Introduction
Helical tomotherapy (TOMO; Accuray Incorporated, Sunnyvale, CA, USA)Reference Mackie, Balog and Ruchala1, Reference Mackie2 is a relatively new modality with integrated treatment planning and delivery hardware for radiation therapy treatments.Reference Langen, Papanikolaou and Balog3 The TOMO delivery system consists of a 6-MV linear accelerator mounted on a computed tomography (CT)-like ring gantry. Therapeutic radiation is delivered using a rotating fan beam that is modulated by a multi-leaf collimator (MLC) system while the patient moves through the gantry in the longitudinal direction.Reference Mackie, Holmes and Swerdloff4 The therapy combines intensity-modulated radiation therapy treatment delivery and megavoltage CT (MVCT) imaging capabilities to integrate the treatment planning, patient set-up and treatment process. TOMO’s clinical application is extensive; not only can it treat head and neck (HN) tumours with anatomical complexityReference Nguyen, Vos and Vinh-Hung5 and chest–abdomen tumoursReference Goddu, Chaudhari and Mamalui-Hunter6, Reference Hsieh, Wei and Lee7 with proximity to vital organs at risk (OARs), but it can also be used to treat brain metastases,Reference Nagai, Shibamoto, Yoshida, Wakamatsu and Kikuchi8 craniospinal tumours,Reference Bauman, Yartsev, Coad, Fisher and Kron9 central nervous system tumoursReference Hui, Kapatoes and Fowler10 and multiple tumours in different locations of the body. TOMO was first introduced in mainland China in 2007. Information on its long-term clinical application is therefore somewhat incomplete. Moreover, there is a shortage of surveys of TOMO’s current application status both domestically and abroad. Here, we report the results of a survey examining the utilisation and management of TOMO clinical programmes in mainland China and the level of user satisfaction with the technology. Our aim was ultimately to promote radiation treatment capabilities and developments in China, overall.
Methods
The survey examined hospitals in mainland China that commenced treatments with TOMO before 30 April 2016. The survey covered China’s 31 provinces, municipalities and autonomous regions. Hong Kong, Macau and Taiwan were excluded.
The survey stages were as follows: (1) initial planning of the survey’s content; (2) finalization of the content based on discussions with experts in hospitals equipped with TOMO, including the distribution of installation and staffing levels, types of cancers treated, utilisation efficiency, quality assurance, maintenance, optional features and satisfaction levels; (3) sending the survey questionnaires to each hospital by e-mail, where designated staff members completed and returned the surveys; (4) examining, cross-checking, normalising and standardising the data, as well as establishing a database; and (5) collecting the data through a census and analysing the data qualitatively and quantitatively.
Results
Distribution of installation and staffing levels
From the first TOMO installation in September 2007 to date, 22 hospitals in mainland China have installed 23 TOMO units for clinical application. Figure 1 presents the cumulative numbers of TOMO units installed by year. After the first introduction in 2007, no additional TOMO units were introduced until 2011. Since then, several new installations have occurred each year, with a peak of seven installations in 2015. At the end of 2015, there were a total of 1,931 linear accelerators that conducted radiation therapy in mainland China,Reference Wang, Lu, Yin and Lang11 which puts TOMO’s percentage at 1·2%.
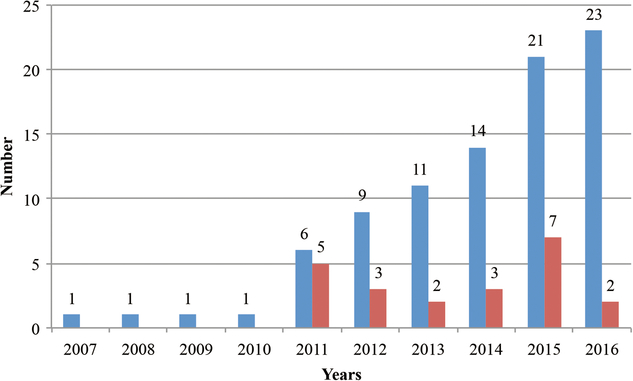
Figure 1. Cumulative installations of TOMO in mainland China by year.
