Bipolar disorders have a mean recurrence rate of about 50% at 1 year after an index episode and over 70% at 4 years (Reference Harrow, Goldberg and GrossmanHarrow et al, 1990; Reference Keller, Lavori and CoryellKeller et al, 1993; Reference Gitlin, Swendsen and HellerGitlin et al, 1995). Published treatment guidelines (American Psychiatric Association, 2002; Reference GoodwinGoodwin, 2003) advocate adding psychological therapies to medication to reduce recurrences. Recent randomised controlled trials (RCTs) of efficacy suggest that pharmacotherapy plus brief evidence-based manualised therapy may significantly reduce recurrence rates compared with treatment as usual (Reference Perry, Tarrier and MorrissPerry et al, 1999; Reference Miklowitz, Simoneau and GeorgeMiklowitz et al, 2000; Reference Scott, Garland and MoorheadScott et al, 2001; Colom et al, Reference Colom, Vieta and Martinez-Aran2003a ,Reference Colom, Vieta and Reinares b ; Reference Lam, Watkins and HaywardLam et al, 2003). However, these were single-centre studies that predominantly recruited euthymic patients with relatively little psychiatric comorbidity. In our pragmatic multicentre RCT we aimed to establish whether cognitive–behavioural therapy (CBT) plus treatment as usual is more effective than treatment as usual alone in reducing recurrence rates and lowering weekly symptom levels in a clinically representative sample of individuals with recurrent bipolar disorder.
METHOD
Trial design
Ethical approval was obtained from the UK North East Multicentre Research Ethics Committees to undertake this multicentre, pragmatic, randomised parallel-group controlled treatment trial in people with bipolar disorder, employing independent marked assessments of progress and outcome. We randomised all consenting patients with a definite diagnosis of bipolar disorder who would potentially benefit from CBT because of a recent or recurrent acute bipolar episode. As in the National Health Service, we excluded only those where pilot work showed CBT was not feasible, for example, acute mania (Reference Scott, Garland and MoorheadScott et al, 2001), where CBT was unethical because another psychological treatment was clinically indicated, for example, severe borderline personality disorder with suicidal ideation, or where no appropriate pilot data were available, for example, rapid-cycling bipolar disorder. Participants with recurrent disease were treated at five sites (Cambridge, Glasgow, Liverpool, Manchester and Preston), including teaching and non-teaching centres, and were followed-up for 18 months from entry.
Sample size
With actuarial analysis of time to recurrence (log-rank test) and two-tailed testing, a sample size of 110 per treatment group provides 90% power to detect a reduction in recurrence rate from 50% in treatment as usual to 25% in CBT, with an α <0.02 and 85% power to detect a more modest reduction from 50% to 30% at P=0.05. To allow for a predicted drop-out rate of about 20%, we set a target of 250 participants (50 per study centre).
Inclusion/exclusion criteria
Each centre aimed to recruit as many eligible people as possible who had experienced at least one recurrence of bipolar disorder in the preceding year. The goal was to minimise exclusions and records were kept to identify selection biases. Individuals approached were provided with verbal and written information about the trial and those agreeing to participate gave written informed consent.
Inclusion criteria were:
-
(a) age 18 years or more;
-
(b) a DSM–IV diagnosis of bipolar disorder (American Psychiatric Association, 1994);
-
(c) a history of two or more episodes of illness meeting DSM–IV criteria for mania, hypomania, major depressive disorder or mixed affective disorder, one of which must have been within 12 months of recruitment; and
-
(d) in contact with mental health services within the past 6 months.
Exclusion criteria were:
-
(a) rapid-cycling bipolar disorder (defined as more than four episodes of mania and depression alternating with less than 1 month in between in the past year);
-
(b) bipolar disorder secondary to an organic cause;
-
(c) evidence of severe DSM–IV borderline personality disorder with suicidal ideation or intent in the past 3 months;
-
(d) continuous illicit substance misuse resulting in uncertain primary diagnosis;
-
(e) currently meeting DSM–IV criteria for mania (although these people could be included when their symptoms no longer met criteria for mania of the Structured Clinical Interview for DSM–IV; Reference First, Spitzer and GibbonFirst et al, 1997a );
-
(f) current exposure to a systematic psychological treatment specifically aimed at managing bipolar disorder;
-
(g) unable to read and write English; or
-
(h) unable or unwilling to give written informed consent.
Randomisation procedure
After initial assessment, the researcher undertaking the baseline interview communicated key assessment details to the trial coordinator, who then contacted the Independent Trials and Biostatistics Office at Christie Hospital, Manchester. This office allocated patients to the two treatment groups using a minimisation algorithm that balanced across two clinical variables that have been shown to predict outcome, namely number of previous episodes (five or fewer ν. six or more, as used by Reference Perry, Tarrier and MorrissPerry et al, 1999) and current mental state (three categories of euthymia, depressive episode and hypomania/mixed affective episode; Reference Keller, Lavori and KaneKeller et al, 1992), plus centre. No feedback was given about randomisation to the assessors. If patients were allocated to CBT plus treatment as usual, the trial coordinator made direct contact with the therapist at the appropriate centre who then offered an appointment within 2 weeks.
