INTRODUCTION
Clostridium difficile, a spore-forming and Gram-positive bacterium produces two major diarrhea-producing toxins, which are toxin A (TcdA) and toxin B (TcdB) [Reference Carter, Rood and Lyras1]. The genes for these toxins, tcdA and tcdB, are not carried by non-toxigenic C. difficile strains. Completely non-toxigenic strains of C. difficile do not cause disease. Some strains of C. difficile produce a third toxin, a binary toxin (CDT), the significance of which remains controversial [Reference Eckert2]. Since C. difficile is one of the most common nosocomial infections worldwide [Reference Martin, Monaghan and Wilcox3–Reference Sartelli5], colonization with toxigenic or non-toxigenic C. difficile is higher in hospitalized patients than in healthy adults (i.e. 20–40% vs. 2–3%) [Reference Heinlen and Ballard6]. More than 90% of C. difficile infection (CDI) occurs after or while patients on antimicrobial therapy [Reference Barbut, Jones and Eckert7]. On the other hand, asymptomatic colonization in the adult and elderly communities has been more variable with prevalence ranging from 0% to 51% [Reference Furuya-Kanamori8].
The prevalence of CDI has increased significantly over the past two decades [Reference Lo Vecchio and Zacur9]. A Canadian nosocomial surveillance project reported a fourfold increase in the incidence of CDI from 22·2 cases per 100 000 population to 92·2 cases per 100 000 population from 1998 until 2006 [Reference Gilca10]. Moreover, certain strains of C. difficile cause more severe infection, especially ribotypes (RTs) 027 and 078 [Reference Vedantam11]. RTs 027 and 078 produce TcdA and TcdB in higher quantities than other strains, and a third binary toxin (CDT) probably due to the mutated TcdC protein [Reference Carter12], although this may be irrelevant in terms of disease pathogenesis. Diagnosis of CDI requires detection of toxin in diarrheal stool [Reference Crobach13]. The quickest and cheapest method of toxin detection is by enzyme immunoassay (EIA). Otherwise, culture and/or PCR detection of tcdB are effective ways to detect toxigenic C. difficile, but may not differentiate colonized patients from infected patients.
Although data on the epidemiology of CDI in North America and Europe are plentiful, limited data are available for the rest of the world, particularly Asia [Reference Collins, Hawkey and Riley14]. This is because comprehensive diagnostic testing for C. difficile is lacking in many Asian hospitals. In addition, it is perceived that awareness of CDI among physicians especially outside the Western hemisphere is low [Reference Mavros15]. There have been only five papers published on C. difficile in Malaysia and, of these, three were published prior to 1997 [Reference Boey, Ramanujam and Looi16–Reference Parasakthi18]. Although Hassan et al. reported a hospital prevalence of 14% by toxin EIA [Reference Hassan19], Syuhada et al. reported a lower prevalence of 6% [Reference Syuhada20], and the differences might be because of low awareness and testing of CDI, or differences in patient populations. No data on carriage of C. difficile by the elderly in the community are available in Malaysia but these data may be important to help explain the high prevalence of CDI reported in hospitals.
Therefore, the aims of our study were: (1) to investigate the prevalence, associated risk factors and ribotyping of C. difficile in hospitalized patients; (2) to determine the carriage rate of C. difficile and associated risk factors in an elderly community and (3) to explore awareness of CDI among staff and students in a tertiary academic hospital.
MATERIALS AND METHODS
Hospital study population
Inpatients from the only tertiary academic hospital (Hospital Universiti Sains Malaysia, Kota Bharu, Kelantan) in the north-eastern region of Peninsular Malaysia were recruited from April 2015 to September 2015. They were aged between 18 and 80 years, with or without antibiotic-associated diarrhea within 48 h of hospital admission (either the acute-care hospital or long-term care facility that provided skilled nursing care for ⩾1 overnight stay) and those suspected to have CDI. The duration of hospitalization was defined as time from admission until discharge. The 48 h was selected according to a surveillance definition paper by McDonald et al. [Reference McDonald21]. Those who were unable to provide stool samples due to medical or psychiatric reasons were excluded from study. Data entry collection forms for eligible participants were completed by interviewing or reviewing their case notes, and radiological and microbiological data.
Community study population
Elderly people aged between 60 and 90 years were recruited between July 2015 and September 2015 from two randomly selected communities of Tumpat and Kota Bharu districts and from an aged residential care facility in Kota Bharu. Exclusion factors were a history of healthcare contact within the 12 weeks prior to enrolment, or previous hospitalization due to C. difficile in the last 28 days, or current suspicion of CDI and inability to provide stool sample. Questionnaires were completed through interviews of eligible elderly participants by a trained research assistant.