Table 1 displays basic information on the TOMO units installed in mainland China, including geographical location, the category and function of the corresponding hospital, the number and model of the equipment, and the start date of the clinical application. All of the TOMO units are distributed to top-level hospitals. In terms of hospital function, 13 are installed in polyclinics (including eight in military hospitals), and 10 are installed in oncology-specialised hospitals. Sixteen TOMO units have been in clinical use for more than a year by 30 April 2016. Regarding geographical distribution, these units are located in Beijing, Shanghai, Guangdong, Jiangsu, Hubei, Zhejiang, Liaoning, Shandong, Sichuan, Hunan, Fujian, Yunnan and Henan. Figure 2 displays the geographical distribution and the corresponding quantity across mainland China. Notably, there are six units installed in Beijing, accounting for 26·1% of all installations in the country.
Table 1. Basic information on TOMO units installed in mainland China


Figure 2. Geographical distribution and quantity of TOMO units in mainland China.
The 534 employees associated with TOMO units in mainland China consist of 172 radiation oncologists (including 61 senior staff), 57 medical physicists (including 7 senior staff), 128 therapists, 167 nurses and 10 engineers. Previous work reported that at the end of 2015, there were 52,496 employees and staff members associated with radiation therapy in mainland China, including 15,841 radiation oncologists (4,824 senior staff), 3,294 medical physicists (562 senior staff), 8,454 therapists, 23,152 nurses and 938 engineers.Reference Wang, Lu, Yin and Lang11 TOMO staffing levels accounted for only 1·0% of these employees, corresponding to TOMO’s percentage of all radiation therapy equipment. The ratio of radiation oncologists to medical physicists among TOMO staffing levels in mainland China is 3:1, which surpasses the 4·8:1 at national level reported in the previous work,Reference Wang, Lu, Yin and Lang11 but remains lower than the United States ratio of 1·2:1.Reference Chen, Arnone, Sillanpaa, Yu and Mills12–15 (Note: medical physicists in mainland China include dosimetrists and physicists, while in the United States, only physicists). Hence, it can be concluded that medical physicists are in high demand in mainland China, compared with the situation in developed countries.
Types of cancers treated
A total of 22,558 cancer patients by 30 April 2016 have received TOMO treatment in mainland China, including 18,186 primary tumour cases and 4,372 metastatic tumour cases. The top three primary tumour types treated with TOMO are nasopharyngeal carcinoma (19·2%), pulmonary cancer (16·0%) and other HN cancers (15·2%), together accounting for 50·4% of all primary tumour cases. The top three metastatic tumour types treated with TOMO are brain metastases (28·4%), lung metastases (17·5%) and liver metastases (10·5%), together making up 56·4% of all metastatic tumour cases (as illustrated in Figure 3). TOMO treatment covers a wide range of tumours and primarily focuses on complex tumours such as HN cancer and regular cases of pulmonary cancer.
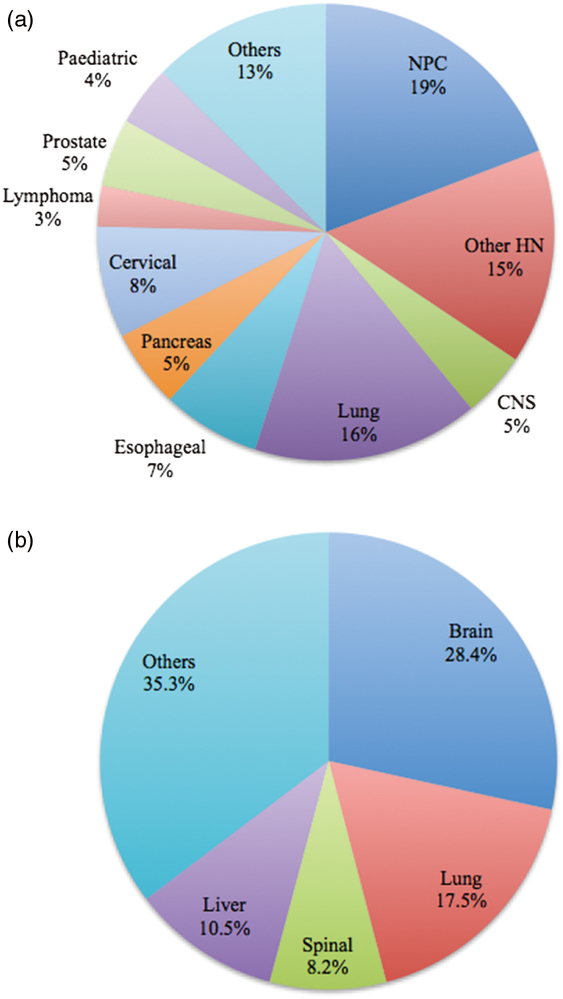
Figure 3. (a) Primary and (b) metastatic cancers treated by TOMO.
