Depression is a common illness that can severely affect people's quality of life (Malhi Reference Malhi and Mann2018) and it is expected to be the leading cause of burden of disease worldwide by 2030 (World Health Organization 2011). Despite various treatments, people can experience recurrent and difficult-to-treat episodes (Malhi Reference Malhi and Mann2018). Music therapy is one form of therapy used in depression and other mental and cognitive disorders. Previous reviews support its use, including in Parkinson's disease (Machado Sotomayor Reference Machado Sotomayor, Arufe-Giráldez and Ruíz-Rico2021), dementia (Gómez-Romero Reference Gómez-Romero, Jiménez-Palomares and Rodríguez-Mansilla2017), anxiety (Lu Reference Lu, Jia and Liang2021), schizophrenia, post-traumatic stress disorder, post-natal depression and social anxiety (Witusik 2019). Music therapy is not simply asking patients to listen to music (coined ‘music medicine’), but rather involves the cultivation of a therapeutic relationship between participant and therapist (Dileo Reference Dileo2006), as in other forms of psychological therapy. This is done using components of music (e.g. melody) with the goal of promoting physical, psychological and social well-being (Dileo Reference Dileo2006).
This commentary looks at the Cochrane Review (Aalbers Reference Aalbers, Fusar-Poli and Freeman2017) in this issue's Cochrane Corner, which synthesised evidence on music therapy for depression.
The Cochrane Review
Summary
The review cited the World Federation of Music Therapy's definition of the intervention (Box 1) and split the four types into two groups: receptive (listening to music) and active forms (‘making’ music). The review's inclusion criteria identified ‘well-defined’ music therapy using criteria that appeared to follow from the definition (Box 1) and background literature, but they were not explicit in their formulation.
BOX 1 What is music therapy?
The World Federation of Music Therapy defines music therapy as ‘the professional use of music and its elements as an intervention in medical, educational, and everyday environments with individuals, groups, families, or communities who seek to optimize their quality of life and improve their physical, social, communicative, emotional, intellectual, and spiritual health and wellbeing’ (World Federation of Music Therapy Reference Witusik and Pietras2023).
There are four main types of music therapy/method (Bruscia Reference Bruscia2013):
• receptive (listening)
• composition
• improvisation
• re-creative (or performance).
The Cochrane Review outlined the following criteria to identify ‘well-defined’ music therapy (Aalbers Reference Aalbers, Fusar-Poli and Freeman2017). Music therapy had to:
• include sessions with a structured therapeutic framework
• involve a musical interaction between therapist and participant or between therapist and a group of participants
• aim to improve health
• have a main therapeutic change agent that could be described as music, the relationship or reflections induced by the music.
The evidence base for music therapy has only more recently been systematically examined. This may be due to the difficulty in defining music therapy because of its heterogeneity, as it is shaped by its cultural context (Bruscia Reference Bruscia2013) and has been developed from different therapies (e.g. behavioural and psychoanalytical models) (Scovel Reference Scovel and Gardstrom2012). Previous reviews (Van Assche Reference Van Assche, De Backer and Vermote2015; Zhao Reference Zhao, Bai and Bo2016) indicate its potential to improve depression. However, of the two earlier reviews, one did not perform a meta-analysis (Van Assche Reference Van Assche, De Backer and Vermote2015) and the other focused on older adults (Zhao Reference Zhao, Bai and Bo2016). Aalbers et al's (Reference Aalbers, Fusar-Poli and Freeman2017) Cochrane Review aimed to include unexamined newer trials and perform a meta-analysis on populations of all ages, comparing:
(a) music therapy plus ‘treatment as usual’ (TAU) versus TAU
(b) music therapy versus psychological therapy
(c) active versus receptive music therapy.
The review examined randomised controlled trials (RCTs) or clinical controlled trials (CCTs) (Box 2) and used standardised mean differences (s.m.d.) for continuous outcomes measured on different scales (Box 3) with their confidence intervals (95% CI) (Box 4).
BOX 2 What are clinical controlled trials?
