Breast-feeding has multiple health benefits for both mothers and children, including maternal protection against breast and ovarian cancer, as well as Type 2 diabetes(Reference Chowdhury, Sinha and Sankar1). Children who are breastfed have increased intelligence, protection against infections and reductions in the prevalence of asthma, allergies, obesity and diabetes(Reference Victora, Bahl and Barros2–Reference Azad, Vehling and Lu4). In addition to the multiple physical health benefits, maternal–infant bonding during breast-feeding promotes security and emotional stability for the child(Reference Gibbs, Forste and Lybbert5).
In Canada, 89 % of women initiate breast-feeding, but only 26 % exclusively breastfeed to 6 months, despite the WHO recommendations for a minimum duration of 6 months(Reference Gionet6). Early breast-feeding cessation is related to many different factors, including socio-demographic characteristics such as younger maternal age, lower education and family income, returning to work and maternal smoking(Reference Lok, Wang and Chan7–Reference Tavoulari, Benetou and Vlastarakos9); hospital practices such as delayed initiation of breast-feeding and separation of the mother and infant and intrapartum and birth factors such as caesarean section and gestational age(Reference Bai, Wu and Tarrant10–Reference Hobbs, Mannion and McDonald13). Because of cultural practices, the country of birth can also play a critical role in breast-feeding. Women who live in low- and middle-income countries(Reference DiGirolamo, Grummer-Strawn and Fein14) generally breastfeed their children for longer when compared with women in high-income countries(Reference Victora, Bahl and Barros2). Among immigrant women in high-income countries, maternal ethnicity and birth country have been shown to influence breast-feeding practices(Reference Ladewig, Hayes and Browne15). Within countries, race and ethnicity are associated with the rate of breast-feeding, with Caucasian Americans usually having a higher rate of breast-feeding when compared with African Americans(Reference Anstey, Chen and Elam-Evans16).
A recent review of breast-feeding practices among immigrant and non-immigrant women by Dennis et al. (Reference Dennis, Shiri and Brown17) reported that immigrant women were twice as likely to breastfed for 3–6 months and were 33 % more likely to breastfeed for longer than 6-month postpartum. Studies also show that although immigrant women have higher breast-feeding rates when compared with native-born women, these rates decrease with the length of time that the immigrant lives in the country(Reference Lok, Bai and Chan18). However, one study showed that in Spain, native-born women were more likely to exclusively breastfeed at the time of postpartum hospital discharge when compared with Chinese immigrant women(Reference Aguilar-Ortega, Gonzalez-Pascual and Cardenete-Reyes19). Although the USA and Canada are culturally diverse, immigrants in both countries tend to assimilate to a new culture for social acceptance. Immigrant women often feel conflicted between family and cultural practices and the accepted practices in a new country(Reference Schmied, Olley and Burns20). Additionally, age at the time of migration and the country where women receive their education can influence the way they adapt and can be a strong predictor of breast-feeding initiation and duration(Reference Hendrick and Potter21).
Over the last several decades, there have been increased efforts to promote and encourage breast-feeding in Canada. Immigration is also on the rise, especially for women of childbearing age(22). Non-Canadian-born residents now account for 20 % of the Canadian population(Reference Hudon23). Few studies have assessed how patterns of immigration and the length of time spent in Canada affect immigrant women’s breast-feeding behaviours and how this compares with Canadian-born women(Reference Hawkins, Gillman and Shafer24). Therefore, the current study aimed to compare breast-feeding initiation and continuation rates among Canadian-born and non-Canadian-born women and to examine factors associated with breast-feeding initiation and continuation among both groups.