Utilisation efficiency
Table 2 presents the average number of patients treated per year, the average hours of effective operation per day, the average treated patient headcount per day and the average treatment time per person. For TOMO units with over a year of clinical use, the average number of annual treatments is in the range of 365 ± 114 (median = 378, minimum = 162, maximum = 534); average daily operation time is within the range of 9·9 ± 2·6 (median = 10·5, minimum = 5·5, maximum = 14·0), average daily treatment headcount is within the range of 37·4 ± 10·2 (median = 38·3, minimum = 20·0, maximum = 50·0) and average treatment time per person is within the range of 16·3 ± 3·1 (median = 15·9, minimum = 11·7, maximum = 23·3).
Table 2. Application efficiency. 1, Average number of patients treated per year; 2. Average hours of operation per day; 3, Average treatment headcount per day; 4. Average treatment time per person
Note: * indicates an actual value under 1 year of clinical use; otherwise the average annual value was more than a year.
The average daily operation time should be 11 hours, considering the machine’s warm-up and maintenance requirements. Assuming the regular daily working time is 8 hours, the TOMO units in majority of hospitals are overloaded. Foreign TOMO units’ full capacity is about 20 patients per day, which puts the units in mainland China at twice the full capacity. The number of patients treated may affect the quality of care, and such operational overload undoubtedly jeopardises quality assurance and safety.
Quality assurance
For TOMO units with over a year of clinical utilisation, the results are based on data from the most recent year; for units with under a year of clinical utilisation, the results are based on actual values. There were 6,239 annual dosimetry check plans of the TOMO units in mainland China. The average annual dosimetry check plans per machine are 326 ± 160 cases (median = 293, minimum = 30, maximum = 632) for units with over 1 year of clinical use. The overall passing rate (the ratio of plans that passed check to total) was 98·2% ± 2·4 (median = 99·0%, minimum = 92·1%, maximum = 100%). In total, 16 of the units checked all plans and 7 checked plans partially. The phantoms used for dosimetry check were the ‘cheese’ phantom (Accuray Incorporated, Sunnyvale, CA, USA) (13 TOMO units), ArcCheck (Sun Nuclear Corporation, Melbourne, FL, USA) (9), Delta4 (ScandiDos, Uppsala, Sweden) (3) and cylindrical solid water (2). The detectors used were ion chamber (13 TOMO units), film (9) and semiconductor (5). The passing standard for the tested units were 95%/±3mm/3% (16 TOMO units), 90%/±3mm/3% (6) and 95%/±2mm/2% (1).
Figure 4 presents the causes of dosimetry check failures in the most recent year. The most frequent causes of dosimetry check failures are measurement factors (i.e. film or scanner factors, problems with the ion chamber location), special cases (i.e. complex cases, large fraction and stereotactic body radiation therapy cases), and delivery quality assurance (DQA) problems.
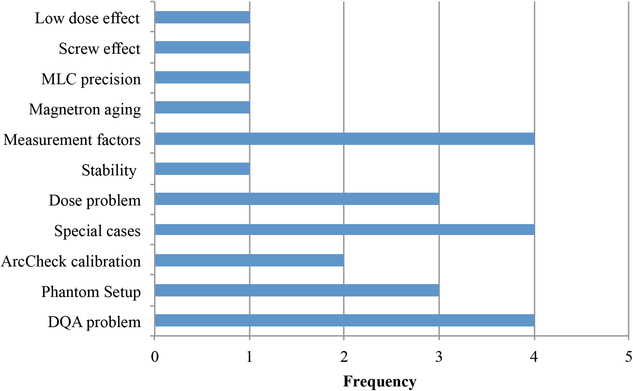
Figure 4. Causes of dosimetry check failures.
