Introduction
There has been a steady increase in emergency department (ED) visits and resource use by adults over 65 years of age.Reference Pines, Mullins and Cooper 1 About 20% of current ED patients are geriatric, and that proportion is expected to increase substantially.Reference Woford, Schwartz and Timerding 2 In fact, the geriatric demographic is the only age cohort with increasing ED visit rates in Canada.Reference Benjamin, Schull and Schultz 3 Most clinicians indicate that older patients are among the most complex, time- and resource-intensive of all ED patients.Reference Strange and Chen 4 - Reference Gray, Peel and Costa 6
In an environment that increasingly incentivizes flow and rapid management, emergency physicians (EPs) are required to rapidly assess older patients who can have atypical presentations of disease, cognitive impairment or multiple other chronic conditions, be on multiple medications, and have either inadequate social supports or multiple community-care providers.Reference Strange and Chen 4 - Reference Carpenter and Platts-Mills 7 Older patients are more likely to experience adverse events in the ED,Reference Liu, Thomas and Gordon 8 including iatrogenic injury,Reference Fakih, Shemes and Pena 9 missed diagnoses,Reference Sanders and Morley 10 omitted treatments,Reference Krumholz, Radford and Wang 11 - Reference Rathore, Mehta and Wang 13 poor medical outcomes,Reference Denman, Ettinger and Zarkin 14 , Reference Friedmann, Jin and Karrison 15 death,Reference McCusker, Bellavance and Cardin 16 functional decline,Reference Chin, Jin and Karrison 17 - Reference McCusker, Bellavance and Cardin 19 prolonged stays,Reference McCusker, Bellavance and Cardin 16 necessity for a discharge to a higher level of care,Reference McCusker, Bellavance and Cardin 20 and repeat ED use.Reference Caplan, Brown and Croker 21 , Reference McCusker, Cardin and Bellavance 22 A 1992 American study reported that EPs found it challenging to provide consistently high-quality care for older patients.Reference McNamara, Rousseau and Sanders 23 Improving the balance between rapid flow and optimal outcomes in the geriatric population may require both readjustment of the model of care for older adultsReference Carpenter and Platts-Mills 7 and disruptive innovation—beginning with geriatric emergency medicine education.Reference Hwang, Shah and Han 24
It is expected that EPs develop the ability to care for older patients during undergraduate medical education (UGME) and postgraduate medical education (PGME). However, evidence suggests that current EM training relating to the care of the elderly may not provide adequate preparation for the “Silver Boom” about to hit our EDs.Reference McNamara, Rousseau and Sanders 23 , Reference Carpenter, Lewis and Caterino 25 This training gap has been recognized in the United States, where both the Institute of Medicine 26 and the American College of Emergency Physicians 27 have called for improved geriatric EM training.
In 2011, Biese et al. found that geriatric educational curricula for EM residents may positively affect knowledge base and appropriate decision-making, and may place elderly patients at less risk of adverse outcomes in the ED.Reference Biese, Roberts and LaMantia 28 In 2010, Hogan et al. established a set of eight core geriatric EM competency domains using a consensus-based approach.Reference Hogan, Losman and Carpenter 29 These represent a minimum set of behaviourally based performance standards that arguably all EM residents should be able to demonstrate by completion of their residency training.
Our primary objective was to determine whether graduating Canadian postgraduate year (PGY)-5 residents are comfortable with the above-mentioned geriatric EM competency domains. Our secondary objectives were to assess whether Canadian EM residents become more comfortable through the course of their residency, and whether a relationship exists between geriatric educational exposures and resident comfort with geriatric EM. We hypothesized that the majority of graduating Canadian EM residents would not report being comfortable with all of the core geriatric EM competency domains.
Methods
Study design
This was a national cross-sectional study of Canadian Royal College EM PGY-1 and PGY-5 residents. We evaluated resident self-reported comfort with the eight previously reported geriatric EM competency domains (Figure 1). In order to limit non-response, coverage, sampling, and measurement error, we used Dillman’s tailored design method guidelinesReference Dillman, Christian and Smyth 30 to develop an eight-question online survey tool (Appendix 1). We pilot tested the survey on five PGY-3 residents and two medical students to ensure clarity, face validity, and content validity. We deemed that a peer-reviewed pre-study of the internal and external validity and reproducibility of our survey tool was unnecessary, owing to our adherence to established survey creation guidelines,Reference Dillman, Christian and Smyth 30 internal pilot testing, and ease of access to, and high expected response rate from, our study population. We incentivized participation with a $10 gift certificate provided to residents who completed the survey through an anonymous link. The study was approved by the Mount Sinai Hospital Research Ethics Board in Toronto, Ontario.
