Introduction
Diabetes mellitus (DM) has become one of the most important public health challenges of the 21st century. Over 150 million adults suffer from DM worldwide, and this number is expected to double in the next 25 years (Mathers and Loncar, Reference Mathers and Loncar2006; World Health Organization, 2016). The IDF Diabetes Atlas estimated that healthcare expenditure for diabetes accounted for 12% of the total healthcare expenditure worldwide in 2015 (International Diabetes Federation, 2015).
Efforts to guarantee good-quality chronic disease management in the primary care setting (taking a proactive population-based approach to chronic diseases early in their cycle with a view to preventing their progression and containing potential related complications) must be based on the awareness that the vast majority of patients receive the bulk of their care at primary care practices, and are likely to do so for the foreseeable future.
There is growing evidence to suggest that female general practitioners (GPs) perform better than their male colleagues in this situation. In particular, the former adhere more closely to clinical guidelines (Baumhäkel et al., Reference Baumhäkel, Müller and Böhm2009), more often provide preventive care (Journath et al., Reference Journath, Hellénius, Manhem, Kjellgren and Nilsson2008; Reference Journath, Hellénius, Carlsson, Wändell and Nilsson2010; Ince-Cushman et al., Reference Ince-Cushman, Correa, Shuldiner and Segouin2013), use a more patient-centered communication approach with longer visits (Roter and Hall, Reference Roter and Hall2004), perform at least as well as male GPs on standardized examinations, and provide more psychosocial counselling.
Kim et al. (Reference Kim, McEwen, Gerzoff, Marrero, Mangione, Selby and Herman2005) were the first to explore the influence of physicians’ gender on the diabetes management process and outcome measures in a primary care setting. Examining data on 1686 physicians serving a North American population, they found that the patients of female physicians were slightly more likely to receive lipid measurements and Hb1AC measurements and more likely to achieve an low-density lipoprotein (LDL)<130, but due to the difference slightness they conclude for a similar quality of care. A cross-sectional study on a diabetes management program adopted by German primary care physicians on a larger population showed instead that prognostically relevant risk control factors were better achieved by DM type 2 patients treated by a female physician. To be specific, these patients were more likely to benefit from a structured education about diabetes, a better glycemic control, and lower mean LDL-cholesterol levels, and they more often reached target LDL values and had better blood pressure levels (Berthold et al., Reference Berthold, Gouni-Berthold, Bestehorn, Böhm and Krone2008). In Italy, only one previous study (conducted in the Veneto Region) investigated the influence of physicians’ characteristics on their adherence to the care process for managing diabetes, which showed a small but significant effect of gender (Ferroni et al., Reference Ferroni, Casotto, Pigato, Scroccaro, Corti, Fedeli and Saugo2016). Finally, a recent study performed in Canada (Dahrouge et al., Reference Dahrouge, Seale, Hogg, Russell, Younger, Muggah, Ponka and Mercer2016) focused on the quality of care provided by physicians in family medicine, also considering diabetes management process indicators. Among others, some indicators [eg, eye test, metformin or lipid-lowering agent, glycosylated hemoglobin (HbA1c) tests] led them to conclude that the diabetic patients of female physicians were better managed.
These studies examined the association between GPs’ gender and their performance in homogeneous contexts, without checking whether organizational models interacted with the family physicians’ gender in predicting performance disparities.
In an Italian sample of family physicians working in different parts of the country with different organizational models, our study aimed to investigate whether any differences in diabetes process indicators relating to primary care physicians’ gender are associated with these doctors’ different performance, and/or the interaction between gender and different organizational models.
Materials and methods
Context
Italy is divided administratively into 19 regions and two autonomous provinces, whose governments have the important task of fulfilling the objectives of the National Health Plan at the regional level. They are responsible for planning and organizing healthcare facilities and related activities through regional health departments. They also coordinate and control the local health units (LHU), each of which is an autonomous Health System body that organizes and plans for the services in a given area, providing community healthcare closer to where people live. The LHUs are organized into districts that coordinate all healthcare services and publicly funded facilities and services delivered outside the hospital for a portion of the LHU community. The main primary care providers in Italy are GPs, who are self-employed, independent doctors paid on the basis of a partially weighted capitation fee on the number of patients registered with them, plus fee-for-service payments according to specific performance indicators, managed at regional or local level. As the main primary care providers and system gatekeepers, GPs play a pivotal role in the management of chronic diseases: they decide the care program, and the pathways for its delivery for each patient. In the case of care for diabetic patients, they also cooperate with local or regional diabetes clinics and services.
