Introduction
Much of the excess risk of violent behaviour in psychotic disorders can be explained by substance use disorder (SUD) (Fazel et al., Reference Fazel, Gulati, Linsell, Geddes and Grann2009). In a meta-analysis of 16 studies with a total of 5365 cases, SUD more than doubled the odds of violence [odds ratio (OR) 2.2, 95% confidence interval (CI) 1.6–2.9] (Witt et al., Reference Witt, Van Dorn and Fazel2013).
However, it is unclear to what extent different categories of illicit substances, as defined by their psychopharmacological effects, are related to violent behaviour. Another uncertainty is whether subthreshold use, as opposed to SUD, is a risk factor for violence. These questions may be clinically relevant, as the psychopharmacological properties of substances modify violence risk in the general population (Tomlinson et al., Reference Tomlinson, Brown and Hoaken2016) and people with psychotic disorders are highly sensitive to the harmful effects of substances (Gregg et al., Reference Gregg, Barrowclough and Haddock2007). The few studies of cannabis (Koen et al., Reference Koen, Kinnear, Corfield, Emsley, Jordaan, Keyter, Moolman-Smook, Stein and Niehaus2004; Moulin et al., Reference Moulin, Baumann, Gholamrezaee, Alameda, Palix, Gasser and Conus2018; Oluwoye et al., Reference Oluwoye, Monroe-DeVita, Burduli, Chwastiak, McPherson, McClellan and McDonell2019) and stimulants (Bell et al., Reference Bell, Greig, Gill, Whelahan and Bryson2002; Miles et al., Reference Miles, Johnson, Amponsah-Afuwape, Finch, Leese and Thornicroft2003; Harris et al., Reference Harris, Large, Redoblado-Hodge, Nielssen, Anderson and Brennan2010) have produced conflicting results. Moreover, these studies have been limited by small samples of inpatients and proxy measures of violent behaviour (e.g. hostility, aggression). A recent meta-analysis of 12 studies involving 3873 subjects with severe mental illness – but not psychotic disorders specifically – reported a significant association between cannabis use and violence [pooled odds ratio (pOR) 3.0, 95% CI 2.0–4.5] (Dellazizzo et al., Reference Dellazizzo, Potvin, Beaudoin, Luigi, Dou, Giguère and Dumais2019). To our knowledge, there have been no studies of depressants (besides alcohol) or hallucinogens.
To address the limitations of previous studies, we have investigated the associations of daily and nondaily use with violent behaviour for cannabis, stimulants, depressants and hallucinogens in two nationwide samples of individuals with psychotic disorders.
Methods
We used baseline data from two research projects: Genetic Risk and Outcome of Psychosis (GROUP) (Korver et al., Reference Korver, Quee, Boos, Simons and de Haan2012) and National Evaluation of the Development and Impact of Early Intervention Services (NEDEN) (Birchwood et al., Reference Birchwood, Lester, McCarthy, Jones, Fowler, Amos, Freemantle, Sharma, Lavis, Singh and Marshall2014).
Setting and participants
GROUP
GROUP is conducted by four university medical centres (i.e. Amsterdam Medical Centre, Maastricht University Medical Centre+, University Medical Centre Groningen, University Medical Centre Utrecht) and affiliated mental health centres (k = 36) in the Netherlands. These centres are located in geographically representative areas of the country and provide access to treatment in a variety of settings (e.g. psychiatric hospitals, outpatient clinics) to approximately 75% of the population. Recruitment took place in 2004. To be eligible for participation, patients had to (i) be aged between 16 and 50, (ii) have a good command of the Dutch language and (iii) meet Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) (American Psychiatric Association, 2000) criteria for schizophrenia or another psychotic disorder. In accordance with standard local practice, DSM-IV-TR diagnoses were made with the Comprehensive Assessment of Symptoms and History (Andreasen et al., Reference Andreasen, Flaum and Arndt1992) or Schedules for Clinical Assessment for Neuropsychiatry (Wing et al., Reference Wing, Babor, Brugha, Burke, Cooper, Giel, Jablenski, Regier and Sartorius1990).