For daily, weekly, monthly, and annual inspections, the average time consumption was 0·5 ± 0·3, 1·1 ± 0·9, 3·0 ± 2·1 and 9·1 ± 6·2 hours, respectively. The most frequent quality assurance issues were problems involving the laser. Other problems included the percent deviation in depth-dose, 1-cm treatment plan with a low passing rate, serious sinking of the treatment couch after long-term usage, difficulties in operating the original factory-supplied dosimetry check phantom, high cost of non-rinsed film and problems adjusting the horizontal line for the two dimensions water tank.
Maintenance
The common malfunctions of the TOMO units in mainland China during 1 year included uninterruptible power supply (UPS), ventilator, laser, control panel, microwave system, treatment couch, air compressor, MVCT, accelerator waveguide, solid-state modulator, flow failures, on-board computer and stationary computer, jaw, data server and network, dose control system, magnetron, MLC and gantry. The most frequent occurrence of a malfunction was in the MLC (14 TOMO units). An analysis of the cause of this breakdown indicated that patients receiving TOMO treatment generally required intensity-modulated radiation therapy. Consequently, the MLCs are frequently modulated during treatment. The movement is very fast (60 m/s) and the brakes need to be applied in time. This results in the MLC’s brake components being overheated during continuous treatment. This condition tends to produce more damage compared with non-continuous treatment.
Figure 5 presents the information about the treatment delay time and malfunction rate of TOMO units in mainland China in 1 year and includes data extracted from 22 TOMO units (actual values are employed for units with under a year of clinical use). Treatment delays caused by breakdowns were an average of 95·6 ± 111·4 hours in duration (median = 63·5), and the average breakdown rate was 4·3% ± 3·8 (median = 2·6%). As indicated by these data, the overall breakdown rate was within an acceptable range, with specific cases of slightly higher rates. These cases were directly related to factors such as overloaded system operations, records of treatment delay times and actual daily working hours.
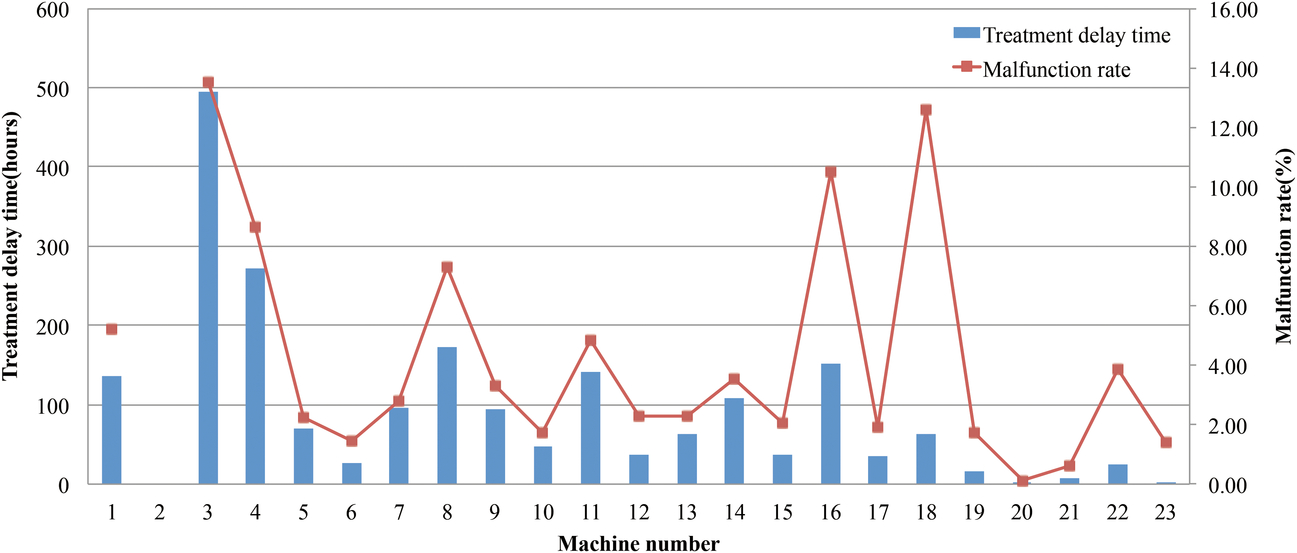
Figure 5. Treatment delay time and malfunction rate of TOMO units over 1 year.
