Introduction
The COVID-19 outbreak and its public health control measures have generally substantially increased the prevalence of social isolation and loneliness among older adult populations since the beginning of the pandemic (Savage et al., Reference Savage2021). Although loneliness and social isolation can co-occur, they are distinct concepts. Loneliness refers to a subjective psychological state or feeling of being alone, whereas social isolation is an objective observable state which is inferred by the lack of social proximity and engagement with others even though the individuals involved may not feel lonely (Cacioppo and Cacioppo, Reference Cacioppo and Cacioppo2018; McClelland et al., Reference McClelland, Evans, Nowland, Ferguson and O'Connor2020). Loneliness has been found to have a weak correlation with social isolation that can occur without one another (Coyle and Dugan, Reference Coyle and Dugan2012). Individuals can have feelings of loneliness despite having frequent social involvement, whereas others without frequent social interactions may not feel lonely. It is important to distinguish between loneliness and social isolation.
The literature has accumulated ample evidence on the negative consequences of loneliness and social isolation on a wide range of physical and mental health problems (Hwang et al., Reference Hwang, Rabheru, Peisah, Reichman and Ikeda2020; Smith and Victor, Reference Smith and Victor2019). Lonely individuals in comparison to others have been found to have increased all-cause morbidity and mortality (Cacioppo and Cacioppo, Reference Cacioppo and Cacioppo2018), increased risk of cardiovascular diseases (Barth et al., Reference Barth, Schneider and Von Känel2010; Thurston and Kubzansky, Reference Thurston and Kubzansky2009), impaired functional status and quality of life (Lee et al., Reference Lee2019). Similarly, being socially isolated has been found to have negative consequences on well-being, including increased risk of morbidity and mortality (Holt-Lunstad et al., Reference Holt-Lunstad, Smith and Layton2010), coronary heart diseases (Lee et al., Reference Lee2019), impaired cognitive function (Wilson et al., Reference Wilson2007), and major depression (Cacioppo et al., Reference Cacioppo, Hawkley and Thisted2010).
The literature on loneliness/social isolation during COVID-19 in the general population has been synthesized (Buecker and Horstmann, Reference Buecker and Horstmann2021). However, to our knowledge, no systematic review has been published on the prevalence of loneliness and/or social isolation among those aged 65+ during pandemics, such as COVID-19. Because of the circumstances of aging involving relationship losses, medical morbidities, and functional declines, older adults are more likely to experience loneliness and social isolation (Bryant et al., Reference Bryant2004). The COVID-19 and its related public health measures have significantly increased the likelihood of social isolation and loneliness among older adults living in care facilities and the general community (Gorenko et al., Reference Gorenko, Moran, Flynn, Dobson and Konnert2021; Plagg et al., Reference Plagg, Engl, Piccoliori and Eisendle2020; Schmitz et al., Reference Schmitz, Holley, Meng, Fish and Jedwab2020). It has had negative consequences on the mental health of older adults (Sarbadhikari and Sarbadhikari, Reference Sarbadhikari and Sarbadhikari2020). The COVID-19 pandemic has also led to significant changes in the delivery of physical and mental health care (i.e., virtual care by phone or video). It is important to have a timely update on the prevalence of social isolation and loneliness among older adults during this current COVID-19 pandemic.
As countries each have their own manner and pace in dealing with the pandemic, it is possible that the pandemic may affect people differently in different jurisdictions (Varga et al., Reference Varga2021). Indeed a substantial variation in the prevalence of loneliness across different regions of the world has been reported (Dean et al., Reference Dean2021). Furthermore, the prevalence of loneliness and social isolation among the elderly has varied during different periods of the pandemic and is closely linked to the duration of the pandemic, public health control measures, and the severity of the pandemic (Harden et al., Reference Harden, Price, Mason and Bigelow2020; O’Shea et al., Reference O’Shea, Finlay, Kler, Joseph and Kobayashi2021). A detailed and comprehensive overview of the impact of the COVID-19 pandemic on loneliness and social isolation is warranted to understand how the prevalence of loneliness and social isolation is related to different phrases of the COVID-19 pandemic, different global regions, as well as the severity of the pandemic and the restrictiveness of public health control measures taken.