Methods
Design, setting and participants
We accessed data from the CHILD Cohort Study, a multi-center national birth cohort study that recruited pregnant women from four Canadian provinces. From 2008 to 2012, the study recruited 3621 participants in their second and third trimester, and prospective follow-up is still ongoing(Reference Subbarao, Anand and Becker25). At the time of the study, only one recruitment site was designated as a Baby-Friendly Hospital(26). The present analysis excluded participants from the Vanguard cohort and only focused on the general cohort of 3405 participants (see Fig. 1). Among these, seventy-seven infants were ineligible at or before birth, 64 mothers subsequently withdrew and 254 were missing relevant breast-feeding data. Complete baseline and breast-feeding initiation data were available for 3010 participants. There was a small loss to follow-up (n 104) with 6-month breast-feeding status was available for 2906 of these participants. A comparison of the demographic characteristics of those with full follow-up and those with missing data or who were lost to follow-up at 6 months shows that participants with missing date were more likely to be younger, have lower education and poorer socio-economic status (see online supplementary material, Supplemental Table S1). There were fewer observed differences between participants with full follow-up and those missing only the 6-month follow-up data. Eligibility criteria for the CHILD study included pregnant women aged 18 and older (19 in Vancouver) with a singleton pregnancy. Women were excluded if they used in vitro fertilization to conceive, gave birth before 35 weeks’ gestation or were unable to speak and read English. Recruitment methods included referrals from physicians and midwives, community and social media advertising and word of mouth.
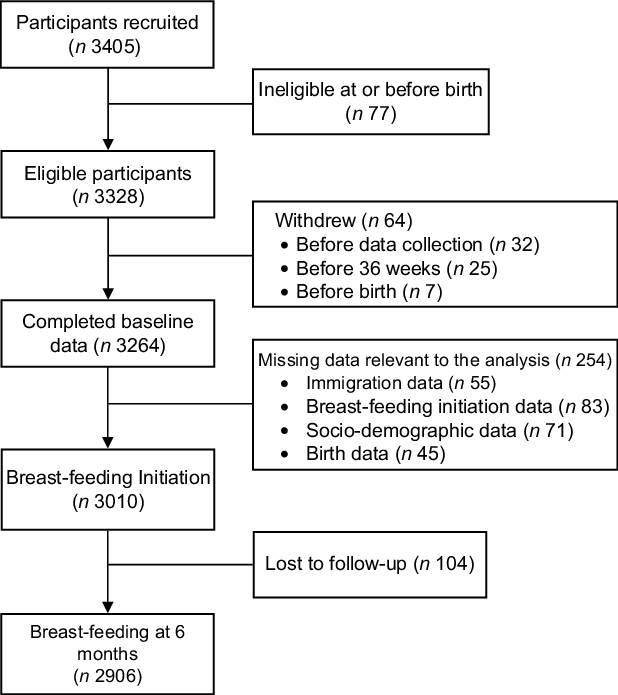
Fig. 1 Participant flow diagram
Data collection procedures
All participants signed written consent before participation in the study. Participants completed baseline socio-demographic questionnaires that recorded ethnicity, country of birth, years lived in Canada, education and socio-economic status. Detailed questionnaires were completed prenatally and at 3, 6, 12, 18 and 24 months postpartum. Participants were asked about breast-feeding initiation and duration. Hospital information (gestational age, birth mode, feeding and birth weight) was collected by hospital labour and delivery nurses and research staff.
Study variables
Breast-feeding initiation was recorded in the postpartum period on the hospital records and was extracted by the study research staff. Continuing breast-feeding status was self-reported on the follow-up questionnaires at multiple intervals after delivery (3, 6, 9, 12, 18 and 24 months). In these questionnaires, we assessed breast-feeding initiation, breast-feeding status at 6-month postpartum and total duration of any breast-feeding. Any breast-feeding was defined as the receipt of any breast milk, either at the breast or expressed, irrespective of the concurrent receipt of infant formula or other breast milk substitutes(27).
Immigration status variables were extracted from the demographic questions on country of birth, age at the time of migration and length of time lived in Canada. The country of birth was used to determine the geographic region, country income level and gender-related development index. The geographic region of birth and country income level were categorised according to data from the World Bank(28). Gender Development Index is a measurement created by the UN to measure gender inequalities in three dimensions of human development for females as compared with males: life expectancy at birth, years of education and estimated earned income(29).