Outcome measures
Trained research assistants masked to treatment condition conducted all assessment interviews immediately prior to randomisation and then face-to-face interviews every 8 weeks for 72 weeks.
Baseline data
Data collected before randomisation included diagnostic classification according to SCID–DSM–IV (First et al, Reference First, Spitzer and Gibbon1997a ,Reference First, Spitzer and Gibbon b ), diagnoses of past episodes of bipolar disorder (American Psychiatric Association, 1994), detailed background data (including demography) and initial ratings on outcome measures.
Primary outcome measures
Primary outcome measures included:
-
(a) time to recurrence of an episode of bipolar disorder of sufficient severity to reach DSM–IV criteria for major depressive, hypomania, mania or mixed episode, based on the SCID interview (Reference First, Spitzer and GibbonFirst et al, 1997b ), following at least 8 weeks below this level for that pole;
-
(b) a longitudinal severity rating of overall symptom levels for each week since the last assessment interview (2 months), based on the Longitudinal Interval Follow-up Evaluation (LIFE–II; Keller et al, Reference Keller, Lavori and Friedman1987, Reference Keller, Lavori and Kane1992). Two LIFE scores were included, one for mania and one for depression and both employed a six-point scale (1=no symptoms, through to 6=DSM–IV major depressive episode or mania with psychotic symptoms or severe impairment of function);
-
(c) total costs – these data will be reported separately.
Secondary outcome measures
We also collected data on some secondary outcome measures (not reported here) such as social adjustment and quality of life.
Interventions
Cognitive–behavioural therapy
Twenty sessions of CBT were held weekly until week 15 and then with gradually reducing frequency until week 26. Two ‘booster sessions’ were offered (at weeks 32 and 38) to review the skills and techniques learned. The CBT approach used was based on Beck's model and is similar to the formulation-based approaches described for other severe mental disorders (Reference ScottScott, 2002). The goals for CBT were to: facilitate acceptance of the disorder and need for treatment; help reduce day-to-day variability in mood and symptoms; recognise and manage psychosocial stressors and interpersonal problems; teach CBT strategies to cope with depression, cognitive and behavioural problems; identify and modify dysfunctional automatic thoughts, underlying maladaptive assumptions and beliefs; improve medication adherence and, if required, tackle substance misuse; teach early recognition of symptoms of recurrence and coping techniques for these symptoms. In individuals who were euthymic, the therapist and patient determined the order of priority for tackling the problems identified. In those currently with an acute episode, the immediate focus was on symptom reduction and stabilisation of mental state, followed by tackling key concerns from the problem list.
Treatment as usual
This was administered to all participants by their usual psychiatric team and included prescription of medications and contact with key mental health professionals with whatever frequency was considered appropriate. Clinicians were specifically asked not to introduce any form of systematic psychotherapy for bipolar disorder for the duration of the study, but there were no other treatment constraints.
Quality assurance
All therapists had attended a 1-year post-qualification training course in CBT and/or met minimum internationally agreed criteria for accreditation as a CBT therapist. Specific training in CBT for bipolar disorder was given for 3 months prior to the trial. During the study, therapists were supervised individually for about an hour per week and all five therapists met for half a day approximately every 6 weeks to discuss specific issues regarding the implementation of the trial protocol and to ensure they adhered to the CBT manual. Differences in therapist competency and adherence to CBT for bipolar disorder were monitored by audio-recording of therapy sessions.
Training of research assistants in all the interview assessment measures was undertaken through joint monthly meetings for 3 months prior to the study. Audio-taped practice interviews were reviewed and rerated by research assistants from other trial centres. Issues of validity or reliability were discussed and resolved at the joint meetings. If interviewers became unmasked, they were asked to report this, with the circumstances, to the trial coordinator.
Statistical analysis
All analyses were carried out on an intention-to-treat basis, including all participants randomised in the trial. The interval in weeks from randomisation to recurrence was analysed using Kaplan–Meier recurrence-free curves with significance tests based on the Cox proportional-hazards regression model. Treatment effects and pre-stratification design factors, trial centre, number of previous episodes of bipolar disorder (five or fewer, six or more) and mental state (euthymic, depressed, and hypomanic/mixed), were included as covariates, along with gender, prescription (or not) of any mood stabiliser and psychiatric comorbidity (defined as substance misuse, other mental disorder or personality disorder). Separate analyses were conducted for three different types of recurrence (any, depressive, and hypomanic/manic/mixed). Statistical significance was set at P<0.05.