A clinical controlled trial (CCT) is a controlled trial (i.e. a trial with a control arm) in which randomisation to the arms of the trial is not made clear or where there is quasi-randomisation (not pure randomisation), for example where the assignment method is alternation or date of birth.
(Higgins Reference Higgins, Thomas and Chandler2023)BOX 3 Standardised mean difference
The standardised mean difference (s.m.d.) is:
• a summary statistic (it summarises a set of observations) in meta-analysis
• used when studies assess the same outcome but measure it in different ways (e.g. depression by different tools/scales)
• used because you need to convert results of different studies with different scales to the same scale before they can be combined.
It is calculated as the intervention effect (difference in mean outcome between groups) in the study, divided by the between-participant variability in the study (i.e. the standard deviation of outcome among participants):
BOX 4 95% confidence intervals: what do they tell us?
It is important to have not only measures of an effect, translated into effect sizes (e.g. s.m.d.), but also measures of how precise the estimate of that effect is (this is the 95% confidence interval). In other words, how sure can you be that the true effect of music therapy is around the estimated effect given in the Cochrane Review? The 95% confidence interval gives you this information, giving you a range of values in which you can expect the true effect to lie 95% of the time.
The review found that music therapy plus TAU appears to be more effective than TAU alone in reducing depressive symptoms and comorbid anxiety and improving functioning in the short term (up to 3 months). More studies are needed examining longer-term outcomes. It was not clear whether music therapy was better than psychological therapy or whether one form of music therapy was better than another.
Method
The review outlined two objectives: (a) to assess the effects of music therapy for depression in people of any age compared with TAU and psychological, pharmacological and/or other therapies; and (b) to compare the effects of different forms of music therapy for depression in people of any age.
The review outlined five comparisons (music therapy versus TAU; music therapy plus TAU versus TAU alone; music therapy versus psychological therapies; music therapy versus pharmacological therapies; and one form of music therapy versus another form), which slightly differed from the two objectives in, for example, including a music therapy plus TAU versus TAU comparison. The review made three comparisons: comparison 1, music therapy plus TAU versus TAU alone; comparison 2, music therapy versus psychological therapy; comparison 3, active versus receptive music therapy (no studies compared music therapy versus TAU or music therapy versus pharmacological therapies). With no comparisons outlined in a protocol, this could be a source of reporting bias, whereby what is reported is decided on post hoc (after the analysis).
The review authors clearly outlined the population, intervention (music therapy), primary outcomes (depressive symptoms and adverse events) and secondary outcomes (functioning, quality of life (QoL), leaving the study early, anxiety, self-esteem, cost/cost-effectiveness and satisfaction with treatment).
The review limited the studies to RCTs and CCTs, but did not give a rationale. This limiting is appropriate, however, because the review examined one intervention and there were a limited number of RCTs.
The review authors conducted a thorough search of the literature, searching the Cochrane Common Mental Disorders Group's specialised register of RCTs for mental disorders, in addition to databases, clinical trial registers, dissertations/theses, grey literature and references, and contacting trial authors and subject experts. The review was published in November 2017, and searches were conducted between May and September 2016. Confusingly, they ran a pre-publication update search in August 2017, identifying three more studies, but did not include these in their analysis and did not provide a rationale for this – a clear source of potential bias. They also did not include two studies identified from their initial search, owing to insufficient information on study design, intervention and analysis, again a potential source of bias.
They assessed risk of bias in included studies using the Cochrane Handbook for Systematic Reviews of Interventions criteria (Higgins Reference Higgins and Green2015) and assessed the overall quality of evidence using the GRADE approach (Schünemann Reference Schünemann, Broz˙ek and Guyatt2013: Chapter 5.2).