Figure 1 Geriatric competency domains for EM residents.Reference Hogan, Losman and Carpenter 29
Study settings and participants
An anonymous survey was distributed in June 2014 to the program directors of the 14 Canadian Royal College EM residency training programs who then forwarded it to the incoming PGY-1 cohort (in July) and the graduating PGY-5 cohort (in June). This timing allowed access to incoming residents in the first month of their postgraduate training and outgoing residents in their last month. All Canadian PGY-1 residents and PGY-5 residents were eligible to participate. The potential sample included 141 residents from across Canada: 77 PGY-1 residents 31 and 64 PGY-5 residents. 32
Variables
Each survey question contained a completely described, common geriatric ED scenario linked to one of the eight domains of geriatric EM competence followed by the specific core competencies associated with that domain. The questions were closed-ended with naturally ordered responses. The survey asked residents to rank their comfort level in providing competent care with respect to each scenario on a seven-point Likert scale. The scale options were “Very Uncomfortable,” “Uncomfortable,” “Somewhat Uncomfortable,” “Neither Comfortable nor Uncomfortable,” “Somewhat Comfortable,” “Comfortable,” or “Very Comfortable.”
We also assessed the types of geriatric education that the residents experienced during training (UGME or PGME). The types of geriatric EM training exposures are described in Appendix 2. Our primary outcome was the proportion of “comfort” for each geriatric EM competency domain, and we established, a priori, that “comfort” in any domain would be attributed to “Comfortable” or “Very Comfortable” responses. Our secondary outcome was the number of geriatric EM competency domains scored as “Comfortable” or “Very Comfortable.” Independent variables captured included the PGY as well as the type and number of different geriatric EM exposures per PGY. We did not collect data on standard demographics to maintain the anonymity of participants from smaller residency programs.
Data analysis
Stratified analyses were used to investigate the prevalence of self-reported comfort in geriatric EM competencies by PGY. Ninety-five percent confidence intervals for prevalence statistics were based on the binomial estimation of the standard error of a proportion. Because this was a population level survey, these confidence limits mainly show the presumed representativeness of the proportions across resident EM cohorts. The chi-square test was used to examine the relationship between comfort in geriatric EM competency domains and the variation in geriatric educational exposures, and p less than or equal to 0.05 was considered statistically significant. All analyses were performed using SAS version 9.2 for Windows (SAS Institute, Inc., Cary, NC). The results of this study were reported according to the STROBE statement.Reference von Elm, Altman and Egger 33
Results
Of the 141 eligible residents from across Canada, 77% (109) participated: 88% (68) of PGY-1 residents and 64% (41) of PGY-5 residents. All Canadian EM residency training programs were represented in the responses. The response rate for individual programs ranged from 20% to 94%.
The proportion of residents who reported being comfortable with each competency domain by PGY is shown in Figure 2. Among PGY-5 residents, between 68% and 88% (28–36) reported being comfortable in each geriatric EM competency domain. Although variation was seen, no statistically significant difference was found in PGY-5 comfort between the eight geriatric EM competency domains. Among PGY-1 residents, between 6% and 25% (4–19) reported being comfortable in each domain. With the exception of the domain of “Emergency Intervention Modifications,” no significant difference was found in PGY-1 comfort between the geriatric EM competency domains. PGY-5 EM residents were found to be significantly more comfortable relative to PGY-1 residents across all eight geriatric EM competency domains (p<0.05).
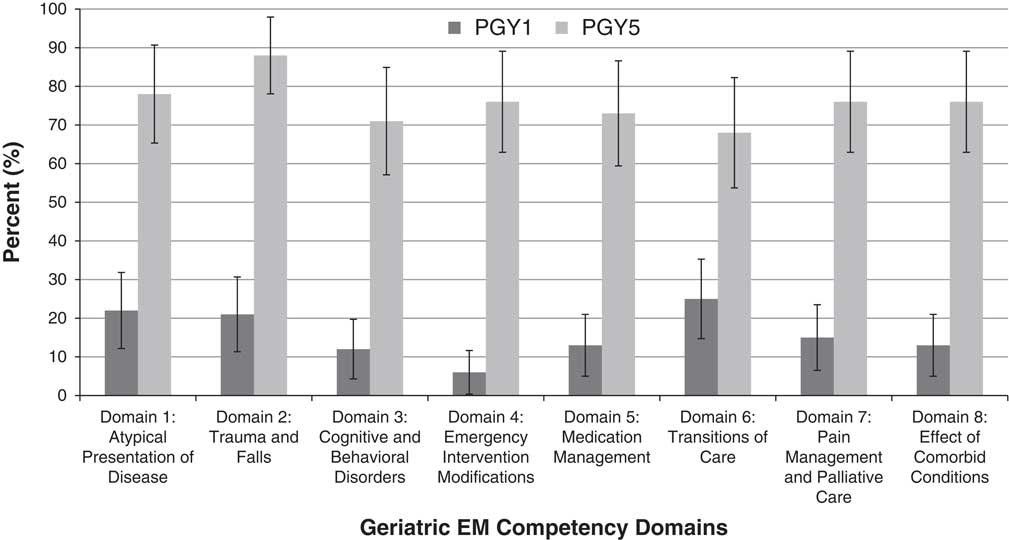
Figure 2 Proportion of residents reporting comfort for each geriatric EM competency domain, by postgraduate year.
