Research suggesting that disgust has a role in psychiatric illness has emerged (Reference Phillips, Senior and FahyPhillips et al, 1998). Although a well-developed theory of disgust exists in the literature (Reference Rozin and FallonRozin & Fallon, 1987), it does not indicate how extreme disgust reactions relate to psychopathology. Briefly, disgust is readily distinguished from other emotions, has robust behavioural correlates such as avoidance and distinct facial expressions, and has specific physical effects such as nausea. Disgust follows a developmental pattern whereby the aforementioned reactions are taught by caregivers, generally as a defence against oral ingestion of items considered contaminated.
At its core, disgust means ‘bad taste’. The notion that disgust might have evolved from the food rejection system is evidenced by the gagging reflex that is a characteristic response to offensive foods. This function of disgust is important, as the probability of ingesting offensive or unhealthy foods is often high. Appraisals of non-offensive foods as disgusting may emerge by their association with offensive objects. Consider the commonly held belief, ‘you are what you eat’. This phrase suggests that ingestion of offensive foods may also cause one to become offensive. Specifically, the act of eating offensive foods transfers the offensiveness of the food to the psychological self as well as the physical body. Based on appraisals that disgusting objects are debasing or demeaning, the incorporation of offensive foods may not only cause physical harm, it may also cause psychological harm.
DISGUST AND PSYCHIATRIC ILLNESS: AN UPDATE
The editorial by Phillips et al (Reference Phillips, Senior and Fahy1998) provided a convincing argument that the experience of disgust has expanded beyond a food-related emotion and may be implicated in a wide range of psychiatric conditions. The proposed role of disgust in psychiatric illness was largely based on inferences from other lines of research (e.g. subtypes of obsessive–compulsive disorder), the biological and neurological manifestations of disgust (e.g. impaired recognition of disgust in patients with Huntington's disease), intuitive speculation (the physiological response of people with blood phobia is similar to the perception of disgust) and clinical observations (e.g. people with eating disorders experience disgust with respect to their bodies).
Since that editorial there has been a steady stream of papers examining the role of disgust in psychiatric conditions. We conducted a literature search on PsycINFO for articles with the term disgust appearing in the title and the term disorder appearing anywhere in the subject field; the results indicate that interest in disgust as it relates to psychiatric illness is on the rise (Fig. 1). The increase in the appreciation of disgust in clinical conditions may be partially due to the understanding that there is variability in people's disgust reactions.
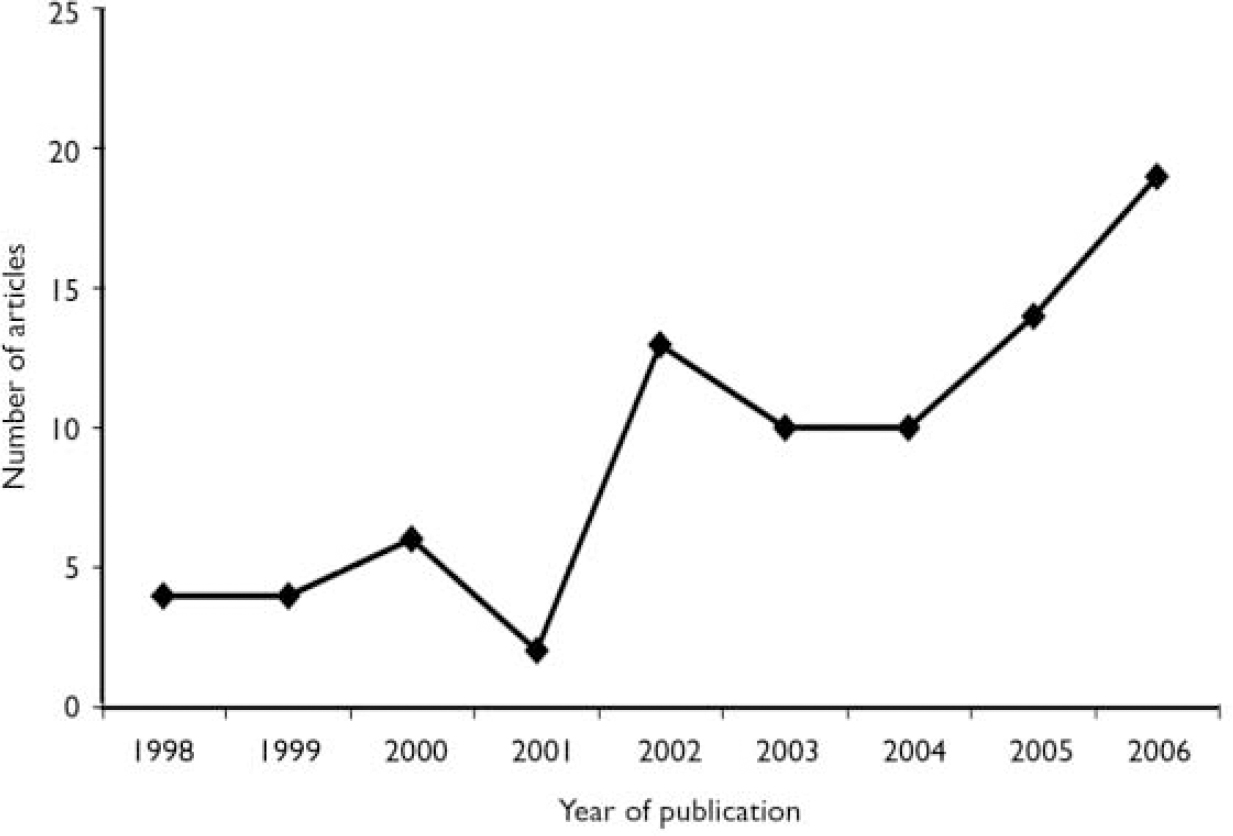
Fig. 1 Number of published articles examining disgust in the context of a disorder since the publication of ‘Disgust – the forgotten emotion of psychiatry’ (Reference Phillips, Senior and FahyPhillips et al, 1998) in the British Journal of Psychiatry.
Conditions based on phobic avoidance