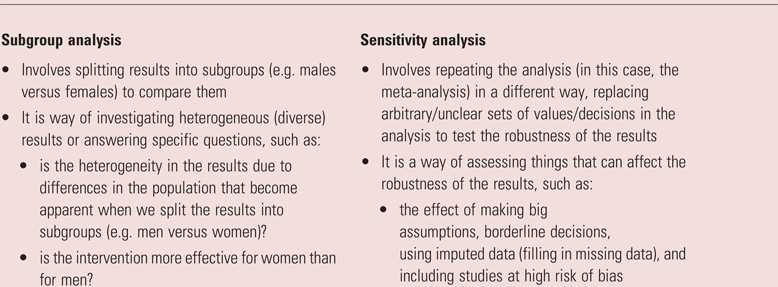
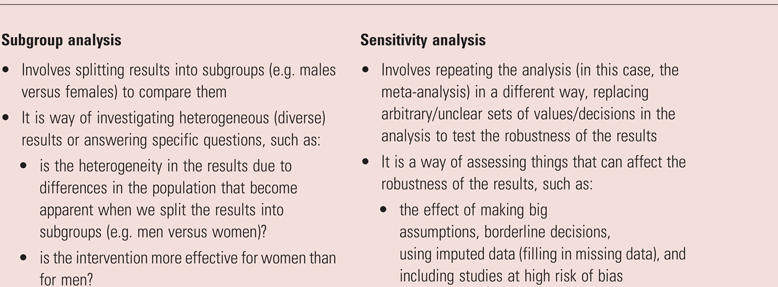
They performed a meta-analysis using a random-effects model, which is appropriate owing to the expected heterogeneity in music therapy. They planned to explore heterogeneity by examining subgroups (subgroup analysis) (Box 5) according to participant characteristics, duration of therapy, modality of therapy and type of therapy. They also planned to undertake a sensitivity analysis (Box 5), repeating the analysis after excluding studies at high risk of bias.
Results
Nine studies were included, with a total of 421 participants, 411 of whom were included in the meta-analysis. They did not explain this discrepancy (a potential source of bias).
Comparison 1: music therapy plus TAU versus TAU alone
Four studies examined clinician-rated short-term depressive symptoms (up to 3 months) and found significant symptom reduction in the music therapy plus TAU group (s.m.d. = −0.98; 95% CI −1.69 to −0.27; high heterogeneity I 2 = 83%; moderate-quality evidence). One study examined clinician-rated depressive symptoms in the medium term (up to 6 months) and found no significant difference. Four studies looked at patient-reported short-term depressive symptoms and found a significant reduction in the music therapy plus TAU group (s.m.d. = −0.85, 95% CI −1.37 to −0.34,; moderate heterogeneity I 2 = 49%; moderate-quality evidence). A significant reduction in anxiety and improvement in functioning was found in the short term (music therapy plus TAU group), but not in the long term. One RCT looked at adverse events and found no significant difference. No significant difference was found for self-esteem (one study), QoL (one study) or leaving the study early. No studies looked at cost/cost-effectiveness or satisfaction with treatment.
Comparison 2: music therapy versus psychological therapy
One RCT looked at clinician-rated and four RCTs at patient-reported depressive symptoms and found no significant differences in the short/medium term. No significant differences were found in QoL (one study) or in leaving the study early. There were no data on adverse events, self-esteem, functioning, anxiety, cost-effectiveness or satisfaction with treatment.
Comparison 3: active versus receptive music therapy
One RCT looked at clinician-rated and patient-reported depressive symptoms and found no significant difference in the short/medium term. There was no difference found in QoL or leaving the study early. There were no data on adverse events, functioning, anxiety, self-esteem, cost/cost-effectiveness or satisfaction with treatment.
Duration of outcome evaluation
Significant findings in shorter-term outcomes but not medium-term outcomes may be a reflection of the paucity of studies examining medium-term outcomes rather than a true pattern of effect. Only one RCT compared music therapy plus TAU versus TAU alone in the medium term, finding a non-significant result favouring music therapy plus TAU. Similarly, only one study looked at medium-term outcomes comparing music therapy versus psychological therapy and active versus receptive music therapy.
Subgroup analyses
The review authors did not examine heterogeneity based on predefined subgroups. They examined duration of treatment but not as planned, examining months of music therapy (short: <3 months; medium: 3–6 months; and long term: >6 months). Researchers cannot always follow planned review protocols (e.g. owing to the limited number of studies found), but they should have made this explicit.