NEDEN
All individuals enrolled into Early Intervention Services (EIS) at five sites across England (i.e. Birmingham, Cornwall, Cambridge, Norwich, Lancashire) between 2005 and 2009 were invited to participate. Sites were chosen to reflect urban and rural differences. The Department of Health and Social Care requires that people receiving EIS are between 14 and 35 years old and present with a first episode of psychosis. No additional inclusion criteria were set. The Operationalized Criteria System (McGuffin et al., Reference McGuffin, Farmer and Harvey1991) was used to determine International Statistical Classification of Diseases and Related Health Problems, Tenth Edition (ICD-10) (World Health Organization [WHO], 1992) diagnoses of mental disorders.
Measures
Information about the instruments' psychometric properties can be found in the relevant publications for GROUP (Korver et al., Reference Korver, Quee, Boos, Simons and de Haan2012) and NEDEN (Birchwood et al., Reference Birchwood, Lester, McCarthy, Jones, Fowler, Amos, Freemantle, Sharma, Lavis, Singh and Marshall2014). Unless otherwise specified, the reference period was the lifetime.
GROUP
Substance use: The Substance Abuse Module of the Composite International Diagnostic Interview (CIDI-SAM) (WHO, 1990) was used to measure the frequency (i.e. daily use, nondaily use, no use) and severity (i.e. problematic use, nonproblematic use, no use) of substance use. The CIDI-SAM distinguishes between the following categories of substances: (i) alcohol; (ii) cannabis; (iii) cocaine; (iv) stimulants (e.g. amphetamine, khat); (v) sedatives (e.g. pentobarbital, diazepam); (vi) opiates (e.g. heroin, codeine); (vii) inhalants (e.g. toluene, butane); (viii) phencyclidine (PCP); (ix) psychedelics [e.g. lysergic acid diethylamide (LSD), mescaline]; and (x) other substances [e.g. amyl nitrite, 3,4-methylenedioxymethamphetamine (MDMA)]. Based on considerations of statistical power and similarities in psychopharmacological effects, we combined cocaine and stimulants as ‘stimulants’, sedatives, opiates and inhalants as ‘depressants’ and PCP and psychedelics as ‘hallucinogens’ (cf. Hill and Thomas, Reference Hill and Thomas2016). Cannabis, which has stimulant, depressive and hallucinogenic properties, was treated separately owing to the high prevalence of its use. We defined problematic alcohol use as an average intake of more than 18 standard drinks per week for men and more than 12 standard drinks per week for women during a minimum period of 2 weeks in the past year or 4 weeks at any other point in the past. These cutoffs reflect the median of several national guidelines and a consistent 1.5:1 male to female consumption ratio (Furtwaengler and de Visser, Reference Furtwaengler and de Visser2013). For other substances, problematic use corresponded to a DSM-IV-TR diagnosis of abuse or dependence.
Violent behaviour: Violent behaviour was established with the Life Chart Schedule (LCS) (Susser et al., Reference Susser, Finnerty, Mojtabai, Yale, Conover, Goetz and Amador2000). Designed to record the development of symptoms, health care consumption and social functioning in schizophrenia patients, the LCS contains the following question regarding violence: ‘Did the patient physically attack or abuse someone else?’ The LCS was filled out based on review of clinical case notes and interviews with the patient and, if possible, one or both parents.
NEDEN
Substance use: A purposely designed questionnaire was used to assess substance use. For 15 substance categories, patients were asked whether they had used them: (i) almost every day; (ii) 1 to 3 times per week; (iii) less than once per week; (iv) 3 times or less; or (v) never. For the sake of consistency, we combined frequency categories ii, iii and iv as ‘nondaily use’ and refer to ‘almost every day’ as ‘daily’. The substance categories were rearranged as follows: (i) cannabis; (ii) stimulants (i.e. cocaine, amphetamine, khat); (iii) depressants (i.e. opiates, γ-hydroxybutyric acid, barbiturates, benzodiazepines, solvents, ‘poppers’); (iv) hallucinogens (i.e. LSD, psilocybin, ketamine); and (v) other substances (i.e. MDMA, ‘other’) (cf. Hill and Thomas, Reference Hill and Thomas2016).