People with spider phobia often report disgust rather than fear-based beliefs about spiders, particularly in reference to their physical attributes and movement. Evidence of disgust mediation in spider phobia includes physiological measures, as it has been shown that when exposed to spiders, people with this phobia respond with greater disgust-specific facial electromyographic activity, such as activity of the levator labii muscle (Reference de Jong, Peters and Vanderhallende Jong et al, 2002).
People with blood injection injury phobia exhibit a unique biphasic response pattern of typical sympathetic activation followed by significant parasympathetic activation. This biphasic process may account for the fainting that is observed in up to 75% of people with this condition when exposed to phobic stimuli. Disgust has become implicated in the vasovagal syncope response because it is associated with parasympathetic activity and reductions in diastolic blood pressure leading to fainting sensations (Reference PagePage, 2003). Although the disgust–fainting relationship in blood injection injury phobia has not been a consistent finding (Reference Olatunji, Williams and SawchukOlatunji et al, 2006), there is consistent evidence that people with this phobia report more disgust levels than controls.
Theoretical developments have implicated a potential role of disgust in contamination-based obsessive–compulsive disorder. Individuals with this disorder often present with heightened appraisals of perceived vulnerability to infection and the spread of contamination upon exposure to offensive agents. Disgust serves a protective, sanitising function by eliciting intense washing rituals upon perceived contact with contaminants. Empirical evidence supporting the role of disgust has shown that measures of disgust correlate with measures of obsessive–compulsive disorder, and disgust appears to account for behavioural avoidance in this condition (Reference Olatunji, Lohr and SawchukOlatunji et al, 2007). Functional magnetic resonance imaging (fMRI) studies have also implicated disgust in this disorder with people who wash obsessively displaying activation of the insula (which is important for the perception of disgust) secondary to the presentation of disgusting pictures. Different distributions of brain activation (mainly in the insula) during disgust-inducing visual stimulation have also been found in comparison with neutral stimulation among people with obsessive–compulsive disorder, and it has been concluded that neurocircuits involved in disgust processing are relevant to this disorder and in particular to the contamination subtype (Reference Husted, Shapira and GoodmanHusted et al, 2006).
As described by Phillips et al (Reference Phillips, Senior and Fahy1998), social phobia may reflect an internalisation of disgust (i.e. self-disgust) that is reflected in shame. There is evidence that social phobia may involve dysfunction with disgust in relation to others. For example, a recent study found that patients with social anxiety disorder are less sensitive to the negative facial expressions of anger and disgust compared with controls (Reference Montagne, Schutters and WestenbergMontagne et al, 2006). Furthermore, it has been shown that individuals with social phobia exhibited a significant increase in anterior cingulate cortex activity compared with non-anxious control group participants when processing disgust v. neutral faces (Reference Amir, Klumpp and EliasAmir et al, 2005). Additionally, compared with a control group, people with social phobia were faster in making accurate ratings of disgust faces.