Analyses were conducted using the Statistical Package for the Social Sciences version 11.01 and SAS system release 8.2 for Windows. Repeated measures analysis of variance (ANOVA) was conducted by averaging weekly LIFE–II ratings over 4-week intervals separately for depression and mania. In addition, a ‘worst LIFE score’ was created by taking the highest LIFE rating for either depression or mania at each point and again averaging over a 4-week period. This analysis was carried out using SAS system release 8.2 and a mixed model (PROC MIXED) that takes account of the unbalanced effect that arises from missing observations. The analysis incorporated two between-participant effects (between groups and between participants within groups) and three within-participant effects (between times, group by time interactions and random variation).
Previous RCTs of psychological treatment in bipolar disorder have explored an interaction between treatment and number of previous episodes (Lam et al, Reference Lam, Bright and Jones2000, Reference Lam, Watkins and Hayward2003; Reference Miklowitz, Simoneau and GeorgeMiklowitz et al, 2000). We therefore undertook a secondary analysis incorporating number of previous episodes divided into quartiles (≤6, 7–11, 12–29, ≥30) and the remaining baseline covariates used for the main analyses.
RESULTS
Recruitment, retention and sample characteristics
Flow of patients into the trial and sample characteristics
Entry of the patients into the trial (organised according to the CONSORT recommendation; Reference Moher, Schulz and AltmanMoher et al, 2001) is shown in Fig. 1. Case-note or other identifying information was assessed to uncover potential study participants. Patients who refused to give consent but were otherwise eligible for the study did not differ in age and gender from those who consented to take part.

Fig. 1 Trial CONSORT diagram. CBT, cognitive–behavioural therapy; TAU, treatment as usual.
There were 253 patients that met the inclusion criteria and gave written informed consent to participate. Demographic and clinical characteristics of the CBT plus treatment as usual (n=127) and the treatment as usual alone (n=126) groups were well matched (Table 1). There were 161 patients (64%) with one or more of the following clinical features: current episode (major depression, mixed, or hypomania), current substance misuse or dependence, current Axis 1 psychiatric comorbidity, comorbid borderline or antisocial personality, and 30 or more previous episodes of bipolar disorder.
Table 1 Baseline characteristics of groups

| Treatment | ||
|---|---|---|
| TAU (n=126) | CBT (n=127) | |
| Age, years: mean (s.d.) | 42.7 (11.4) | 39.7 (10.3) |
| Gender, n (%) | ||
| Female | 79 (63) | 85 (67) |
| Male | 47 (37) | 42 (33) |
| Status, n (%) | ||
| Living with partner | 56 (44) | 46 (36) |
| Single | 70 (56) | 81 (64) |
| Centre, n (%) | ||
| Cambridge | 25 (20) | 24 (19) |
| Glasgow | 26 (21) | 29 (23) |
| Liverpool | 24 (19) | 26 (21) |
| Manchester | 25 (20) | 24 (19) |
| Preston | 26 (21) | 24 (19) |
| HRSD score: median (IQR) | 6.0 (2-14) | 8.0 (3-13) |
| BDI score: median (IQR) | 11.0 (4-23) | 12.5 (6-22.8) |
| BRMS score: median (IQR) | 1.0 (0-3) | 2.0 (0-3) |
| Bipolar disorder, n (%) | ||
| I | 119 (94) | 119 (94) |
| II | 7 (6) | 8 (6) |
| Current episode, n (%) | ||
| Not in episode | 85 (68) | 86 (68) |
| Depressed | 30 (24) | 30 (24) |
| Hypomanic | 8 (6) | 6 (5) |
| Manic/mixed | 3 (2) | 5 (4) |
| Number of previous episodes, n (%) | ||
| 2-6 | 39 (31) | 35 (28) |
| 7-11 | 29 (23) | 25 (20) |
| 12-29 | 27 (22) | 32 (25) |
| ≥ 30 | 31 (25) | 35 (28) |
| Depressive episodes: median (IQR) | 5 (2-15) | 6 (3-20) |
| Hypomanic/manic/mixed episodes: median (IQR) | 4 (2-9) | 4 (2-8) |
| Lifetime or current other psychiatric diagnosis, n (%) | ||
| Yes | 42 (33) | 52 (41) |
| No | 84 (67) | 75 (59) |
| SCID borderline and/or antisocial personality disorder, n (%) | ||
| Yes | 9 (7) | 9 (7) |
| No | 117 (93) | 118 (93) |
| Lifetime or current substance misuse or dependence, n (%) | ||
| Yes | 59 (47) | 59 (47) |
| No | 67 (53) | 68 (54) |
| On antidepressant at inclusion, n (%) | ||
| Yes | 54 (43) | 55 (43) |
| No | 72 (57) | 72 (57) |
| Imipramine equivalent dose at inclusion, mg: median (IQR) | 125 (90-250) | 125 (60-180) |
| On mood stabiliser at inclusion, n (%) | ||
| Yes | 106 (84) | 107 (84) |
| No | 20 (16) | 19 (15) |
| Drug dose at inclusion, mg: median (IQR) | ||
| Lithium | 800 (600-1000) | 800 (800-1000) |
| Carbamazepine | 550 (400-800) | 400 (350-800) |
| Sodium valproate | 900 (525-1200) | 750 (400-1200) |
| On neuroleptic at inclusion, n (%) | ||
| Yes | 56 (44) | 71 (56) |
| No | 70 (56) | 55 (44) |
| Chlorpromazine equivalent dose at inclusion, mg: median (IQR) | 150 (75-300) | 150 (50-300) |
| Previous psychological treatment | ||
| Yes | 15 (12) | 17 (13) |
| No | 111 (88) | 110 (87) |
Attrition rates
Figure 1 shows that 105 participants receiving CBT (83%) and 111 receiving treatment as usual (88%) remained in the study during the treatment phase; 99 (78%) and 101 (80%) respectively completed follow-up to 72 weeks of the study: information on recurrences was available for all participants except 4 (2%).