This present systematic review and meta-analysis aim to address the knowledge gap on social isolation and loneliness among older adults during the COVID-19 pandemic by providing up-to-date pooled estimates of the prevalence of social isolation and loneliness among older adults during the COVID-19 pandemic. This review also provides quantitative syntheses on subgroup differences in the pooled prevalence of social isolation and loneliness, in terms of geographical regions, phases of the pandemic, prevalence estimate period, and the severity level of the Covid-19 pandemic in the study region. The findings of the review offer the best available current evidence on the issues of loneliness and social isolation among older adults during the COVID-19 pandemic and identify the major correlates of these attributes among older adults.
Methods
Searching strategy
This systematic review and meta-analysis were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., Reference Moher, Liberati, Tetzlaff and Altman2009). This review was registered prospectively with PROSPERO (CRD42021259103). Four electronic databases, EMBASE, PsychoInfo, Medline, and Web of Science, were comprehensively searched from January 2000 to November 2021 to identify potentially relevant studies. The search strategies were developed and tailored for each database by YS, WR, ML, GC, and XM. Grey literature resources including National Technical Information Service (NTIS) and publications in the King’s Fund were also searched. In addition, we manually searched the reference lists of selected articles, and review articles on relevant topics.
Inclusion criteria and exclusion criteria
Articles were included in this review according to the following inclusion criteria: (a) studies of human subjects; (b) had a measure of loneliness or social isolation; (c) provided statistical estimates to be able to calculate the prevalence of loneliness and/or social isolation during pandemics; (d) studied older adults aged 65+; (e) published in English, Chinese, Danish, French, German, Italian, Norwegian, Portuguese, Spanish and Swedish. Articles were excluded if: (a) the study had no data that could be used to calculate the prevalence of loneliness or social isolation; (b) the study was not conducted during pandemics in the past two decades.
The study protocol initially called for a wider search for any pandemic occurring in the last two decades, so the search terms included Ebola or influenza or flu or grippe or orthomyxovirus or myxovirus*or plague or MERS or middle east respiratory syndrome, however, no relevant studies were found, only studies on COVID-19 pandemic. So we proceeded with the systematic review and meta-analysis of these studies.
Study selection and data extraction
Two reviewers (YS and WR) independently reviewed and screened the titles and abstracts of all retrieved literature. The full texts of potentially eligible studies were then reviewed independently, and any discrepancies between reviewer selections were resolved by a group discussion. The extraction form recorded study data on the first author, publication year, study country, study setting, sample size, sample collection, sampling methods, study period, phases of a pandemic, sex proportion, age range, the severity of a pandemic, mean age, study design, instruments used to measure social isolation and/or loneliness, cut-offs used to define the presence of loneliness or social isolation, the prevalence of social isolation or loneliness, and measurement of prevalence estimates. The study information was extracted independently by two authors (YS and WR); also a colleague was used to help with articles not published in English, French, or Chinese (GC). In addition, we contacted the authors of articles for further information when the prevalence was not reported in the original articles.
Quality assessment
The study quality of each selected article was assessed by the Loney’s 8-item scale (Loney et al., Reference Loney, Chambers, Bennett, Roberts and Stratford1998). The scale includes eight items: definition of the target population, sampling method, response rate, non-responder description, representativeness of samples, data collection method, diagnostic criteria, and precision of prevalence estimates. The total score ranged from zero to eight. The study quality was assessed by two reviewers (YS and WR), independently. The quality assessment of each reviewed study is shown in Supplementary Table S1.
Meta-analysis
A random-effects (DerSimonian and Laird method) model was used to pool the prevalence and 95% confidence intervals (CI). Heterogeneity across the included studies was assessed using the Cochran Q test and Higgins and Thompson I 2 statistic, which indicates the percentage of total heterogeneity due to variations in studies (Higgins and Thompson, Reference Higgins and Thompson2002). Publication bias was evaluated with the funnel plots and Egger’s and Begg’s tests, and the significance level was set at 0.05 (two-sided). The trim and fill procedure was used to detect and adjust for publication bias (Duval and Tweedie, Reference Duval and Tweedie2000). Subgroup analyses of loneliness and social isolation were conducted for different geographical regions, phases of the COVID-19 pandemic, prevalence estimate period, and a severity level of COVID-19 spread. The severity level of the COVID-19 was grouped based on the newly confirmed COVID-19 cases per million population (low “<10/1M”, moderate “10–100/1M”, and high “>100/1M”) in specific countries at the time of the individual study was conducted. Meta-regression analyses were used to further assess the influence of different study characteristics including mean age, male proportions, sample size, mode of data collection, sampling methods, study design, and each item in the study quality assessment criteria. Sensitivity analysis was used to assess the influence of each individual study on the pooled prevalence estimate by recalculating the pooled estimates, excluding this particular study at a time. Statistical analyses were performed by Comprehensive Meta-Analysis (CMA) Version 3.0 (Biostat, Inc., Englewood, NJ, USA).