Violent behaviour: Violent behaviour was ascertained from patient and clinician interviews using the Adverse Outcomes Questionnaire (AOQ). In the AOQ, a shortened version of the questionnaire used in the MacArthur Violence Risk Assessment Study (Steadman et al., Reference Steadman, Mulvey, Monahan, Robbins, Appelbaum, Grisso, Roth and Silver1998), violence is operationalized to encompass: (i) battery that resulted in physical injury; (ii) sexual assault; (iii) assault involving the use of a weapon; (iv) threats made with a weapon in hand; and (v) battery that did not result in physical injury. The AOQ referred to the past 12 months.
Analyses
First, we used logistic regression models to estimate the associations of daily and nondaily use with violent behaviour for cannabis, stimulants, depressants and hallucinogens in the GROUP and NEDEN samples separately. Three comparisons were made: (i) daily use v. nondaily or no use; (ii) daily use v. no use; and (iii) nondaily use v. no use. For theoretical reasons, we included the confounders age, sex and educational level (Lamsma and Harte, Reference Lamsma and Harte2015). Educational level, indicating whether a patient had completed secondary school, served as a proxy for socioeconomic status (Maksimović et al., Reference Maksimović, Vlajinac, Radak, Maksimović, Marinković and Jorga2008). We only analysed complete cases. Depending on the scale of measurement, complete and incomplete cases were compared on each model variable with the χ2-test (dichotomous) or t test (continuous). To improve validity, we required models with at least 5 observations per cell in the 2 × 2 table of the exposure and outcome of interest.
We then combined the results for the GROUP and NEDEN samples in random-effects meta-analyses. The I 2 statistic was used as a measure of heterogeneity. Values of 25, 50 and 75% denoted low, moderate and high levels of heterogeneity, respectively (Higgins et al., Reference Higgins, Thompson, Deeks and Altman2003).
For sensitivity analyses, we examined severity of use. Alcohol, which has consistently been found to increase violence risk in people with psychotic disorders (Witt et al., Reference Witt, Van Dorn and Fazel2013), was used as a positive control.
The level of statistical significance was set at 5%. Analyses were carried out in STATA 12.1.
Results
Of the 1013 patients in the GROUP sample, 871 (86%) had data on all model variables and were thus included in the analyses. The corresponding numbers in the NEDEN sample were 1027 and 921 (90%), respectively. Complete cases differed significantly from incomplete cases on age [t (1011) = 3.31, p = 0.001] in the GROUP sample (online Supplementary Table S1) and educational level [χ2 (1) = 3.89, p = 0.049] in the NEDEN sample (online Supplementary Table S2).
Demographic and clinical characteristics of patients
GROUP
Demographic and clinical characteristics of the patients (N = 871) are presented in Table 1. The mean age was 27.3 years (s.d. = 7.1). Most patients were male (n = 673, 77%) and had received a diagnosis of schizophrenia (n = 602, 69%). Use of illicit substances was reported by 602 (69%) patients. About one if five patients had been violent (n = 179, 21%).
Table 1. Demographic and clinical characteristics of patients in the GROUP (N = 871) and NEDEN (N = 921) samples
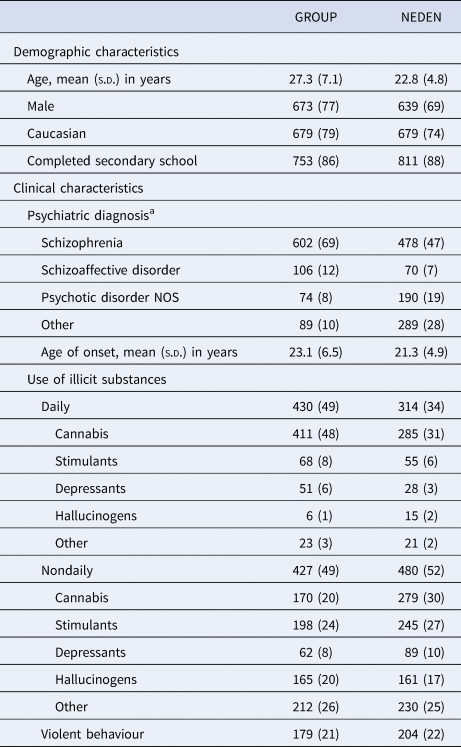
s.d., standard deviation; NOS, not otherwise specified.