Participants
Our data were obtained from the Italian, MEDINA project, during 2013–2015, a national scheme designed to assess the quality of care provided for chronic diseases, and to monitor how primary healthcare services are organized. Seven Italian regions, two in northern Italy (Lombardy and Veneto), three in central Italy (Emilia Romagna, Tuscany, and Marche), and two in southern Italy (Apulia and Sicily) took part in the MEDINA project. For each region, one LHU district was involved in the study (seven in all). The proactive primary care models we analyzed were specifically selected for each region: a Chronic Care Model in Tuscany, an adaption of the Chronic Care Model in Marche, a care manager-based model in Apulia, an empowerment and self-management support program in Emilia Romagna, Integrated Primary Care Model in Sicily, an Integrated Primary Care Model associated with population risk stratification in Veneto and an integrated care model associated with population risk stratification and a bundle payment scheme in Lombardy. The regional authorities and the LHUs that took part in the project were selected on a voluntary basis. All the GPs working for the chosen LHU were included, however, without any further selection.
For the purposes of the study, a GP was considered as a statistical unit and we recorded: age, gender, total number of registered patients, total number of patients with diabetes, average age of diabetic patients, patients’ gender ratio, percentage of patients over 75 years old. The data set was built identifying diabetes patients of each general practitioner by means the Matrix, an open-source software that enables the linkage of different administrative data by means of an automated algorithm (Moirano and Bellentani, Reference Moirano and Bellentani2014) and the extraction of relevant variables. A deterministic record linkage was performed to connect patient registries, disease-specific exemptions from healthcare copayments, drug usage recorded in drug dispensing records, hospitalizations retrieved from hospital discharge records, and specialist outpatient visits.
The Diabetes Quality Improvement Project (DQIP) has developed and implemented a comprehensive set of performance measures for assessing the care provided for patients with diabetes, and improvements in its quality, which could be widely accepted and broadly implemented.
Each GP’s performance was assessed according to standards for the quality of care, based on their adherence to recommendations concerning patient monitoring and treatment, using internationally validated indicators (Nicolucci et al., Reference Nicolucci, Greenfield and Mattke2006; OECD, Reference O’Connor, Bodkin, Fradkin, Glasgow, Greenfield, Gregg, Kerr, Pawlson, Selby, Sutherland, Taylor and Wysham2015), including:
(a) at least two HbA1c tests annually;
(b) at least one test for microalbuminuria annually;
(c) at least one creatinine level measurement annually;
(d) at least one lipid profile measurement annually;
(e) proportion of diabetic patients treated with cholesterol-lowering drugs.
Adherence to these requirements was estimated from the administrative databases recording drug prescriptions and diagnostic service usage in 2014, as described in detail elsewhere (Dahrouge et al., Reference Dahrouge, Seale, Hogg, Russell, Younger, Muggah, Ponka and Mercer2016). The reliability and of the extraction algorithms of these databases was assessed in recently published papers (Gini et al., Reference Gini, Schuemie, Mazzaglia, Lapi, Francesconi, Pasqua, Bianchini, Montalbano, Roberto, Barletta, Cricelli, Cricelli, Dal Co, Bellentani, Sturkenboom and Klazinga2016).
Statistical analysis
A total score was calculated for the average performance in the previously listed five indicators, representing global adherence to quality management of patients with diabetes. The score for each GP was built as the average of the patients’ proportions of the single aforementioned measure of quality of care (HbA1c, microalbuminuria, creatinine, lipid profile measurement, adherence to cholesterol-lowering regime). Albeit they convey less granular clinical information, composite performance scores have been widely adopted, and may improve the reliability of performance measures and rankings by comparison with single measures, however they should be supplemented with individual physician measure data (O’Connor et al., 2011), as in our study.
A non-parametric test was used, consistently with the Shapiro–Wilk normality test, which states that the assumption of normality in the distribution of the scores is not met at a significance level of 0.05. The Mann–Whitney test was consequently used to analyze the differences between male and female GPs’ performance scores. Confidence intervals were calculated as Wald intervals.
Then the analysis proceeded using multivariate approaches to quantify the gender association on the performance score, adjusting for the covariates (LHU, GP’s age, number of patients, and average age of diabetic patients). First, we carried out a multilevel analysis (mixed effects model) applying the performance score as the dependent variable, and considering GPs as first-level units, and LHUs as second-level units, to see how LHUs affected the outcome and obtain the intra-class correlation coefficient.