Awareness survey population
University hospital staff (i.e. doctors, non-clinical medical professionals and paramedics) and students (i.e. undergraduates and postgraduates) who were involved with in-hospital patient care were surveyed during a workshop. They were asked to answer a Malay language structured questionnaire comprising of five multiple-choice questions with a single answer, as reported by Mavros et al. [Reference Mavros15]. Briefly, the first four questions were related to CDI awareness which included knowledge of likelihood of treatment failure or recurrence after first episode of treated C. difficile-associated diarrhea (CDAD), knowledge of approximate percentage of antibiotic-associated colitis due to C. difficile, knowledge of antibiotic(s) that put(s) patient at risk for CDAD and knowledge of the type of patients with diarrhea that may have CDAD. The last question asked about the respondent estimation of CDAD frequency and morbidity in his or her current clinical practice.
Laboratory analysis
Once stool samples were collected from hospital inpatients and community participants, they were stored at 2–8 °C in the microbiology laboratory of the same hospital and analyzed within 24 h. The stool samples were tested for C. difficile glutamate dehydrogenase (GDH) antigen and toxin using the C. DIFF QUIK CHEK COMPLETE® rapid test EIA kits (Techlab, Blacksburg, Virginia, USA) [Reference Eckert2].
Stools were also sent in Cary Blair transport medium at ambient temperature to the Microbiology Department of PathWest Laboratory Medicine in Perth, Australia for further tests as described in Putsathit et al. [Reference Putsathit22]. The gold standard was toxigenic culture, and this was performed by direct plating the stool samples onto ChromID C. difficile agar (bioMérieux, Marcy l'Etoile, France). Selective enrichment was also undertaken in Robertson's cooked meat broth supplemented with gentamicin, cefoxitin and cycloserine and with addition of taurocholic acid as a germinant. All agar plates were incubated at 35 °C in an A35 anaerobe chamber (Don Whitley Scientific, Otley, West Yorkshire) for up to 48 h. Putative colonies of C. difficile were sub-cultured onto pre-reduced blood agar plates and identified by their morphology, horse-dung odor and chartreuse (yellow-green) fluorescence under 360 nm UV light. Ambiguous colonies were further tested with Gram staining and the L-proline amino peptidase test.
All isolates were screened for tcdA and tcdB genes, binary toxin (cdtA and cdtB) genes and for changes in repeating region of tcdA using PCR [Reference Kato23–Reference Stubbs25]. Products were run on the QIAxcel capillary electrophoresis platform and visualized on the QIAxcel ScreenGel software (Qiagen, Germany). Ribotyping was performed by PCR [Reference Stubbs26]. BioNumerics Software package v.6.5 (Applied Maths, Saint-Martens-Latem, Belgium) was used for dendrogram and cluster analysis of PCR ribotyping band patterns using Dice coefficient. PCR ribotyping banding patterns were identified by comparison of patterns with a reference library consisting of a collection of 30 reference strains from the European Centre for Disease Prevention and Control (ECDC), a collection of the most prevalent PCR RTs currently circulating in Australia (many of which are published), and a selection of binary toxin-positive strains which included RTs 027 and 078. Isolates that could not be assigned a RT were designated with internal nomenclature (prefix QX). Once all the tests were completed, stool samples were disposed in accordance to standard operating procedure of the laboratory.
Significance of test results
C. difficile was considered present if the GDH antigen and/or direct culture were positive. If the GDH antigen was negative but a toxigenic strain of C. difficile was isolated, the GDH result was deemed a false negative. A positive EIA result for toxin or isolation of toxigenic C. difficile was considered to indicate the presence of CDI.
Ethical approval
These studies were approved by the Universiti Sains Malaysia (USM) human research and ethics committee (Ref. no: USM/JEPeM/14080295). Study consent from the relevant authorities (i.e. the directors from the hospital and the aged residential care facility, respectively) were also obtained for the studies prior to commencement.
Statistical analysis
For the hospital study, participants who had C. difficile were categorized either to non-toxigenic C. difficile colonization and CDI based on our laboratory analysis. Analysis was performed using IBM Statistical Package for Social Sciences (SPSS) version 20.0 (IBM Corp., New York, USA). Numerical variables were expressed as mean ± standard deviation (s.d.) and the values of categorical variables were summarized by frequency and percentage. In the univariate analysis, χ 2 was used to assess for independent variables associated with non-toxigenic C. difficile colonization and CDI. A P-value < 0·05 was used to indicate good fitting of the models.
