Pregnancy is associated with an increased risk of both hemorrhagic and ischemic stroke. Reference Swartz, Cayley and Foley1 Apart from traditional risk factors, hemorrhagic stroke in pregnancy can be due to a rupture of pre-existing vascular lesions, such as cerebral aneurysms or brain arteriovenous malformations (AVMs). Reference Liew, Feghali and Huang2 There are also conditions unique to pregnancy that can cause hemorrhagic stroke, such as preeclampsia/eclampsia or coagulopathies like HELPP syndrome (hemolysis, elevated liver enzymes, low platelet count). Reference Liew, Feghali and Huang2 We describe a unique case of a ruptured blister aneurysm during the first trimester of pregnancy that was successfully treated with overlapping flow diverter stent placement.
A 32-year-old, pregnant female presented to the emergency department with a sudden onset severe frontal headache. She was in the first trimester of pregnancy with an approximate gestational age of 12 weeks. Her pregnancy was otherwise uncomplicated apart from hyperemesis gravidarum. Her vitals were within the normal range and neurological examination was unremarkable at admission. CT brain showed Fischer grade 3 diffuse subarachnoid hemorrhage (SAH) associated with intraventricular hemorrhage (modified Fischer grade 4) and mild hydrocephalus (Figure 1). CT angiography (CTA) brain showed an aneurysm, arising at a nonbranching point of the lateral wall of the right supraclinoid internal carotid artery (ICA). It was half dome shaped with a broad neck measuring 4 mm in size. The location and angioarchitecture were consistent with a blister aneurysm (Figure 1).
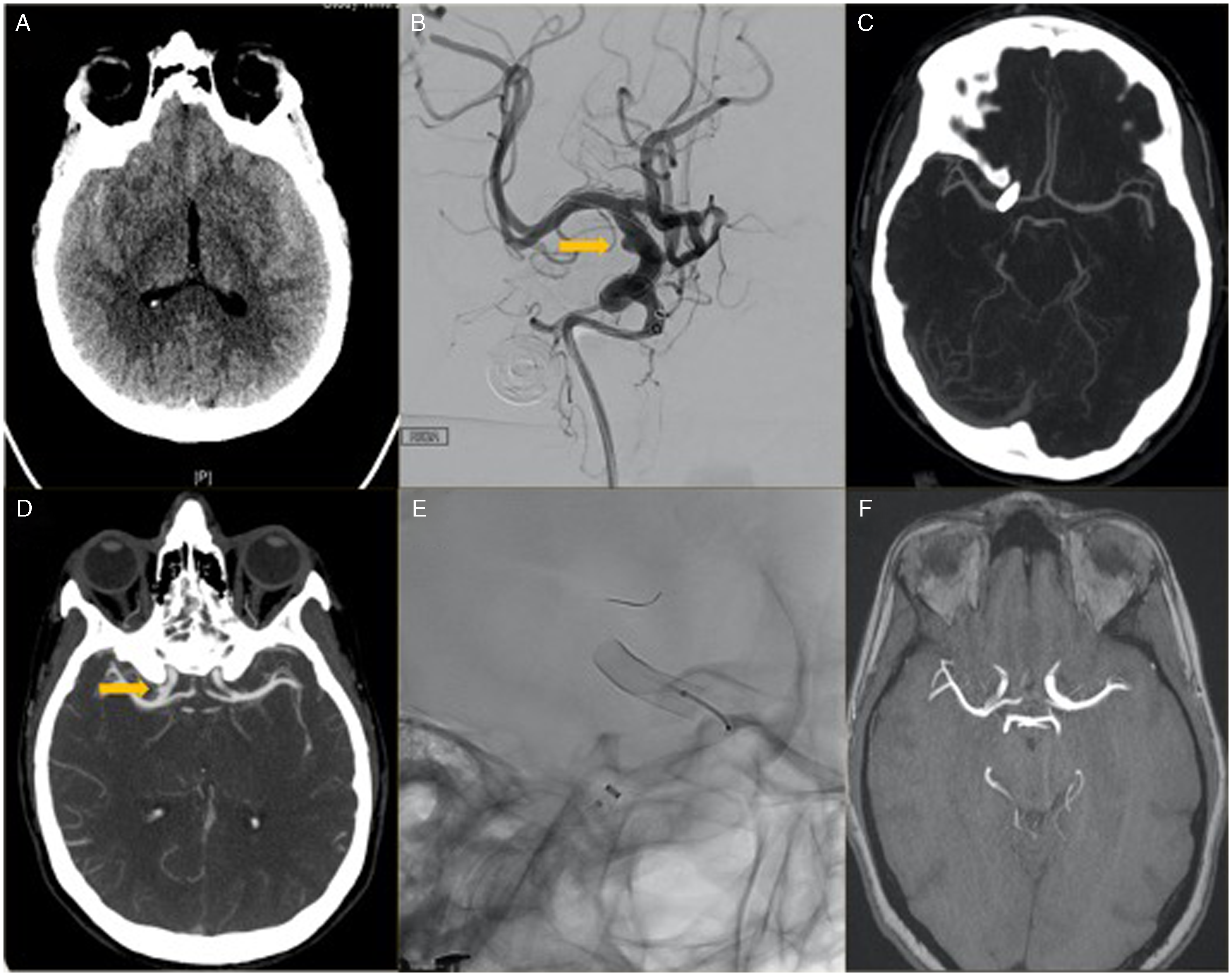
Figure 1: A & D: CT and CTA head showing subarachnoid hemorrhage in the b/l sylvian fissures with right supraclinoid ICA blister aneurysm. B & E: 2D DSA of right ICA showing blister aneurysm and native fluoro images showing deployment of overlapping flow diverter stent (Silk vista). C & F: post-procedure 24 hour CTA and 2-month follow-up. MRA brain showing complete aneurysm occlusion.