A quantile regression model (Koenker and Bassett, Reference Koenker and Bassett1978) was also fitted, adjusting for the covariates (LHU, GP’s age, number of patients, and average age of diabetic patients). This model is more robust in case of deviation from normality, and quantifies the association of explanatory variables (gender) at several levels of the quantiles of the outcome variable (performance score). The association with GPs’ gender, when GPs’ performance was poor, normal, or very good, was addressed by using three different levels for the global score, that is, the first quartile (25th percentile), the median (50th percentile), and the third quartile (75th percentile).
The interaction between gender and LHU was also considered.
Analyses were conducted using R package version 3.2.3.
Results
Our study was conducted on a population-based database of 2287 Italian GPs, accounting for almost 5% of the country’s total family physician workforce (45 203 GPs among them 71.6% male in 2013); there were 586 females (25.6%) and 1701 (74.4%) males, with a mean age of 55 years. They provided care for a total of 2 646 059 patients, with an average of 1157 patients each (1180 for the male GPs and 1090 for the female GPs). The prevalence of patients with diabetes was 6.6%, with a total of 174 693 patients, and a mean 81 diabetic patients each for the male GPs and 67 for the female GPs.
Table 1 shows the GPs’ characteristics.
Table 1 Characteristics of the sample of GPs
Descriptive analysis: means and SD.
A graphical analysis of the global scores for male and female GPs reveals a difference between the two distribution densities, with females scoring higher than males (Figure 1). There was a significant difference in each process indicator, so female GPs systematically performed better than their male colleagues (Table 2).
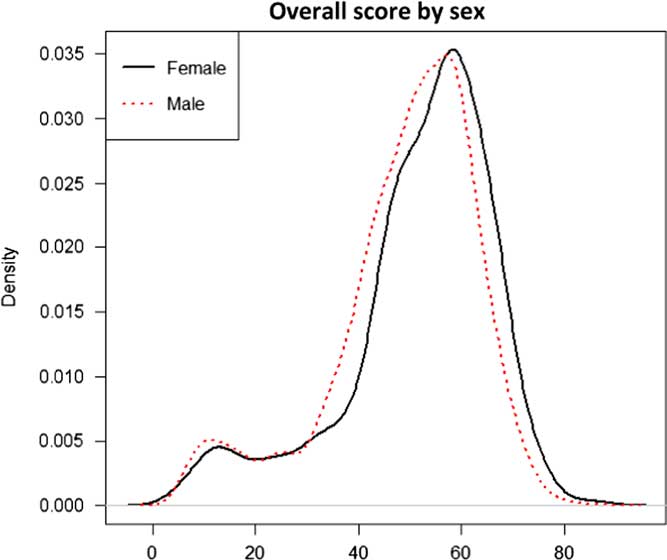
Figure 1 Estimated density of total performance scores by gender of GPs (586 women GP and 1701 men GP).
Table 2 Average overall score (%) for the performance of male and female GPs with 95% confidence intervals (CI) and P-values (Mann–Whitney test)
To examine the specific association between GPs’ gender and LHU districts, a mixed effects model was fitted that pointed to about 71% of the estimated variability being due to differences between LHU districts (intra-class correlation coefficient 0.7097, P<0.05). The fitted multilevel models confirmed that, all other variables remaining equal, female GPs obtained better results than male GPs, with a 2.095% higher global score. This better overall performance derived from female GPs performing better systematically, on every item tested: the increase coinciding with female gender was 2.474 percentage points in the 25th percentile, 1.689 percentage points in the median values, and 2.847 percentage points in the 75th percentile.
The confidence intervals never overlapped, meaning that the three associations differed significantly. We can thus conclude that females performed better than males regardless of whether the sample’s overall performance was poor (25th percentile) or very good (75th percentile) (Tables 3 and 4).
Table 3 Estimated quantile regression coefficients by gender, with SE and 95% confidence intervals (CI) on outcome (total performance score) adjusted for GPs’ age, number of patients, local health units, and average age of diabetic patients
The interaction between gender and LHU was not significant.
Table 4 Estimated quantile regression coefficients by gender, with SE and 95% confidence intervals (CI) on outcome (five indicators) adjusted for GPs’ age, number of patients, local health units, and average age of diabetic patients
Discussion
Summary
Our study disclosed a positive association between female gender in physicians and quality process indicators in the management of diabetes. We also found that the association of the gender depended on the GPs’ levels of performance, the gap between women’s and men’s performance being smaller for the median levels, and larger at the extreme quartiles. In other words, the gap between women’s and men’s performance was significantly higher among those GPs whose performance was below average, but highest among the best performers. This picture was not modified by the different organizational models because the interaction between gender and LHU was not significant.