We also included socio-demographic and maternal and birth characteristics that have been shown to affect breast-feeding in most populations. Socio-demographic characteristics that were included in the analysis were maternal age, maternal education, household income, home ownership, marital status, recruitment site and maternal and household smoking, all self-reported at enrolment. Maternal and birth characteristics included parity, mode of birth, gestational age, birth weight and rooming-in, all extracted from the postpartum hospital record.
Statistical analysis
We used descriptive statistics to summarise the socio-demographic characteristics and birth-related factors of Canadian-born and non-Canadian-born participants. Bivariable and multivariable logistic regression analysis was used to assess the association between place of birth and breast-feeding initiation and continuation at 6 months as well as factors associated with breast-feeding in Canadian-born participants and non-Canadian-born participants. Figure 2 presents the directed acyclic graph of the explanatory model(Reference Williams, Bach and Matthiesen30). The directed acyclic graph was used to determine the minimum set of covariates required for adjustment when each variable was set as the exposure. Hosmer–Lemeshow tests were used to test the goodness of fit. Data were analysed using Stata version 15.1(31). A 95 % CI and 0·05 level of significance were used for analysis.

Fig. 2 Directed acyclic graph of the explanatory model of the factors related to breast-feeding outcomes
Results
Table 1 shows the characteristics of Canadian-born and non-Canadian-born participants. Of 3010 participants included in the current study, the majority were Canadian-born (75·4 %) with a university degree or higher (62·9 %). Although a higher proportion of non-Canadian-born participants (69·2 %) had a university degree when compared with Canadian-born participants (60·9 %), household income was lower in non-Canadian-born participants. Among non-Canadian-born participants, approximately one-half lived in Canada for < 10 years, 63·1 % migrated when they were 18 years of age or older and 63·3 % lived in Vancouver or Toronto. Around 40 % of non-Canadian-born participants were born in South & East Asia & Pacific Region and almost one-half were from a country with a high Gender Development Index.
Table 1 A comparison of the characteristics of immigrant and Canadian-born study participants (n 3010)

GDI: Gender Development Index.
The median breast-feeding duration was 10 months in Canadian-born participants and 11 months in non-Canadian-born participants (P < 0·001). Participants who migrated before 18 years of age had the same median duration of breast-feeding as Canadian-born participants (10 months), while participants who migrated after 18 years of age had a median duration of breast-feeding of 11 months. When compared with Canadian-born participants, non-Canadian-born participants were more likely to initiate breast-feeding (95·5 % v. 92·7 %; P = 0·007) and to continue breast-feeding at 6 months (80·9 % v. 75·2 %; P = 0·002) in unadjusted analyses (Table 1). After adjusting for all socio-demographic and labour and birth factors, however, these differences were no longer significant for breast-feeding initiation (OR = 0·76; 95 % CI: 0·50, 1·14) or for breast-feeding continuation at 6 months (OR = 0·92; 95 % CI: 0·72, 1·16) (data not shown).
Table 2 shows the unadjusted and adjusted OR for associations between the socio-demographic, labour and birth factors and breast-feeding initiation among Canadian-born participants and non-Canadian-born participants. Canadian-born participants were more likely to initiate breast-feeding if they were older, had some post-secondary education, were married or living with their partner and were rooming-in during the hospital stay (all P < 0·05). In non-Canadian-born participants, older maternal age and higher education were also associated with breast-feeding initiation, but the association was only significant in participants 30–34 years of age and those with a university degree or above. When compared with participants from other centres, Canadian-born participants recruited in Vancouver were more likely to initiate breast-feeding, but there were no significant differences in breast-feeding initiation by study site among non-Canadian-born participants. Maternal smoking was associated with lower odds of breast-feeding initiation in non-Canadian-born participants, while living with a current smoker, caesarean birth and early-term birth (37–< 39 weeks) were associated with lower odds of breast-feeding initiation in Canadian-born participants.
Table 2 Unadjusted and adjusted odds ratios for breast-feeding initiation by birthplace (n 3010)

* Covariates for each model are as follows:
Maternal age: no adjustment needed.