Figure 3 illustrates the number of competencies in which PGY-1 and PGY-5 residents reported being comfortable. We found that 34% (14) of PGY-5 residents and 0% of PGY-1 residents reported comfort with all eight domains (p<0.05). Fifty percent of PGY-1 residents and 2% of PGY-5 residents reported being “Very Uncomfortable” with all eight domains (p<0.05).
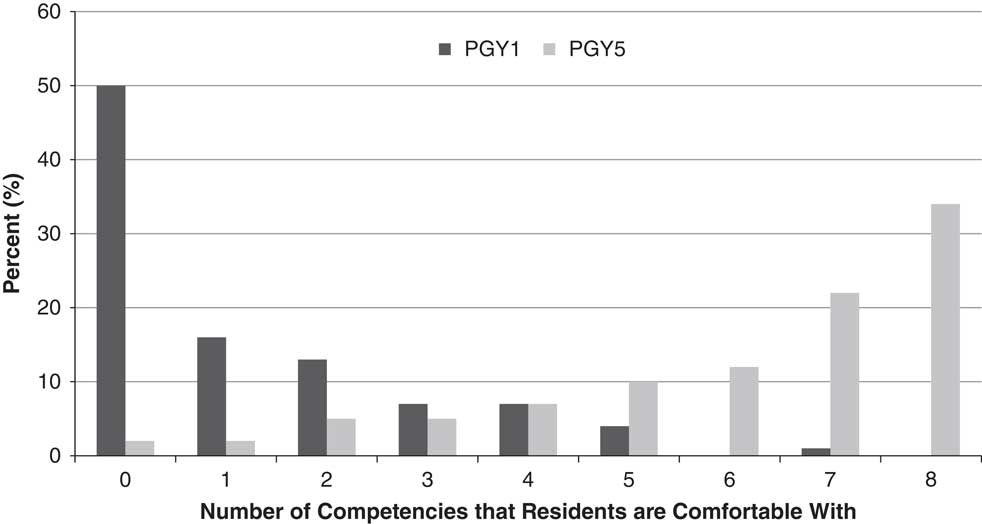
Figure 3 Number of competencies that residents reported being comfortable with, by postgraduate year.
Figure 4 illustrates the types of geriatric-specific educational exposures reported. Residents reported a highly variable range of geriatric educational exposures obtained during training. On average, PGY-5 residents reported experiencing seven different geriatric EM exposures during PGME (with a range of one and twelve exposures). The majority (>50%) of PGY-5 residents had some geriatric-specific educational exposure through clinical teaching, lectures, rounds, oral exams, directed readings, and journal clubs. Less than 20% of PGY-5 residents reported that they had exposure to geriatric-specific rotations, courses, research, premed training, problem-based learning, and assignments during PGME. On average, PGY-1 residents had experienced six different geriatric EM exposures during UGME (with a range of 1 and 10 exposures). The majority of PGY-1 residents reported that they had some exposure to clinical teaching, lectures, problem-based learning, rounds, and directed learning related to geriatrics. We found no relationship between resident comfort with geriatric EM competency domains and the nature or number of geriatric educational exposures that the residents had previously received.