Comparison with existing literature
In particular, our study showed that female GPs scored better on all five diabetes management process indicators used to retrospectively assess the quality of care delivered across the whole population with diabetes. These measures are already widely used in surveillance systems for monitoring the quality of primary care at population level, but whether or not closer monitoring is necessarily linked to better intermediate or final outcomes for diabetes patients is still being debated (Petitti et al., Reference Petitti, Contreras, Ziel, Dudl, Domurat and Hyatt2000). One recent study (Giorda et al., Reference Giorda, Picariello, Nada, Tartaglino, Marafetti, Costa and Gnavi2012) found that patients receiving the worst-quality care (in terms of the fulfillment of quality-of-care indicators based on screening guidelines similar to those considered here) carried a higher risk of all-cause mortality and cardiovascular morbidity than those receiving the best-quality care. Credible evidence emerged of a link between these process indicators (on the frequency of certain prescribed laboratory or clinical tests) and major clinical outcomes that can be modified by the healthcare system’s efforts and intervention (Fleming et al., Reference Fleming, Greenfield, Engelgau, Pogach, Clauser and Parrott2001).
Our finding that female family physicians are more likely than their male colleagues to follow chronic disease management guidelines are consistent with previous reports (Kim et al., Reference Kim, McEwen, Gerzoff, Marrero, Mangione, Selby and Herman2005; Berthold et al., Reference Berthold, Gouni-Berthold, Bestehorn, Böhm and Krone2008). One possible reason for this may lie in their different clinical approach to patient care. For example, female physicians are more likely to refer patients to a specialist, and this could reflect a better patient management, based on cooperation between GP and specialist. Our results might also be at least partly due to the fact that female physicians have different communication and decision-making styles from their male colleagues – attributes that may facilitate their patients’ engagement in monitoring their own health. In fact, female physicians tend to use a more participatory decision-making process (Cooper-Patrick et al., Reference Cooper-Patrick, Gallo, Gonzales, Vu, Powe, Nelson and Ford1999) that encourages self-management and self-monitoring, which are a fundamental part of diabetes care and may result in better disease control (Skovlund and Peyrot, Reference Skovlund and Peyrot2005).
Previous studies addressed the effect of healthcare reforms on gender equity in patient management. One particular study examined whether the type and extent of the gender-related differences in GPs’ provision of care varied in different models of primary care. They found that the type of healthcare system mainly influenced the male and female GPs’ different responses to their patients’ healthcare needs in terms of health promotion. To the best of our knowledge, nobody had investigated whether different models of primary care interplay a different performance in GPs by gender. Our study showed that the female GPs’ better performance was not influenced by the way in which the primary care service was organized.
Implications for practice
It could be argued that the size of the differences observed in our study was small and therefore of limited clinical relevance. On the other hand, data from the UKPDS study suggest that the use of statins and antihypertensive drugs in diabetic patient has the greatest effect in reducing cardiovascular risk, hypoglycemic agents, and aspirin being the next most important interventions (Holman et al., Reference Holman, Paul, Bethel, Matthews and Neil2008). The marked change in the gender balance of the medical-doctor workforce means that women will make up around 65% of the world’s medical doctors by 2030 (US Department of Health and Human Services, 2006; Koike et al., Reference Koike, Matsumoto, Kodama, Ide, Yasunaga and Imamura2009; General Medical Council, 2010; 2016), and this could lead to a better management of chronic patients in different healthcare systems. In fact, even if our results demonstrated that women brought only a modest improvement in the quality of the process of care, they could take effect on a large population. Small changes in large populations can have a considerable overall effect, as seen with prevention strategies, where shifting the risk distribution in the population (Rose, Reference Rose2001) can bring larger benefits to the population as a whole than achieving larger improvements in a small group.