Reliability and quality assurance
Pairs of raters independently assessed 70 taped interviews. There was good agreement on DSM–IV episode diagnosis (kappa=0.92, 95% CI 0.81–1.00), and only 6% of LIFE depression and 4% of LIFE mania scale ratings fell outside the acceptable range (two standard deviations above or below the mean difference between the two ratings).
In 34 instances (29 CBT, 5 treatment as usual) the research assessor was unmasked. However, only 11 of these (9 CBT, 2 treatment as usual) occurred before the first recurrence of a bipolar episode.
Ratings of audiotapes of CBT sessions indicated that therapists met the criteria for competency, although some scored consistently higher than others. Assessment of adherence to the CBT protocol suggests that therapists found it difficult to complete the full course of CBT in the time available. A significant proportion of patients (40%) did not receive all the planned components of the package. However, 98 patients (77%) received 13 or more sessions of CBT.
Outcomes
Recurrence
Of the 253 patients entered into this trial, 131 (52%) had a recurrence during follow-up, 67 receiving CBT (53%) and 64 (51%) on treatment as usual. Of the first recurrences 78 (60%) were depressive episodes (39 patients receiving CBT (58%) and 39 receiving treatment as usual (61%)) and 53 (40%) were manic, hypomanic or mixed (28 patients receiving CBT (42%) and 25 receiving treatment as usual (39%)).
Table 2 and Fig. 2 show no between-group differences in rates of recurrence (hazard ratio=1.05, 95% CI 0.74–1.50), with rates of about 30% at 6 months and about 60% at 18 months. The same pattern was demonstrated in per protocol analyses and when depressive and manic recurrences were considered separately. Stratified analyses of patients who were or were not in episode at baseline gave similar results. There were also no significant differences in duration of each illness episode between treatment groups. There was no effect of CBT on adherence to any psychotropic medication.
