To the Editor:
A recently published study found a 96.2% prevalence rate for significant posttraumatic stress symptoms in quarantined patients diagnosed with COVID-19 (Bo et al., Reference Bo, Li, Yang, Wang, Zhang, Cheung and Xiang2020). In addition, various psychiatric disorders have been found in patients in the early stages of the COVID-19 outbreak (Talevi et al., Reference Talevi, Socci, Carai, Carnaghi, Faleri, Trebbi and Pacitti2020). Thereby, the rates for posttraumatic stress disorder (PTSD) in COVID-19 affected patients appear higher when compared to PTSD rates in the general population or in emergency service staff after terrorist attacks (11% to 25%; Berninger et al. Reference Berninger, Webber, Niles, Gustave, Lee, Cohen and Prezant2010; Brackbill, Hadler, DiGrande, Ekenga, & Farfel, Reference Brackbill, Hadler, DiGrande, Ekenga, Farfel, Friedman and Thorpe2009; Schlenger et al. Reference Schlenger, Caddell, Ebert, Jordan, Rourke, Wilson and Kulka2002; Wesemann et al., Reference Wesemann, Zimmermann, Mahnke, Butler, Polk and Willmund2018b; Wesemann, Mahnke, Polk, & Willmund, Reference Wesemann, Mahnke, Polk and Willmund2020). In addition, the rates established by Bo et al. were significantly higher than those in previous studies by Fang, Zhe, and Shuran (Reference Fang, Zhe and Shuran2004) or Mak, Chu, Pan, Yiu, and Chan (Reference Mak, Chu, Pan, Yiu and Chan2009) on patients with the Severe Acute Respiratory Syndrome (SARS).
The aim of this study was to determine the prevalence of ‘general stress’ and severe posttraumatic stress in patients who were hospitalized with the initial suspect of a COVID-19 infection. The suspicion of COVID-19 was considered a critical event for mental health, since the vast majority of the patients also had comorbidities that were known to translate in a worse outcome together with a COVID-19 infection (Clark et al., Reference Clark, Jit, Warren-Gash, Guthrie, Wang and Mercer2020). The second goal was to compare patients with and without definitive confirmation of a COVID-19 diagnosis for general stress and posttraumatic stress. Our hypothesis was that there was no difference in patients with and without COVID-19, since we assumed that risk perception was the same in both groups. All patients with suspect of a COVID-19 infection who were admitted to the University Hospital of Essen between 8 March and 26 May were encouraged to participate in the study. After hospital admission, they were provided with the PTSD Checklist for DSM-5 (PCL-5; Weathers et al., Reference Weathers, Litz, Keane, Palmieri, Marx and Schnurr2013) and the Patient Health Questionnaire (PHQ) stress module (Löwe, Spitzer, Zipfel, & Herzog, Reference Löwe, Spitzer, Zipfel and Herzog2002). At this stage, patients and treating medical staff were not aware of their COVID-19 infection status which resulted in a double-blinded design of the study. Written informed consent was given by all participants and the study was approved by the local Ethics Committee of the University of Essen Medical School (IRB number 20-9263-BO).
A total of N = 60 patients with an average age of 59 ± 17.8 years were included (n = 33, men). The diagnosis of COVID-19 was later confirmed in n = 19 (31.7%).
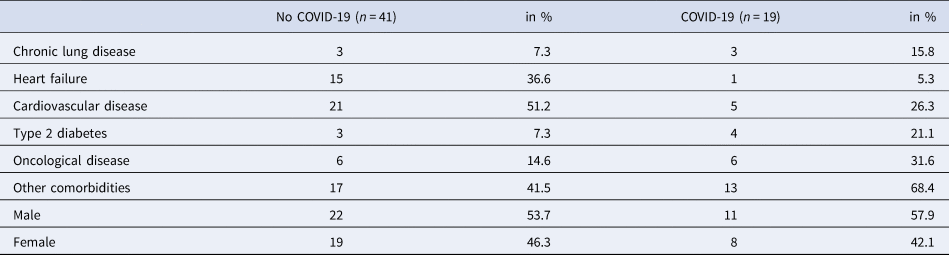
About half of the patients included presented with dyspnea, especially dry coughing, one of the leading symptoms of the SARS-CoV-2 infection (Jiang et al., Reference Jiang, Deng, Zhang, Cai, Cheung and Xia2020; Tabata et al., Reference Tabata, Imai, Kawano, Ikeda, Kodama, Miyoshi and Tamura2020). Chi-squared testing showed no sample bias between the groups with and without COVID-19. A detailed list of comorbidities is provided in Table 1.
Table 1. Descriptive statistics of comorbidities in patients with and without COVID-19
The prevalence of significant posttraumatic stress symptoms was 37.9% [95% confidence interval (CI) 35.5–40.3 in all patients and 42.1% (95% CI 37.2–47.0) in the subgroup of patients with later confirmation of a COVID-19.
The 2 × 2 chi-squared tests were performed to test the second goal: regarding patients with v. without COVID-19 there was no significant difference in the dichotomized severity of posttraumatic stress symptoms: χ2(1, N = 58) = 0.21, p = 0.647. Accordingly, there were no significant correlations between the groups with or without COVID-19 and the PCL-5 scales. However, there was a significant correlation (r = 0.35; p = 0.019) between the diagnosis of COVID-19 and stress of the PHQ stress module. In a subsequent chi-squared test with the dichotomized values, there was a significant difference between the groups: χ2(1, N = 50) = 5.56; p = 0.018 with more patients with COVID-19 in the high general stress group.
We could not replicate the findings of Bo et al. (Reference Bo, Li, Yang, Wang, Zhang, Cheung and Xiang2020) with prevalence rates of ‘significant posttraumatic stress symptoms’ far above 90%. Nevertheless, our established prevalence rates are still high when compared to other studies (Berninger et al., Reference Berninger, Webber, Niles, Gustave, Lee, Cohen and Prezant2010; Brackbill et al., Reference Brackbill, Hadler, DiGrande, Ekenga, Farfel, Friedman and Thorpe2009; Schlenger et al., Reference Schlenger, Caddell, Ebert, Jordan, Rourke, Wilson and Kulka2002). This can be partly explained by the high-risk population examined in our study. Chronic lung diseases, severe cardiovascular diseases or oncological diseases in combination with suspected COVID-19 may have had a negative impact on the severity of PTSD symptoms in our patients.
These results clearly support the hypothesis that patients with COVID-19 develop a higher level of general stress compared to patients without COVID-19. In this case, stress would not only be a psychological factor, but could also have an organic correlate. It is also conceivable that the high level of stress in patients with COVID-19 could be a predictor of the later onset of posttraumatic stress symptoms after the diagnosis has been received.
Routine screening for mental fitness in this high-risk population is recommended, as is the case in the military (Peterson, Park, & Castro, Reference Peterson, Park and Castro2011; Wesemann et al., Reference Wesemann, Willmund, Ungerer, Kreim, Zimmermann, Bühler and Kowalski2018a).
The influence of COVID-19 on general and posttraumatic stress should receive a special focus and might be adapted to diseases with a similar pandemic character.
Acknowledgements
We would like to thank the hospital staff that was involved in data collection for the present study.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
None.