Data are n (%), unless otherwise stated.
a Psychiatric diagnoses were only available for the full NEDEN sample (N = 1027).
NEDEN
The patients (N = 921) had a mean age of 22.8 years (s.d. = 4.8) and were predominantly male (n = 639, 69%). (Table 1). The most common diagnosis was schizophrenia (n = 478, 47%). Almost two thirds of the patients had used illicit substances (n = 589, 64%). The prevalence of violent behaviour was 22% (n = 204).
Primary analyses
GROUP
Daily use, compared with nondaily or no use, and nondaily use increased the adjusted odds of violent behaviour for all substance categories (Table 2). The increases were significant for daily use of stimulants [adjusted odds ratio (aOR) 2.2, 95% CI 1.3–3.8] and nondaily use of hallucinogens (aOR 1.8, 95% CI 1.2–2.7).
Table 2. Prevalence and risk of violent behaviour by different categories of illicit substances and frequency of their use in the GROUP (N = 871) and NEDEN (N = 921) samples
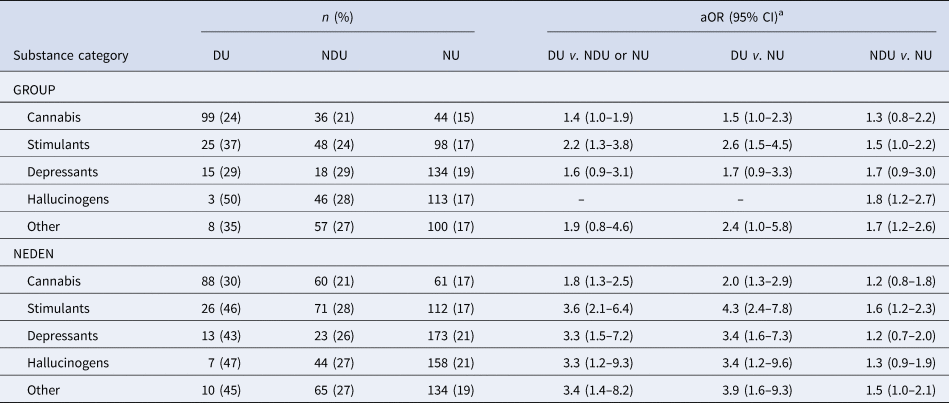
aOR, adjusted odds ratio; CI, confidence interval; DU, daily use; NDU, nondaily use; NU, no use.
Due to missing data, the total number of patients varies by substance category.
a Adjusted for age, sex and educational level.
NEDEN
When comparing daily use with nondaily or no use, cannabis (aOR 1.8, 95% CI 1.3–2.5), stimulants (aOR 3.6, 95% CI 2.1–6.4), depressants (aOR 3.3, 95% CI 1.5–7.2) and hallucinogens (aOR 3.3, 95% CI 1.2–9.3) significantly increased the adjusted odds of violence (Table 2). Nondaily use increased the aORs for these substance categories as well, with that for stimulants reaching statistical significance (aOR 1.6, 95% CI 1.2–2.3).
Meta-analyses
Pooled across the GROUP and NEDEN samples, daily use of cannabis (pOR 1.6, 95% CI 1.2–2.0), stimulants (pOR 2.8, 95% CI 1.7–4.5) and depressants (pOR 2.2, 95% CI 1.1–4.5) significantly increased the odds of violence compared with nondaily or no use (Table 3). The same was found for nondaily use (compared with no use) of stimulants (pOR 1.6, 95% CI 1.2–2.0) and hallucinogens (pOR 1.5, 95% CI 1.1–2.1). Moderate heterogeneity was present for daily use of depressants in both comparisons (I 2 = 46%, 50%). Otherwise, heterogeneity was low (I 2 ⩽ 36%).