Maternal education: adjusted for maternal age.
Household income: adjusted for maternal age, education, marital status and study site.
Home ownership: adjusted for maternal age, education, marital status, household income, study site.
Marital status: adjusted for maternal age and education.
Smoked during pregnancy: adjusted for maternal age, education, marital status, household income and live with current smoker.
Live with current smoker: adjusted for household income and maternal education.
Study recruitment site: no adjustment needed.
Parity: adjusted for maternal age, education, marital status and household income.
Mode of birth: adjusted for maternal age, education, marital status, household income, smoked during pregnancy, live with a current smoker, parity, gestational age and birth weight.
Gestational age: adjusted for maternal age, education, household income, smoked during pregnancy, live with current smoker and parity.
Birth weight: adjusted for maternal age, education, household income, smoked during pregnancy, live with current smoker, parity and gestational age.
Baby rooming in with mother: adjusted for mode of birth, gestational age and birth weight.
The median breast-feeding duration was 12 months in Vancouver participants, 10 months in Winnipeg participants and 9 months in both Edmonton and Toronto participants (P < 0·001). The unadjusted and adjusted associations between the predictors of breast-feeding continuation at 6-month postpartum in Canadian-born participants and non-Canadian-born participants are shown in Table 3. In Canadian-born participants, older maternal age, post-secondary education and married or living with a partner were significantly associated with breast-feeding continuation at 6-month postpartum in the adjusted analyses, whereas in non-Canadian-born participants, only maternal age was associated with breast-feeding continuation. In both groups, participants recruited in Vancouver had significantly higher odds of breast-feeding continuation at 6-month postpartum, when compared with participants recruited in Edmonton. Maternal smoking was significantly associated with lower odds of breast-feeding continuation at 6-month postpartum in both Canadian-born (OR = 0·47; 95 % CI 0·29, 0·76) and non-Canadian-born participants (OR = 0·08; 95 % CI 0·02, 0·42). Living with a current smoker (OR = 0·49; 95 % CI 0·37, 0·64), having a caesarean section (OR = 0·62; 95 % CI 0·49, 0·79) and early-term birth (OR = 0·65; 95 % CI 0·51, 0·82) were associated with lower odds of breast-feeding continuation at 6 months in Canadian-born participants only. The results of the Hosmer–Lemeshow goodness-of-fit tests for the logistic regression models were all > 0·05, indicating that the models fit the data.
Table 3 Unadjusted and adjusted odds ratios for any breast-feeding at 6-month postpartum by birthplace (n 2906)

* Covariates for each model are as follows:
Maternal age: no adjustment needed.
Maternal education: adjusted for maternal age.
Household income: adjusted for maternal age, education, marital status and study site.
Home ownership: adjusted for maternal age, education, marital status, household income and study site.
Marital status: adjusted for maternal age and education.
Smoked during pregnancy: adjusted for maternal age, education, marital status, household income and live with current smoker.
Live with current smoker: adjusted for household income and maternal education.
Study recruitment site: no adjustment needed.
Parity: adjusted for maternal age, education, marital status and household income.
Mode of birth: adjusted for maternal age, education, household income, smoked during pregnancy, live with a current smoker, parity, gestational age and birth weight.
Gestational age: adjusted for maternal age, education, household income, smoked during pregnancy, live with current smoker and parity.
Birth weight: adjusted for maternal age, education, household income, smoked during pregnancy, live with current smoker, parity and gestational age.
Baby rooming in with mother: adjusted for mode of birth, gestational age and birth weight.
We found no association between any of the assessed migration characteristics and breast-feeding initiation or breast-feeding continuation at 6-month postpartum in non-Canadian-born participants (see online supplementary material, Supplemental Table S2), although power was limited for the current analysis. As a sensitivity analysis, we also repeated our analysis on the predictors of breast-feeding at 6 months on a restricted subset of participants, including only participants who had initiated breast-feeding (n 2707). Findings from the restricted subset showed similar associations between participant characteristics and breast-feeding outcomes and the models showed similar point estimates (see online supplementary material, Supplemental Table S3).