The endovascular procedure was performed via right transfemoral route, under heparinization with a target activated clotting time (ACT) two times the baseline. Cerebral angiography again showed conical, broad based, laterally projecting aneurysm arising from the communicating (C7) segment of right ICA between the origins of posterior communicating (P-comm) and anterior choroidal artery (Ach) (Figure 1). The aneurysm dome measured 4 × 3 mm in size, with a neck size of 5 mm. At this point, 10 mg of eptifibatide was given intra-arterially (IA) followed by the intravenous infusion (IV) at 1 mcg/kg/hr. Two overlapping Silk Vista (SV, Size 4 × 12 mm) flow diverter stents were then deployed, with double coverage of the neck of the aneurysm (Figure 1). Despite adequate heparinization and eptifibatide administration, we noticed thromboembolism involving the pre-rolandic branch of the right middle cerebral artery immediately post-deployment of the second stent. Stent retriever-based thrombectomy was performed using Solitaire stent 4 × 20 mm. We carefully avoided pulling the stent retriever through the flow-diverting stents. Instead, the 6F Sofia was carefully advanced past the Silk Vista stents into the proximal M1, and the Solitaire stent was gently pulled into the Sofia. Two passes were performed with improvement in the forward flow of the pre-rolandic artery. Control angiogram showed marked stasis in the blister aneurysm. At this point, the patient was loaded with 300 mg of clopidogrel through a nasogastric tube and 300 mg of aspirin was inserted rectally. The patient was extubated and woke up without any neurologic deficits. The eptifibatide infusion was stopped 3 hours after the loading dose of antiplatelets.
Post-procedure CT/CTA brain showed complete occlusion of the blister aneurysm and no new ischemic infarcts (Figure 1). The patient continued on dual antiplatelet therapy (DAPT) consisting of aspirin 81 mg and clopidogrel 75 mg daily. She was closely monitored in hospital for 2 weeks post-procedure and was eventually discharged home without residual neurodeficits. Three-month MRI with MRA showed complete occlusion of blister aneurysm (Figure 1). She underwent elective cesarean section at 39th week of gestation with the delivery of a healthy baby. She remained on DAPT throughout the pregnancy. Clopidogrel was discontinued 1 week prior to her scheduled C-section and restarted on post-op day 1. She continues to do well with NIHSS 0 and mRS 0 at 6 weeks postpartum follow up. Follow-up MRA at 1 year showed no evidence of aneurysm recurrence and she was stepped down to aspirin 81 mg daily single-agent therapy.