Table 3. Risk of violent behaviour by different categories of illicit substances and frequency of their use, pooled across the GROUP (N = 871) and NEDEN (N = 921) samples
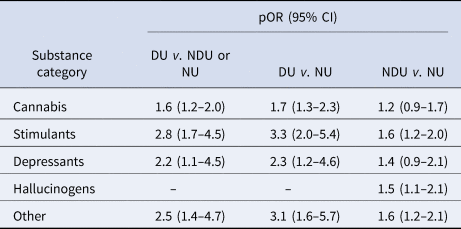
pOR, pooled odds ratio; CI, confidence interval; DU, daily use; NDU, nondaily use; NU, no use (using random-effects models).
Sensitivity analyses
We observed no material differences in results after repeating the analyses in the GROUP sample with severity of use. As expected, alcohol increased the adjusted odds of violence (online Supplementary Table S3).
Discussion
In two nationwide samples totalling 1792 individuals with psychotic disorders, we investigated associations between frequency of use and violence for different categories of illicit substances. Overall, daily and nondaily use of cannabis, stimulants, depressants, and hallucinogens were found to increase violence risk.
There are at least four ways in which substance use may lead to violent behaviour in psychotic disorders. First, psychopharmacological effects of intoxication with or withdrawal from substances (e.g. disinhibition, intensification of negative emotions) may lower the threshold for violence (Kuhns and Clodfelter, Reference Kuhns and Clodfelter2009). Substance use may also induce or exacerbate positive symptoms (e.g. delusions, hallucinations) (Winklbaur et al., Reference Winklbaur, Ebner, Sachs, Thau and Fischer2006), which are risk factors for violent behaviour (Witt et al., Reference Witt, Van Dorn and Fazel2013). This may be particularly relevant for cannabis and hallucinogens. The former has been found to increase the risk of developing a psychotic disorder (Di Forti et al., Reference Di Forti, Quattrone, Freeman, Tripoli, Gayer-Anderson, Quigley, Rodriguez, Jongsma, Ferraro, La Cascia, La Barbera, Tarricone, Berardi, Szöke, Arango, Tortelli, Velthorst, Bernardo, Del-Ben, Menezes, Selten, Jones, Kirkbride, Rutten, de Haan, Sham, van Os, Lewis, Lynskey, Morgan and Murray2019), and the latter – with the possible exception of PCP – are thought not to increase violence risk in the general population (Tomlinson et al., Reference Tomlinson, Brown and Hoaken2016). Second, substance use may interfere with treatment. Individuals with problematic substance use are less likely to seek and adhere to treatment than those without these substance problems (Winklbaur et al., Reference Winklbaur, Ebner, Sachs, Thau and Fischer2006). At the same time, substances may be used in an attempt to alleviate psychotic symptoms or unpleasant side effects of antipsychotics (Gregg et al., Reference Gregg, Barrowclough and Haddock2007). Self-medication increases the likelihood of avoidance or discontinuation of treatment and vice versa (Swartz et al., Reference Swartz, Swanson, Hiday, Borum, Wagner and Burns1998). Substances may also reduce the therapeutic activity of antipsychotics (Lindsey et al., Reference Lindsey, Stewart and Childress2012). In the absence of effective treatment, positive symptoms may persist or worsen. Third, violence may occur during the commission of crimes to gain access to substances or the money to buy them (McGinty et al., Reference McGinty, Choksy and Wintemute2016). Finally, users may become involved in illegal drug markets where violent behaviour is commonplace (Hodgins, Reference Hodgins2008). Other explanations for the findings are confounding or mediation by biological (e.g. genetics, neurobiological abnormalities), psychological (e.g. cognitive impairment, personality pathology) or environmental (e.g. childhood maltreatment, erosion of social support) risk factors (Lamsma and Harte, Reference Lamsma and Harte2015).