Results
Selection of articles
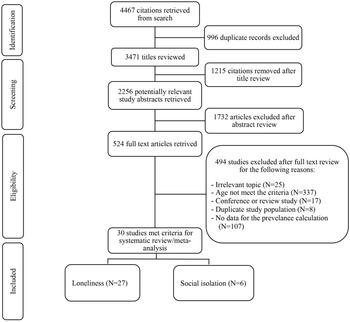
The initial search produced 4467 titles, from which 2256 abstracts were reviewed, 524 articles were then retrieved for a full evaluation. A total of 30 original articles that provided the period prevalence data at different time points were included, including 27 articles on loneliness and 6 articles on social isolation. Since the experience of loneliness and social isolation can vary in intensity and frequency during an individual’s different life stages therefore all eligible studies reported period prevalence of the loneliness and social isolation which was measured over an interval of time for easy interpretation. Figure 1 shows the process of the study selection. All articles were published during the COVID-19 pandemic. These articles were from 15 countries of four continents: Europe (14 studies: four in UK, three in German, two in Spain, and one each in Austria, Ireland, Denmark, Norway, and Finland), North America (five studies in the USA and three studies in Canada), South America (one study in Brazil), and Asia (four studies in Japan and one each in China, Korea, and Turkey). Twenty-eight of the articles were published in English and two were published in German. The sample size of the study cohorts ranged from 10 to 4840. These studies covered a total of 20,188 participants for loneliness and 7862 subjects for social isolation. Table 1 provides detailed data on the characteristics of the included articles.

Figure 1. PRISMA flow diagram.
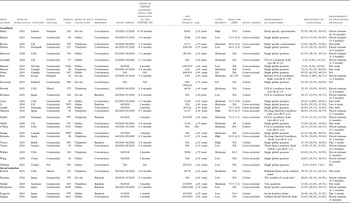
Table 1. Characteristics of studies included in the meta-analysis

NA: not available.
a The cutoff of 50th percentile was defined.
b The cutoff of 80th percentile was defined.
The total score of quality assessment ranged from 2 to 8, with a median score of 4. Sixteen studies had good quality with their quality scores greater than the median score. All studies had a clear definition of a target population and a standardized data collection approach. Nine studies (30%) used a random sampling method and adequately described their sampling frame, and thirteen studies (43%) had information on the response rate. Fourteen studies (47%) used reliable and validated measurement methods to assess loneliness or social isolation according to standardized criteria. Supplementary Table S1 reports on the quality assessments of the studies included in the review.
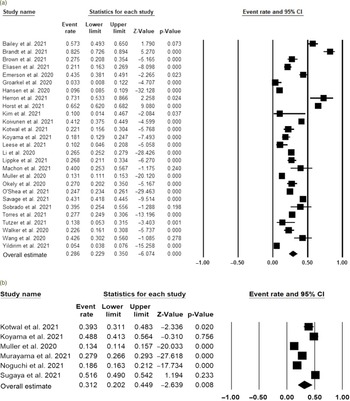
Evaluation of the publication bias
We ran the Egger’s test and Begg’s test to assess whether there was any potential publication bias for loneliness studies (Egger linear regression: t = 0.552, P = 0.586; Begg rank correlation: z = 0.553, P = 0.580) as well as social isolation studies (Egger linear regression: t = 0.041, P = 0.969; Begg rank correlation: z = 0.188, P = 0.851). Both the Egger’s test and Begg’s test and the funnel plots did not identify any publication bias (Figure 2a and b).

Figure 2. Funnel plots for the prevalence of loneliness (a) and social isolation (b) among older adults during the COVID-19 pandemic.
The pooled period prevalence of loneliness and social isolation among elderly people during the COVID-19 pandemic
A total of 27 studies were included to quantify the pooled period prevalence of loneliness and six studies for the pooled period prevalence of social isolation. Figure 3 presents forest plots of the prevalence of loneliness (Figure 3a) and social isolation (Figure 3b) among older adults during the COVID-19 pandemic. The pooled prevalence of loneliness was 28.6% (95% CI: 22.9–35.0%, P = 0.001, I 2 = 98.5%) based on the random-effects model. The pooled prevalence of social isolation was 31.2% (95% CI: 20.2–44.9%, P = 0.008, I 2 = 99.0%).