Discussion
This large prospective study identified factors associated with breast-feeding initiation and continuation in Canadian-born and non-Canadian-born women. Approximately one-quarter of the sample were non-Canadian-born participants, but contrary to other studies,(Reference Dennis, Shiri and Brown17,Reference Lok, Bai and Chan18) we found only minimal differences in the breast-feeding duration of Canadian-born and non-Canadian-born women. We also did not find that migration characteristics affected either breast-feeding initiation or breast-feeding continuation in non-Canadian-born participants, although study power may have been limited for the current analysis. Multivariable analyses indicate that different factors affect breast-feeding initiation and continuation in the two groups of participants. In Canadian-born participants, socio-demographic characteristics, such as older maternal age, higher education, and living with a partner, were positively associated with breast-feeding initiation and continuation, while living with a smoker was negatively associated with both breast-feeding outcomes. These associations were observed less consistently in non-Canadian-born participants. Maternal smoking decreased the odds of breast-feeding initiation in Canadian-born participants and decreased the odds of breast-feeding continuation in all participants. In Canadian-born participants, those recruited in Vancouver had breast-feeding initiation rates that were higher than participants recruited at the other study sites. Among all participants, those recruited in Vancouver had approximately two to three times higher odds of continuing breast-feeding at 6-month postpartum. Early-term and caesarean birth were associated with lower rates of breast-feeding initiation and continuation in Canadian-born participants only.
The association between socio-demographic characteristics (e.g. maternal age, education and marital status) and breast-feeding initiation and duration has been a common finding in other studies(Reference Thulier and Mercer33,Reference Cohen, Alexander and Krebs34) . However, in our study, the associations between breast-feeding and maternal age and education more consistent among Canadian-born women, which is similar to previous Canadian data showing that women who do not breastfeed are more likely to be younger and have less education than those who do breastfeed(Reference Gionet6). Non-Canadian-born women in our sample were more likely than Canadian-born women to have a university degree or above (69·2 % v. 60·9 %) and to initiate breast-feeding (95·5 % v. 92·7 %). Therefore, it is possible that among non-Canadian-born participants, cultural norms are more influential than socio-demographic characteristics. Studies in other countries have shown that breast-feeding practices are less associated with socio-demographic characteristics than in Western countries, and breast-feeding is sometimes more prevalent in women with lower education levels(Reference Tavoulari, Benetou and Vlastarakos32,Reference Tarrant, Fong and Wu35–Reference Bulk-Bunschoten, Pasker-de Jong and van Wouwe37) .
Our findings on the differences in breast-feeding rates between study sites are consistent with national data reporting that British Columbia has the highest breast-feeding rates across Canada(Reference Gionet6). Breast-feeding rates in Canada vary substantially across the country, with an east-to-west gradient of lower to higher initiation rates ranging from 57 % in Newfoundland and Labrador to 96 % in British Columbia(Reference Green, Chalmers and Hanvey38). Furthermore, participants recruited at the Vancouver study-site were all recruited from a large tertiary hospital that was a designated Baby-Friendly Hospital Initiative (BFHI) facility, the only study site to have received that designation at the time of recruitment. Studies show that exposure to BFHI practices improves breast-feeding initiation and duration(Reference Tarrant, Lok and Fong39,Reference Brodribb, Kruske and Miller40) , but further research is needed to explain why these disparities in breast-feeding practices continue within Canada.
Negative associations between maternal and household smoke exposure and breast-feeding duration have been consistently reported in previous studies(Reference Lok, Wang and Chan7,Reference Horta, Kramer and Platt41) . Smoking during breast-feeding lowers prolactin levels, reduces the volume of breast milk and alters the composition and protective properties of breast milk(Reference Napierala, Mazela and Merritt42,Reference Baron, Bulbrook and Wang43) . Women who smoke or who live in a smoking household are also less likely to intend to and initiate breast-feeding(Reference Lok, Bai and Tarrant44), indicating that psychosocial factors are also associated with the lower rates of breast-feeding among smoking mothers(Reference Donath, Amir and Team45). Also, research has found that when compared with non-smoking partners, fathers who smoke are more likely to prefer infant formula feeding over breast-feeding(Reference Lok, Wang and Chan7), and a father’s infant feeding preferences are strongly associated with breast-feeding initiation and duration(Reference Bai, Fong and Lok46,Reference Lok, Bai and Tarrant47) .