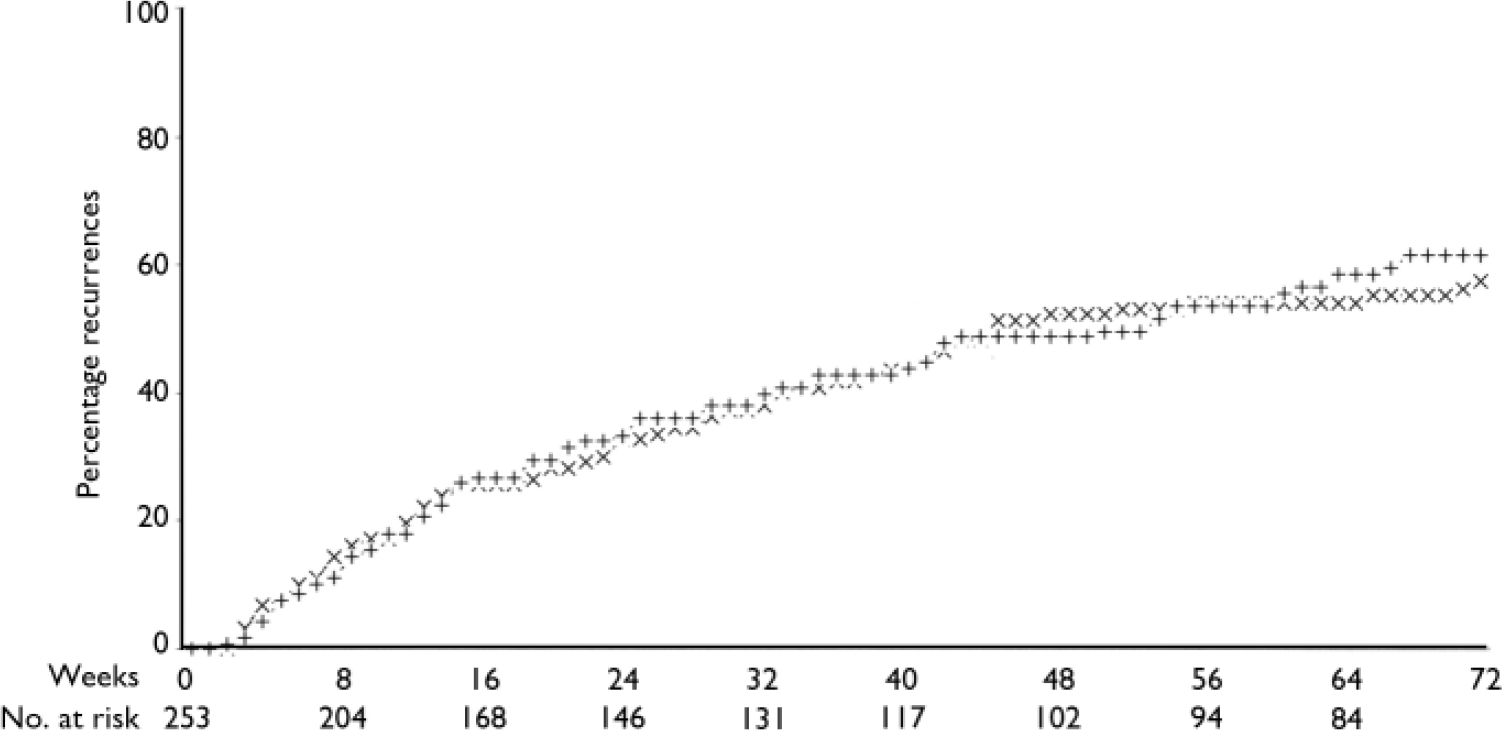
Fig. 2 Actuarial cumulative percentage recurrence curves (Kaplan–Meier): intention-to-treat analysis of any recurrence. –6–, treatment as usual; +++, cognitive–behavioural therapy.
Table 2 Actuarial cumulative recurrence rates (intention-to-treat analysis)
| Recurrence1 | Follow-up | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 24 weeks | 48 weeks | 72 weeks | |||||||
| n | % | n | % | n | % | ||||
| Any | |||||||||
| TAU | 38 | 32.6 | 59 | 52.2 | 64 | 57.4 | |||
| CBT | 38 | 33.2 | 54 | 48.6 | 67 | 61.6 | |||
| TAU minus CBT (95% CI) | -0.6 (-12.8 to 11.6) | 3.6 (-19.6 to 16.8) | -4.2 (-17.4 to 9.0) | ||||||
| Depressive | |||||||||
| TAU | 28 | 24.0 | 44 | 38.9 | 49 | 43.9 | |||
| CBT | 28 | 24.8 | 42 | 38.4 | 50 | 46.5 | |||
| TAU minus CBT (95% CI) | -0.8 (-11.9 to 10.3) | 0.5 (-12.4 to 13.4) | -2.6 (-15.9 to 10.7) | ||||||
| Manic | |||||||||
| TAU | 16 | 13.9 | 30 | 27.4 | 37 | 34.8 | |||
| CBT | 22 | 19.4 | 32 | 29.1 | 43 | 40.6 | |||
| TAU minus CBT (95% CI) | -5.5 (-15.2 to 4.2) | -1.7 (-13.7 to 10.3) | 1.16 (0.74 to 1.82) | ||||||
LIFE ratings
As shown in Fig. 3, repeated-measures ANOVA for the symptom ratings (LIFE–II) showed no between-group differences over 18 months. Analyses of the number of weeks with LIFE scores of 5 or 6 (indicative of relapse), area under the curve of LIFE scores for depression, mania or the worst score, and time to remission (8 consecutive weeks with a LIFE score=1) failed to show any effect of treatment group. There was also no treatment effect when patients were stratified according to whether they were in episode or not at the time of randomisation.