Other psychiatric disorders
As discussed above, the function of disgust has been described in the context of food ingestion (Reference Rozin and FallonRozin & Fallon, 1987). Therefore, pathological disgust as a disposition towards eating disorders may be expected, in light of the primary focus on food. Food itself often acquires disgust-provoking properties, leading to avoidance of foods that are considered to be fattening. The research thus far has shown that disgust sensitivity tends to correlate positively with eating disorder symptoms in women. There is also evidence to suggest that significant group differences emerge for disgust domains directly related to food, the physical body and bodily products when comparing samples of people with and without eating disorders. High-energy foods and overweight body shapes also tend to be evaluated as more disgusting by women reporting more abnormal eating attitudes than those without such attitudes (Reference Harvey, Troop and TreasureHarvey et al, 2002).
Phillips et al (Reference Phillips, Senior and Fahy1998) also implicated disgust in depression, dysmorphophobia, coprophagia and various sexual dysfunctions. Whether it is involved in a direct or indirect manner in these and other disorders has not been determined. For example, Schienle et al (Reference Schienle, Walter and Schäfer2003) found elevated global disgust proneness in patients with schizophrenia and the presence of psychotic symptoms – irrespective of whether they had occurred once or recurrently and irrespective of whether they were part of different schizophrenia subtypes (paranoid v. non-paranoid) – predicted enhanced disgust reactivity. However, the study also found that depressive episodes were not related to the tendency for more intense disgust experiences. The role of disgust in various psychiatric disorders highlights the importance of differentiating its components. In some disorders (e.g. emetophobia) the experience of disgust may be critically involved, whereas in other disorders (e.g. blood injection injury phobia) the psychophysiological concomitants of disgust may be more critical. Disgust may also mediate other disorders (e.g. obsessive–compulsive disorder) through dysfunctional appraisals of various stimuli that may give rise to fear of contamination.
DISGUST AND PSYCHOPATHOLOGY: EXTRACTING A BROAD THEORETICAL MODEL
The aetiology of disgust-related disorders probably consists of six factors: genetic factors; aversion vulnerability; parental disgust propensity or sensitivity; environmental support of avoidance of contaminants; transmission of contamination and coping information; and external environmental events. Evidence for a genetic component to disgust is mixed. Although the parent–child correlation on disgust/contamination is relatively high (r=0.52), correlations for monozygotic and dizygotic twins are minimal r=0.29 and r=0.24, respectively (Reference Rozin, Haidt, McCauley, Lewis and HavilandRozin et al, 2000). However, inheriting a genetic predisposition toward disgust is likely to result in an aversion vulnerability that is manifested by increased physiological arousal (nausea). The monitoring of physical symptoms associated with disgust, specifically gastrointestinal symptoms and changes in peripheral blood flow (e.g. dizziness), relates well to the acquisition of disgust-related disorders, because these reactions quickly lead to vigilance for sources of contamination. Heightened disgust-mediated physiological arousal may lead to processing biases erring towards the overestimation of contamination and subsequent avoidance and rejection of perceived contaminants. Indeed, there is now evidence that the experience of disgust causes a negative interpretation bias that may be the causal role for disgust in anxiety-related disorders.
The interaction between an aversion vulnerability and environmental support of avoidance and rejection may also contribute to the development of disgust-related disorders. For instance, parents high in disgust propensity or sensitivity with a child with aversion vulnerabilities might be more protective and limit their child's environmental interaction in an effort to reduce the likelihood of contamination. Disgust propensity is the ease of becoming disgusted, whereas disgust sensitivity is the tendency to negatively appraise feelings of disgust. These two vulnerability factors may have very different roles in the aetiology of various disorders; however, parents presenting with either factor may be more likely to provide the child with information regarding sources of potential contaminants (e.g. spiders, door knobs) as well as means of coping after contact (e.g. excessive washing). Stressful environmental events may also increase one's vulnerability for the development of disgust-related disorders.
Since the publication of the editorial by Phillips et al (Reference Phillips, Senior and Fahy1998), researchers are remembering to consider disgust in their conceptualisation of the development and maintenance of various psychiatric conditions. However, many basic questions remain unanswered. For example, is disgust a cause or a consequence of specific phobias? Can excessive disgust be treated? Continued growth of this line of research will largely depend on addressing these basic questions as well as examining the boundaries of the disgust–disorder analysis. No study to date has examined disgust in relation to sexual dysfunction, although feelings of disgust may oppose the generation of sexual arousal. Other disorders (e.g. post-traumatic stress disorder) may also warrant such an analysis. However, future studies must be conducted in light of evidence regarding the physiology (parasympathetic activation) and neurocircuitry (increased activation of the insula and basal ganglia) of disgust. Such a multimethod approach will provide grounds for making more definitive inferences regarding the role of disgust in psychiatric illness.




eLetters
No eLetters have been published for this article.