In the literature, the associations between breast-feeding and maternal and birth factors, such as early-term birth, caesarean section and rooming-in, are inconsistent(Reference Tarrant, Lok and Fong39,Reference Prior, Santhakumaran and Gale48,Reference Fan, Wong and Fong49) . Participants in our study with early-term birth were 30–50 % less likely to initiate breast-feeding, and Canadian-born participants with early-term birth were 35 % less likely to continue breast-feeding at 6 months. Women giving birth early-term are more likely to have caesarean section(Reference Fan, Wong and Fong50), and their infants are more likely to be admitted to the neonatal intensive care unit(Reference Sengupta, Carrion and Shelton51) and to have a prolonged hospitalisation(Reference Tita, Landon and Spong52), all of which can interfere with breast-feeding initiation and duration. A review of 53 studies concluded that caesarean section reduced the odds of breast-feeding initiation by over 40 % but had no effect on breast-feeding duration in women who initiated breast-feeding(Reference Prior, Santhakumaran and Gale48). However, our analysis showed that caesarean birth remained significantly associated with lower odds of breast-feeding continuation at 6 months in Canadian-born participants, even among the subset of participants who initiated breast-feeding (see online supplementary material, Supplemental Table S3).
Studies in other countries have shown that immigrant women tend to breastfeed longer than native-born women(Reference Lok, Bai and Chan18,Reference Rio, Castello-Pastor and Del Val Sandin-Vazquez53) and that breast-feeding duration decreases with longer time since migration(Reference Lok, Bai and Chan18,Reference Barcelona de Mendoza, Harville and Theall54,Reference Harley, Stamm and Eskenazi55) . A recent meta-analysis of twenty-nine studies found that while immigrant women were marginally more likely to initiate breast-feeding than non-immigrant women, they were twice as likely to continue breast-feeding for 12 to 24 weeks(Reference Dennis, Shiri and Brown17). However, more than one-half of the included studies (16/29) did not adjust for key socio-demographic variables, such as maternal age, education and family income. In our study, we found no significant association between migration status and migration characteristics and breast-feeding initiation or continuation and other studies in Canada have also shown conflicting findings. In one study of Canadian-born and immigrant women, Dennis et al. (Reference Dennis, Gagnon and Van Hulst56) found that migrant women were less likely to be breast-feeding exclusively at 16 weeks compared with Canadian-born women. As previously discussed, Canadian-born and non-Canadian-born participants in our study had high maternal education levels, possibly contributing to the similarity of breast-feeding rates. Furthermore, one-third of our non-Canadian-born participants immigrated to Canada before 18 years of age, possibly making them more acculturated to the Canadian lifestyle.
The current study used a large prospective national cohort with detailed data collection at numerous time points throughout the first several years of life. The dropout rate was low, and breast-feeding follow-up data were collected on 88·2 % of the sample. However, study participants had higher maternal education levels and socio-economic status when compared with the general Canadian population(57), which may account for the high breast-feeding initiation rates and fewer differences between Canadian-born and non-Canadian-born participants than shown in other studies. Therefore, these findings may not be generalisable to the larger population of breast-feeding women. High breast-feeding initiation rates may have affected our ability to determine factors affecting initiation. Another limitation was the exclusion of participants who did not speak and read English as this could have excluded newly arrived immigrants who may be less acculturated to Canadian society and have higher breast-feeding rates. In addition, participants without follow-up breast-feeding data were more likely to be younger with lower socio-economic status, factors which have repeatedly been shown to be associated with lower rates of breast-feeding initiation and continuation(Reference Cohen, Alexander and Krebs34). Because global breast-feeding rates vary substantially(58), the analysis of all non-Canadian-born participants as a single group may have affected the findings. Furthermore, variations in participant recruitment practices at different sites many limit the conclusions drawn from the regional differences in breast-feeding practices. In Vancouver, participants were recruited from a single site and all resided in the Lower Mainland of British Columbia, while in Winnipeg, participants were recruited either in Winnipeg or in a rural location in the province of Manitoba. Lastly, in an observational study, we may not be able to fully account for unmeasured confounders.