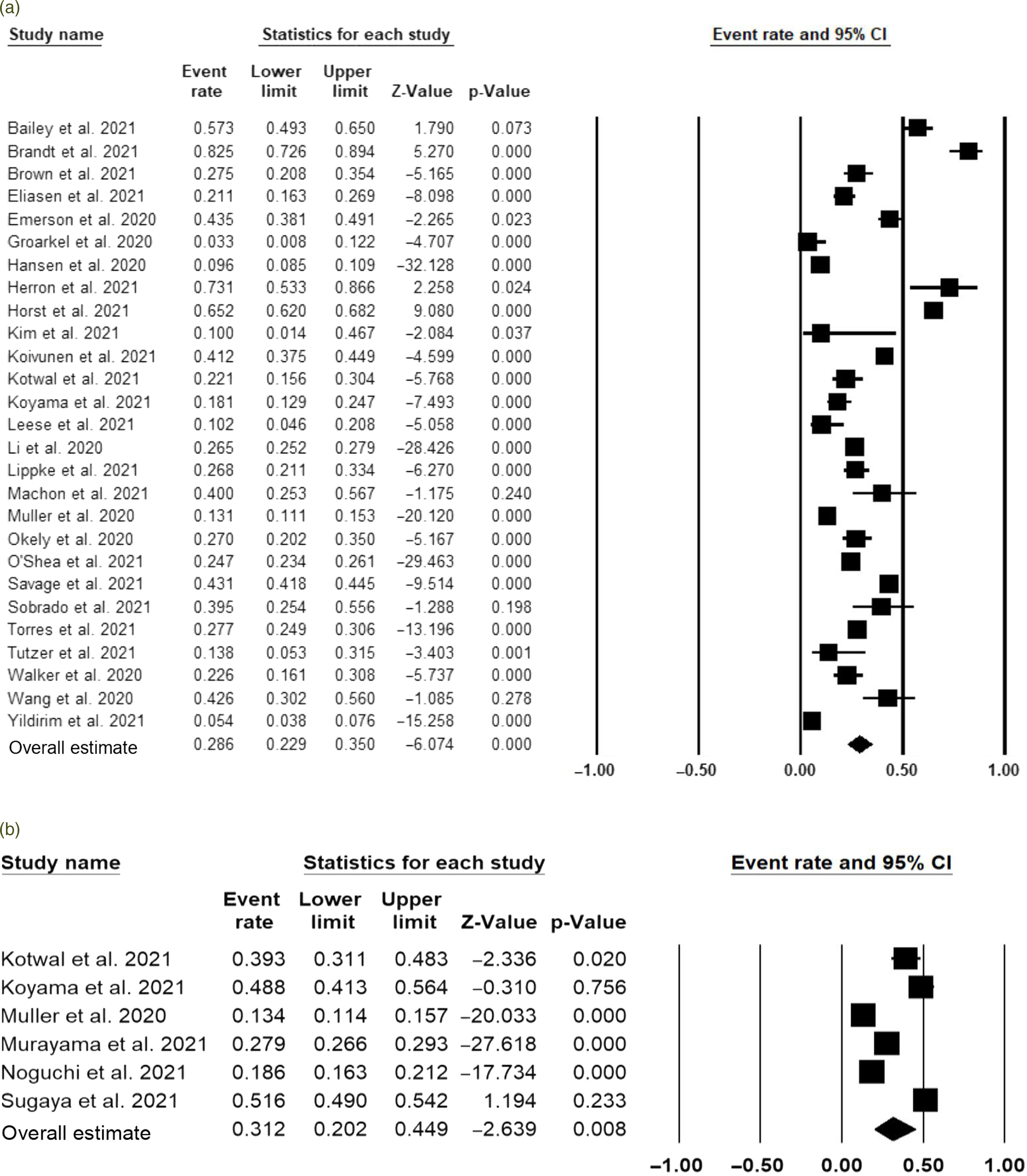
Figure 3. Forest plots of prevalence of loneliness (a) and social isolation (b) among older adults during the COVID-19 pandemic.
