Research into self-harm in adolescents has been heavily weighted toward the study of suicide and behaviours related to it. Those episodes of self-harm which owe little or nothing to consistent or lasting suicidal intent are recognised, but mostly studied in relation to young adults. Studies include women with borderline personality disorder, incarcerated men with antisocial personality disorder, people with an intellectual disability and other organic conditions, and those with psychoses or gender identity disturbances who engage in major self-mutilation (Reference FavazzaFavazza, 1989; Reference Pies and PopiPies & Popi, 1995).
The incidence of non-suicidal self-harm in adolescents has been rising year on year and the UK now has the highest rates of this behaviour in Europe (National Institute for Health and Clinical Excellence, 2004), although rates of depression do not show similar geographic or cultural variation. It is estimated that one in ten adolescents in the UK will self-harm (Reference Hawton and JamesHawton & James, 2005), although the actual number may be much higher. These behaviours lead to 24 000 hospital admissions per year (Samaritans & Centre for Social Research, 2002). The report Truth Hurts (Mental Health Foundation, 2006) urges us all ‘to hear the voices of the young people’ and commit to playing an active part in ‘transforming the experience of the 1 in 15 young people in the UK who are in such pain that they are harming themselves’.
Particular groups at risk include girls (with seven times the incidence in boys), prisoners and young Asian women (National Institute for Health and Clinical Excellence, 2004). Reasons for self-harm include relationship problems with peers, family and school, depression, bullying, alcohol and drug misuse, and low self-esteem (Reference Fox and HawtonFox & Hawton, 2004; Reference Hawton and JamesHawton & James, 2005).
A number of explanations are offered for the behaviour, including a release of tension, frustration and anger, and using self-harm to communicate difficult feelings. Self-harming may begin in adolescence, but it frequently persists into adulthood and can become addictive (Reference Favazza and ConterioFavazza & Conterio, 1989).
It is clear that such behaviour, when it occurs within defined communities, for example at hospital in-patient units, can be followed by fellow in-patients (Reference Taiminen, Kallio-Soukainen, Nokso-Koivisto, Kaljonen and HeleniusTaiminen et al, 1998).
Interventions designed to reduce or eliminate self-harm have been researched mostly in young adults, with a scarce number of studies that include adolescents. The literature on self-harm in adults suggests that whereas medical interventions have an impact on some of the associated factors, such as low mood and low self-esteem, few lead to lasting success in reducing the incidence of self-harm.
Oakwood Young People's Centre
Oakwood Young People's Centre is a sub-regional in-patient and day-patient National Health Service (NHS) adolescent unit with 13 beds and 12 day places, although staffed for only 3 beds at weekends and public holidays. Like most similar units, we have moved from operating as a therapeutic community at the centre's inception in 1981 to an acute general psychiatric adolescent ward. We continue to utilise the therapeutic opportunities afforded by having a managed group of adolescents under our care.
The mean length of stay in the centre is 6 months. The centre is open 365 days per year and a third of total admissions are acute emergency admissions. The centre's admission criteria specifically exclude those with a moderate or severe intellectual disability.
In the last 3 months of 2002 the generally steady background level of self-harm on the unit (mean number of episodes per week 1.2, s.d.=1.3) escalated to alarming proportions (mean number of episodes per week 8.1, s.d.=4.0). Here, we defined self-harm as making cuts on one's body or over-dosing on purchased prescription drugs. The acute management of self-harm was detracting from other therapeutic work and teenagers who had not previously self-harmed were learning and practising these behaviours during their admission. Those who were not self-harming, as well as their parents, clearly expected staff to protect them from the distressing sights and repercussions of self-harm occurring on the unit.
Intervention
We addressed the self-harm problem directly and drew up a new policy to guide staff. We introduced this to the in-patients in December 2003, allowing time for discussion and questions and indicating that the new policy would take effect after the New Year holiday.
The essence of the policy was to emphasise that we recognise that many struggle with self-harm and have used it in the past. We offer a range of support and alternative coping techniques, for example the use of ice, rubber bands and marker pens instead of sharp objects, diaries, relaxation and distraction, as well as a wide range of therapeutic interventions to address the patient's underlying distress and problems. We would view self-harm on the unit as analogous to the use of alcohol or illicit substances - completely unacceptable and resulting in immediate suspension from the unit. Following suspension, a person would return to a meeting, in which their care givers would participate, to consider and renegotiate their therapeutic contract with us. Such contracts are rarely written and signed, although the care plans are. Any repeated self-harm would be grounds for discharge.
We recognised the need to make rare exceptions to the policy, for example behaviour stemming from genuine and persistent suicidal intent.
Results
Monitoring and reporting incidents is rigorous on the unit and gives us confidence that few, if any, episodes of self-harm would go undetected.
There were three distinct periods in data collection.