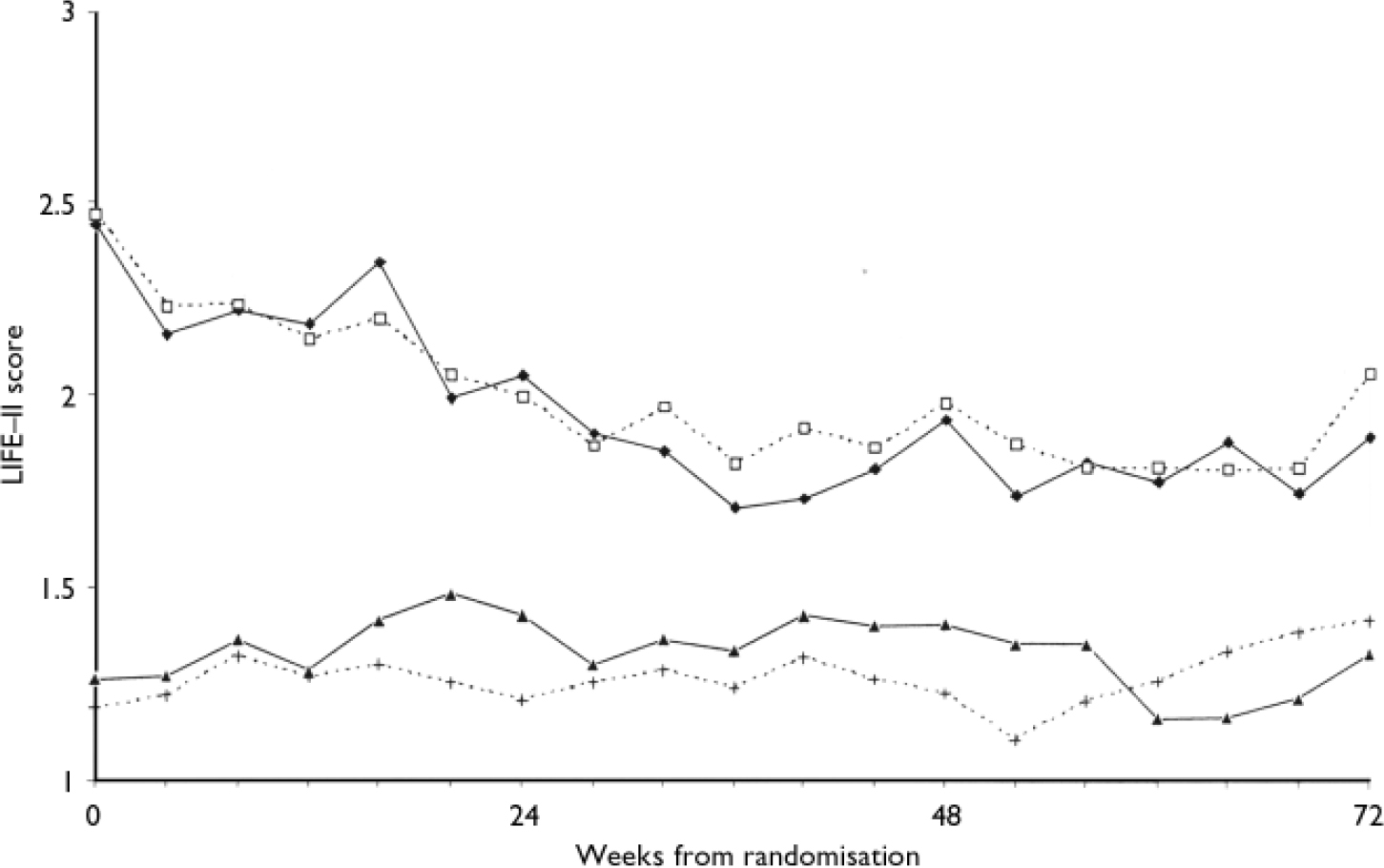
Fig. 3 LIFE–II depression and mania scores (4-week averages) according to weeks from randomisation. –♦–, treatment as usual depression; –▴–, treatment as usual mania; ---□---, cognitive–behavioural therapy (CBT) depression; ---+---, CBT mania.
Interaction with number of previous episodes
In a post hoc analysis a significant interaction was found between randomised treatment and number of episodes recorded at baseline assessment (hazard ratio=0.74, 95% CI 0.56–0.98, P=0.04). Figure 4 shows that treatment as usual resulted in a slight increase in the proportion who experienced recurrence (55% in those in the first quartile, 66% in those in the last quartile), whereas the CBT group had a steeper increase from 41% (first quartile) to 81% (last quartile). A similar post hoc interaction was found with a median split (<12, 12 or more) in number of previous episodes (hazard ratio=0.51, 95% CI 0.26–0.98, P=0.043).
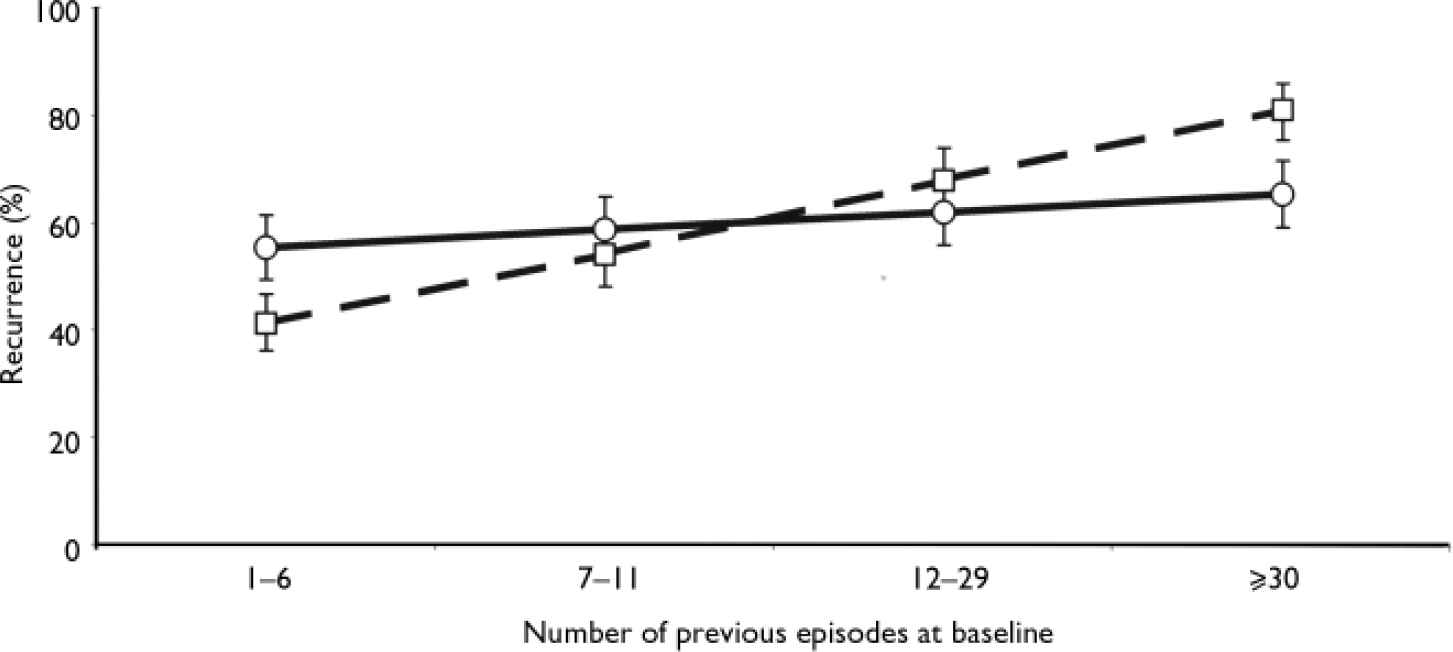
Fig. 4 Actuarial percentage recurrence according to treatment group and number of previous episodes (Cox regression analysis). —○—, treatment as usual;— —□— —, cognitive–behavioural therapy.
DISCUSSION
In keeping with other recent research we have demonstrated that when individuals with bipolar disorder are closely monitored they experience significant subsyndromal symptoms and high rates of recurrence (e.g. Reference Harrow, Goldberg and GrossmanHarrow et al, 1990; Reference Keller, Lavori and CoryellKeller et al, 1993; Reference Gitlin, Swendsen and HellerGitlin et al, 1995). Attrition rates for both CBT and treatment as usual in this trial are comparable with treatment trials for psychological therapies in general and trials for bipolar disorder in particular. However, nearly all the RCTs of psychological therapies for bipolar disorder published to date have shown statistically significant reductions in recurrence rates in the experimental compared with the control treatment conditions. These previous findings are promising rather than conclusive; for example, in some instances, the effect was apparent only for mania (Reference Perry, Tarrier and MorrissPerry et al, 1999) or was related to total admissions rather than survival time (Reference Miklowitz, Simoneau and GeorgeMiklowitz et al, 2000; Reference Scott, Garland and MoorheadScott et al, 2001). Nevertheless, explanations for the differences between our findings and those of other RCTs need to be considered in terms of patient characteristics, treatment approach and methodology employed.