Subgroup analyses
The pooled prevalence of loneliness and social isolation was further compared by different subgroups, including whether studies were conducted during the first 3-month of the pandemic, measurement of prevalence estimates, geographical regions, and the severity level based on the new COVID-19 positive cases at the time each study was conducted (per 1 million population). Table 2 presents subgroup analyses of the pooled prevalence of loneliness and social isolation. For both loneliness and social isolation, studies conducted after the third month of the pandemic reported higher prevalence rates than those conducted within the first 3 months: 31.3% vs. 25.6% for loneliness; 41.5% vs. 15.9% for social isolation. No significant differences on the pooled prevalence of loneliness or social isolation were found for different measurements of prevalence estimates, geographical regions, and the severity levels of the COVID-19 pandemic.
Table 2. Subgroup analysis of the pooled prevalence of loneliness and social isolation
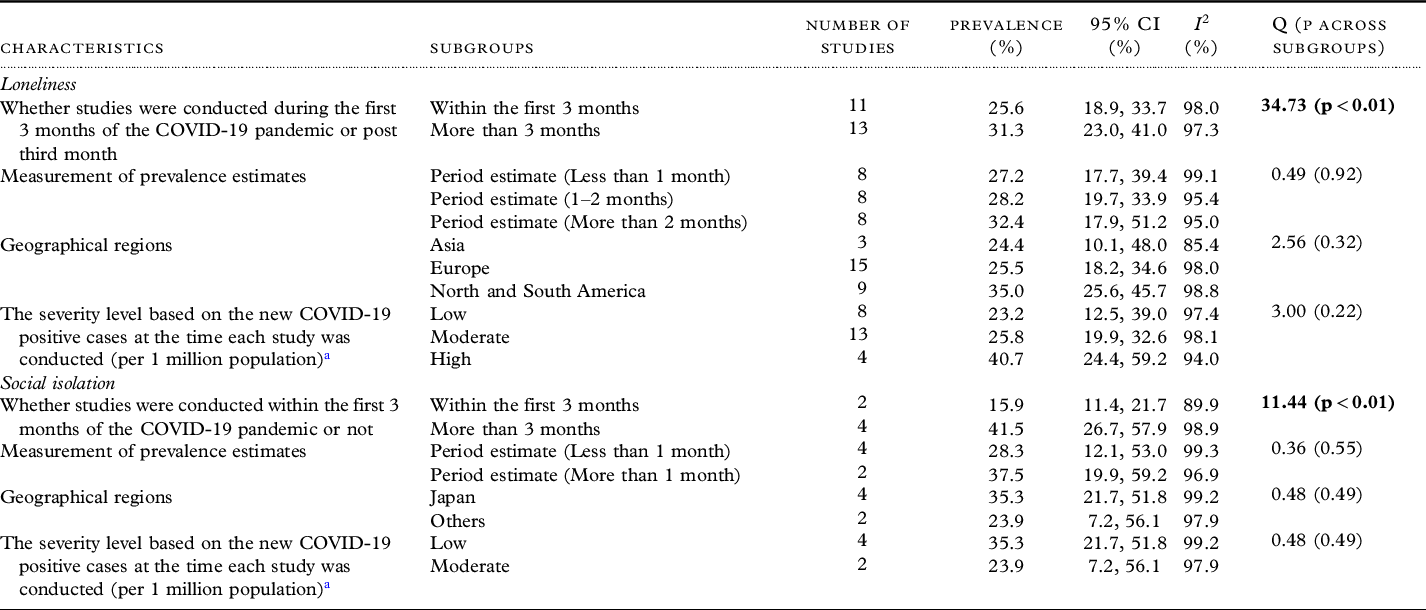
a The source of the estimate is from: https://ourworldindata.org/covid-cases.
Meta-regression and sensitivity analysis
Meta-regression was used to evaluate the impact of study characteristics as well as the quality assessment items on the pooled estimates. For loneliness, none of the study characteristics (age, male proportion, sample size, mode of data collection, sampling methods, and study design) was associated with the pooled estimates (P > 0.05). Only two quality assessment items (sample selection (probability sampling or total population surveyed), and the representativeness of the target population) were associated with the pooled prevalence of loneliness. For social isolation, only the male proportion was statistically associated with the prevalence estimates (P < 0.01) with a higher proportion of males associated with greater reported isolation. Table S2 provides the details on all the variables analyzed in meta-regression.