-
1. The background level from April 2002 until the end of September 2002.
-
2. The 3-month period when the self-harm escalated (October to December 2002).
-
3. The period following policy implementation up to the present (February 2003 to the present).
The rates of self-harm for the 2 weeks following implementation were similar to those in the 3 months before implementation. Initially, many in-patients did not believe that the policy would be implemented or that it would be followed consistently. Thereafter, the rates fell and have remained low to the present (Table 1).
Table 1. The number of self-harm episodes on the unit before and after intervention
| Period | Episodes per week, mean (s.d.) |
|---|---|
| Background level, April 2002–September 2002 | 1.2 (1.3) |
| October 2002–December 2002 | 8.1 (4.0) |
| February 2003–present | 0.2 (0.59) |
Managing self-harm on the unit is no longer a task which detracts staff from other aspects of their work (Fig. 1).
There were no differences in the levels of occupancy or in the patients’ diagnoses in the three periods identified, namely at baseline, in the 3 months before the Christmas holidays 2002 and after the policy was implemented.
Our policy is explained to all individuals being assessed for admission to the unit. To date, we have not discharged any patient as a consequence of the policy, nor has anyone refused admission as a direct result of being unable to comply with the policy. Rather, patients and parents at admission generally welcome and support the efforts made to maintain the safety of the individual and the community of patients. We monitor patients’ weekend activities by telephone or face-to-face contact with carers upon return to the unit on Sunday evening; we have not noted any increase in self-harm at weekends. Rigorous incident reporting procedures support our impression that self-harm behaviours have not been replaced by alternative injurious acts not specifically included in the policy.
Discussion
During the drafting of the policy, not all the unit's staff supported the initiative. Some feared that it might be perceived as punitive or judgemental and suggested we ought to accept these behaviours or ‘work with them’. Nevertheless, the danger posed by these behaviours and their disruptive and distressing effect was clear to staff and other in-patients. Through a prolonged period of consultation, staff were helped to realise the lack of alternative, effective therapeutic interventions available to us and the need to act consistently. This helped stem the tide of opinion suggesting that we should maintain a very flexible response to self-harm behaviours.
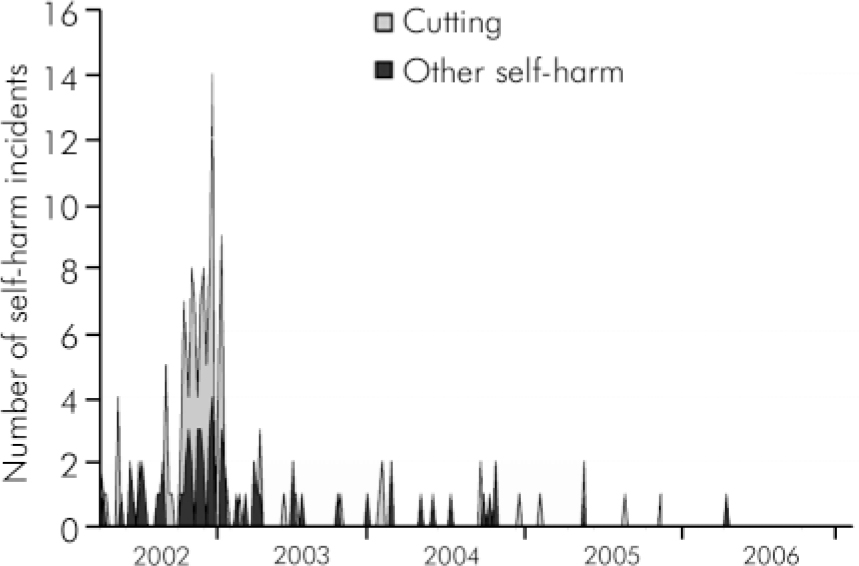
Fig. 1. The number of self-harm incidents on the unit before and after the policy was implemented. Data were collected monthly; last self-harm incident recorded in April 2006.
The policy is specifically limited to addressing behaviours on the unit and does not include weekend activities off the unit.
In retrospect, the commitment of the in-patients to their place on the unit is evident in their efforts to stem behaviours which might result in their discharge.
This approach depends upon the staff's ability to offer meaningful sanctions for self-harm, while continuing to offer support, alternative coping strategies and therapies. Such an approach is not necessarily directly applicable to non-institutional settings, for example in the community. However, the contagious nature of self-harm is well recognised in schools, where consideration of the model may prove useful.
Conclusions
There is an obvious and pressing need for more research into the area of self-harm, in particular non-suicidal self-harm in adolescents, not least in the areas of intervention and treatment. We cannot rely with confidence upon extrapolation of adult findings to support our work with teenagers.
There is a risk that a need to understand the behaviour (for self-harm is not an illness) may be confused with an apparent acceptance, condoning or even fostering the behaviour. Since violence towards others is unacceptable, perhaps we might consider violence towards oneself, at least, in a similar vein. We may accept the continuation of self-harm behaviours when working with adults, but I view it as an inappropriate response when working with adolescents.
Declaration of interest
None.





eLetters
No eLetters have been published for this article.