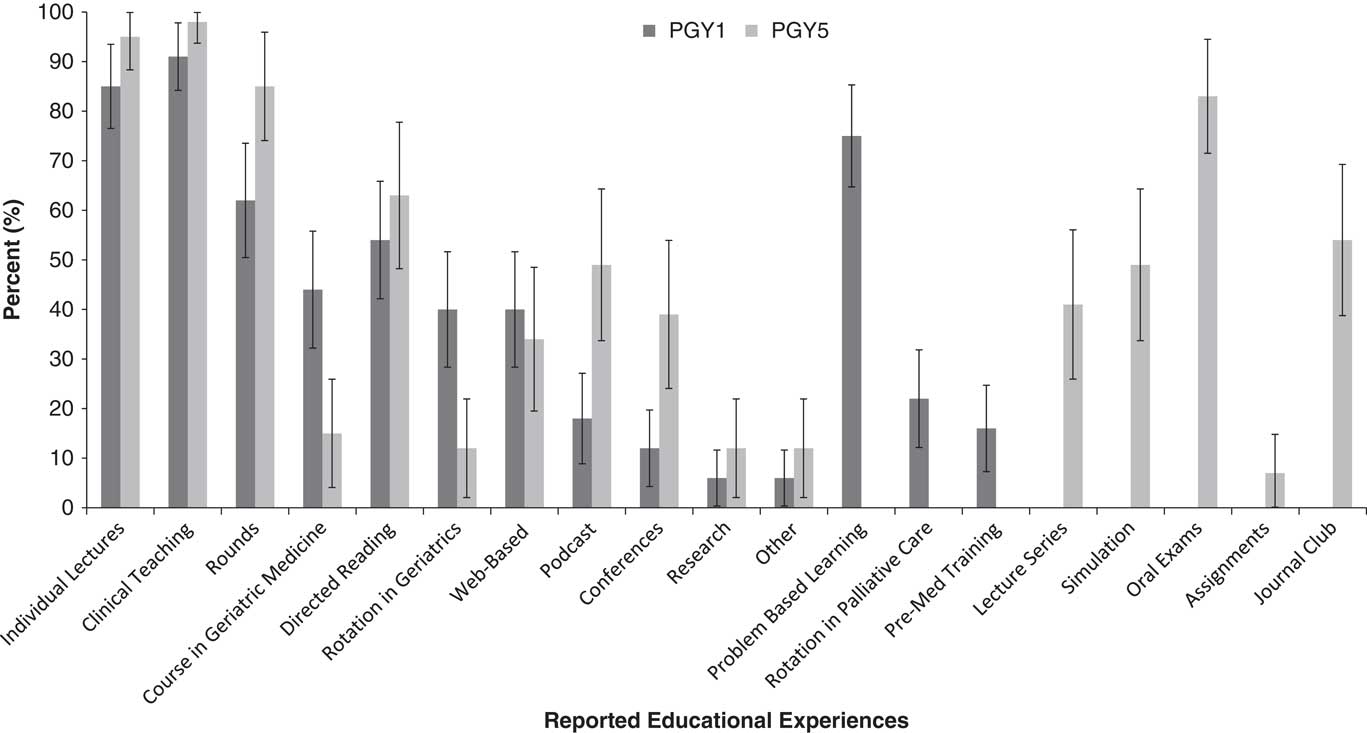
Figure 4 Reported geriatric educational exposures, by postgraduate year.
Discussion
To our knowledge, this is the first study to investigate EM residents’ comfort with geriatric ED care both at the beginning and end of their training, and the educational experiences that they receive in this area.
Our findings suggest that comfort level with the core domains of caring for older ED patients does increase dramatically throughout the 5 years of residency training. However, we also found that in the month immediately before completing their training, only 34% of Canadian EM residents report feeling comfortable in all domains of geriatric EM, and, for any given domain only, 68%–88% of residents felt comfortable. These findings can be interpreted from either a “glass half full” or “glass half empty” perspective. However, we doubt that it would be considered acceptable if only one-third of graduating EM residents reported feeling comfortable with, for example, the core competency domains of pediatrics, trauma, or resuscitation. Our findings suggest that current Royal College EM residency training in Canada may not adequately be preparing graduates to be comfortable with defined competencies for the care of older ED patients, and by extension may not adequately be preparing future EPs to provide care to the geriatric EM population. It is conceivable that this finding may be generalizable both to other specialties and to other countries regarding their preparation of future physicians for upcoming demographic shifts in EM presentations.
Fifty percent of residents in their first month of postgraduate training said that they are not comfortable with any geriatric EM competency domains. We acknowledge that early residency is a period marked by perceived inadequacy and uncertainty about competence. Nonetheless, we would be surprised if the same lack of comfort were expressed about other areas of standard EM care, including trauma, resuscitation, procedural skills, and critical illness.