RESULTS
Hospital study
In total, 76 participants (mean age 45 ± 19 years, 50% females) were recruited and 29% of them (n = 22) were elderly (i.e. ⩾60 years). By EIA, 26% of the 76 stool samples (n = 20) were positive for GDH, and of the 20 positive samples, 9% (n = 7) were positive for toxin. By culture, 19 (16 positive by direct culture, additional three positive by enrichment only) out of 76 stool samples (25%) were positive for C. difficile, seven of which were toxigenic (7%). Overall, the prevalence of CDI and non-toxigenic C. difficile colonization was 13% (n = 10) and 16% (n = 12), respectively, and among the elderly, 4% (n = 3) and 7% (n = 5), respectively. There was no significant difference between non-toxigenic C. difficile colonization and CDI in prevalence for the overall group (P = 0·67) and the elderly (P = 0·48).
When compared to toxigenic culture (i.e. culture followed by tcdB PCR) as the reference method, the sensitivity, specificity and negative predictive value of the EIA for GDH were 0·84 (95% confidence interval (CI) 0·59–0·96), 0·93 (0·82–0·97), 0·95 (0·84–0·99), respectively. When compared to toxigenic culture, the sensitivity, specificity and negative predictive value of toxin detection were 0·32 (CI 0·14–0·57), 0·98 (CI 0·89–0·99), 0·81 (CI 0·69–0·89), respectively.
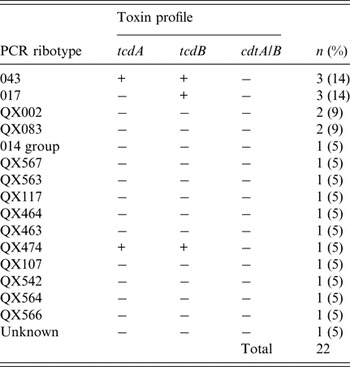
Of the 19 positive cultures, two distinct isolates were identified in three specimens giving a total of 22 strains. Of these 22 strains, RT 043 (14%) and RT 017 (14%) were the most common (Table 1).
Table 1. Summary of Clostridium difficile PCR ribotypes and toxin profiles in hospitalized participants
History of prior use of antibiotics was significantly associated with non-toxigenic C. difficile colonization (P < 0·001) and CDI (P < 0·001). The most commonly used antibiotics were penicillin (37%), followed by cephalosporin (29%), carbapenem (15%), macrolide (5%), metronidazole (4%), fluoroquinolones (4%), aminoglycoside (1%) and vancomycin (1%). Of these antibiotics, non-toxigenic C. difficile colonization was associated with penicillin and carbapenem (both P < 0·05) and CDI with penicillin and cephalosporin (both P < 0·05). A proton pump inhibitor (PPI) was prescribed for 40% of participants and a history of prior use of a PPI was significantly associated with non-toxigenic C. difficile colonization (P = 0·02) and CDI (P = 0·02).
Table 2 shows risk factors and clinical presentations associated with the prevalence of C. difficile. Duration of hospitalization, presence of underlying medical illnesses and increasing Charlson Comorbidity Index were significantly associated with non-toxigenic C. difficile colonization (all P < 0·05). On the other hand, duration of hospitalization and use of nasogastric tube were significantly associated with CDI (all P < 0·05). Fever (temperature >38 °C) was the only symptom that was significantly associated with CDI (P = 0·015). Of the clinical parameters, lower mean of albumin and higher CRP levels were significantly associated with both non-toxigenic C. difficile colonization (all P < 0·05) and CDI (all P < 0·05).
Table 2. Comparison between prevalence of Clostridium difficile with risk factors and clinical presentations in hospitalized participants
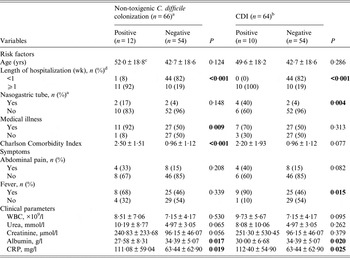
Figures with significant p values are indicated in bold. CRP, C-reactive protein; WBC, white blood cells; wk, weeks; yrs, years.
a CDI cases were excluded from the non-toxigenic C. difficile colonization total.
b Non-toxigenic C. difficile colonization cases were excluded from the CDI total.
c Mean ± s.d. (all such values).
d Due to rounding, the total may not add to 100% exactly.