Sensitivity analyses
The sensitivity analyses, in which studies with high risk of bias were removed, did not change the results.
Clinical significance of the findings
The review used guidelines for behavioural science interventions to translate findings into meaningful outcomes, where effects sizes (s.m.d.) up to 0.2 are considered ‘small’, those around 0.5 are ‘medium’ and those at 0.8 and above are ‘large’ (Cohen Reference Cohen1988). An effect size is meaningful if it translates to a clinically meaningful difference (Ranganathan Reference Ranganathan, Pramesh and Buyse2015), for example in the review an s.m.d. of −0.98 was a ‘large’ effect size, translating to a difference of 9.8 points on the Hamilton Rating Scale for Depression – something clinicians may better relate to. The review authors felt this was a clinically significant difference; however, clinical significance is open to interpretation, as it requires the consideration of clinically important factors such as cost-effectiveness and treatment acceptability (Ranganathan Reference Ranganathan, Pramesh and Buyse2015).
Discussion
The review concluded that music therapy plus TAU may be more effective than TAU alone in reducing depressive symptoms and anxiety and improving functioning, as evidenced by large effect sizes (translating to clinically meaningful differences) and moderate-quality evidence; however, there needs to be more evidence examining longer-term outcomes, adverse effects and patient-driven outcomes (e.g. functioning). We need to consider sources of heterogeneity and how this affects our interpretation. Depression was a comorbid diagnosis alongside substance misuse or anxiety in some studies and one study included some participants with a history of bipolar disorder. This heterogeneity makes the results translatable to more patients, although simultaneously less certain in the treatment effect specific to a particular patient (Box 6).
BOX 6 Generalisability versus specificity
There is a tension between the generalisability and specificity (and thus precision) of your results. On the one side, having a study with a heterogeneous population (people with very different characteristics) will make the results more generalisable (more applicable to a larger number of patients); however, it may muddy the waters in understanding the effect for a specific patient with specific characteristics. For example, music therapy may not work so well for people with depression and comorbid substance misuse. Examining diverse populations together does not allow you to identify potential differences in how well music therapy works for different patient groups. This makes you less certain about the precision of the estimate of the effect (how close the result is to the true value) for a specific patient.
Since this Cochrane Review, another review and meta-analysis of 55 RCTs (Tang Reference Tang, Huang and Zhou2020) has been published examining music-based interventions (music therapy and ‘music medicine’) in depression. In keeping with the Cochrane Review, it found that music therapy significantly reduced depressive symptoms (s.m.d. = −0.66; 95% CI −0.86 to −0.46; P < 0.001), but this effect did not last in the long term. The authors argued that this may be due to the limited number of studies examining longer-term outcomes. Another review found that music therapy significantly improved depression in people with dementia, but this did not last after the intervention ended (Li Reference Li, Wang and Lu2019). Music therapy appeared beneficial in a pilot study of adolescents with depression, but again this did not last after the intervention ended (Geipel Reference Geipel, Koenig and Hillecke2022). Music therapy requires a trained music therapist. Even if funds and evidence were available to support music therapy in the long term, having the trained personnel may limit its implementation. Currently, it is challenging to argue for its implementation from a policy and practice perspective, without more evidence on longer-term outcomes and cost.
Conclusions
This Cochrane Review did well to attempt to synthesise the evidence on something that is challenging to define and heterogeneous (music therapy), but it would benefit from including the updated studies identified – its key limitation. Nevertheless, the review is important, owing to the need to bring evidence-based medicine to music therapy, a therapy that has been used for years to treat a variety of psychiatric conditions.
Data availability
Data availability is not applicable to this article as no new data were created or analysed in this study.
Acknowledgement
I would like to thank Dr Riccardo De Giorgi for providing feedback on this manuscript.
Funding
Dr Tessa Lomax has been funded to undertake this research by the National Institute for Health and Care Research (NIHR); NIHR Award number: ACF-2021-13-010.
Declaration of interest
None.




eLetters
No eLetters have been published for this article.