We found that medical students and residents are exposed to a variable range of geriatric EM experiences. We also found no relationship between the nature or number of different educational exposures that residents reported and their reported comfort with the core geriatric competencies. This lack of correlation may be explained by inadequacies of our surveying technique or by inadequacies in the educational content of experiences that may do little to change skills, knowledge, or attitudes with regards to geriatric EM. Currently, there is no standard geriatric EM training across Canada, and thus the skills that a new EP has with respect to geriatric EM will vary. Section 2.3 of the Royal College of Physicians and Surgeons of Canada, “Objectives of Training in Emergency Medicine,” specifically notes that geriatric EM care is an area in which residents must be competent. 34 However, despite the high proportion of complex geriatric patients in EDs, the Royal College “Minimum Training Requirements for Specialty Training in Emergency Medicine” do not stipulate a specific rotation in geriatrics, whereas, in contrast, they do require a minimum of 4 months with a pediatric clinical emphasis. 35 Given the lack of requirement for a specific rotation in geriatrics, it is perhaps not surprising that less than 20% of PGY-5 residents reported undertaking a rotation in geriatrics.
Because numerous studies have demonstrated deficiencies in ED care for older adultsReference Aminzadeh and Dalziel 36 , Reference Schnitker, Martin-Khan and Beattie 37 with falls,Reference Tirrell, Sri-on and Lipsitz 38 dementia,Reference Schnitker, Martin-Khan and Burkett 39 , Reference Schnitker, Martin-Khan and Burkett 40 or delirium,Reference Schnitker, Martin-Khan and Burkett 40 a concern exists that EPs—whose training is focused on the time-dependent skills in areas such as trauma, resuscitation, procedures, and critical illness—may be inadequately prepared to manage the complexity associated with providing care for the geriatric population. The management of frail elderly patients with atypical presentations, polypharmacy, and polymorbidity who are navigating transitions through a complex health care system, is often at odds with the classic “single patient/single problem” paradigm of EM training. It stands to reason that the implementation of a standard geriatric EM curriculum or addition of curricular expectations across all Canadian EM programs may produce a cohort of EPs that is more consistently comfortable with care of elderly patients. Strategies may include focused geriatric EM rotations, online modules, or supplementary rotations in relevant fields such as palliative medicine, acute geriatric medicine, and community-based geriatric clinics. Our results show that such educational strategies are rarely employed in Canada. As EM moves towards a competency-based education model, it will be important to identify competent care of the older ED patient as an “entrustable professional activity” with clear milestones and benchmarks identified for EM residents progressing through residency.Reference ten Cate 41
We acknowledge that it is difficult for PGME programs to find time and resources to expand resident curricula, and there are many topics to cover for a generalist specialty such as EM. The introduction of a self-directed online competency-based approach may address the problem of limited time and resources. This method is already in place at one Canadian postgraduate site, using a flipped classroom approach through the website, www.geri-em.com.
Limitations
The ideal study design to assess resident ability to care for older adults would be direct observation and assessment of resident competence in caring for older patients. In the absence of that ideal, we assessed a possible surrogate for competence, that is, residents self-reported level of comfort with each of the eight competency domains of geriatric EM. We chose this approach as a first step knowing that, while the education literature suggests that self-assessment of competence is unreliable, self-assessment of comfort is intrinsically accurate.Reference Eva and Regehr 42 , Reference Brian and Hodges 43 We posited that there is a connection between self-perceived comfort with an activity and actual competence with that activity. The survey tool used in the study was original and was designed for our specific purpose and thus lacks criterion validity (there are no current measures of resident comfort or ability to test our survey against). Our survey did not provide information about the quality of educational exposures, only the number and nature of different exposures. As a result, a 1-hour lecture in medical school and a full clinical rotation in residency would both count as one experience. This study was limited to the Royal College EM residency program and did not include the EM residents in the College of Family Physicians of Canada CCFP(EM) program. Finally, the demographic characteristics of neither the sample population nor the nonparticipants were collected and the survey was available in English only.
Conclusions
Our data show that one-third of graduating Canadian Royal College EM residents are comfortable with all core competency domains of care of older persons in the ED. Canadian EM residents are exposed to a variable range of geriatric EM exposures across. However, current EM residency training in Canada may not be preparing practitioners adequately to provide competent care for older patients. The addition of focused geriatric EM content may improve resident comfort with geriatric EM competencies.
Acknowledgements: The authors gratefully acknowledge the generous support of their clinical and research emergency department colleagues who made this study possible. TS and DM led recruitment in consultation with all of the listed authors. APC led the analysis in consultation with all of the listed authors. TS led the manuscript. All authors contributed to the final manuscript and approved its content.
Competing interests: Funding sources and disclosures - Support for this project was provided by the Penny Rubinoff Fellowship Fund in Geriatric Emergency Medicine and the Schwartz/Reisman Emergency Medicine Institute. The opinions and conclusions expressed in this article are those of the authors and do not necessarily reflect the views of the contributing centers or funders.
Supplementary Material
To view supplementary material for this article, please visit http://dx.doi.org/10.1017/cem.2016.27