Optional features
There are nine optional features for TOMO units. It is clear that there are varied configuration options across hospitals. In terms of feature options, six units of TOMO (26·1% of the total TOMO units surveyed) were equipped with all nine features.
Table 3 shows the optional features activated, frequency of application and effect of each feature. The frequency of use was assessed as ‘always’, ‘frequently’, ‘occasionally’ or ‘never’. The usefulness of the option was rated as ‘excellent’, ‘good’, ‘average’ or ‘lacking’. The top three features in terms of the varied configuration options were adaptive treatment planning, 1-cm treatment beam and additional planning workstation. Features with most frequently used were VoLo computing system, additional planning workstation, digital imaging and communications in medicine-radiotherapy (DICOM-RT) export, and operator station couch control. Features with used least often were 1-cm treatment beam, adaptive planning software and TomoDirect mode. The most useful options were additional planning workstation, DICOM-RT export and operator station couch control.
Table 3. Optional features activated, frequency of application and effect of each optional features of the TOMO units

Abbreviations: TOMO, helical tomotherapy; OSI, Open System Interconnection Reference Model; DICOM RT, Digital Imaging and Communications in Medicine Radiotherapy; TQA: tomotherapy quality assurance.
Satisfaction levels
Table 4 summarises the medical staff members’ satisfaction levels with TOMO units in mainland China. Surveyed factors included distribution of installation and staffing levels, types of cancers treated, application efficiency, treatment planning system (TPS), treatment planning verification, quality assurance, maintenance and repairmen, costs and overheads, optional features, and overall satisfaction level. Respondents to the questionnaires rated their satisfaction levels across five categories: ‘very satisfied’, ‘satisfied’, ‘average’, ‘unsatisfied’ and ‘extremely unsatisfied’.
Table 4. Satisfaction levels regarding TOMO units in mainland China

Abbreviations: TOMO, helical tomotherapy; MVCT, megavoltage computed tomography; TPS, treatment planning system; OARs, organs at risks.
For overall satisfaction level, the results showed that 3 hospitals were very satisfied, 16 were satisfied and 3 considered their satisfaction level average. Satisfaction was highest in terms of the versatility TOMO units offered for various types of cancers treated, the capability to address complex cancers, the level of difficulty in operations, the level of difficulty in designing treatment plans, the level of conformity and homogeneity of targets, the protection of vital OARs, the time consumption of quality assurance and the frequency of breakdown occurrence. Dissatisfaction was highest for the TPS’s contouring tools, the MVCT image quality, the dose drop-off in the head and foot direction, the low-dose region, maintenance costs, equipment costs, payment standards, optional features fees and the cost effectiveness of the optional features.
Discussion
The results of this survey demonstrate an overall favourable application status for TOMO in mainland China. Clients responded with high levels of satisfaction: 86·4% of all hospitals were satisfied or higher. The majority of hospitals run the system at full or even overloaded capacity. The median actual daily working time is 10·5 hours, with the longest being 14 hours, and an individual case running up to 23 hours. We suggest increasing the allocation quota of TOMO which is governed by Chinese Health Ministry on the medical devices with its huge capital investment, high running cost and high demand of technical support during Chinese government 13th Five-Year Plan period accordingly. Further allocation should effectively respond to the regional market demand and the medical requirements of patients. Hospitals with technological advantages and high levels of demand from patients should be prioritised to reduce limitations caused by inefficient allocation based on region and existing equipment.