Alongside its clinical relevance, the present study corroborates other evidence to suggest that female physicians may provide higher-quality care, whatever the organizational model of primary care, in the areas of health promotion, prevention strategies, in-hospital activities, as well as in primary care practice, as already demonstrated in previous studies (Andersen and Urban, Reference Andersen and Urban1997; Ferguson et al., Reference Ferguson, James and Madeley2002; Roter et al., Reference Roter, Hall and Aoki2002; Roter and Hall, Reference Roter and Hall2004; Kim et al., Reference Kim, McEwen, Gerzoff, Marrero, Mangione, Selby and Herman2005; Berthold et al., Reference Berthold, Gouni-Berthold, Bestehorn, Böhm and Krone2008; Baumhäkel et al., Reference Baumhäkel, Müller and Böhm2009; Tsugawa et al., Reference Tsugawa, Jena, Figueroa, Orav, Blumenthal and Jha2017). It is still crucial to underscore this evidence because of the persistent ‘stigma’ surrounding the assessment of women in the workforce, based on the argument that career suspensions for childrearing, higher rates of part-time employment, and greater trade-offs between responsibilities at home and at work (Jolly et al., Reference Jolly, Griffith, DeCastro, Stewart, Ubel and Jagsi2014) may negatively affect the quality of care provided by female physicians, and justify higher salaries for male physicians. That is why empirical evidence on whether the outcomes of patients with male and female physicians really differ is warranted. Recent research points to ongoing systemic gender discrimination and inequalities in pre-service and in-service health education and employment systems. A good human resource for health (HRH) leadership, governance, and management should focus instead on recognizing the diversity of healthcare workforces, acknowledging gender constraints and opportunities, eliminating gender discrimination and equalizing opportunities (Newman, Reference Newman2014). The WHO has also established that gender equality should be an HRH research, leadership, and governance priority (Standing, Reference Standing2000).
Finally, our results are consistent with findings in the international literature confirming that women demonstrated a better performance in terms of the quality of healthcare: this warrants further study to ascertain exactly why these differences in quality of care and practice patterns exist, with a view to providing valuable insight on how to improve the quality of care for all patients, irrespective of who provides their care (Tsugawa et al., Reference Tsugawa, Jena, Figueroa, Orav, Blumenthal and Jha2017). This could point to the need to prepare diversified training packages and incrementing the provision of education or supervision for men.
Strengths and limitations
Our analysis was conducted on a large, robust administrative data set, using a validated set of process indicators that reflect how chronic diseases are managed in different parts of Italy. The main drawback of the present study lies in that GPs’ performance was measured only by means process indicators, considered as a proxy for performance in terms of outcome measures. Moreover, our study does not register the degree of the disease severity, such lack of adjustment could give a confounding bias, although we are confident that the severity of disease was not differentially distributed in men and women physicians, resulting in a confounding bias in the association among gender and performance score. Another possible shortcoming of our investigation lies in that using record linkage may have failed to identify some diabetic patients. The validity of our record linkage procedures, based on three data sources (hospital discharge records, drug prescriptions, and payment exemptions for chronic diseases) was addressed in a recent study, which found that these routinely collected data enable a disease’s prevalence to be estimated just as accurately as in other studies conducted in Italy using more costly and time-consuming methods (Gini et al., Reference Gini, Schuemie, Mazzaglia, Lapi, Francesconi, Pasqua, Bianchini, Montalbano, Roberto, Barletta, Cricelli, Cricelli, Dal Co, Bellentani, Sturkenboom and Klazinga2016).
The sample of regional authorities and LHUs that took part in the project on a voluntary basis may introduce a sort of sample selection bias, although all GPs working for the LHU chosen by each regional authority were included, without any further selection. Moreover, the regional authorities and LHUs taking part in the survey were not aware of the purpose of the study (to test differences in their GPs’ performance by gender). This type of sample selection could give rise to a non-differential misclassification, which would bias toward the null. In addition, we used the same measurement methods to assess performance in both genders, and this enabled us to avoid introducing any measuring bias.
Conclusion
In conclusion, our study confirms that female physicians perform better than males in the primary care of patients with diabetes, and this may have an important impact on chronic disease management, from which the community may benefit considerably. Further investigations are warranted on the determinants of these gender-related differences in GPs’ behavior in this setting.
Acknowledgments
The Medina Project was an initiative of the Italian National Agency for Regional Health Services. The Medina Project Group includes the following members: Stefania Arniani, Mara Azzi, Valentina Barletta, Antonio Brambilla, Salvatore Brugaletta, Massimiliano Correani, Nunziata Cosentino, Paolo Da Col, Mina De Gennaro, Enrico Desideri, Andrea Donatini, Manuele Falcone, Bruno Federico, Pietro Gallina, Gilberto Gentili, Gavino Maciocco, Francesco Marcato, Verdiana Morando, Vito Piazzolla, Francesco Profili, Domenico Scibetta, Stefano Sforza, Valeria D. Tozzi, Elisabetta Verdelli, Modesta Visca.
Conflicts of Interest
The authors have no conflict of interest to declare.