Community study
With a high prevalence of C. difficile found among elderly in the hospital study, we continued with the community study to observe if there was a similar trend. There were 138 elderly subjects who consented to the study and 78% (n = 108) were of ethnic Malays. There was an equal distribution of gender between participants (females 51% (n = 71) and males 49% (n = 67)). The mean age was 72 ± 8 years. Only 6% of participants (n = 8) used a PPI and 3% of participants (n = 4) had a recent hospital admission within 12 weeks. Of 4% of participants (n = 5) who reported the use of antibiotics, most (80%) took penicillin followed by macrolide (20%). Most participants (94%) did not have symptoms. Only 1% (n = 2), 2% (n = 3) and 3% (n = 4) of participants reported that they had experience of abdominal pain, diarrhea and fever, respectively.
Of the 138 stool samples, nine were discarded because they were inadequate, leaking or overflowing. The remaining 129 samples were analyzed. The prevalence of GDH, toxin by EIA and C. difficile by direct culture was 2% (n = 2), 0% (n = 0) and 2% (n = 2), respectively. The two non-toxigenic C. difficile isolates were typed as QX 083 and QX 565.
Awareness survey
There were 154 participants who were surveyed. The mean age of participants was 35 ± 7 years and almost two-thirds were females (66%; n = 102). Sixty percent of participants (n = 92) were clinicians. Of 154 participants, 33% (n = 51), 14% (n = 22), 4% (n = 6) and 3% (n = 4) of respondents answered one, two, three or four awareness questions correctly, respectively. The remaining 46% of participants (n = 71) provided wrong answers for all the four awareness questions. For the fifth question, there were 20% participants (n = 31) reported C. difficile as underestimated in their practice and 31% (n = 47) of participants reported not sure.
DISCUSSION
Our hospital prevalence of CDI was similar to previous reported studies from South East Asia [Reference Hassan19, Reference Putsathit27, Reference Hassan28], but we also found a significant rate of non-toxigenic C. difficile colonization not commonly reported in other Asian populations [Reference Putsathit29]. A recent study from Thailand [Reference Putsathit29] reported a similar prevalence of non-toxigenic C. difficile colonization (16%) as in our study. The authors suggested that the high prevalence of non-toxigenic C. difficile colonization may play an important role in reducing the risk of developing CDI [Reference Putsathit29]. This is because patients with non-toxigenic C. difficile colonization may mount a sufficient immune response to C. difficile toxins [Reference Furuya-Kanamori8]. There are limited data on non-toxigenic C. difficile colonization in Asia countries because most molecular epidemiological studies on the prevalence of C. difficile only focused on the characterization and isolation of the toxigenic C. difficile strains associated with CDI [Reference Collins, Hawkey and Riley14]. Therefore, the prevalence and molecular epidemiology of non-toxigenic strains may not have been properly investigated and documented [Reference Putsathit29].
In our study, 22 different strains were identified with RTs 043 and 017 being the most common. Prior to our study, there are no published data on C. difficile ribotyping in Malaysia. According to available data, the most prevalent RTs in Asia include 001, 002, 014, 017 and 018 [Reference Collins, Hawkey and Riley14], but our study also reported other new and unknown RTs. Although RT 014/020 is usually toxigenic, we found some unusual isolates of RT 014/020 that are non-toxigenic, which has been reported from Thailand previously [Reference Putsathit29]. Furthermore, the epidemic RTs 027 and 078 were not identified in our study. These findings suggest that there is an undefined and widely distributed reservoir of C. difficile strains in Malaysia. It is likely also that the C. difficile strains circulating in Malaysia are different from that in North America and Europe. The above suggests that CDI is as much a problem in South East Asia as elsewhere in the world; however, the molecular epidemiology may be specific for the country and the region.
In our hospital study, non-toxigenic C. difficile colonization and CDI shared some risk factors, including history of prior use of antibiotics, history of prior use of PPI, length of hospitalization, albumin and C-reactive protein. All these risk factors were known risk factors for C. difficile, which are consistent with previous studies [Reference Al-Tureihi30–Reference Hardt34]. The prescription of antibiotic in our setting is mainly based on the Malaysian National Antibiotic Guidelines 2014, which is not much different from other guidelines from the Western countries. The common prescription of high doses of broad-spectrum antibiotics and possible resistance to metronidazole in our hospital may explain the high prevalence of CDI observed in our study [Reference Hassan28]. Broad-spectrum antibiotic causes significant disruption of the gut microbiome and alter the gut ecology [Reference Francino35]. A disturbed gut ecology allows C. difficile to proliferate and causes infection in a susceptible human host [Reference Langdon, Crook and Dantas36].
