chmielewska et al., Reference Chmielewska, Barratt and Townsend2021). Furthermore, a WHO survey of 11 African countries has demonstrated a 16% increase in maternal deaths during the Covid-19 pandemic (Senkyire et al., Reference Senkyire, Ewetan and Azuh2023). Thus, from a policy perspective, designing and implementing interventions that maintain access to maternal health services during pandemics is a critical component of pandemic preparedness and response. Such interventions are important in maintaining gains in maternal health outcomes during pandemics, particularly in LMICs. Further research studies with large sample sizes or national datasets are needed to improve understanding of the drivers of poor ANC in pandemics in LMICs.
Acknowledgements
Great appreciation to the DHS programme (https://dhsprogram.com/data/) for providing access to the DHS data used in this study.
Author contributions
All authors made substantial contributions to the paper, including study conception and/or interpretation of data, drafting and/or revising the article critically for intellectual content, and approval of the final version of the manuscript being submitted. Specifically, MM led the study conceptualisation and design, data acquisition and analysis/interpretation, and drafting of the original draft and revisions. FO contributed to the study conceptualisation and design, data interpretation, and revising the article critically for intellectual content. Both NK and PW contributed to data interpretation and writing – critical revision of the manuscript for intellectual content. All authors approved the final version of the manuscript being submitted.
Funding statement
This research received no specific grant from any funding agency, commercial entity, or not-for-profit organisation.
Competing interests
The corresponding author (MM) is a member of the Editorial Board of the Journal of Biosocial Science. The other authors have no competing interests to declare.
Ethical statement
This article is based on a secondary analysis of anonymised publicly available data from the international DHS programme, so ethics approval was not required. The DHS data collection procedures comply with rigorous international ethical standards. ‘Procedures and questionnaires for standard DHS surveys have been reviewed and approved by ICF Institutional Review Board (IRB). Additionally, country-specific DHS survey protocols are reviewed by the ICF IRB and typically by an IRB in the host country. ICF IRB ensures that the survey complies with the U.S. Department of Health and Human Services regulations for the protection of human subjects (45 CFR 46), while the host country IRB ensures that the survey complies with laws and norms of the nation’ (https://dhsprogram.com/Methodology/Protecting-the-Privacy-of-DHS-Survey-Respondents.cfm.