Conclusion
In the CHILD birth cohort, Canadian-born and non-Canadian-born women had similar breast-feeding initiation and continuation rates. Our findings suggest that rates of breast-feeding initiation and continuation in Canadian-born women are more strongly associated with socio-demographic characteristics than in non-Canadian-born women. Place of residence continues to be highly predictive of breast-feeding continuation in both groups of women, and further research is required to identify the causes of these disparities and to develop strategies to improve breast-feeding rates nationally.
Acknowledgements
Acknowledgements: We thank the CHILD Cohort Study (CHILD) participant families for their dedication and commitment to advancing health research. We thank the whole CHILD Cohort Study team, which includes interviewers, nurses, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers and receptionists. A special thank you to Lorena Vehling for generating the breast-feeding variables used in the current study. We sincerely thank the Labour and Delivery and Health Information Services staff at St. Boniface Hospital, Health Sciences Centre and Boundary Trails Health Centre for their support of the birth chart abstraction. Financial support: The CHILD Cohort Study was funded by the Canadian Institutes of Health Research and supported by the Allergy, Genes and Environment Network of Centres of Excellence (AllerGen NCE). No financial assistance was received in support of this secondary analysis. MBA is supported by the Canada Research Chairs program and is a Fellow of the Canadian Institute for Advanced Research (CIFAR) Humans and the Microbiome Program. ST is a Vanier Scholar funded through the Canadian Institutes of Health Research. Authorship: The research question and design of the project was formulated through discussions between R.C. and M.T., they performed statistical analysis, interpretation of results, wrote the manuscript and had primary responsibility for the final content. H.S.L.F. and K.D.B. performed statistical analysis, interpretation of results and reviewed the manuscript. S.T. developed the directed acyclic graph, advised the analysis plan and reviewed the manuscript. S.M. performed critical review and revision of the manuscript. A.B.B., P.M., S.E.T., T.M., M.R.S., P.S. and M.B.A. aided in acquisition of study data, reviewed manuscript and had approved the final content. Ethics of human subject participation: The current study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by Health Research Ethics Boards from academic institutions at each study site (The Hospital for Sick Children, McMaster University, University of Manitoba, University of Alberta, and University of British Columbia) as well as the birth hospitals at each recruitment site. Written informed consent was obtained from all participants.
Conflicts of interest:
M.B.A. receives research funding from the Canadian Institutes of Health Research, Research Manitoba, the Canada Foundation for Innovation, the Bill and Melinda Gates Foundation, the Manitoba Children’s Hospital Foundation, Prolacta Biosciences, Mitacs, CIFAR and the Garfield G. Weston Foundation. She regularly speaks at conferences and workshops on infant nutrition, some sponsored by Medela, the Institute for the Advancement of Breastfeeding & Lactation Education and Prolacta Biosciences. She has contributed without remuneration to online courses on breast milk and the infant microbiome produced by Microbiome Courses. She serves in a volunteer capacity as Secretary to the International Society for Research on Human Milk and Lactation and as a member of the National Academy of Sciences, Engineering and Medicine Committee on Scanning New Evidence on the Nutrient Content of Human Milk. ST serves in a volunteer capacity as the Mentorship Series coordinator for the International Society for Research in Human Milk and Lactation. R.C., M.T., K.D.B., H.S.L.F., A.B.B., P.M., S.E.T., T.M., M.R.S. and P.S. have no conflicts to report.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S1368980021004699