Patient characteristics
Our RCT targeted individuals with recurrent and often complex presentations of bipolar disorder, a group highly representative of persons with bipolar disorder using adult mental health services. It has been argued that, given the relative scarcity of qualified therapists, this group should be given clinical priority for combined medication and psychological treatments because they are less likely to achieve good outcomes with pharmacotherapy alone (Reference GoodwinGoodwin, 2003). However, the clinical features manifested by these individuals often lead to their exclusion from any RCT, so the empirical basis for this proposal is weak. Our study recruited a sample that was more heterogeneous than previous RCTs, which have rarely included individuals with:
-
(a) current substance misuse or dependence;
-
(b) frequently recurrent bipolar disorder (often reporting 20–30+ previous episodes) with relapse in the previous 6 months;
-
(c) other comorbid Axis I disorders; or
-
(d) those in an acute episode at the time of randomisation.
One or more of these features was present in 30% or less of the samples recruited to the seven previous RCTs of psychological treatments in bipolar disorder (Reference Perry, Tarrier and MorrissPerry et al, 1999; Lam et al, Reference Lam, Bright and Jones2000, Reference Lam, Watkins and Hayward2003; Reference Miklowitz, Simoneau and GeorgeMiklowitz et al, 2000; Colom et al, Reference Colom, Vieta and Martinez-Aran2003a ,Reference Colom, Vieta and Reinares b ; Reference Rea, Tompson and MiklowitzRea et al, 2003), compared with 57% of our sample. Therefore, as with unipolar disorders, patient characteristics may be as predictive of the outcome of psychological treatments for bipolar disorder as the specific therapy model used (American Psychiatric Association, 1993).
Treatment approach
We ensured that we used skilled CBT therapists who adhered to the CBT protocol. All had appropriate experience and qualifications, and they were given intensive pre-trial training. Use of a treatment manual, level of ongoing supervision, regular joint therapists’ meetings, and independent evaluation of both therapist competence and adherence to the protocol, combined with a lack of between-centre differences in outcomes for the CBT group, all suggest that our results cannot be accounted for by variation in therapist expertise or the delivery of substandard therapy.