All existing TOMO units are installed in public high-end hospitals. The overall staffing level is beyond the national average, but two problems remain. First, seven hospitals lack a senior medical physicist, and one hospital has no senior radiation oncologists. Second, there is a shortage of medical physicists. According to a 2012 white paper of the American Society for Radiation Oncology, (Safety is No Accident),Reference Zietman, Palta and Steinberg16 three medical physicists and two dosimetrists per accelerator should be employed to conduct precise radiation therapy. The current number for each TOMO unit in mainland China is an average of 2·5 personnel, which reflects a significant shortage, considering that TOMO units are advanced radiotherapy equipment that are technologically complex and have a high level of quality assurance standards. Therefore, more medical physicists are essential. However, the physicist training programmes are not well organised and career developing path for physicists are not clear in mainland China, there is no job title of ‘medical physicist’ existing in the current Chinese healthcare professionals. This fact subsequently leads to human resource insufficiencies. We suggest creating a series of titles for medical physicists, allocating at least one senior medical physicist to each hospital that conducts precise radiotherapy, and employing additional medical physicists based on equipment status and patient demand.
Each of the studied hospitals conducts effective quality assurance work and reports few problems in this regard. We suggest that each department should continuously conduct effective supervision, formulate and introduce quality assurance standards and guidelines for TOMO, and actively promote and periodically revise these documents. This will enhance national capabilities in terms of quality assurance and equipment management of TOMO units. In this process, guidance and help should be provided, with priority given to hospitals with relative disadvantages. We also suggest that national department heads take a leadership role to create full-cycle dynamic supervision and management systems that ensure coordination and cooperation within the sector and the formulation of standards regarding TOMO’s clinical operations.
From the introduction of first TOMO system in September 2007 to the date of the most recent statistical information, 22,558 cancer patients across the nation have been treated via TOMO. However, the statistics on the treatment’s clinical effectiveness are insufficient. We suggest that each hospital should actively engage in clinical research, identify and prioritise the appropriate patient population, rationally utilise TOMO units, establish collaborative units, standardise clinical usage and enhance the application efficiency of the equipment.
The field of radiation therapy within mainland China has seen significant development. Progress has been demonstrated in terms of both distribution of installation and staffing levels, and the accessibility of radiotherapy at the national scale has been improved significantly. However, a large gap remains between actual cancer patients’ treatment needs and the configuration/structure of personnel and equipment. Especially considering the disparity between China’s technical capability for advanced radiotherapy and that of developed countries, improving the overall level of radiotherapy remains a challenging task.
Conclusions
The present results reflect the application status of TOMO in mainland China. The overall operation is good, but there are some problems regarding running at full capacity, lacking clinical efficacy research and insufficient quality assurance regulations. It is recommended that the allocation be increased appropriately during the 13th Five-Year Plan period. Additional recommendations are proposed in terms of conducting more clinical research and implementing regulations for quality assurance.
Author ORCIDs
Zhiqiang Liu 0000-0003-2135-8581
Acknowledgements
Zhiqiang Liu performed the analysis and drafted the manuscript. Luhua Wang and Jianrong Dai were involved in the overall conception and design of this study, analysis and interpretation of data, and revising and finalising the manuscript. Tinglin Qiu was involved in the design of the study and revising the manuscript. Ye Zhang was involved in the acquisition, analysis and interpretation of data. Jufang Shi was involved in the design of the study and analysis of data. Zhihui Hu was involved in the design of the study and acquisition of data. Bo Chen and Ting Gao were involved in the acquisition of data. All authors are in agreement with the content of the manuscript. We thank all the units involved in the research. We thank Jennifer Barrett, PhD, from Liwen Bianji, Edanz Group China (www.liwenbianji.cn/ac), and Dr Lisa Goggin and Dr Jiuhong Chen (Accuray Incorporated) for editing the English text of a draft of this article.
Financial support
This study was supported by grants from International Exchange and Cooperation Center, National Health Commission of the People’s Republic of China, during the conduct of the study.
Conflicts of interest
The authors declare that they have no competing interests.