To assess the impact of an individual study on the pooled estimates, sensitivity analysis was conducted by excluding one study at a time. For both loneliness and social isolation, sensitivity analyses yielded similar results, indicating no individual study influenced the pooled prevalence of loneliness or social isolation (Supplementary Figure S1–S2).
Discussion
This systematic review and meta-analysis are the first to provide a timely update on the prevalence of loneliness and social isolation among the older population aged 65 years and over during pandemics. All the studies included in this review were conducted during the COVID-19 pandemic. By synthesizing a total of 30 observational studies covering 28,050 participants, the meta-analysis found that the overall period prevalence of loneliness and social isolation for the elderly people during the COVID-19 pandemic was 28.6% and 31.2%, respectively. Significant differences in the pooled prevalence of loneliness and social isolation were identified for studies conducted within the first 3 months of the COVID-19 pandemic versus those conducted after 3 months into the pandemic. The pooled prevalence of loneliness was also associated with sample selection as well as the representativeness of the target population, whereas the pooled prevalence of social isolation was associated with male proportion.
The pooled period prevalence of loneliness and social isolation during the pandemic substantially increased compared to similar rates before the COVID-19 pandemic. The prevalence of loneliness among the older population was estimated between 5% and 10% across Australia, Northern Europe, and North America, and ranged from 10% to 18% in Southern Europe (Yang and Victor, Reference Yang and Victor2011). Studies from Asia had reported a much higher prevalence, which was up to 30% (Chen et al., Reference Chen, Hicks and While2014). The global prevalence of social isolation among persons aged 60 years and above ranged from 7% to 24% (Chen and Schulz, Reference Chen and Schulz2016). Many countries have reported an increase in the prevalence of loneliness and social isolation after the outbreak of the COVID-19 pandemic (Robb et al., Reference Robb2020). The elevated prevalence of loneliness and social isolation is partially associated with various public health control measures (Rodney et al., Reference Rodney, Josiah and Baptiste2021). The negative consequences of public health control measures (i.e., masking, physical distancing, and limited contacts) may reduce social interactions and decrease the buffering effect of social support during the COVID-19 pandemic (Lee, Reference Lee2020).
This review reiterates the vulnerability of older adults during the pandemic not only because of their high likelihood of physical diseases and are more prone to the severity of the COVID-19 symptoms, but also because they are more susceptible to psychological issues, in particular, loneliness and social isolation (Hoogendijk et al., Reference Hoogendijk2020). Interestingly, recent studies have found that, compared to younger age groups, older adults tended to report lower levels of loneliness and social isolation during the COVID-19 outbreak (Li and Wang, Reference Li and Wang2020; Teater et al., Reference Teater, Chonody and Hannan2021). This is in part explained by Carstensen’s socio-emotional selectivity theory, which posits that older populations require fewer social interactions than younger populations, thus loneliness is not as prevalent among older people (Carstensen, Reference Carstensen1992). Future research is warranted to examine whether older populations are more resilient to the issues of loneliness and social isolation than younger people during the medical pandemics.
Evidence has been well established to illustrate the detrimental effects of loneliness on health, in particular, focusing on the stress response. For example, increased cortisol levels could create physiological changes, and potential mechanisms may be related to behavioral changes such as unhealthy lifestyles (Kobayashi and Steptoe, Reference Kobayashi and Steptoe2018; Xia and Li, Reference Xia and Li2018). Given the high prevalence of loneliness and social isolation, it is urgent to address these psychological needs and to guide psychological interventions that not only address the negative consequences of social isolation and loneliness among the elderly but also make interventions accessible and appropriate for older adults.
The review identified a slightly higher prevalence of social isolation compared to loneliness among older adults during the COVID-19 pandemic. Social isolation and loneliness assessed the objective and subjective aspects of being alone, respectively (Wenger and Burholt, Reference Wenger and Burholt2004). Social isolation and loneliness were generally non-overlapping social experiences, with only 5% of older adults experiencing both (Kotwal et al., Reference Kotwal2021). The higher prevalence of social isolation in part may be associated with social distancing which adds difficulties to connect others among the older population (Sepúlveda-Loyola et al., Reference Sepúlveda-Loyola2020), whereas loneliness may occur through pathways unrelated to the frequency of social network interaction, including from existing distress and anticipatory grief (Kotwal et al., Reference Kotwal2021). In the situation of a pandemic, older adults may downgrade their subjective perception of what constitutes adequate feelings of companionship (Shiovitz-Ezra et al., Reference Shiovitz-Ezra, Shemesh, McDonnell, Ayalon and Tesch-Römer2018). Identification of differences in social isolation and loneliness can better prepare health care systems to address these needs and make interventions accessible and appropriate for older adults.