In addition, review of our CBT intervention demonstrates that we used techniques that are common to the majority of therapy models employed in previous trials of psychological treatments in bipolar disorder (targeting education about bipolar disorder, medication adherence, substance misuse, lifestyle regularity, and symptom management and relapse prevention). Although there have been differences in emphasis between the therapies, we did not exclude previously effective interventions or include any techniques that adversely affected the individual. However, the goals of CBT were not achieved in 40% of patients allocated to CBT in this trial, indicating that the intervention may not have been delivered optimally for many. Therapists’ reports suggest a variety of reasons for this, including difficulties in engagement with therapy, lack of time to focus on other therapy targets after overcoming acute episode symptoms, or difficulties associated with comorbid mental disorders and/or complex presentations.
Treatment as usual was not standardised across centres or different psychiatric teams within centres. Results of a multicentre RCT that recruits from different psychiatric teams at each centre are more widely generalisable and more likely due to therapy rather than a charismatic therapist. However, in a multicentre RCT there is greater heterogeneity in both the treatment as usual and patient characteristics than in a single-centre RCT that often recruits from one service (Reference Perry, Tarrier and MorrissPerry et al, 1999; Lam et al, Reference Lam, Bright and Jones2000, Reference Lam, Watkins and Hayward2003; Reference Miklowitz, Simoneau and GeorgeMiklowitz et al, 2000; Reference Scott, Garland and MoorheadScott et al, 2001; Colom et al, Reference Colom, Vieta and Martinez-Aran2003a ,Reference Colom, Vieta and Reinares b ). Thus the benefits of a new intervention over treatment as usual may be more difficult to demonstrate.
Methodology
We went to great lengths to reduce between-centre differences in the quality, independence and masking of the assessment interviews of the research assistants. We undertook prospective intensive face-to-face 8-weekly re-evaluations of the participants’ symptom ratings and social functioning using established and robust measures to ensure an accurate picture of each individual's progress. The sample was large and the study well powered. The recurrence rate in the treatment as usual group was almost exactly what we had predicted prior to the study and is similar to that reported in the treatment as usual group in the RCT of CBT ν. treatment as usual undertaken by Lam et al (Reference Lam, Watkins and Hayward2003). The frequency and comprehensive nature of the follow-up interviews meant that we were extremely unlikely to miss any recurrences meeting criteria for an episode of bipolar disorder. We were not reliant on self-completed patient questionnaires or hospital admission data alone to determine outcomes. The few instances of unmasking before the first recurrence (4%) were unlikely to have biased the results of the study.
Implications for practice
The main recommendation from our findings is that they do not support the use of brief evidence-based CBT to prevent future recurrence of bipolar disorder if the individual has already experienced a very high number of previous episodes. In such cases there was no observable additional health gain over usual treatment alone. A post hoc analysis suggests that CBT may be less effective in patients with very frequently recurring episodes. The corollary is that psychological therapies such as CBT may particularly benefit those with less complex mood disorders who are at an earlier stage of their illness. In our study this subgroup represented about 30% of the sample recruited and may constitute a minority of patients with bipolar disorder who are in contact with adult mental health services.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Overall, when people with recurrent and complex presentations of bipolar disorder who are usually excluded from psychological or pharmacological efficacy treatment trials were studied intensively for18 months, they were more rather than less likely to experience a major relapse.
-
▪ Adjunctive cognitive–behavioural therapy (CBT) was only of significant benefit to individuals with 12 or fewer episodes of bipolar disorder.
-
▪ If CBT is to be offered widely to people with bipolar disorder, it may be better viewed as an early option, rather than an intervention for difficult-to-treat chronic illness (as suggested in current treatment guidelines).
LIMITATIONS
-
▪ The constraints of the trial protocol reduced the options for more individualised CBT;for example, more sessions or extending CBT; for example, more sessions or extending the time to deliver the time to deliver the course of the course of therapy.
-
▪ It was more difficult to make direct comparisons between our findings and other studies because we included people in episode as well as those who were euthymic.
-
▪ As with many trials, only about one in five of those using the clinical services were eligible and gave written informed consent to participate.
Acknowledgements
This study was supported by a grant from the Medical Research Council in the UK.
We acknowledge the commitment and input of all the other members of the multicentre trial of CBT for Bipolar Disorders (MCTBP) research team: Michaela Rodger, Yvonne Potts, Bernadette O'Reilly, Talia Gutenstein, Kim Bowen Jones, Chris Healey, Paul Hammersley, Helen Morey, Mark Christie, John Davies, Gillian Todd, Sandra Secher and Carolyn Crane.We also thank staff at the Biostatistics Office at the Christie Hospital in Manchester. We particularly acknowledge the patients who participated in the trial.









eLetters
No eLetters have been published for this article.