As far as we know, this is the largest study to investigate the relationship between use of illicit substances and violent behaviour in psychotic disorders. It has several strengths. First, the samples were drawn from diverse geographic areas and care settings. Sampling was also independent of the exposures and outcome of interest. This enhanced the generalizability of the results. Second, the use of multiple data sources increased the sensitivity of the LCS and AOQ as measures of violence. Finally, the findings for alcohol (as a positive control) were in the expected direction, supporting the validity of the design. However, there are several limitations. First, causality cannot be inferred, as the temporal relationship between substance use and violent behaviour was not known and we did not control for other confounders besides age, sex and educational level. Second, we included individuals who had used substances belonging to different categories, which may have biased risk estimates. Exclusion would have made cell counts too low for meaningful analyses of most substance categories. Third, daily use was a proxy measure of SUD. However, similar results were obtained for DSM-IV-TR diagnoses of abuse and dependence in the GROUP sample. Fourth, the definition and reference period for violence varied between GROUP and NEDEN. The more stringent definition and shorter reference period may explain why aORs were slightly higher in the NEDEN sample. Fifth, missing data may have limited the validity of the results. Sixth, the results of the meta-analyses should be treated with some caution: the estimation of the between-study variance, which is used in the calculation of the pooled effect size and its confidence interval, may be inaccurate when the number of studies is small (Borenstein et al., Reference Borenstein, Hedges, Higgins and Rothstein2009). Seventh, we were unable to analyse PCP separately. Either too few patients had used PCP (GROUP) or no specific information was recorded for PCP (NEDEN). Finally, there has been a large increase in the use of novel psychoactive substances (NPS) in the years following data collection (Tracy et al., Reference Tracy, Wood and Baumeister2017). NPS are synthetic compounds designed to mimic the psychopharmacological effects of traditional substances (Miliano et al., Reference Miliano, Serpelloni, Rimondo, Mereu, Marti and De Luca2016). Therefore, we hypothesize that NPS increase violence risk.
A clinical implication of the findings is that violence risk assessment in psychotic disorders should target any substance use. For structured instruments, it should be determined whether items for SUD and subthreshold use of different substance categories have incremental validity over a single item for SUD. The findings also suggest that interventions, which currently focus on SUD, may assist in the prevention of violent behaviour in patients with subthreshold use (Chang et al., Reference Chang, Lichtenstein, Langstrom, Larsson and Fazel2016). To clarify causal mechanisms, we recommend that studies further isolate the psychopharmacological effects of substances, use prospective designs and test for additional confounders and mediators.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291719002125.
Financial support
GROUP was funded by the Geestkracht programme of The Netherlands Organisation for Health Research and Development (10-000-1001) and matching funds from the coordinating university medical centres (i.e. Academic Medical Centre, Maastricht University Medical Centre+, University Medical Centre Groningen, University Medical Centre Utrecht), their affiliated mental health centres (i.e. Altrecht, Arkin, Delta, Dimence, Dijk en Duin, Erasmus UMC, GGNet, GGZ Breburg, GGZ Centraal, GGZ Drenthe, GGZ Eindhoven en De Kempen, GGZ Friesland, GGZ inGeest, Mondriaan, GGZ Noord-Holland-Noord, GGZ Oost-Brabant, GGZ Overpelt, GGZ Rivierduinen, Lentis, Mediant GGZ, Met GGZ, Parnassia Psycho-Medical Centre, Psychiatric Centre Ziekeren, Psychiatric Hospital Sancta Maria, Public Centre for Mental Health Rekem, The Collaborative Antwerp Psychiatric Research Institute, Vincent van Gogh voor Geestelijke Gezondheid, Virenze riagg, University Psychiatric Centre Sint Jozef, Yulius, Zuyderland GGZ) and participating pharmaceutical companies (i.e. Lundbeck, AstraZeneca, Eli Lilly, Janssen Cilag). NEDEN was funded by the United Kingdom Department of Health and Social Care (PO261680). JL received funding from the Prins Bernhard Cultuurfonds and Dr Hendrik Muller Fonds. SF is funded by a Wellcome Trust Senior Research Fellowship in Clinical Science (202836/Z/16/Z).
Conflict of interest
None.