We also found that the prevalence of loneliness and social isolation varied according to the phases of the COVID-19 pandemic. The prevalence of loneliness and social isolation was significantly higher after the first 3 months of the pandemic. It is understandable that loneliness and social isolation increased over time as the pandemic and its control measures continue and produce cumulative effects on these psychological issues. As the pandemic is likely to last longer than anticipated, leading to long-term consequences due to its health, economic, and societal impacts (The Lancet Public Health, 2020), the need to tackle the rising tide of social isolation and loneliness becomes more important. The findings of the meta-regression analyses also showed that two study quality items (probability sampling methods and whether using representative samples) were linked with the pooled prevalence of loneliness. Sampling procedures are related to selection bias, which negatively influences the interval validity of the results. Our finding also supports the previous studies suggesting that older women tended to report more frequent and greater perceived intensity of social isolation and were more vulnerable than older men in regard to social isolation (Baumeister et al., Reference Baumeister, Kriston, Bengel and Härter2010). This may represent that older women rely more heavily on social connections. Thus, they may be more vulnerable to be socially and emotionally affected by being less connected with their social environment and more likely to use healthcare services for social isolation, especially during the pandemic (Shukla et al., Reference Shukla2020). We did not observe statistical significances in geographical regions, the severity level of COVID-19 spread, or measurements of prevalence estimates for both loneliness and social isolation. The high heterogeneity in the review adds variations across studies, which are linked with wide confidence intervals. The high heterogeneity indicates that period prevalence varied considerably between the included studies. These pooled estimates should be interpreted with caution given to the existence of high heterogeneity. The high heterogeneity across prevalence studies was also expected compared to meta-analyses of other types of data (Migliavaca et al., Reference Migliavaca2022). Future studies with more consistent study characteristics (including measurements, sampling procedures, and the phrases of the pandemic) are warranted.
There are several limitations to be noted. First, this review identified the high heterogeneity between studies, and the heterogeneity was not associated with study characteristics examined in subgroup analysis and meta-regression analysis, except the phases of the COVID-19 pandemic and study sample selections. Different measurements of loneliness and social isolation, study population, and study design of the included studies could be the sources of heterogeneity. Second, the majority of the included studies were cross-sectional, which provided only a snapshot of the prevalence. It limited us to compare the rates across different phases of the COVID-19 pandemic. Third, although a comprehensive search strategy was used to assess the prevalence of loneliness and social isolation during the last two decades, this review only identified studies published during the COVID-19 pandemic. No comparison on the impact of a pandemic on these psychological issues can be inferred. Lastly, most of the included studies were conducted within the first 6-month of the COVID-19 outbreak. The medium and long-term impact of the COVID-19 pandemic on social isolation and loneliness is not currently available. Future research on the long-term impact of the COVID-19 pandemic or other pandemics on loneliness and social isolation is needed.
Conclusions
Overall, the pooled prevalence of loneliness and social isolation among older adults during the COVID-19 pandemic was striking. As the COVID-19 pandemic continues to last, the pooled prevalence of loneliness and social isolation among the older population is likely to increase as the prevalence of loneliness and social isolation was significantly higher in studies conducted after the third month of the COVID-19 pandemic compared to the similar prevalence reported in studies conducted within the first 3 months of the pandemic. Health policymaking and the healthcare systems need to address the rising demand of psychological needs by applying effective psychological interventions that are tailored to the needs of older adults. The findings of the review also highlighted the need for longitudinal studies to examine the long-term impacts of pandemics, such as COVID-19, on loneliness and social isolation among older populations.
Conflict of interest
None.
Description of authors’ roles
All the authors contributed to the planning, development, and editing of the systematic review. XM designed this review. YS and WR conducted the search, together with XM reviewed the articles returned by the search for eligibility and reviewed all data extraction. YS prepared the first manuscript draft. XM, ML, GC, and CD oversaw the project, provided feedback on all steps of the search and data extraction and interpretation. All authors contributed to the writing, revisions, and editing of the final manuscript.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1041610222000199