Since high prevalence of CDI in elderly in the hospital is a relatively common finding, we conducted the community study in an elderly population to determine if there would be a similar trend of C. difficile in the community as in the hospital. However, our study reported a low prevalence of C. difficile carriage (1·6%) in the elderly community and none of the elderly had CDI. The low prevalence in our elderly community may be due to several reasons, especially the little or no contacts with the hospital environment and the absence of other traditional risk factors of CDI, in particular the low usage of antibiotics.
In addition, little or no exposure of PPI in our elderly community may explain the low prevalence of C. difficile observed in this population. The prevalence in our community study was also low when compared with other studies that reported asymptomatic colonization between 6% and 50% in long-term care facility residents [Reference Sartelli5]. A recent meta-analysis of nine studies reported that 15% of long-term care facility residents were asymptomatic carriers of toxigenic C. difficile [Reference Ziakas37]. It is possible that cleaning and disinfection, or appropriate hand hygiene in the hospital might not be adequate, allowing spores to be transmitted frequently in the hospital.
Our awareness study reported a low level of awareness with regards to CDI among hospital staff and students. The low awareness means a low CDI detection rate in our hospital and subsequently causes delays in the provision of antibiotics. Our findings were similar with an international survey that reported only 2% of respondents answered all questions correctly and 44% reported C. difficile to be underestimated [Reference Mavros15]. The international survey was conducted among clinicians from North America (55%), Europe (32%), Asia/Pacific (12%), Central and South America (1%), and Africa (1%) [Reference Mavros15]. Mavros et al. [Reference Mavros15] reported that clinicians from Asia had a significantly lower score than those from North America, suggesting that there was an inadequate awareness level of CDI among clinicians, particularly in Asia.
Our study had strengths but also limitations. Our study generated novel local data regarding the prevalence of CDI in hospitalized participants and the elderly in the community. In addition, we also investigated awareness of CDI among healthcare personnel and the low awareness shown in our study may mean that the hospital is missing many CDI cases and therefore new policy measures are urgently needed. There was a high carriage rate of non-toxigenic strains among hospitalized participants, and it is possible that some cases where toxigenic C. difficile was isolated may have been colonized rather than infected. RTs 017 and 043 were the most commonly found RTs in our hospital; however, there was also a significant number of new and unknown RTs, which may be unique to the population in Asia. Further investigation is needed to determine the significance of RT diversity with high rates of non-toxigenic strains. However, currently only a limited number of centers around the world, mainly in Europe, carry out ribotyping routinely so the assigning of new RTs is a slow process. Unfortunately, there are no recognized reference centers in Asia, and this will be required before the development of a useable Asian database.
In conclusion, our study demonstrates that the high prevalence of CDI in a Malaysian hospital is similarly reported by other Asian countries, despite a high prevalence of non-toxigenic C. difficile colonization. Important risk factors for CDI include duration of hospitalization and use of antibiotics. Although C. difficile colonization was highly prevalent in the hospital setting, C. difficile colonization was rare among the elderly in the community largely due to the absence of hospital exposure and absence of other traditional risk factors including antibiotics and PPI. The alarmingly low awareness of CDI among Malaysia hospital staffs needs to be addressed.
ACKNOWLEDGEMENTS
This study was partly funded by an Exploratory Research Grant Scheme (ERGS) from the Ministry of Higher Education of Malaysia (USM/203/PPSP/6730022). This work was also supported by a grant from the University of Western Australia and Alere.
The authors are extremely grateful to all the subjects who took part in the study.
AUTHOR CONTRIBUTIONS
N. H. Zainul, A. Besari, S. A. Hassan, D. A. Collins, T. V. Riley and Y. Y. Lee participated in study recruitment and study design. R. A. Rahman, D. A. Collins and T. V. Riley were involved in the preparation and analysis of the biological samples. N. H. Zainul, Z. F. Ma, N. Hamid and Y. Y. Lee conducted statistical analysis and interpreted the data. N. H. Zainul and Z. F. Ma wrote the first draft of the manuscript. Z. F. Ma and Y. Y. Lee revised the manuscript. All authors read and approved the final version of the manuscript.
DECLARATION OF INTEREST
None.