Although, female sex is a known risk factor for SAH, the pathophysiology of aneurysm formation, growth, and rupture during pregnancy remains unclear. The risk of SAH is highest in the third trimester of pregnancy and the immediate postpartum period. Pregnancy-related physiological changes may contribute to SAH risk, including increased cardiac output occurring from the beginning of the third trimester, exposure to the pregnancy-related hormones and pregnancy-related hypertensive disorders. Reference Liew, Feghali and Huang2 Pregnancy itself is very uncommon risk factor for dissection, which are most often noticed in the third trimester or postpartum period and exclusively in the extracranial circulation. Reference Beyer, Dicks and Shainker3,Reference Kadooka, Suemitsu, Saito, Kadooka, Mitsutake and Tanaka4 Other typical risk factors for craniocervical artery dissection (CAD) are major or minor trauma, cervical manipulation, violent coughing, genetic connective tissue disorder etc, but there are multiple reports suggesting association between recurrent vomiting and CAD in the literature. Reference Echefu, Mahat, Vatsavai and Zuckerman5 We hypothesize that the recurrent vomiting due hyperemesis gravidarium contributed to the development of arterial dissection in our patient.
Our case uniquely illustrates that aneurysmal SAH due to a blister aneurysm can occur in the first trimester of pregnancy and can be successfully treated endovascularly with overlapping flow-diverting stents. We placed overlapping flow diverter stents out of concern for poor vessel wall integrity in this type of dissecting aneurysm. Precautions were taken throughout the procedure to reduce the radiation and contrast exposure in pregnancy. Both microsurgical clipping as well as endovascular coiling can be employed for the treatment of the ruptured aneurysm in pregnancy. Compared to surgical clipping, endovascular coiling is less invasive, associated with shorter operative time, and reduced fetus exposure to the anesthetic agents, which are known to be associated with adverse impact on the fetus with the risk of premature labor. 6 Better outcomes have also been noted with endovascular treatment in pregnant patients, similar to results from previous randomized trials in the general population. Reference Molyneux7 The main concerns with endovascular coiling are contrast and radiation exposure. Although the risks associated with radiation exposure are most pressing in the first trimester of pregnancy, they can be effectively reduced by using a combination of strategies including radiation shields over the abdomen and pelvis, low dose and pulsed fluoroscopy, limiting the number of angiographic exposures, tight collimation, minimum use of magnification, and reducing the gap between detector and the patient in order to minimize X-ray scatter. Reference Mahesh8 A report from the International Commission on Radiation Protection advised that fluoroscopy of areas remote from the fetus can be done safely at any time during pregnancy, provided shielding and X-ray beam collimation has been optimized. Reference Valentin9 Similarly, iodinated contrast has not been found to produce any teratogenic effect in animal studies. Reference Puac, Rodríguez, Vallejo, Zamora and Castillo10
The use of intracranial stents and DAPT has been rarely reported in the pregnancy and optimal strategies around antiplatelet therapy are unclear in this patient population. 11 Aspirin is the safest and most commonly used antiplatelet in pregnancy. Similarly, animal data and human studies do not suggest higher than acceptable risk, with a congenital anomaly rate comparable to background risk with the use of clopidogrel. Reference Nana, Morgan, Moore, Lee, Ang and Nelson-Piercy12 The primary risk with the use of clopidogrel is a potentially increased chances for intrapartum and postpartum hemorrhage. In nonpregnant patients, the use of clopidogrel within a week prior to surgery is associated with increased risk of significant bleeding. Hence, we decided to stop Plavix 7 days before the planned CS. Overall, the paucity of data about other antiplatelet agents beyond aspirin and clopidogrel precludes any evidence-based recommendations. Reference Yarrington, Valente and Economy13
Our case was unique in multiple aspects. Firstly, aneurysmal SAH in the first trimester of pregnancy is unusual. Secondly, blister aneurysms involving the anterior circulation and it’s treatment with the flow-diverting stent in pregnancy have not been previously reported. Thirdly, intracranial stenting in pregnancy and associated use of dual antiplatelet has been reported only on few occasions and not in the setting of SAH with use of EVD. Current evidence is insufficient to make strong recommendations regarding a universal management strategy of ruptured aneurysms in pregnancy, particularly in this rare type of blister aneurysm. Reference Molyneux7 Treatment planning requires an individualized and interdisciplinary approach. Maternal and fetal safety should be considered throughout all phases of management.
Author contributions
AD: Conception and design of study, acquisition of data, and drafting the manuscript.
CH: Revising the manuscript critically for important intellectual content.
BA: Revising the manuscript.
AA: Acquisition of data.
BW: Analysis and/or interpretation of data.
Conflict of interest
There are no conflicts of interest to disclose related to this publication.



